Abstract
BACKGROUND:
While Medicaid expansion has improved access to primary care services, its impact on surgical specialty utilization remains unclear. To determine whether Medicaid expansion was associated with increased compared utilization rates of total hip arthroplasty (THA) and total knee arthroplasty (TKA) in Illinois (which expanded Medicaid) relative to Missouri (which did not expand Medicaid).
METHODS:
Using administrative data sources, we analyzed 374,877 total hospitalizations (236,333 in Illinois and 138,544 in Missouri) for THA/TKA from 2011–2016 (Illinois’ Medicaid expansion date: 1/1/2014).
RESULTS:
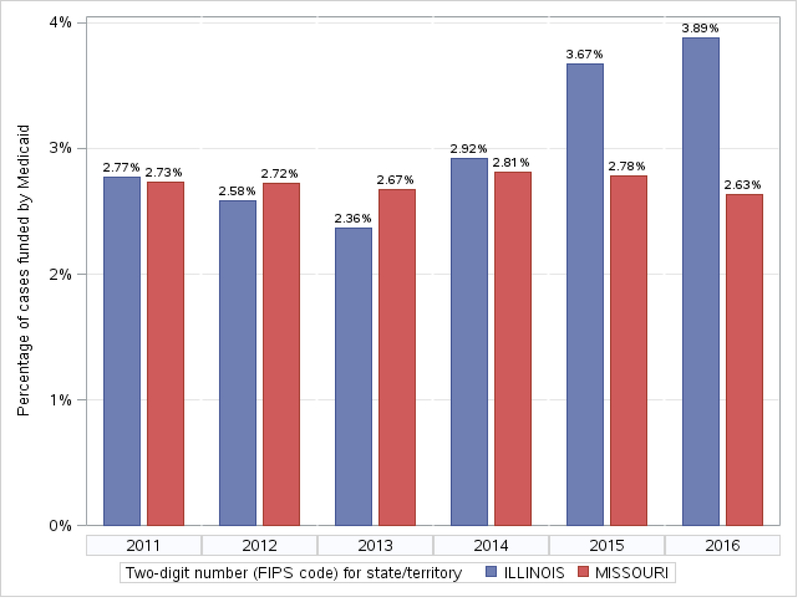
The percentage of THA/TKA funded by Medicaid in Illinois was 2.4% in 2013 and 3.9% in 2016 (Missouri - 2013: 2.7%; 2016: 2.6%). A difference-in-difference analysis (adjusted for patient age and sex, county-level Area Deprivation Index, and number of orthopaedic surgeons) demonstrated a statistically significant increase in Medicaid-funded THA/TKA in Illinois in 2016 compared to 2013 (p=0.012).
CONCLUSIONS:
Our study demonstrates that Medicaid expansion in Illinois was associated with increased utilization of THA and TKA. Further study is needed to understand the impact of Medicaid expansion in other states and for other procedures.
Keywords: health policy, total hip arthroplasty, total knee arthroplasty, Medicaid expansion, Affordable Care Act
Introduction
Passage of the Affordable Care Act (ACA) has led to increases in health insurance coverage, with 90% of Americans having health insurance in 2015.[1] Many Americans who recently gained health insurance under ACA are covered by Medicaid, particularly in states that expanded Medicaid programs. In Medicaid expansion, income-based enrollment thresholds were relaxed with the intent of increasing the number of enrollees. This has allowed low-income adults greater self-reported access to primary care providers, medical specialists, preventive care, and medications[2]; however whether Medicaid expansion also improved access to specialty surgical care remains unclear. In particular, patients with Medicaid insurance seeking elective specialty surgeries have difficulty scheduling appointments, require a PCP referral, have longer waits, and travel further for care than patients with commercial insurance.[3–6] These challenges, combined with the fact that 40% of orthopaedic surgeons were not accepting new patients with Medicaid as of 2011[7], demonstrate how patients can be at risk for under-utilization of specialty services like orthopaedic care.
Prior population-based studies have analyzed utilization of orthopaedic services under Medicaid expansion that occurred before the ACA. There was a steady increase in utilization of orthopaedic and plastic surgeries among Medicaid beneficiaries after New York expanded Medicaid in 1999.[8, 9] Another study demonstrated an increase in elective, preference-sensitive procedures after Massachusetts implemented health care reform in 2007.[10] However, the generalizability of these findings is limited by the absence of a contemporary comparison population, specifically in the light of recent ACA-related Medicaid expansion. Of the 50 states and the District of Columbia, 32 have implemented Medicaid expansion; 5 have adopted Medicaid expansion but not yet implemented it; and 14 states have chosen not to adopt Medicaid expansion.
