Abstract
A new strategy has been introduced in human health care, namely, achieving the best outcomes for the lowest cost and thus maximizing value for patients. In value‐based care, the only true measures of quality are the outcomes that matter to patients. When outcomes are measured and reported, it fosters improvement and adoption of best practices, thus further improving outcomes. Understanding outcomes is central in providing value and represents an opportunity for redefining veterinary patient care.
Value is created by improving the outcomes of patients with a particular clinical condition over the full cycle of care, which normally involves multiple specialties and care sites. To be successful, a key aspect of value based care is working as teams (integrated practice units) centered around the patient's clinical condition. As veterinary medicine has become more specialized and more complex, multidisciplinary communication and trust among the care team are paramount in providing value to patients (and clients).
Use of patient‐reported outcomes is an essential aspect for improving clinical care, because it enhances the connections among doctors and with patients. Designing and implementing owner‐reported outcomes in veterinary clinical practice will lead to an understanding of the effects of treatments on outcomes and quality of life (QOL) of our patients from the owner's perspective, a key way to assess a veterinary patient's QOL.
Keywords: integrated practice units, patient‐reported outcomes, value‐based care, veterinary care
Abbreviations
- ICHOM
The International Consortium for Health Outcomes Measurements
- IPU
integrated practice units
- OROMs
owner‐reported outcome measures
- PROMs
patient‐reported outcome measures
- QOL
quality of life
- TPLO
tibial plateau leveling osteotomy
- VBHC
value‐based health care
- VBVC
value‐based veterinary care
1. INTRODUCTION
The aim of this perspectives paper is to compare and cross‐learn from 2 industries, human and veterinary health care in the United States. Despite differences, commonalities do exist, such as the need to make decisions and trade‐offs with respect to medical spending that could improve or extend life, or treatment decisions triggered by health episodes that are difficult to forecast and involve emotional and financial trade‐offs. Both industries have experienced a rapid rise in spending as well as consolidation into large conglomerates.1, 2, 3 Care delivery for people and animals is provided by individuals with extensive education, training, and requirements for occupational licensure.3 Modern medicine is rapidly changing, powered by advances in information technology. Some argue that the field of medicine will advance more in the next 10 years than it has in the past century.3, 4 Two main differences are pet health insurance is less common and regulation is less prevalent in the veterinary care space.3
Traditional health care systems have rewarded volume over value, creating fee‐for‐service or procedure‐based payment and delivery systems that are highly fragmented, siloed, and disconnected.5 Health care spending has increased unsustainably to approximately double the rate of gross domestic product growth in most developed countries.6 Regardless of the higher costs, outcomes fluctuate across hospitals, regions, and countries, and there is not a clear causal relationship between money invested and health care delivered.6, 7
In the United States, 68% of households own a pet and approximately $69 billion was spent on pets during 2017. Of that, veterinary care represented $17 billion.8 Yet, even though the number of pets in the United States continues to increase, veterinary visits are down.9 Similar to human health care, the cost of veterinary medical care has been increasing faster than inflation for the last 20 years. One study concluded that veterinary compensation, when adjusted for inflation, has been decreasing. Thus, labor was not the source for the rising costs in that study, the cause of which remains elusive.3, 9 The human animal bond is very strong, meaning that pets are considered family members (humanization).10 In the event of illness, pet owners are likely to seek more specialized high‐end medical care for their animals. Multiple veterinarians (specialists and generalists), who may or may not be part of the same practice or building, are likely to be part of the diagnosis and treatment of sick animals. Hence, multidisciplinary collaboration and communication are fundamental for increasing the value provided to patients. As in human health care, communication is not only important among the care team but also with the patient's family.11
Over the past 50 years, an explosion in biomedical knowledge has occurred, with great innovations in treatments, surgical procedures, and management of conditions previously deemed untreatable. The future promises even further improvements.12 Despite this, the US health care is falling short in areas such as quality, outcomes, costs, and equity.12 Available knowledge is seldom applied to improve the patient's care experience, and the information arising from the care experience also is rarely used to advance the available knowledge base.12 It has been argued that the health care system needs to learn continuously with each care experience to provide improved outcomes and become more affordable.12
The foundation for a learning health care system is continuous knowledge development, improvement, and application. Despite the vast amount of information, doctors and patients often lack access to guidance that is relevant, timely, and useful for the circumstances at hand. To overcome this hurdle, the development of computing capabilities and analytics that will give real‐time information on patient care, and the ability to disseminate knowledge to the care team and to address regulations that could hinder progress, would be of paramount importance.12
Creating a culture that promotes a learning organization would mean knowledge generation and sharing from every patient interaction. This will require systematic problem solving, application of system engineering techniques, operational models that encourage and reward sustained quality and improved outcomes, transparency on cost and outcomes, and strong leadership and governance that define, disseminate, and support a vision of continuous improvement.12
2. VALUE‐BASED CARE
An innovative model called value‐based health care (VBHC) has been under implementation in the health care space and aims for a continuous improvement in health care through outcomes (learning) for a given level of cost.
