Abstract
Purpose:
We developed BMT Roadmap, a health information technology (HIT) application on a tablet, to address caregivers’ unmet needs with patient-specific information from the electronic health record. We conducted a preliminary feasibility study of BMT Roadmap in caregivers of adult and pediatric HSCT patients. The study was registered on ClinicalTrials.gov (NCT03161665; NCT02409121).
Methods:
BMT Roadmap was delivered to 39 caregivers of adult and pediatric patients undergoing first-time HSCT at a single study site. We assessed person reported outcome measures (PROMs) at baseline (hospital admission), discharge, and day 100: usefulness of BMT Roadmap (Perceived Usefulness); activation (Patient Activation Measure, caregiver version [PAM-C]); mental health ([POMS]-2®: depression, distress, vigor, and fatigue); anxiety (State-Trait Anxiety Inventory); and quality-of-life (Caregiver Quality-of-Life Index-Cancer [CQOLC]). To identify determinants of caregiver activation and quality-of-life, we used linear mixed models.
Results:
BMT Roadmap was perceived useful and activation increased from baseline to discharge (p=0.001). Further, burden decreased through discharge (p=0.007). Overall, a pattern of increasing vigor and decreasing depression, distress, fatigue, and anxiety was apparent from baseline to discharge. However, overall quality-of-life lowered at discharge after accounting for Roadmap use, depression, anxiety, and fatigue (p=0.04).
Conclusions:
BMT Roadmap was a feasible HIT intervention to implement in HSCT caregivers. BMT Roadmap was associated with increased activation and decreased burden, but quality-of-life lowered across hospitalization. Findings support the need to further develop caregiver-specific self-directed resources and provide them both inpatient and outpatient across the HSCT trajectory.
Keywords: Information technology, bone marrow transplantation, caregivers, mental health
INTRODUCTION
Hematopoietic stem cell transplantation (HSCT) is a high-risk, but potentially curative therapy for a number of malignant and non-malignant conditions [1]. Given the risks associated with HSCT, patients require a dedicated, full-time caregiver. As a result, HSCT caregivers commonly experience significant anxiety and distress during the peri-transplant period [2,3], which can be associated with significant decline in emotional, physical, and social functioning [4]. Furthermore, the reciprocal relationship between emotional distress in patients and caregivers [5] strongly supports the need to promote caregiver activation, health, and well-being. With the growing population of HSCT patients and survivors coupled with increased demands of caregivers to provide intense and episodic care, there is an urgent public health need to improve both patient and caregiver outcomes [6]. Self-directed supportive care interventions have been recommended to address this need [6], but little has been studied in the HSCT population. Thus, examining the potential use of scalable, user-centered technology is warranted.
Health information technology (HIT) has opened up exciting opportunities for capturing, delivering, and sharing data by secure electronic means and provides a scalable and flexible platform to promote and support quality healthcare [7,8]. HIT has the potential to support caregivers of patients with complex healthcare needs, such as the HSCT population, particularly as more care is being performed outpatient. Indeed, over two-thirds of caregivers report wanting mobile technologies to support their caregiving efforts [9]. Major recommendations to move the science of cancer caregiving forward include, “generating and testing strategies for integrating caregivers into formal healthcare settings” and “promoting the use of technology to support cancer caregivers” [6].
Thus, we developed a web-based HIT application, BMT Roadmap, supported by user-centered approaches [10] to integrate patient-specific health information in real-time from the electronic health record (EHR; Epic®) for both patients and caregivers to use throughout the hospitalization. Key stakeholders (patients, caregivers, and healthcare providers) participated in the design and development of BMT Roadmap [10,11]. We have previously reported on the initial feasibility of BMT Roadmap for patients in the inpatient setting [12]. Herein, we report the findings of a preliminary feasibility study among caregivers of HSCT patients using BMT Roadmap, assessing activation, mental health person reported outcome measures (PROMs), and quality-of-life.
METHODS
Study Design and Setting
This study assessed the preliminary feasibility of the BMT Roadmap intervention in caregivers of adult patients (“adult caregivers”) or pediatric patients (“pediatric caregivers”) undergoing HSCT, with an a priori target enrollment of 20 participants in each caregiver group. The protocol was approved by Michigan Medicine’s Institutional Review Board (HUM00107014-adult caregiver study, HUM00100126-pediatric caregiver study) and registered on ClinicalTrials.gov (NCT03161665–adult caregiver study, NCT02409121–pediatric caregiver study). All participants provided written informed consent; all patients agreed for caregivers to participate. The adult caregiver study was conducted 01/2016–06/2016 and the pediatric caregiver study was conducted 09/2015–02/2017.
