Abstract
Introduction:
Older minority individuals are less likely to receive adequate health care than their white counterparts. This study investigates whether perceived racism is associated with delayed/forgone care among minority older adults, and whether poor doctor communication mediates this relationship.
Methods:
Study cohort consisted of minority participants, aged ≥65 years, in the 2015 California Health Interview Survey (n=1,756). Authors obtained data in November 2017, and statistical analyses were performed from February to April 2018. Multivariable logistic regression analyses were conducted with relevant covariates, including insurance coverage, years living in the U.S., and language. A mediation analysis was also performed.
Results:
Among minority older individuals, perceived racism was significantly associated with delayed/forgone care (AOR=3.92, 95% CI=1.38, 11.15, P=0.010). Poor doctor communication significantly and partially mediated the relationship (AOR=3.64, 95% CI=1.30, 10.21, p=0.014), accounting for 9.9% of the total effect.
Conclusions:
Perceived racism may contribute to health disparities for older minority individuals in part through doctors communicating messages that discourage adequate utilization of health care. Future research should explore culturally sensitive communication skills that reduce this barrier to receiving adequate health care.
INTRODUCTION
Although more than 98% of adults aged 65 years or older are covered through Medicare and other combinations of insurance types,1 racial/ethnic minority older adults continue to inadequately access health care, contributing to disparities in their health outcomes.2 Moreover, the proportion of Americans aged 65 years or older are projected to increase from 14.5% in 2014 to 23.5% in 2060, and the older population is becoming more racially and ethnically diverse.3 Improving the healthcare access of ethnic minority older adults is a national goal in the Healthy People 2020 initiative.4
Previous research documents that black and Hispanic older individuals are at higher risk of having unmet or undermet healthcare needs compared with white older people.5,6 Also, prior research has found a tendency for some healthcare providers to hold negative implicit attitudes toward patients of color and to express these biases through communications with their patients (e.g., subtle forms of disrespect or not recommending procedures).7 However, to the authors’ knowledge, the current study is the first to investigate whether perceived racism contributes to health disparities in delayed/forgone care among ethnic minority older adults. Furthermore, previous studies have not explored whether poor doctor communication, the mediator of the current study, may contribute to this disparity in delayed/foregone care.
Thus, two hypotheses are examined in minority older adults: (1) perceived racism contributes to delayed/forgone care, and (2) poor doctor communication mediates the association of perceived racism with delayed/forgone care.
METHODS
Study Population
The 2015 California Health Interview Survey (CHIS), the most recent year available when this study was conducted, was analyzed. A strength of the CHIS, the largest U.S. state-health survey,8 is that it is conducted in five languages to over-sample Asians, Hispanics, and other racial/ethnic minority groups.8 Inclusion criteria consisted of participants aged 65 years or older (n=6,972), who were racial/ethnical minority-group members with complete data (n=1,756).
The mean age of the sample was 71.7 (SD=6.4 years), consisting of non-Hispanic blacks (13.3%), Hispanics (32.3%), Asians (23.3%), and two or more racial/ethnic groups (31.1%; Table 1 provides further description of the cohort).
Table 1.