Value maximization should be the goal for the health care team. Value is defined as health outcomes achieved that matter to patients relative to the cost of achieving those outcomes. Improving value requires either improving 1 or more outcomes without increasing costs or lowering costs without negatively affecting outcomes, or both.7 Important considerations regarding this concept are: value is not synonymous with cost savings; outcomes should be multidimensional and be defined by the context of the patient; cost determinations should include all costs and, as a result, some costs may increase for others to decrease; and, value is best considered on a long‐term basis.13
This approach signifies a shift in health care moving towards a patient‐centered system organized around the patient's needs.7 Patient‐centered care entails meaningful awareness, discussion, and engagement among patients, families, and clinicians on the evidence, risks and benefits, options and decisions in play.12 Patient‐centered care has been shown, in some instances, to improve outcomes, decrease costs, and improve patient experience and quality of life (QOL).12, 14 However, the ability of most hospitals and health care systems to achieve or assess improvements in multidimensional long‐term outcomes, at the same time as lowering overall costs, is far from optimal.13
Veterinary care also is facing difficulties, such as increasing cost, decreasing number of visits, and the need to foster better communication among the animal care team.9, 15, 16 If our objective in veterinary medicine is to provide medical care that is centered on the patient and its owner, then developing a framework called value‐based veterinary care (VBVC) would be ideal. Veterinarians embracing VBVC should enhance collaboration and cooperation by creating multidisciplinary health care teams, as well as beginning to develop ways to measure patient outcomes and the costs of care, which will lead to cross‐learning and improving the value provided to patients and clients. Doing so would bring veterinary care to a new level that will provide a competitive advantage for those embracing it.
3. WHAT IS OUTCOME?
As a Mayo Clinic cardiac surgeon stated: “All 5 of us are very good at what we do, but we all do it differently. At least 4 of us must be doing it wrong.” It has been documented that physicians can be overly optimistic about their ability to perform procedures. This phenomenon has been described as “macro uncertainty, micro certainty” in which physicians and nurses are overconfident in the value of their treatment for a particular patient (micro‐certainty) even in the absence of a general consensus as to which procedure is more clinically effective (macro‐uncertainty). Furthermore, a psychological bias exists for clinicians to perform more aggressive treatment. If the patient improves, the clinician gets the credit, but if the patient worsens, the doctor can say that he or she tried everything possible.17 Physicians and veterinarians may have starkly different views about how to treat the same patient.17 In health care, increased standardization and customization is leading to improved value care.2, 18 Should we in veterinary medicine follow the same path? If so, understanding how to better collaborate, cooperate, share information, and develop outcome measures will be necessary to assess how procedures and treatments impact care. A recent survey analyzing the use of fluid therapy among small animal practitioners indicated a lack of uniformity regarding rates of administration, route, and type of fluid therapy used for resuscitation and anesthesia.19 For example, the rate of intraoperative fluid administration during anesthesia is likely excessive, which could cause harm to patients.19 Guidelines on fluid therapy for specific conditions in veterinary patients are lacking, hence the importance of evaluating the effects of fluid therapy on outcomes and developing recommendations. Doing so likely will lead to improved standards of care and promote standardization of fluid therapy protocols in veterinary health care.
Outcomes are the result of care in terms of the patient's health over time.20 Advancing patient outcomes should be the ultimate goal for patient care, both in humans and animals.