Inclusion Criteria
Eligible participants were caregivers who identified themselves as the primary caregiver of a patient undergoing their first HSCT, willing to adhere to the study procedures, proficient in English, and able to provide informed consent. Caregivers were recruited pre-HSCT by a nurse coordinator and/or HSCT physician. After obtaining informed consent, a research coordinator provided a tutorial of BMT Roadmap.
Intervention
BMT Roadmap was designed on an Apple® iPad and integrated with the MiChart (Epic®; Verona, WI) EHR to visualize real-time: laboratory results and medications; clinical-trial enrollment; healthcare provider directory; and discharge checklist (see Supplemental Table [ST]1). Each participant was given their own Apple® iPad and was instructed to use BMT Roadmap freely throughout the patients’ hospitalization. The endpoint of the study was day 100 post-HSCT (D100).
Person Reported Outcome Measures (PROMs)
PROMs were administered on an Apple® iPad using Qualtrics, a secure online HIPAA-compliant platform for administering surveys (www.Qualtrics.com). Usefulness (Perceived Usefulness) [18] was measured at discharge only. All other PROMs were assessed at three time-points: baseline (hospital admission), discharge, and D100. Well-validated measures included Activation (Patient Activation Measure-Caregiver Version [PAM-C]) [13,14], Quality of Life (Caregiver Quality-of-Life Index-Cancer [CQOLC]) [15]. Anxiety (State–Trait Anxiety Inventory; STAI–S) [16], Global Distress (Profile of Mood States-2® [POMS–2®–Total])[17], Depression (POMS–2®–Depression) [17], Vigor (POMS–2®–Vigor)[17], Fatigue (POMS–2®–Fatigue) [17]. See Table 1 for detailed psychometric properties of the measures.
Table 1.
Person Reported Outcome Measures (PROMs)
| PRO | DESCRIPTION | SCORING | PSYCHOMETRICS | HIGH SCORES | |
|---|---|---|---|---|---|
| Usefulness | Perceived Usefulness (PU)1 | 6-item scale assessing “the degree to which a person believes a particular system would enhance their job performance” | 7-point Likert scale ranging from 1=extremely likely to 7= extremely unlikely. Total score is created by summing the item scores. Total range = 6 – 42. | Cronbach’s α = 0.92 – 0.98; good convergent validity (r = .63 - .85).1 | Less desirable, reflecting less perceived usefulness |
| Activation | Patient Activation Measure (PAM-C)2,3 Caregiver version |
13-item measure that assesses the caregiver’s skills, knowledge, and confidence for patient-management. | 4-point Likert scale ranging from 1=disagree strongly to 4=agree strongly. All responses are summed and scaled from 0–100, which are then converted to an “activation score” using a scale provided by the developers of the PAM. | Cronbach’s α = 0.86; construct and content validity supported in a population of parents undergoing BMT.2,3 | More desirable, reflecting greater activation. |
| Quality of Life | Caregiver Quality of Life Scale –Cancer (CQOL-C)4 | 35-item rating scale. Total score represents Caregiver Quality of Life. Four subscales: Burden, Disruptiveness, Positive Adaptation, Financial Concerns. | 5-point Likert scale ranging from 0= not at all to 4=very much. Total score is created by summing all responses after reverse-scoring the items of the Positive Adaptation subscale. Total score range = 0–140. | Cronbach’s α = 0.90 for Total; α = .73 - .89 for subscales. Test-retest reliability (r = .94 for Total; r = .82 - .91 for subscales). Convergent validity r = .69 with Mental Component Summary Score of MOS-SF-36. | Less desirable, reflecting lower quality of life and higher caregiver strain/onus/hardship |
| Anxiety | State Trait Anxiety Inventory (STAI)5 | 20-item subscale of STAI assessing State Anxiety (transitory state of tension, nervousness or worry within a specific situation or context). | 4-point Likert scale ranging from 1=not at all, to 4=very much so. Z scores (mean = 0; SD=1) used in these analyses. | Cronbach’s α = .86 - .95; Test-retest reliability = 0.31 – 0.86. Good convergent validity with other measures of anxiety and divergent validity from non-anxiety measures.5 | Less desirable, reflecting more anxiety |