While some contemporary studies have shown that expanded Medicaid coverage increases access to care compared to non-expansion states, these findings are limited to self-reported access to outpatient medical services and preventative care - not actual utilization of specialty surgical procedures.[11] The only surgical procedures that have been compared between non-expansion and expansion states post-ACA are urgent interventions, such as heart valve arthroplasty or coronary bypass procedures.[12] Examining utilization of non-elective procedures is a suboptimal indicator of access to surgical specialty care, as it does not address ability of patients to undergo elective, discretionary procedures occurring outside of emergency conditions. We chose to evaluate access to total hip arthroplasty (THA) and total knee arthroplasty (TKA) because they improve quality of life and are commonly performed, but represent a substantial cost center for insurers.[13,14] Furthermore, disparities in both access to THA/TKA and postoperative outcomes have been demonstrated among Medicaid beneficiaries.[15,16]
In our study, we compared utilization rates of THA and TKA between two adjacent states, Illinois and Missouri, with divergent Medicaid expansion policies: Illinois underwent Medicaid expansion under the ACA while Missouri did not. We hypothesized that rates of Medicaid-funded THA/TKA increased in Illinois relative to Missouri, starting in 2014.
Methods
Data for this retrospective cross-sectional study were obtained from Hospital Industry Data Institute (HIDI; Missouri Hospital Association, Jefferson City, MO). The datasets from HIDI include all hospital discharges in Missouri and Illinois from 2011 to 2016. Exemption from further human subjects research review was obtained from our institutional review board. Cohort selection included all hospital admissions in Missouri and Illinois from 2011 to 2016 for adults aged 18–99 years coded with an ICD-9-CM procedure code for THA (81.51) or TKA (81.54). Hospitalizations coded for spina bifida and craniotomy were excluded to minimize influence of complex chronic conditions associated with multiple hospitalizations (Appendix Table A). Hospitalizations coded with multiple fractures (likely representing a polytrauma; Appendix Table A) were similarly excluded. Additional admission-level variables included patient age and sex. Patients under age 18 years or over age 99 were excluded.
DEPENDENT VARIABLE:
The dependent variable in our analysis was percentage of THA and TKA with Medicaid listed as primary payer. The other primary payer categories were Medicare, commercial insurance, Workers Compensation, and other (including uninsured).
COUNTY-LEVEL MARKET CHARACTERISTICS:
Market characteristics were calculated at the county level, using information from the primary dataset (HIDI) and Area Health Resources File (AHRF, https://datawarehouse.hrsa.gov/topics/ahrf.aspx). Hospital zip code was linked to AHRF via hospital’s county Federal Information Processing Standard (FIPS) code. Each variable was linked per county and year; when HIDI data contained more years than AHRF, the last complete prior year of AHRF data was used. Physician supply data (number of non-federally employed orthopaedic surgeons) and county insurance estimates (Medicaid and Medicare eligibility) from AHRF were included. The number of non-federally employed orthopaedic surgeons were not available for 2015 and 2016; for these years, the 2014 data were used. Socioeconomic data for each county were median household income (from AHRF) and Area Deprivation Index, a measure of social deprivation obtained from University of Wisconsin Health Innovation Program.[17] Market competitiveness for THA/TKA was measured by Herfindahl-Hirschman Index (HHI),[18] which was calculated from the dataset of eligible THA/TKA hospitalizations by summing number of THA/TKA admissions per hospital (h), aggregating to total in a county (c) and computing sum of all hospital market shares squared, per FIPS and year.
EXPOSURE TO MEDICAID EXPANSION:
Illinois Governor Pat Quinn signed Medicaid expansion into law in July 2013, with expanded eligibility going into effect on January 1,2014. Missouri did not expand its Medicaid program. The contrasting Medicaid expansion policies in these adjacent states provide the opportunity to study the natural experiment of whether the policy has resulted in increased utilization of care.