Health care outcomes are a true measure of quality.20 In business, quality should always be measured from the customer's perception and not the supplier's point of view. Health care (and veterinary care) should not be any different, and outcomes should be centered on the patient (and owner) and not on the individual units or specialty services providing the care.20
Outcomes should be measured by medical condition (eg, diabetes, Cushing's syndrome, asthma) and not by specialty (eg, internal medicine, surgery) or intervention (eg, neurologic examination, echocardiography). Furthermore, outcome measurement ought to cover the full cycle of care for the condition, as well as follow‐up care.7 It is the overall results that matter, not the outcome of an individual intervention (too narrow), or a single visit or care episode (too short).20 For example, if a surgical procedure is performed flawlessly, but the animal develops a surgical site infection, then the outcome would be negatively affected and the costs of care would increase. Some examples of outcomes in health care include QOL improvement post‐surgery or decreasing disease prevalence because of implementation of preventative measures.6 Other outcome measures are discomfort, timelines, and complications of care.20 Even though primary care and preventive care are not the main targets of this article, outcomes in these settings should be measured for a defined patient population with similar health circumstances. An illustration for veterinary care could be healthy adult dogs or horses with Cushing's disease.20
In value‐based care, outcomes that matter to patients for a particular medical condition fall into 3 categories7, 21:
- Health status achieved or retained. Patients (or their owners in veterinary medicine) care about survival but also about functional status. For example, the 5‐year survival rate in men with prostate cancer is 90%, so patients are more interested in their doctor's performance on crucial functional outcomes, such as incontinence. However, in the example of tibial plateau leveling osteotomy (TPLO) or hip replacement, it is:
-
○survival, mortality rate;
-
○degree of health or recovery, pain level achieved or extent of return to physical activity.
-
○
- Process of recovery. Outcomes relate to the nature of the care and recovery. The level of discomfort during care and how long it takes to return to normal activity matter greatly to patients. In the example of TPLO or hip replacement, it is:
-
○time to recovery, or to return to physical activity;
-
○disutility of care or the treatment process (eg, diagnostic errors, ineffective care, complications, adverse events), pain during treatment, duration of hospital stay or infection.
-
○
- Outcomes related to sustainability of health. For example, a hip replacement that lasts 2 years is inferior to 1 that lasts 15 years, which is true from the patient's and the doctor's perspective. Sustainable health outcomes here would be:
-
○sustainability of health or recovery, maintenance of functional level, or the need for further implant replacement;
-
○long‐term consequences of treatment (ie, care‐induced illnesses), possible loss of mobility because of inadequate rehabilitation, or susceptibility to infection.
-
○
4. LEARNING TOOL
Outcomes are a powerful force to improve transparency and the satisfaction of doctors, not just patients (and owners). Measuring and reporting outcomes is crucial for learning and improving care over time. By comparing their performance with peers inside and outside their organization, the care team can advance and thus positively impact outcomes. Furthermore, outcome improvement is a powerful driver for lowering costs and hence improving value.7 Cleveland Clinic, a pioneer on VBHC, publishes several different “outcome books” such as that of their Respiratory Institute.22
A recent study in dogs outlined an aseptic TPLO protocol that led to a significant decrease in post‐TPLO infection rate and implant removal.23 From the value‐based point of view, the lower incidence of complications improved the value (better outcomes and lower costs) provided to dogs that benefited from the aseptic protocol. These dogs would likely return to normal activity more quickly and have a better QOL. This type of learning protocol, if implemented by surgeons, could enhance the value provided to their patients undergoing TPLO surgery (Figure 1).
Figure 1.
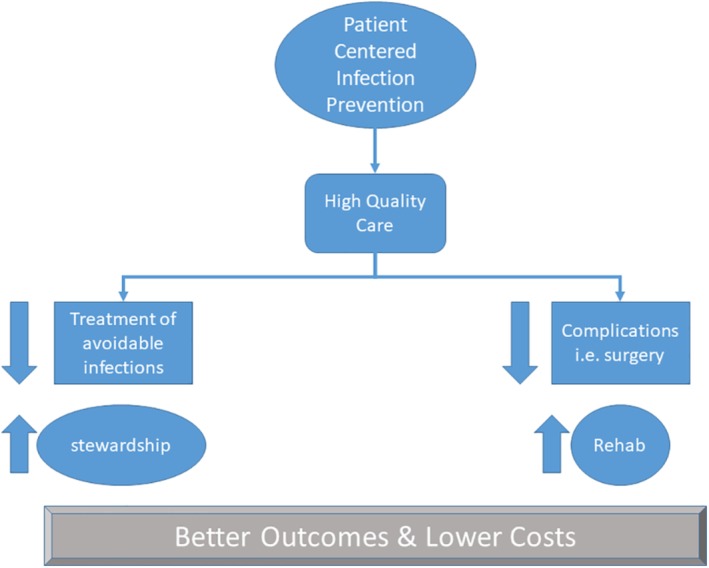
This figure highlights the importance of patient‐centered infection prevention in increasing the quality of care. In the tibial plateau leveling osteotomy example, the improved asepsis protocol will lead to less infections hence improve antibiotic stewardship. Furthermore, the lower complications (surgical site infections) post‐surgery will lead to faster rehabilitation and recovery, overall leading to improved outcomes (improved quality of life) and decrease costs. This is the basis at enhancing the value provided to our patients and clients through the value‐based veterinary care framework
5. CHALLENGES
Measuring outcomes that matter to patients (or their owners) is not an easy task, and progress has been slow. Aside from survival, outcome measurement remains limited.24 Two main challenges for outcome measurement are organizational structure and information technology systems. The tendency is to measure only what the care team directly controls in a particular intervention, what can be measured easily, or the intervention and treatment that can be billed. Furthermore, rather than determining outcomes for the full care cycle over which value is determined, outcomes are assessed for department or billing units. In health care, outcome work often is driven by medical specialty experts or consensus panels, and not multidisciplinary groups for medical conditions. Organizational structure could explain why doctors fail to accept responsibility for outcomes, defending this position by citing their lack of control over “outside” players involved with patient care (even if they belong to the same hospital) or patient compliance.20 An additional barrier is the cost implied in obtaining longitudinal patient data because of organizational fragmentation. Lack of an electronic medical record system that could effortlessly capture outcome data and compile it remains a challenge for many health care systems.20 Many of these hurdles in outcome data measurement can be easily extrapolated to veterinary medical care, and thus we have a great opportunity for learning about and improving the way care is provided to our patients.