| Distress | Profile of Mood states-2 (POMS-2®) -Total6 | 65-item measure indicative of global distress or “Total Mood Disturbance” and 6 subscale scores: Fatigue, Vigor, Tension-Anxiety, Depression, Anger-Hostility, and Confusion. | 5-point Likert scale ranging from 0= not at all to 4=extremely with which respondents rate how descriptive the adjective in each item is of them in the past week. Global Distress (Total Mood Disturbance score) is the sum of all subscales minus Vigor score, converted to a T score (mean = 50; SD=10). | Cronbach’s α = 63 - .96. Test-retest reliability = .61-.69. Good concurrent validity. Factor structure confirmed by multiple studies.6 | Less desirable, reflecting more HCT-related distress |
| Depression | Profile of Mood States (POMS-2®) – Depression subscale6 | 15-item measure indicative of Depressed Mood. Respondents rate the degree to which the adjective in each item is descriptive of their mood in the past week. | 5-point Likert scale ranging from 0= not at all to 4=extremely. Depression is expressed as T score (mean = 50; SD=10). | Cronbach’s α = .95; good convergent validity with other measures of depressed mood.6 | Less desirable, indicating more depressed mood |
| Vigor | Profile of Mood States (POMS-2®) – Vigor subscale6 | 9-item measure indicative of vigor, high energy, positive affect. Respondents rate the degree to which the adjective in each item is descriptive of their vigor in the past week | 5-point Likert scale ranging from 0= not at all to 4=extremely. Vigor is expressed as T score (mean = 50; SD=10). | Cronbach’s α = .87; good convergent validity in the expected direction with other measures of mood disorders.6 | More desirable, reflecting greater vigor |
| Fatigue | Profile of Mood States (POMS-2®) – Fatigue subscale6 | 6-item measure indicative of Fatigue. Respondents rate the degree to which the adjective in each item is descriptive of their fatigue in the past week | 5-point Likert scale ranging from 0= not at all to 4=extremely. Fatigue is expressed as T score (mean = 50; SD=10). | Cronbach’s α = .91; good convergent validity with other measures of mood disorders.6 | Less desirable, indicating more fatigue |
Davis F. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13(3):319–340.
Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40:1918–1930.
Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–1026.
Weitzner MA, Jacobsen PB, Wagner H, Jr., Friedland J, Cox C. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 1999;8:55–63.
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. 1983.
McNair DM, Loor M, Droppelman LF. Profile of mood states. San Diego, CA: Educational and Industrial Testing Service. 1981.
Statistical Analyses
Statistical analyses were conducted using Statistical Package for Social Sciences (SPSS; version 24) and Stata software pack (Stata Corporation, College Station, TX). Demographic and clinical characteristics were described using means, standard deviations, ranges, frequencies, and percentages, as appropriate. Descriptive statistics were calculated for device utilization. ‘Average daily BMT Roadmap use’ was defined as the ratio of total minutes used to days of access. Similarly, ‘average daily individual module use’ was defined as the ratio of minutes the module was used to days of access. Pearson’s correlation was used to determine the degree and significance of association among demographics, medical variables, and PROMs. For all tests, α=0.05.
To investigate determinants of caregiver activation or quality-of-life across the three time-points, we fitted a series of linear mixed models [19]. As mixed model regression does not require a balanced design, individuals who are unobserved at some time points can still contribute at the time points for which they are observed. We included a random effect per participant, which accounted for within subject correlation across time that violated the independence assumption of ordinary least squares. To investigate what variables influenced activation, we fitted a model in which caregivers were specified as a random effect, care group (adult vs. pediatric caregivers) and time-point as factors, and vigor, perceived usefulness, and the interaction of care group and perceived usefulness as covariates. To investigate what variables influenced caregiver quality-of-life, we fitted a model in which caregivers were specified as a random factor, care group and time-point as factors, and depression, anxiety, fatigue, and BMT Roadmap use as covariates. In both models, covariates were included based on conceptual relevance and univariate correlations (threshold p≤0.05).