DIFFERENCE-IN-DIFFERENCES ANALYSIS:
We used a multivariable difference-in differences (DID) model to estimate the association between Medicaid expansion in Illinois vs. the control state of Missouri. DID is a quasi-experimental approach commonly used with observational data.[19] Variation over time and across groups facilitates a longitudinal analysis of trends, and difference between trends across two groups implies causal impacts, subject to model assumptions. Our dependent variable was a binary indicator for whether the primary payer for admission was Medicaid or any other source (Medicare, private insurance, uninsured, other). Following DID conventions, we modeled likelihood of Medicaid payment using linear regression (a linear probability model). Linear regression has the advantage of providing directly interpretable coefficients, which represent changes in proportion of orthopaedic procedures performed in Medicaid patients in a given state-year.[20] Control variables in the final model were a state indicator for Illinois, year fixed effects (2012–2016), county-level Area Deprivation Index, patient sex, patient age, number of orthopaedic surgeons in each county, and county-level Herfindahl-Hirs chman Index. To estimate the impacts of Medicaid expansion on likelihood of a surgery being paid by Medicaid, we examined the interaction terms between time (postexpansion years 2014, 2015, and 2016) and policy variable (Illinois state indicator variable).[19] The reference group is Illinois*2011 (the first year of the study).
SAMPLE SIZE CALCULATION:
An a priori sample size calculation was performed using Healthcare Utilization Project aggregate data from 2013 (HCUPnet, https://hcupnet.ahrq.gov/HCUPnet.jsp), which indicate that Medicaid was the primary payer for 3.17% of all cases for our selected ICD-9 procedure codes. To adjust for unequal population sizes, data from Kaiser Family Foundation (https://www.kff.org/statedata/) were used to calculate an IL:MO population ratio. To evaluate a 25% difference in proportion of cases with Medicaid listed as primary payer in the post-ACA period, a total of 20,743 patients (14,536 in IL and 6,207 in MO) were necessary over the study period with 80% power (alpha=0.05, 2-tailed).