It is paramount for all stakeholders involved in patient care to come together in creating a process for agreeing on a minimum sufficient set of outcomes for each medically important clinical condition and to standardize those measurements nationally and internationally. Once that happens, the care team will be able to collect and share data on outcomes in an efficient manner, which in turn will allow comparisons, ultimately improving care.24 An approach to outcome measurement would be bringing together experts on specific conditions and other parties involved with patient care to develop minimum standard outcome sets and risk factors in an organized structured process.24 The key to using VBHC to drive improvement is to measure a minimum sufficient set of outcomes for every major clinical condition, with well‐defined methods for their collection and risk adjustment, and then standardize those at the national and global level.24 An example is the creation of The International Consortium for Health Outcomes Measurements (ICHOM). The standards created by ICHOM are helping doctors, patients, and information technology vendors to achieve a common ground with respect to what needs to be tracked, making implementation of outcome measurement easier and more efficient.24 The ICHOM has convened experts on specific clinical conditions and patient representatives to outline minimum standard outcomes sets and risk factors, using a structured process.25 Some examples of outcomes sets completed and under consideration by ICHOM are cataracts, stroke, knee osteoarthritis, lung cancer, breast cancer, heart failure, inflammatory bowel disease, and malaria.
Such a complex endeavor requires the cooperation of multiple players, and hence it will take time to occur. If, as veterinarians, we want to improve the value provided to our patients and their owners, as well as bettering ourselves, VBVC could be an interesting path towards improvement.
6. PATIENT‐REPORTED OUTCOME MEASURES AND OWNER‐REPORTED OUTCOME MEASURES
The aim of doctors (and veterinarians) is not only to save lives but also to improve the lives of patients.26 This means decreasing clinical signs such as pain, incontinence, or diarrhea or helping patients get up, lie down, and walk better after surgery.26, 27
Doctors' understanding of the effect of disease and treatment on patients' daily lives is poor.28 Thus, hundreds of standardized measures have been developed to capture patient‐reported outcomes.28 These patient‐reported outcome measures (PROMs) are measurements based on a report that comes directly from the patient about the status of particular aspects of or events related to a patient's clinical condition.29 Two important characteristics of PROMs are: (i) they are clinically meaningful with practical implications for disease recognition and management and (ii) they include reporting of outcomes based on a patient's unique perspective (eg, patient‐reported pain scale).29 The PROMs are powerful assessment tools because by using validated questionnaires, clinical signs could be turned into numerical scores that would describe, for example, how much a knee replacement helps a person walk or to quantify the average difference in outcome between a biologic treatment and traditional pharmacotherapy.26, 27 Patient‐reported outcome measures are essential for real‐time clinical care and for how doctors measure, compare, and improve care as a system.26 Making PROMs an integral part of clinical practice leads to better communication and decision‐making between doctors and patients, improving patient satisfaction and allowing doctors to provide better care at the individual patient's level as well as in aggregate for the population.26, 28, 30 The information gathered can bridge the gap between the clinical reality and the patient's world, triggering learning as well as the correct next action.28
Observer‐reported outcomes are assessments determined by observers who do not have professional training relevant to the measurement being made (eg, teacher, caregiver), and they are used when the patient is unable to self‐report (eg, infants, young children). They should only be used for reporting observable concepts (eg, signs, behaviors) and cannot be validly utilized to assess signs (pain) or other unobservable factors.29 Similar to human pediatric medicine, veterinary patients are unable to self‐report, hence the need for developing observer (owner)‐reported outcomes. In veterinary clinical oncology, treatment outcomes mostly are defined by veterinarian‐measured response variables (eg, tumor size, stage), which are quantifiable measures. However, these measures are not outcomes that are necessarily perceived as important by pet owners.27 A recent study explored the development of OROMs designed to standardize QOL measures in dogs with cancer that could be used as outcome measures in clinical trials.27 This study found that veterinarians and pet owners perceived elements of QOL in different ways, so it is important to develop OROMs to measure outcomes in veterinary medicine to more fully assess the effects that treatment has on patients. It is crucial when developing owner‐reported QOL measurement tools to include pet owners as content experts.27