RESULTS
Demographics
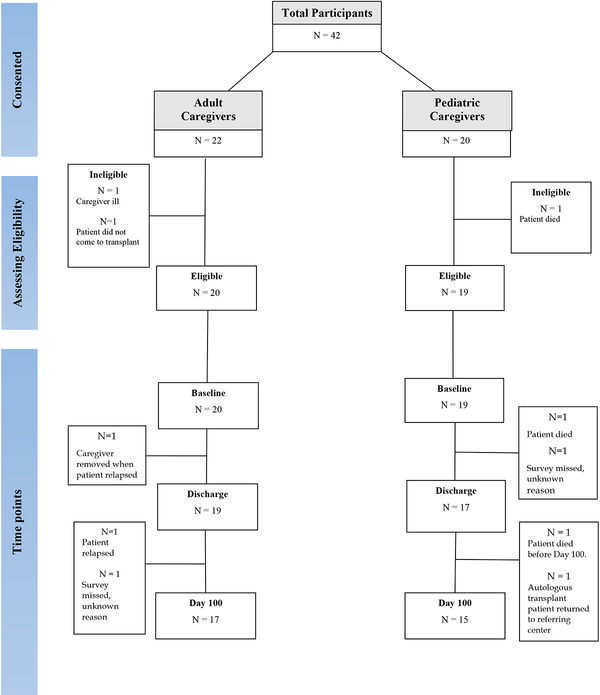
Forty-two consecutive adult and pediatric caregivers were recruited and signed informed consent. All caregivers approached, consented to participate in the study. Only one adult caregiver withdrew due to personal illness; two patients did not come to transplant (Figure 1). Of the remaining 39 individuals, 32 were observed at all three time-points, four were observed at the first two time-points only, and three were observed at baseline only. The final sample of 20 adult and 19 pediatric caregivers were predominantly female (p=0.05) and white/Caucasian (p=0.05), with a mean age of 47 years (range 24–69, Table 2). Adult caregivers were older than pediatric caregivers (p=0.001). Whereas 80% of adult caregivers were spouses, 95% of pediatric caregivers were parents. Both caregiver groups had on average at least a college education, but adult caregivers had more years of education than pediatric caregivers (p=0.007).
Figure 1.
Adult and Pediatric Caregiver Consort Diagram
Table 2.
Caregiver Demographics
| Overall Sample | Adult Caregivers | Pediatric Caregivers | ||||
|---|---|---|---|---|---|---|
| M(SD) | Range | M(SD) | Range | M(SD) | Range | |
| 47.3(14.6) | 24–69 | 57.7(36.4) | 32–69 | 36.4(9.4) | 24–57 | |
| Education (years)‡ | 14.3(2.4) | 8–18 | 15.3(1.9) | 12–18 | 13.2(2.5) | 8–18 |
| n | (%) | n | (%) | n | (%) | |
| Gender§ | ||||||
| Male | 8 | (20.5) | 6 | (30.0) | 2 | (10.5) |
| Female | 31 | (79.5) | 14 | (70.0) | 17 | (89.5) |
| Race¶ | ||||||
| White | 35 | (90.0) | 20 | (100.0) | 15 | (78.9) |
| Black/African American | 2 | (5.1) | 0 | (0.0) | 2 | (10.5) |
| Asian | 1 | (2.6) | 0 | (0.0) | 1 | (5.3) |
| Missing | 1 | (2.6) | 0 | (0.0) | 1 | (5.3) |
| Ethnicity | ||||||
| Hispanic | 3 | (7.7) | 2 | (10.0) | 1 | (5.3) |
| Relationship to the patient | ||||||
| Spouse | 16 | (41.0) | 16 | (80.0) | 0 | (0.0) |
| Parent | 21 | (53.8) | 3 | (15.0) | 18 | (94.7) |
| Grandmother | 1 | (2.6) | 0 | (0.0) | 1 | (5.3) |
| Sister | 1 | (2.6) | 1 | (5.0) | 0 | (0.0) |
Age: Adult caregivers were older than pediatric caregivers (t=6.10, p=0.001)
Education: 8 = 8th grade, 12 = high school, 14 = associate’s degree, 16 = bachelor’s degree, 18 = master’s degree. Adult caregivers were more educated than pediatric caregivers (t=2.89; p=0.007)
Gender: The overall sample was comprised of more females than males (Chi2=6.05; p<0.05)
Race: The overall sample was comprised of more whites than other ethnicities: (Chi2=5.06; p<0.05)
SD=Standard Deviation