Potential sources of confounding included secular trends in THA/TKA utilization (which is accounted for by using a difference-in-differences approach comparing two geographically-contiguous states with similar demographic composition) and the potential for clustering of results at the hospital-level. All models used heteroscedasticity-robust standard errors, clustered at hospital level. The final sample included 374,877 observations, and 241 hospitals, so accounting for correlation (clustering) at hospital level is important. Without this, the model would treat all observations as fully independent and overstate statistical significance.[21]SAS version 9.4 was used for all data management and analysis (SAS Institute, Cary, NC). Models were checked and confirmed using Stata 15.0 (Stata Corp, College Station, TX) by a second analyst.
Results
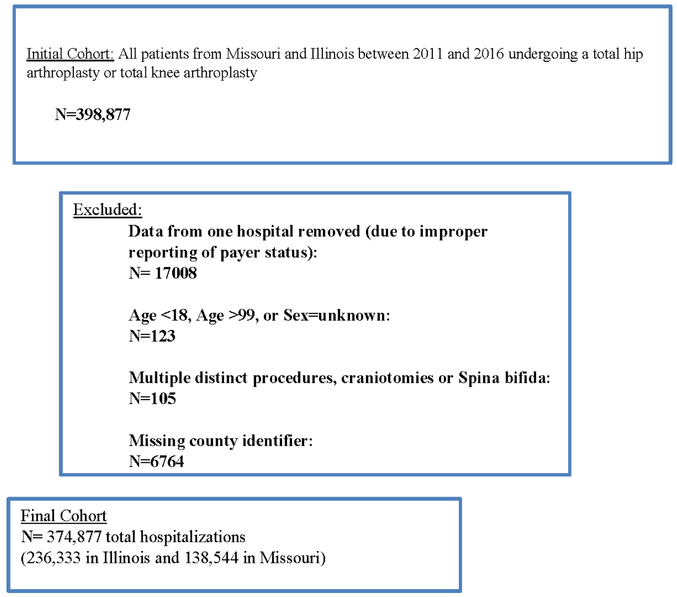
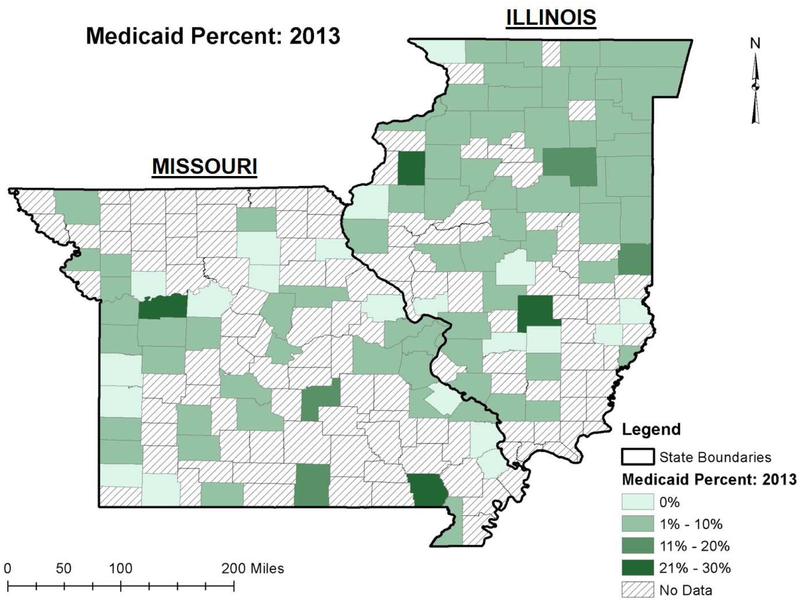
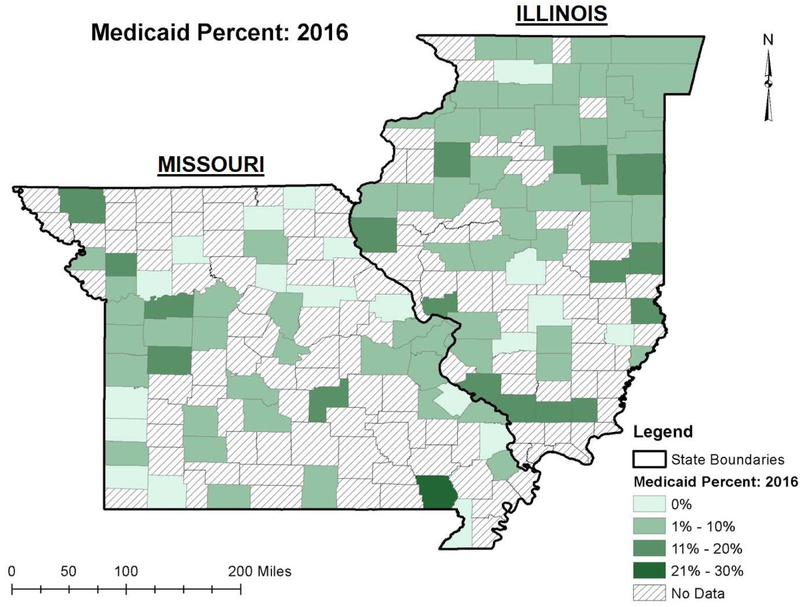
From 2011–2016, there were 374,877 total hospitalizations (236,333 in Illinois and 138,544 in Missouri) associated with THA/TKA (FIGURE 1;TABLE 1). TKA composed 65% of included admissions in Illinois and 69% of included admissions in Missouri (TABLE 1). Over the study period, the percentage of cases paid for by Medicaid was relatively unchanged in Missouri and increased in Illinois (Unadjusted results; TABLE 2). County-level changes are demonstrated in the heat maps in FIGURES 2A–2C. In our DID model adjusted for patient age, patient sex, county-level Area Deprivation Index, county-level Herfindahl-Hirschman Index, and number of orthopaedic surgeons in the county, there was a statistically significant increase in Medicaid-funded THA/TKA in Illinois in 2016 (IL*2016, p=0.012) (relative to IL*2011), indicating that Illinois’ expansion of Medicaid was associated with an increase in Medicaid-funded inpatient orthopaedic surgeries (FIGURE 3). In years 2014 and 2015, there were slight increases that did not reach statistical significance (IL*2014, p=0.719; IL*2015, p=0.092) (relative to IL*2011). There were no significant differences in interaction terms in the pre-expansion years (IL*2012, p=0.702; IL*2013, p=0.458) (relative to IL*2011), satisfying the assumption of parallel trends. In our DID linear regression model, patient age, sex, number of orthopaedic surgeons in the county, and county-level Area Deprivation Index all had statistically significant associations with Medicaid-funded THA/TKA (TABLE 3). Pairwise comparisons of the interaction variables for post-expansion years vs 2013 (last year pre-expansion) indicates significant increases in 2015 and 2016 (p=0.003 and p<0.001, respectively) (TABLE 3).
FIGURE 1.
Flow diagram for cohort assembly.
TABLE 1.