Patient‐reported outcome measures and OROMs are crucial because they capture QOL issues that are central to why most patients (and pet owners) seek care (eg, to address bothersome clinical signs, limited function, or trouble going for a walk).26, 27 In health care, health‐related QOL assesses the impact of disease and treatment on the lives of patients, and it is defined as the capacity to perform the usual daily activities for a person's age and major social role.29 For example, for human patients undergoing prostate cancer treatment, there is a PROM specifically designed for this condition to measure signs such as incontinence, in addition to survival.26 Pet owners are primarily concerned with maintaining good QOL for their pets and will choose humane euthanasia for a suffering animal, independent of test results.27 Thus, owner‐perceived QOL must be considered an important disease end point in veterinary clinical oncology research, because it likely has an impact on treatment and survival.27 It is important for researchers and users of this type of data to understand the scoring system being used, the expected distribution and to be able to recognize and decrease sources of bias. For example, in human medicine, surrogates reporting pain are likely to report less pain than the affected individuals themselves.29
Despite challenges, the use of PROMs is viewed as an integral part of the future of health care. Technology, if not properly implemented, will be a barrier, and thus strong information technology support is critical.26, 31 Patients (owners), staff, and doctors are busy and must work as a team to make PROMs and OROMs a reality, and engagement will lead to success.26, 31 Also important is to strategically use PROMs and OROMs to achieve net time savings by making other activities faster, such as collecting pre‐visit information to minimize administrative burden or making care faster and better by incorporating responses in real time into an electronic medical record.26 Questionnaires should be easy and simple to complete, so there should not be too many questions and they should be made relevant by putting responses in context with graphical information, decision support, and shared decision‐making tools.26, 29
Despite the fact that many different PROMs exist in health care, there is still a lack of consensus regarding which 1 would be better suited for many conditions. Groups such as ICHOM have made strides encouraging agreement around a single set of measures for a particular clinical condition.26, 31 In veterinary medicine, the use of OROMs is still in its infancy, and more research is needed in developing OROMs for different clinical conditions. Proper development and deployment of these measures in veterinary clinical practice would advance our understanding and reporting of outcomes, a key aspect of VBVC.
7. INTEGRATED PRACTICE UNITS
A crucial aspect of VBHC is to organize the health care team around the patient's medical condition, departing from the traditional way of organizing by specialization or service department.7 An integrated practice unit (IPU) is a dedicated team composed of clinical and nonclinical staff that provides full care for the patient's primary and related conditions, as well as complications that could occur.7 The team is responsible for engaging patients and families in care.7
The complexity of health care delivery cannot be addressed by any individual or organization acting in isolation. Care is often poorly coordinated among clinicians within and across settings, and the increase in specialization further adds intricacy to the system because of the involvement of multiple doctors. When multiple doctors participate in the care of patients in a silo, accountability for patient care gets blurred. This leads to a fragmented system where coordination and communication among doctors and patients is difficult.12 A survey showed that 25% of tests had to be repeated because of a lack of sharing results between doctors and that 75% of hospital patients did not know which doctor was in charge of their care. This lack of continuity of care endangers patients (worsens outcomes) and increases waste (increases costs).12 To improve patient care, communication and cooperation among the members of the care team are essential.6, 12 Specialists in key disease areas must agree on the most important outcomes to measure. Doctors must work with patients to help achieve the outcomes most important to patients. Clinicians at different points in the treatment pathway must come together in interdisciplinary teams to create more integrated and customized interventions.6 Communicating among the care team as well as talking with patients can be an inexpensive and very effective way for delivering improved patient care.32 The role of doctors in talking with patients is key to motivate them to make earlier and better decisions about their treatment, leading to better outcomes and lower costs.32
The MD Anderson Head and Neck Cancer Center holds a weekly treatment‐planning conference to discuss new patients' treatment plans and reach a consensus. This approach implies an upfront cost (participating professionals' time), but this team consensus leads to better care because patients are treated correctly, thus eliminating unnecessary and ineffective care.32 This is just a single example highlighting the advantages of creating IPUs to revamp value care.