The indication for transplant was predominantly hematological malignancy (ST2). All adult patients underwent allogeneic HSCT, whereas pediatric patients underwent allogeneic or autologous HSCT. Both allogeneic or autologous pediatric patients were recruited to maximize the available sample. For adults and pediatric patients undergoing allogeneic HSCT, the mean HSCT comorbidity index [20] score was significantly higher for adult patients compared with pediatric patients (p=0.001; ST2). The length-of-stay varied widely (range 18–112 days) with adult patients having shorter mean stay than pediatric patients (p=0.04; Table 3). Consequently, adult caregivers had less access to BMT Roadmap than pediatric caregivers (p=0.03, Table 3). However, after accounting for length-of-stay and duration of access to BMT Roadmap, the average daily use did not differ significantly between caregiver groups. Participants spent the majority of time viewing the laboratory module, followed by medications, and phases-of-care (Table 3). However, adult caregivers spent significantly more time viewing medications and phases-of-care modules compared with pediatric caregivers (p=0.02 and p=0.02, respectively; Table 3). Age and education did not correlate with BMT Roadmap use. However, more educated caregivers were more likely to use the laboratory module (p=0.005; ST3).
Table 3.
Utilization
| Overall Sample | Adult Caregivers | Pediatric Caregivers | |||||||
|---|---|---|---|---|---|---|---|---|---|
| M(SD) | Range | Use/Access† | M(SD) | Range | Use/Access† | M(SD) | Range | Use/Access† | |
| Length-of-Stay† | 31.3(21.2) | 18–112 | 24.5(8.5) | 18–58 | (38.5)27.5 | 18–112* | |||
| General Usage | |||||||||
| Access to iPad† | 29.0(22.0) | 12–112 | 21.5(9.7) | 12–58 | 36.8(28.1) | 18–112 | |||
| Total Time‡ | 90.1(67.4) | 4.0–320.0 | 3.4(2.3) | 92.4(72.7) | 8.9–320.0 | 3.8(2.3) | 87.6(63.4) | 3.97–253.0 | 3.0(2.2) |
| Log-in† | 14.5(13.0) | 1.00–54.0 | 4.4(.9) | 10.9(10.7) | 1.0–49.0 | 0.8(0.3) | 18.3(14.4) | 2.0–54.0 | 1.1(0.9) |
| Module Usageठ| |||||||||
| Laboratory Results | 29.3(34.4) | 0–172.9 | 1.0(0.9) | 18.0(14.8) | 0–49.3 | 0.9(0.8) | 41.2(44.4) | 0.3–172.9 | 1.2(1.1) |
| Medications | 12.9(13.6) | 0–62.0 | 0.5(0.5) | 14.1(13.3) | 0–56.1 | 0.7(0.6) | 11.7(14.2) | 0.6–62.0 | 0.3(0.2)** |
| Phases of Care | 12.9(10.0) | 0–43.0 | 0.5(0.5) | 15.1(11.9) | 0–43.0 | 0.7(0.6) | 10.5(7.0) | 0–24.3 | 0.4(0.3)** |
p=0.04;
p=0.02
days;
minutes;
Total module usage does not equal total time due to other modules not represented in the table (e.g., healthcare provider directory, discharge criteria checklist, patient disease characteristics)
SD=Standard Deviation
Person Reported Outcome Measures (PROMs)
Mental Health.