Selected Characteristics of Adults Aged ≥65 Years in California by Perceived Racism, 2015 CHIS
| Characteristics | Perceived racism | |||
|---|---|---|---|---|
| No, % | Yes, % | Total, % | p-value* | |
| Sample size | ||||
| Unweighted sample, N | 1,668 | 88 | 1,756 | |
| Weighted population in California, N | 1,834,103 | 82,456 | 1,916,559 | |
| Predisposing factors | ||||
| Age, years | ||||
| 65–74 | 63.1 | 83.8 | 64.0 | 0.002 |
| ≥75 | 36.9 | 16.2 | 36.0 | |
| Sex | ||||
| Female | 55.1 | 62.1 | 55.4 | 0.442 |
| Male | 44.9 | 37.9 | 44.6 | |
| Race/ethnicity | ||||
| Non-Hispanic black | 12.8 | 22.5 | 13.3 | 0.389 |
| Hispanic | 32.3 | 33.7 | 32.3 | |
| Non-Hispanic Asian | 23.4 | 21.2 | 23.3 | |
| Othera | 31.5 | 22.7 | 31.1 | |
| Marital status | ||||
| Married | 56.2 | 47.0 | 55.8 | 0.208 |
| Never married | 6.7 | 3.6 | 6.6 | |
| Otherb | 37.1 | 49.4 | 37.6 | |
| Geographic region | ||||
| Urban | 56.8 | 72.1 | 57.5 | 0.121 |
| Second city | 17.7 | 14.1 | 17.5 | |
| Suburban | 17.4 | 12.1 | 17.2 | |
| Town and rural | 8.2 | 1.7 | 7.9 | |
| Years in U.S. | ||||
| U.S. born | 43.4 | 47.3 | 43.5 | 0.700 |
| <5 | 1.4 | 0.0 | 1.3 | |
| 5–9 | 2.4 | 5.6 | 2.5 | |
| 10–14 | 1.0 | 1.5 | 1.0 | |
| ≥15 | 52.0 | 45.7 | 51.7 | |
| English proficiency | ||||
| English only | 34.0 | 38.2 | 34.2 | 0.493 |
| ESLc - very well/well | 32.2 | 21.8 | 31.8 | |
| ESL - not well/not at all | 33.8 | 40.0 | 34.1 | |
| Educational attainment | ||||
| High school diploma or less | 57.5 | 67.6 | 57.9 | 0.258 |
| Some college | 17.9 | 16.4 | 17.8 | |
| College degree or more | 24.7 | 16.1 | 24.3 | |
| Enabling factors | ||||
| Poverty status | ||||
| ≤200% of FPLd | 49.7 | 57.2 | 50.0 | 0.531 |
| 201%–400% of FPL | 28.2 | 27.9 | 28.2 | |
| >400% of FPL | 22.2 | 14.9 | 21.9 | |
| Employment status | ||||
| Employed | 19.7 | 14.1 | 19.4 | 0.664 |
| Unemployed | 77.4 | 82.3 | 77.6 | |
| Othere | 2.9 | 3.5 | 3.0 | |
| Health insurance coverage | ||||
| Employment-based | 4.4 | 0.3 | 4.3 | 0.589 |
| Medicare only | 32.1 | 37.5 | 32.4 | |
| Medicaid only | 3.6 | 0.0 | 3.4 | |
| Medicare and Medicaid (dual eligible) | 38.0 | 38.2 | 38.0 | |
| Other | 20.2 | 22.4 | 20.3 | |
| Uninsured | 1.7 | 1.7 | 1.7 | |
| Need factors | ||||
| Self-reported health status | ||||
| Very good/excellent | 30.5 | 18.4 | 29.9 | 0.180 |
| Poor/fair/good | 69.5 | 81.6 | 70.1 | |
| Serious psychological distress | ||||
| Yes | 3.3 | 9.8 | 3.6 | 0.101 |
| No | 96.7 | 90.2 | 96.4 | |
| Health behavior - Disability status | ||||
| Yes | 50.3 | 66.8 | 51.0 | 0.062 |
| No | 49.7 | 33.3 | 49.0 | |
| Health behavior - Current smoking status | ||||
| Yes | 6.6 | 8.9 | 6.7 | 0.493 |
| No | 93.4 | 91.1 | 93.3 | |
| Health behavior - Binge drinking status | ||||
| Yes | 10.6 | 17.5 | 10.9 | 0.210 |
| No | 89.5 | 82.5 | 89.2 | |
| Health behavior - Obesity status | ||||
| Yes (BMI ≥30.0) | 27.0 | 35.9 | 27.4 | 0.274 |
| No | 73.0 | 64.1 | 72.6 | |
Note: compares proportion differences by perceived racial/ethnic discrimination using a Bonferroni-corrected, weight-adjusted chi-square statistic. Only age was significantly differed by perceived racism (p<0.01).
Includes two or more racial or ethnic groups.
Includes partnered, divorced/separated, or widowed
Indicates English as a second language
Indicates federal poverty level.
Includes with a job/business, but not at work, and looking for work.
Includes privately purchased and other public benefit programs.
Measures
Participants were asked: Was there ever a time when you would have gotten better medical care if you had belonged to a different race or ethnic group? Response options were yes or no.