Baseline characteristics of study cohort. (IQR=interquartile range)
| Variable | Illinois | Missouri |
|---|---|---|
| Total admissions | 236,333 | 138,544 |
| Total knee arthroplasty: number (% of state total) | 154,474 (65.4%) | 96,028 (69.3%) |
| Total hip arthroplasty | 81,859 | 42,516 |
| Female Admissions: number (% of state total) | 143,009 (60.5) | 83,023 (59.9) |
| Median Area Deprivation Index (IQR) | 68.8 (22.8) | 87.3 (19.0) |
| Median number of orthopedic surgeons in each county (IQR) | 90 (489) | 49 (148) |
| Number of admissions by year: | ||
| 2011 | 35,547 | 20,321 |
| 2012 | 36,036 | 21,221 |
| 2013 | 37,485 | 22,597 |
| 2014 | 39,849 | 23,950 |
| 2015 | 41,889 | 23,962 |
| 2016 | 45,527 | 26,493 |
TABLE 2.
Payer mix for all procedures, stratified by state and year. Unadjusted raw percentage point difference between years 2016 and 2013 (last pre-expansion year in Illinois) shown on the right.
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2016–2013 (Unadjusted) | ||
|---|---|---|---|---|---|---|---|---|
| Commercial | MO | 38.8% | 38.5% | 38.8% | 39.2% | 39.7% | 38.6% | −0.2% |
| IL | 41.7% | 41.1% | 41.9% | 43.8% | 44.6% | 41.6% | −0.3% | |
| Medicaid | MO | 2.7% | 2.7% | 2.7% | 2.8% | 2.8% | 2.6% | −0.1% |
| IL | 2.8% | 2.6% | 2.4% | 2.9% | 3.7% | 3.9% | 1.5% | |
| Medicare | MO | 56.0% | 56.4% | 56.2% | 55.3% | 54.4% | 55.7% | −0.5% |
| IL | 52.4% | 52.8% | 53.1% | 51.4% | 49.2% | 51.7% | −1.4% | |
| Other/Uninsured | MO | 2.0% | 2.0% | 2.0% | 2.3% | 2.7% | 2.9% | 0.9% |
| IL | 3.1% | 3.5% | 2.7% | 1.9% | 2.5% | 2.8% | 0.1% | |
| Workers Compensation | MO | *** | *** | *** | *** | *** | *** | n/a |
| IL | *** | *** | *** | *** | *** | *** | n/a | |
indicate that values (number of cases) are less than 11, which cannot be reported in accordance with our data use agreements.
FIGURE 2.
Percentage of total hip and knee arthroplasties in Illinois and Missouri that were funded by Medicaid in 2013 (2A; last year prior to Medicaid expansion in Illinois) and 2016 (2B). Percentage point change within county is demonstrated in 2C.
FIGURE 3.
Bar graph demonstrating year-to-year percentage of total hip arthroplasty and total knee arthroplasty funded by Medicaid in Illinois and Missouri. Note that Illinois expanded Medicaid on January 1,2014.
TABLE 3.
Regression covariate estimates for the difference-in-difference regression model.
| Parameter | Estimate | Std Error | 95% Confidence Interval | p value |
|---|---|---|---|---|
| Illinois (reference: Missouri) | 0.00926 | 0.00698 | −0.00448, 0.02300 | 0.186 |
| Hlinois*2011 | ||||
| Illinois*2012 | −0.00105 | 0.00274 | −0.00645, 0.00435 | 0.702 |
| Illinois*2013 | −0.00250 | 0.00337 | −0.00914, 0.00413 | 0.458 |
| Illinois*2014 | 0.00163 | 0.00452 | −0.00727, 0.01053 | 0.719 |
| Illinois*2015 | 0.00895 | 0.00529 | −0.00147, 0.01938 | 0.092 |
| Illinois*2016 | 0.01405 | 0.00555 | 0.00312, 0.02499 | 0.012 |
| Area Deprivation Index | 0.00065 | 0.00013 | 0.00038, 0.00091 | 0.000 |
| Number of orthopedic surgeons | 0.00004 | 0.00002 | 0.00000, 0.00008 | 0.041 |
| Female (reference: male) | 0.00977 | 0.00119 | 0.00742, 0.01212 | 0.000 |
| Age | −0.00306 | 0.00031 | −0.00366, −0.00246 | 0.000 |
| Herfindahl-Hirschman Index | 0.02011 | 0.01167 | −0.00294, 0.04315 | 0.087 |
| Pairwise comparisons of interaction terms | Contrast sum of squares | Std Error | T value | p value |
| niinois*2012 vs Illinois*2013 | 0.00146 | 0.00240 | 0.61 | 0.544 |
| Illinois*2014 vs Illinois*2013 | 0.00413 | 0.00316 | 1.31 | 0.192 |
| Illinois*2015 vs Illinois*2013 | 0.01146 | 0.00377 | 3.04 | 0.003 |
| Illinois*2016 vs Illinois*2013 | 0.01656 | 0.00393 | 4.21 | <0.001 |
Individual years (without state interaction) and model intercept were also included in the regression model, but are not shown here. State*year interaction terms demonstrate a statistically significant downward associations in Medicaid-funded orthopaedic surgeries prior to the date of Medicaid expansion in Illinois (January 1,2014) and significant upward associations in the post-expansion years. Pairwise comparisons of the state*year interaction variable in post-expansion years vs 2013 are included at the bottom of the table.