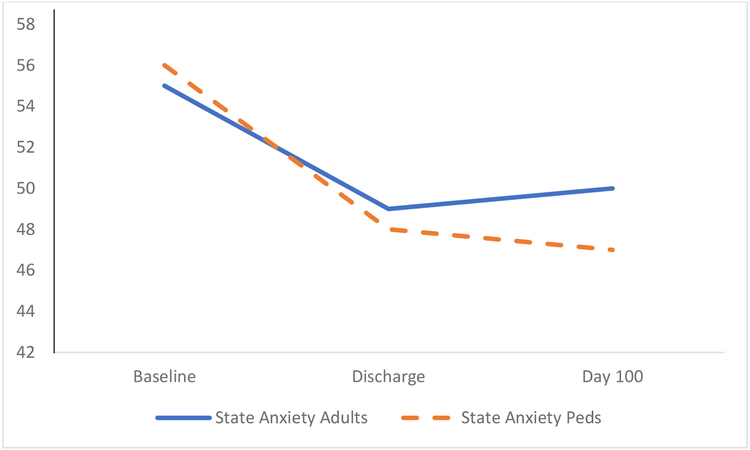
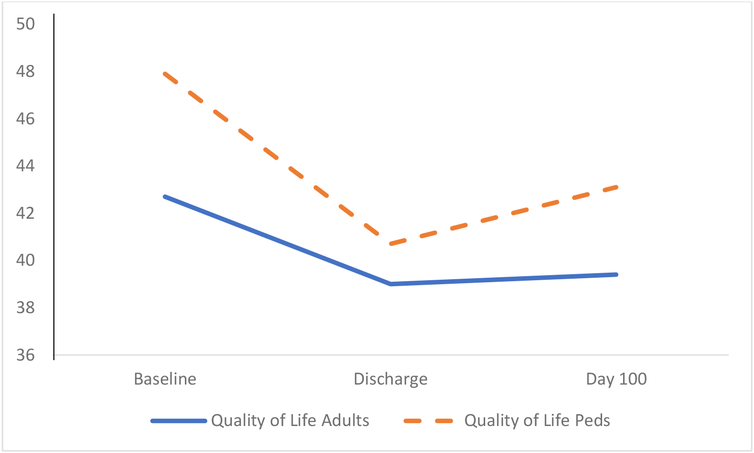
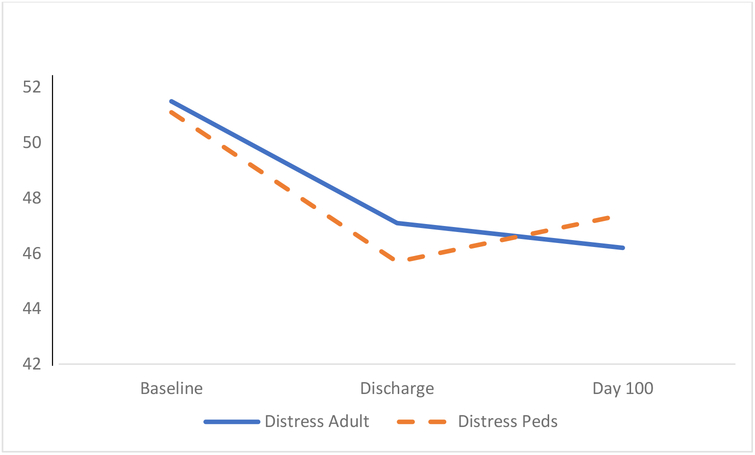
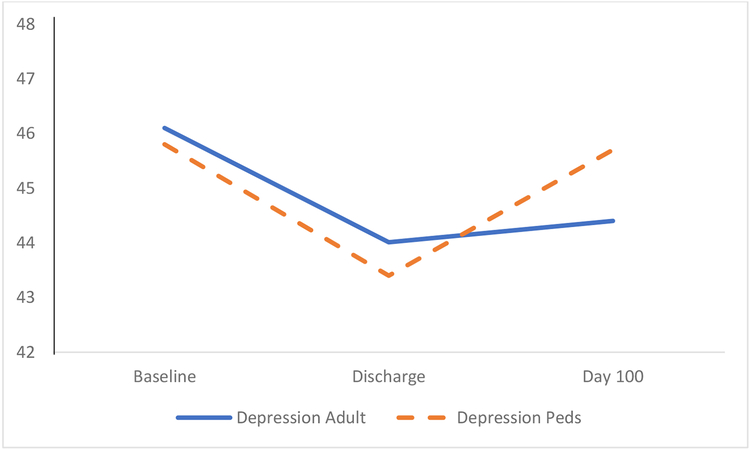
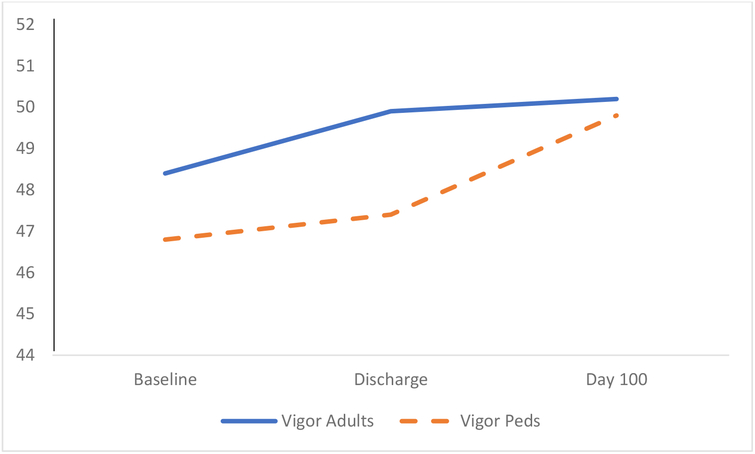
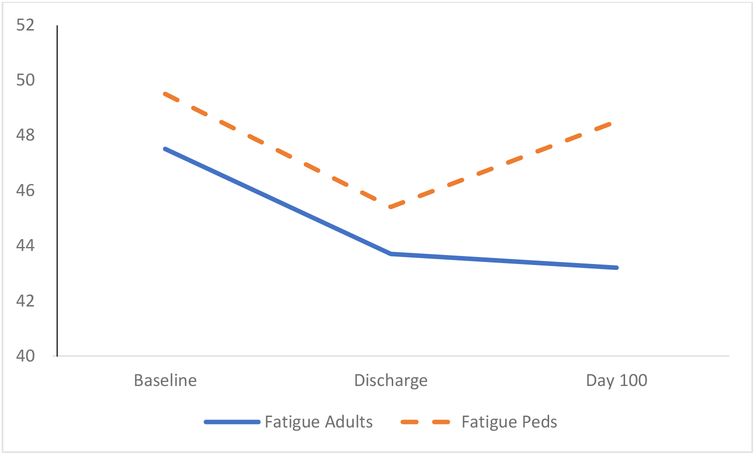
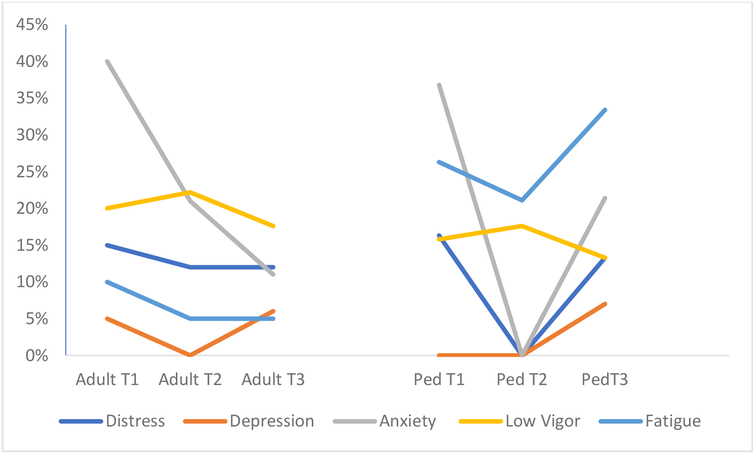
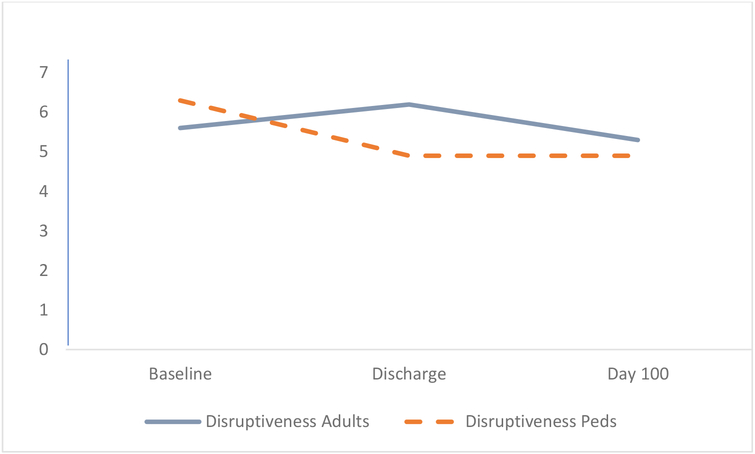
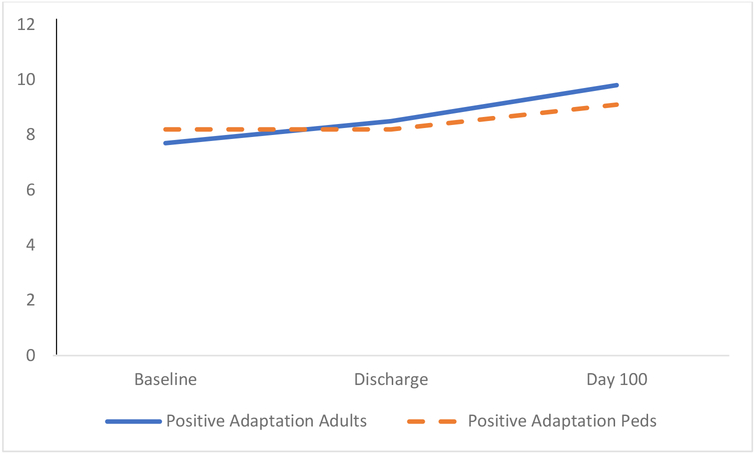
The PROMs response rate at baseline, discharge, and D100 was 100%, 92%, and 82%, respectively (Figure 1). The study sample’s mental health and quality-of-life PROMs (Figure 2A–2L; ST4) were correlated (ST5–ST7). Overall, a pattern of increasing vigor and decreasing anxiety, distress, depression, and fatigue was apparent from baseline to discharge, and caregiver groups did not differ across time. Furthermore, age and education did not correlate with any mental