Participants were asked: How often does your doctor or medical provider listen carefully to you? and How often does your doctor or medical provider explain clearly what you need to do to take care of your health? Responses of never or sometimes were coded as 1; whereas responses of always or usually were coded as 0.
Participants who responded yes to any of the following questions were categorized as having experienced delayed or foregone care: During the past 12 months, did you delay or not get a medicine that a doctor prescribed for you? and During the past 12 months, did you delay or not get any other medical care you felt you needed—such as seeing a doctor, a specialist, or other health professional? Forgoing necessary care was a subset of those reporting delaying/not getting medical care.
Covariates that could predict the outcome consisted of predisposing, enabling, and need factors.9 Predisposing factors included: age, sex, marital status, geographic region, years in the U.S., English proficiency, and education. Enabling factors included: income, employment status, and health insurance coverage. Need factors included: self-reported health status, serious psychological distress, disability status, and health behaviors (i.e., smoking status, binge drinking, and obesity status).
Statistical Analysis
To examine whether perceived racism acted as determinant of delayed/forgone care, regression of delayed/forgone care on perceived racism was performed. To examine whether poor doctor communication mediated the perceived racism-delayed/forgone care association, two complementary mediation analyses10,11 were conducted. These multivariable logistic regression analyses adjusted for all covariates. Analyses were conducted using Stata, version 15.1 MP/Core-6, adjusting for weights that took into account CPUS’s complex survey sample design.8
RESULTS
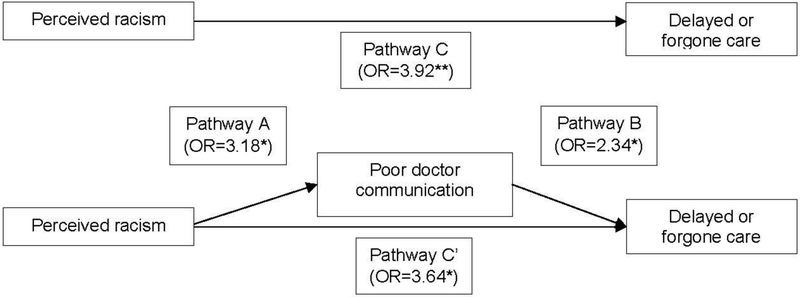
In support of the first hypothesis, perceived racism was associated with 3.92 times greater odds of delayed/forgone care (95% CI=1.38, 11.15, p=0.010). Perceived racism was also associated with 3.18 times greater odds of poor doctor communication (95% CI=1.27, 7.95, p=0.014).Mediation analyses, using the three Baron and Kenny mediation criteria10 and controlling for covariates, supported the second hypothesis that poor doctor communication mediates the association between perceived racism and delayed/forgone care. The first criterion was met by the independent variable predicting the outcome. The second criterion was met by poor doctor communication being associated with 2.34 times greater odds of having delayed/forgone care (95% CI=1.13, 5.03, p=0.024). The third criterion was met by the magnitude of perceived racism decreasing to 3.64 times greater odds of having delayed/forgone care (95% CI=1.30, 10.21, p=0.014; Figure 1). As perceived racism still predicted delayed/forgone care with poor doctor communication entered, the poor doctor communication was a partial mediator.
Figure 1.
Conceptual model of the mediating effect of poor doctor communication on the relationship between perceived racism and delayed/forgone care in minority older adults.
Note: *<0.05, **<0.01, and ***<0.001. All covariates from the full model were adjusted for.
Further, VanderWeele’s mediation approach,11 also confirmed the second hypothesis: controlled direct effect (coefficient=2.18, 95% CI=1.37, 3.45, p=0.001), natural indirect effect (coefficient=1.22, 95% CI=1.15, 1.31, p<0.001), and marginal total effect (coefficient=2.66, 95% CI=1.68, 4.21, P<0.001) were significant. This partial mediator accounted for 9.9% of the total effect.
DISCUSSION
As predicted, the perception of racism increased the likelihood of delaying or forgoing necessary medical care, and poor doctor communication played a significant mediating role in the relationship.
Although the Medical Board of California enacted the Cultural and Linguistic Competency of Physicians Act in 2003,12 the current findings suggest that poor communication skills of doctors and their biases still play roles in older minority patients delaying or forgoing necessary medical care. These findings suggest that healthcare providers treating older minority patients would benefit from training to reduce bias and increase culturally competent communication skills.