Discussion
Patients with scarce financial resources struggle to access health care services. Obtaining health insurance is one major hurdle, only to be followed by difficulty in finding physicians who will accept their insurance. While ACA expansion of Medicaid programs is meant to address the former, the latter remains a major barrier because many physicians (and particularly specialists) have chosen not to treat patients with Medicaid insurance.[7] Prior work has shown that Medicaid expansion has led to improved self-reported access to primary care and medical specialty services.[2] Furthermore, we have demonstrated increased utilization of a subspecialty surgical service (total joint arthroplasty) in a Medicaid expansion state compared to a state without expansion. Examination of insurance types during the study period demonstrated that the proportion of cases with a primary payer of Medicaid in Missouri remained flat during the study period. In contrast, in Illinois, the proportion of Medicaid-funded cases increased (TABLE 2).
Our findings are relevant to the ongoing conversation about access to care following Medicaid expansion. We have substantiated prior findings of increased surgical subspecialty care reported by Aliu et al, Giladi et al, and Ellimoottil et al after pre-ACA Medicaid expansions in New York and Massachusetts. [8–10] We have also expanded on recent ACA-related findings of self-reported increases in access to care following Medicaid expansion by demonstrating increase in actual utilization.[2, 11] While we have demonstrated increased access to total joint arthroplasty in this two-state comparison, access to specialty care remains an issue for other specialties.[22, 23] Additionally, we have not analyzed specific barriers presented to Medicaid beneficiaries attempting to access services, such as narrower networks of providers willing to see patients with Medicaid.[7] Our analysis adjusted for number of orthopaedic surgeons within each county but because we do not have provider-level data, we are unable to evaluate whether Medicaid expansion resulted in changes in surgeon willingness to provide surgery to Medicaid beneficiaries. While it is often proposed that low reimbursements deter physicians from treating Medicaid patients, the fee schedules for these particular surgeries did not appreciably change in either state during the study period.
Because each state administers their own Medicaid program, it is difficult to extrapolate the national implications if more states were to expand their Medicaid eligibility programs. In 2014, there were 44,415 discharges associated with THA and TKA with Medicaid listed as the primary payer (https://hcupnet.ahrq.gov/). This was 4.2% of all THA/TKA cases listed. In our unadjusted analysis, there was a 62.5% increase in Medicaid-funded THA/TKA in Illinois (2.4% in 2013 and 3.9% in 2016) after implementation of Medicaid expansion. If this percentage increase is applied to the national data from 2014, we estimate 72,174 THA/TKA funded by Medicaid. We cannot predict the economic implications of this increase in caseload since Medicaid is administered at a state level (and reimbursement levels vary by state).