In veterinary medicine, there has been an increase in the number of referral and emergency centers staffed with board‐certified specialists; hence, animals increasingly are cared for by multiple veterinarians who often are located at more than 1 hospital.15, 16, 33 Despite the fact that veterinary specialization is beneficial for the patient, its owner, and the veterinary profession as a whole, this creates a challenge for veterinarians who need to work as a team in caring for patients.16 As in human medicine, the delivery of high‐quality veterinary care has become a multi‐tiered system, where the intermediary between the owner and specialist is the primary care practitioner who provides guidance, advice, support, and counsel for care.33, 34 The relationship among patient, owner, general practitioner, and specialist is complex, and, as in human medicine, failure to properly communicate and cooperate will have a negative impact on the care veterinarians provide to patients.15, 16
Humans with heart failure showed improved outcomes and quality of care when their treatment was delivered in a collaborative way between generalists and cardiologists.14 Dogs with congestive heart failure lived 74% longer when animals were treated collaboratively between the primary care veterinarian and the specialist cardiologist.34 These 2 studies showed that working as a health care team (ie, creating IPUs centered around the patient's clinical condition, heart failure in this case) leads to improved QOL, which is an important outcome measure.
8. DISCUSSION
Society's relationship with animals is changing, likely influencing the medical care that owners desire for their pets and contributing to the increase in veterinary patients for which care includes referral to a specialist.15 As veterinary care becomes more complex and costly, VBVC can be a way to provide high value care to patients and clients, while helping us understand the outcomes and costs involved with care.
In order for specialized care to lead to improved outcomes, a framework enhancing the referral process must exist, and VBVC can be that framework.15 A fundamental part of value care is the formation of IPUs, which will be key for improving cooperation and communication, fostering trust among the team members, and leading to better care for patients as well as improving the owners' satisfaction. Technology will play an important role at improving communication between specialists and generalists. For example, the newly launched rVetLink (IDEXX) aims at electronically sharing information between specialists and referring veterinarians thus enhancing the referral process. Technology will help but not replace the personal touch that is so important in creating rapport among care team members. VetSOAP is an organization focused on creating a culture of collaboration between specialists and referring veterinarians, with the aim of showing by research that this collaboration leads to improved value.
The client is a fundamental part in the VBVC framework and must be informed of the status of his or her animal's condition. Depending on the referral dynamics, either the primary care veterinarian or specialist would take the lead in ensuring that this communication proceeds flawlessly and that the owner is aware of the progress with the case. It is paramount for the complex process of referral to occur in an environment where mutual respect, trust, and collegiality among the care team members are practiced.15 Teaching and educating the veterinarians as well as veterinary students about concepts such as VBVC, IPUs, referral dynamics, and communication skills will be crucial to improving the way we practice veterinary medicine in the future.15
Measuring outcomes based on patients' medical conditions for the full cycle of care would mean a paradigm shift in veterinary medicine. Implementing OROMs will be an important advance in understanding the effects of different interventions on outcomes and QOL. Designing OROMs questionnaires that are simple and succinct and easy to complete by clients will be critical for implementation in clinical practice. When developing OROMs questionnaires, it is important to include owners of animals affected with the clinical conditions (eg, cancer) as content experts, as well as veterinary experts in the clinical condition, and to consult the existing literature.27 Pet owners and veterinarians perceive elements of QOL differently. Therefore, constructing and implementing OROMs in clinical practice and research settings will be fundamental in further understanding the effect that treatments have on outcomes and how to improve patient QOL. To advance outcome measures in veterinary health care, it would be useful for a multidisciplinary team of experts to identify 3 to 5 key clinical conditions in dogs, cats, and horses. Creating such a group would facilitate creating consensus on what measures to use for outcomes, rather than generating many different measures without consensus, as has occurred in human medicine.25
Information technology is a key component of value care, and it should be able to support integrated multidisciplinary care as well as enable outcome and costs measurements.7 Banfield Pet Hospital is the largest veterinary practice in the world, highlighting the consolidation occurring in veterinary health care.35 An advantage of this consolidation is that it breaks down information technology silos, allowing access to vast amounts of patient data. A recent report on the use of antimicrobials for treating urinary tract infections and respiratory infections in dogs at Banfield Hospital indicated what can be learned from the current use of these drugs in treating 2 clinical conditions and to improve antimicrobial use in order to provide better patient care.35 As technology continues to advance at a rapid pace, we have an opportunity to break down information technology silos, allowing veterinary medicine to carry out multicenter international studies to help understand the impact that treatment has on the outcomes and costs of certain clinical conditions.