As poor doctor communication was a partial mediator of the association between perceived racism and delayed/forgone care, other mediators should be explored. One possible factor is distrust of healthcare providers by minority elderly patients due to observing or hearing about acts of racism. Regardless of whether this is found to be another factor, healthcare settings might want to find ways to increase trust, and ethnic minority older patients should be encouraged to advocate for treatments and second opinions.
A strength of this study is that a number of factors were adjusted, which could explain unmet/foregone care including: English as a non-native language, years living in the U.S., poor health behaviors, and not having health insurance coverage. That is, perceived racism appears to contribute to the disparity above and beyond these factors.
Future research should explore whether the dynamics reported in this study differ between diverse ethno-geriatric population groups. In the current study, subgroup analyses by minority group were not performed due to limited sample sizes. In addition, future qualitative research can examine which components of doctor communication contribute to unmet health needs of minority older adults.
CONCLUSIONS
Overall, this study highlights that perceived racism contributes to disparities in care access among minority older adults. Inadequate doctor communication may discourage minority older adults from receiving needed medical care in a timely manner. As a key mediator, doctor communication skills should be amenable to intervention, potentially decreasing perceived racism and increasing healthcare access to minority older adults.
Acknowledgments
The National Institute on Aging supported Rhee (#T32AG019134), Van Ness (#P30AG021342), and Levy (U01AG032284-05A1).
This study was presented at the 2018 Annual Scientific Meeting of American Geriatrics Society and was a Presidential Poster Award Finalist.
The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
All authors have completed and submitted the International Committee of Medical Journal Editors Form for Disclosure of Potential Conflicts of Interest, and none were reported. This article does not contain any studies with human participants or animals performed by the authors. All research procedures performed in this study are in accordance with the ethical standards of the IRB at Yale University School of Medicine (#2000021664).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Publicly available data were obtained from the University of California, Los Angeles (UCLA) Center for Health Policy Research (http://healthpolicy.ucla.edu/chis/Pages/default.aspx). Analyses, interpretation, and conclusions are solely those of the authors and do not necessarily reflect the views of the UCLA Center for Health Policy Research.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Research Data Asistance Center (ResDAC). Strengths, weaknesses, and applications of Medicare data, www.resdac.org/training/workshops/intro-medicare/media/2. Published 2012. Accessed October 12, 2018.
- 2.Verhagen I, Steunenberg B, de Wit NJ, Ros WJ. Community health worker interventions to improve access to health care services for older adults from ethnic minorities: a systematic review. BMC Health Serv Res 2014;14:497 10.1186/s12913-014-Q497-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colby SL, Ortman JM. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. Carr Popul Rep Popul Estim Proj 2014;P25–1143. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Accessed October 12, 2018. [Google Scholar]
- 4.HHS. Healthy People 2020 Topics and Objectives: Access to Health Services www.healthypeople.gov/2020/topics-obiectives/topic/Access-to-Health-Services. Accessed October 12, 2018.
- 5.Lima JC, Allen SM. Targeting risk for unmet need: not enough help versus no help at all. J GerontolB Psychol Sci Soc Sci 2001;56(5):S302–S310. https://doi.Org/10.1093/geronb/56.5.S302. [DOI] [PubMed] [Google Scholar]
- 6.Berridge C, Mor V. Disparities in the prevalence of unmet needs and their consequences among black and white older adults. J Aging Health. 2018;30(9): 1427–1449. 10.1177/0898264317721347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60–e76. 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.California Health Interview Survey. CHIS 2015–2016 Sample design. http://healthpolicy.ucla.edu/chis/design/Documents/sample_desc_2015.pdf. Published 2017. Accessed October 12, 2018.
- 9.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health SocBehav 1995;36(1): 1–10. 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 10.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers SocPsychol 1986;51(6): 1173–1182. https://doi.Org/10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 11.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2): 137–150. 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medical Board of California. Cultural and linguistic competency workshop. www.mbc.ca.gov/About_Us/Meetings/2010/Materials/materials_20100511_culture.pdf. Published 2010. Accessed May 25, 2018.