Our analysis is subject to limitations, particularly those surrounding the DID analysis. The DID analysis relies on the assumptions of parallel trends (common trajectories during the pre-expansion period) and common shocks (unobservable or un-modeled events affecting both groups equally). Our model satisfied the assumption of parallel trends, as there were no significant associations in the year*state variable prior to Illinois’ Medicaid expansion on January 1,2014. The common shocks assumption is not directly testable but is reasonable for two bordering Midwest states with similar demographics and economies. Based on our knowledge and work as part of the local health policy and medical/orthopaedic communities, we are not aware of any systematic changes which are not included and which would threaten the validity of this model. The Center for Medicare and Medicaid Services introduced voluntary bundled payment pilot programs (Bundled Payments for Care Improvement; BPCI) from 2013 to 2016 for THA and TKA and the Comprehensive Care for Joint Replacement (CJR) bundled payment program on April 2016, but these payment reforms are specified for Medicare beneficiaries only. While it is possible that hospitals and surgeons may have modified their practices in preparation for these programs, only four hospitals (1 in Missouri and 3 in Illinois) participated in BPCI and only one Metropolitan Statistical Area (St. Louis) has been selected for the CJR program within our two-state sample.[24, 25] Additionally, the physician fee schedules by Medicare and Medicaid for these procedures were stable over this time period. Additional limitations of the model include our limited number of control variables and the possibility of spillover effects across states. Our data use agreements with HIDI permitted us to use only a small set of individual characteristics; if available, other sociodemographic patient factors associated with health care use and insurance would have been desirable (e.g., income, education, family structure, neighborhood). We capture some of these factors through Area Deprivation Index, although this county-level variable was matched to the hospital ZIP code, and some patients reside in a different localities from the hospital of service. Similarly, defining HHI at county level may not capture the broader market environment in some parts of each state. However, we have no reason to believe there are any systematic differences in these measurement differences between Missouri or Illinois or over time.
At a time in which the ACA faces substantial modification or potential repeal, our study provides empirical data that a major component of the ACA (Medicaid expansion) was associated with increased utilization of THA and TKA in Illinois. Given the variability among Medicaid programs, further study is needed to understand the impact of Medicaid expansion in other states and for other procedures.
Supplementary Material
ACKNOWLEDGEMENTS:
Author CJD was supported by grant number UL1 TR000448, Sub award KL2 TR000450 from the NIH-National Center for Advancing Translational Sciences (NCATS), components of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. CJD was also supported by UL1TR002345 from NCATS. CJD received additional funding from Oak Ridge Associated Universities (ORAU Ralph E. Powe Junior Faculty Enhancement Award). The Center for Administrative Data Research (authors MAO, MK) is supported in part by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), Grant Number R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ), and Grant Number KM1CA156708 through the National Cancer Institute (NCI) at the National Institutes of Health (NIH).
APPENDIX
Appendix Table A.
Orthopedic Procedures and Exclusions Identified Through International Disease Classification 9th Revision (ICD9-CM) Procedure and Diagnosis Codes
| CODE DESCRIPTION | ICD9-CM PROCEDURE CODE | ICD9-CM DIAGNOSIS CODE |
|---|---|---|
| TOTAL KNEE REPLACEMENT | 81.54 | |
| TOTAL HIP REPLACEMENT | 81.51 | |
| CRANIOTOMY* | 01.12, 01.14, 01.20, 01.21, 01.22, 01.23, 01.24, 01.25, 01.28, 01.29, 01.31, 01.32, 01.39, 01.41, 01.42, 01.51, 01.52, 01.53, 01.59, 02.11, 02.12, 02.13, 02.14, 02.91, 02.92, 02.93, 07.51, 07.52, 07.53, 07.54, 07.59, 07.61, 07.62, 07.63, 07.64, 07.65, 07.68, 07.69, 07.71, 07.72, 07.79, 38.01, 38.11, 38.31, 38.41, 38.51, 38.61, 38.81, 39.28 | |
| TRAUMA CODES* | 820.09, 820.80, 733.14, 820.21, 820.00, 996.44, 808.00, 820.02, 733.13, 733.15, 820.03, 823.00, 821.23, 733.19 |
used for exclusion criteria
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
ETHICAL REVIEW COMMITTEE STATEMENT: We received an exemption from review from our Human Subjects Protection Office and Institutional Review Board. Please see included documentation.