As in human medicine, VBVC and VBHC are innovative concepts, and veterinarians will need to experiment with them, embracing the opportunity to change the way we provide care and be humble in acknowledging what we do not know.
CONFLICT OF INTEREST DECLARATION
The author is a member of the Advisory Council for Veterinary Specialists Outreach & Awareness Project (VetSoap).
OFF‐LABEL ANTIMICROBIAL DECLARATION
Author declare no off‐label use of antimicrobials.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC) OR OTHER APPROVAL DECLARATION
Author declare no IACUC or other approval was needed.
HUMAN ETHICS APPROVAL DECLARATION
Author declare human ethics approval was not needed for this study.
Pantaleon L. Why measuring outcomes is important in health care. J Vet Intern Med. 2019;33:356–362. 10.1111/jvim.15458
REFERENCES
- 1. Lengyel K. Veterinary consolidation reshaping the market, report says. Veterinarian's Money Digest . 2018. https://www.vmdtoday.com/news/veterinary‐consolidation‐reshaping‐the‐market‐report‐says. Accessed October 25, 2018.
- 2. Gawande A. Restaurant chains have managed to combine quality control, cost control, and innovation. Can health care? The New Yorker Annals of Health Care . 2012. https://www.newyorker.com/magazine/2012/08/13/big-med. Accessed October 25, 2018.
- 3. Einav I. Is American pet health care (also) uniquely inefficient? American Economic Review: Papers & Proceedings. 2017;107:491‐495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. DeAngelis L. Your doctor needs your trust. The Wall Street Journal . 2018. https://www.wsj.com/articles/your‐doctor‐needs‐your‐trust‐1540335833. Accessed October 25, 2018.
- 5. Transforming Medtronic to support progress in healthcare. Medtronic Further, Together . Medtronic, 2018. http://www.medtronic.com/us‐en/transforming‐healthcare/signup‐for‐updates/thank‐you.html. Accessed July 16, 2018.
- 6. Larsson S, Tollman P. Health Care's Value Problem and How to Fix It. Boston Consulting Group Henderson Institute; 2017:1‐44. https://www.bcg.com/en-us/publications/2017/smart-simplicity-health-care-value-problem-how-fix-it.aspx. Accessed October 25, 2018. [Google Scholar]
- 7. Porter M, Lee TH. The strategy that will fix health care. Harv Bus Rev. 2013;91:1‐19. [Google Scholar]
- 8. APPA . Pet Industry Market Size & Ownership Statistics. American Pet Products Association; 2018. https://www.americanpetproducts.org/press_industrytrends.asp. Accessed August 24, 2018. [Google Scholar]
- 9. Quedraogo F, Dicks M. Are rising veterinary salaries driving up the cost of care? DVM360 . 2018.
- 10. HABRI . The Science Behind The Human‐Animal Bond. Human Animal Bond Research Institute; 2017. https://www.habri.org/research/. Accessed January 11, 2018. [Google Scholar]
- 11. Sevransky JE, Nicholl B, Nicholl JB, Buchman TG. Patient‐ and family‐centered care: first steps on a long journey. Crit Care Med. 2017;45:757‐758. [DOI] [PubMed] [Google Scholar]
- 12. Smith M. Best Care at Lower Cost: The Path to Continuously Larning Health Care in America. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 13. Erstad BL. Value‐based medicine: dollars and sense. Crit Care Med. 2016;44:375‐380. [DOI] [PubMed] [Google Scholar]
- 14. Ahmed A, Allman RM, Kiefe CI, et al. Association of consultation between generalists and cardiologists with quality and outcomes of heart failure care. Am Heart J. 2003;145:1086‐1093. [DOI] [PubMed] [Google Scholar]
- 15. Best C, Coe JB, Hewson J, Meehan M, Kelton D, Black B. Referring equine veterinarians' expectations of equine veterinary specialists and referral centers. J Am Vet Med Assoc. 2018;253:479‐489. [DOI] [PubMed] [Google Scholar]
- 16. Block G, Ross J. The relationship between general practitioners and board‐certified specialists in veterinary medicine. J Am Vet Med Assoc. 2006;228:1188‐1191. [DOI] [PubMed] [Google Scholar]
- 17. Cutler D. Physician Beliefs and Patient Preferences: A New Look at Regional Variation in Health Care Spending. Cambridge, MA: National Bureau of Economic Research; 2018:1‐64. [Google Scholar]
- 18. Greenfield D. It takes two to tango: customization and standardization as colluding logics in healthcare. Int J Health Policy Manag. 2018;7:183‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hopper K, Garcia Rojas A, Barter L. An online survey of small animal veterinarians regarding current fluid therapy practices in dogs and cats. J Am Vet Med Assoc. 2018;252:553‐559. [DOI] [PubMed] [Google Scholar]
- 20. Porter M. Measuring health outcomes: the outcome hierarchy (Supplementary Appendix 2 to what is value in health care?). N Engl J Med. 2010;363:1‐18.20573919 [Google Scholar]
- 21. Porter ME. What is value in health care? N Engl J Med. 2010;363:2477‐2481. [DOI] [PubMed] [Google Scholar]
- 22. Hatipoglu U. Respiratory institute outcomes Outcomes 2013 10th ed. Cleveland, OH: The Cleveland Clinic Foundation; 2013;1–39. [Google Scholar]
- 23. Stine SL, Odum SM, Mertens WD. Protocol changes to reduce implant‐associated infection rate after tibial plateau leveling osteotomy: 703 dogs, 811 TPLO (2006‐2014). Vet Surg. 2018;47:481‐489. [DOI] [PubMed] [Google Scholar]
- 24. Porter ME, Larsson S, Lee TH. Standardizing patient outcomes measurement. N Engl J Med. 2016;374:504‐506. [DOI] [PubMed] [Google Scholar]
- 25. Porter ME, Larsson S. Standardizing Patient Outcomes Measurement. NEJM Catalyst: NEJM; 2016. https://catalyst.nejm.org/standardizing-patient-outcomes-measurement/. Accessed June 10, 2018. [DOI] [PubMed] [Google Scholar]
- 26. Wagle N. Implementing Patient‐Reported Outcome Measures. NEJM Catalyst: NEJM; 2017. Accessed June 7, 2018. [Google Scholar]
- 27. Giuffrida MA, Brown DC, Ellenberg SS, Farrar JT. Development and psychometric testing of the Canine Owner‐Reported Quality of Life questionnaire, an instrument designed to measure quality of life in dogs with cancer. J Am Vet Med Assoc. 2018;252:1073‐1083. [DOI] [PubMed] [Google Scholar]
- 28. Nelson EC, Eftimovska E, Lind C, Hager A, Wasson JH, Lindblad S. Patient reported outcome measures in practice. BMJ. 2015;350:g7818. [DOI] [PubMed] [Google Scholar]
- 29. Velentgas P, Dreyer N, Wu A. Developing a Protocol for Observattional Comparative Effectiveness Research. Rockville, MD: Agency for Healthcare Research and Quality; 2013:75‐92. [PubMed] [Google Scholar]
- 30. Foster A, Croot L, Brazier J, Harris J, O'Cathain A. The facilitators and barriers to implementing patient reported outcome measures in organisations delivering health related services: a systematic review of reviews. J Patient Rep Outcomes. 2018;2:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ackerman IN, Cavka B, Lippa J, et al. The feasibility of implementing the ICHOM Standard Set for Hip and Knee Osteoarthritis: a mixed‐methods evaluation in public and private hospital settings. J Patient Rep Outcomes. 2017;2:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kaplan RS, Haas DA, Warsh J. Adding value by talking more. N Engl J Med. 2016;375:1918‐1920. [DOI] [PubMed] [Google Scholar]
- 33. Stoewen DL, Coe JB, MacMartin C, Stone EA, Dewey CE. Factors influencing veterinarian referral to oncology specialists for treatment of dogs with lymphoma and osteosarcoma in Ontario, Canada. J Am Vet Med Assoc. 2013;243:1415‐1425. [DOI] [PubMed] [Google Scholar]
- 34. Lefbom BK, Peckens NK. Impact of collaborative care on survival time for dogs with congestive heart failure and revenue for attending primary care veterinarians. J Am Vet Med Assoc. 2016;249:72‐76. [DOI] [PubMed] [Google Scholar]
- 35. Are we doing our part to prevent superbugs? Antimicrobial usage patterns among companion animal veterinarians. Veterinary Emerging Topics Report 2017:1–13. https://www.banfield.com/getmedia/e6c50f42‐9ded‐4323‐aa03‐4fd92a2aa012/VET‐Report_Final_web.pdf.