REFERENCES
- [1].FastStats. cdc.gov. 2017. updated March 31,2017; cited 2017 October 26]. https://www.cdc.gov/nchs/fastats/health-insurance.htm. Last accessed: 2017
- [2].Wherry LR, Miller S. Early Coverage, Access, Utilization, and Health Effects Associated With the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study. Ann Intern Med. 2016;164(12):795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Calfee RP, Shah CM, Canham CD, Wong AH, Gelberman RH, Goldfarb CA. The influence of insurance status on access to and utilization of a tertiary hand surgery referral center. JBone Joint Surg Am. 2012;94(23):2177–2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Draeger RW, Patterson BM, Olsson EC, Schaffer A, Patterson JM. The influence of patient insurance status on access to outpatient orthopedic care for flexor tendon lacerations. J Hand Surg Am. 2014;39(3):527–533. [DOI] [PubMed] [Google Scholar]
- [5].Kim CY, Wiznia DH, Hsiang WR, Pelker RR. The Effect of Insurance Type on Patient Access to Knee Arthroplasty and Revision under the Affordable Care Act. J Arthroplasty. 2015;30(9):1498–1501. [DOI] [PubMed] [Google Scholar]
- [6].Kim CY, Wiznia DH, Wang Y, Save AV, Anandasivam NS, Swigart CR, et al. The Effect of Insurance Type on Patient Access to Carpal Tunnel Release Under the Affordable Care Act. J Hand Surg Am. 2016;41(4):503–509 e501. [DOI] [PubMed] [Google Scholar]
- [7].In Decker S. 2011 Nearly One-Third Of Physicians Said They Would Not Accept New Medicaid Patients, But Rising Fees May Help. Health Affairs. 2012;31(8):1673–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Aliu O, Auger KA, Sun GH, Burke JF, Cooke CR, Chung KC, et al. The effect of pre-Affordable Care Act (ACA) Medicaid eligibility expansion in New York State on access to specialty surgical care. Med Care. 2014;52(9):790–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Giladi AM, Aliu O, Chung KC. The effect of medicaid expansion in new york state on use of subspecialty surgical procedures by medicaid beneficiaries and the uninsured. J Am Coll Surg. 2014;218(5):889–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ellimoottil C, Miller S, Ayanian JZ, Miller DC. Effect of insurance expansion on utilization of inpatient surgery. JAMA Surg. 2014;149(8):829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance. JAMA Intern Med. 2016;176(10):1501–1509. [DOI] [PubMed] [Google Scholar]
- [12].Charles EJ, Johnston LE, Herbert MA, Mehaffey JH, Yount KW, Likosky DS, et al. Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes. Ann Thorac Surg. 2017;104(4):1251–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dall TM, Gallo P, Koenig L, Gu Q, Ruiz D. Modeling the indirect economic implications of musculoskeletal disorders and treatment. CostEff Resour Alloc. 2013;11(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fingar KR, Stocks C, Weiss AJ, Steiner CA. Most Frequent Operating Room Procedures Performed in U.S. Hospitals, 2003–2012: Statistical Brief #186 Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD)2006. [Google Scholar]
- [15].Browne JA, Novicoff WM, D’Apuzzo MR. Medicaid payer status is associated with in hospital morbidity and resource utilization following primary total joint arthroplasty. JBom Joint SurgAm. 2014;96(21):e180. [DOI] [PubMed] [Google Scholar]
- [16].Dy CJ, Marx RG, Ghomrawi HM, Pan TJ, Westrich GH, Lyman S. The potential influence of regionalization strategies on delivery of care for elective total joint arthroplasty. J Arthroplasty. 2015;30(1):1–6. [DOI] [PubMed] [Google Scholar]
- [17].Area Deprivation Index Datasets. HIPxChange.org. 2017; cited 2017 December 17]. https://www.hipxchange.org/ADI. Last accessed: 2017
- [18].Cutler DM, Scott Morton F. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964–1970. [DOI] [PubMed] [Google Scholar]
- [19].Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2402. [DOI] [PubMed] [Google Scholar]
- [20].Angrist J, Pischke J. Mostly harmless econometrics: an empiricists companion: Princeton: Princeton University Press; 2009 [Google Scholar]
- [21].White H A Heteroskedasticity-Consistent Covariance Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica. 1980;48(4):817–838. [Google Scholar]
- [22].Anandasivam NS, Wiznia DH, Kim CY, Save AV, Grauer JN, Pelker RR. Access of Patients With Lumbar Disc Herniations to Spine Surgeons: The Effect of Insurance Type Under the Affordable Care Act. Spine (Phila Pa 1976). 2017;42(15):1179–1183. [DOI] [PubMed] [Google Scholar]
- [23].Wiznia DH, Maisano J, Kim CY, Zaki T, Lee HB, Leslie MP. The effect of insurance type on trauma patient access to psychiatric care under the Affordable Care Act. Gen Hosp Psychiatry. 2017;45:19–24. [DOI] [PubMed] [Google Scholar]
- [24].Comprehensive Care for Joint Replacement Model. Center for Medicare & Medicaid Innovation Innovationcmsgov. updated April 2, 2018; cited 2018 April 20]. https://innovation.cms.gov/initiatives/cir. Last accessed: April 20
- [25].BPCI Initiative Episodes: Details on the Participating Health Care Facilities.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.