health PROM. Prevalence rates of clinically relevant distress (i.e., PROM exceeded one standard deviation from the standardized mean in the problematic direction) revealed similar prevalence of clinically relevant depression, distress, and low vigor in both caregiver groups, as well as steep decline from baseline clinical anxiety over time (Figure 2A–2L). However, the prevalence of clinically relevant fatigue among pediatric caregivers (33%) compared with adult caregivers (6%) was notably higher at day 100 (p=0.05).
Figure 2.
Person Reported Outcome Measures
Figure 2A. Anxiety T Scores (Lower more desirable)
Figure 2L.
Financial Concerns (Lower more desirable)
Perceived Usefulness.
Perceived usefulness of BMT Roadmap was measured at discharge, and exhibited high internal consistency (Cronbach’s alpha=0.98). Perceived usefulness did not differ between caregiver groups (ST8). However, at discharge, perceived usefulness correlated significantly with depressive symptoms, fatigue, quality-of-life, and overall distress in adult caregivers (ST6). These associations were not seen in pediatric caregivers.
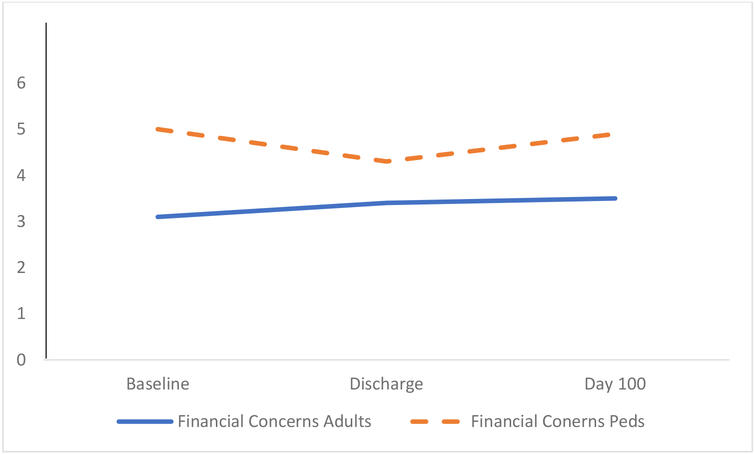
Activation.
Activation increased from baseline to discharge and leveled off at D100 (Figure 2G); and caregiver groups did not differ over time (ST8). Additionally, age and education did not correlate with activation. At baseline, activation was significantly correlated with vigor in pediatric caregivers; this finding was also seen at D100 in both caregiver groups. However, activation was not associated with any mental health PROM at discharge (ST5–ST7).
Figure 2G.
Activation (Higher more desirable)
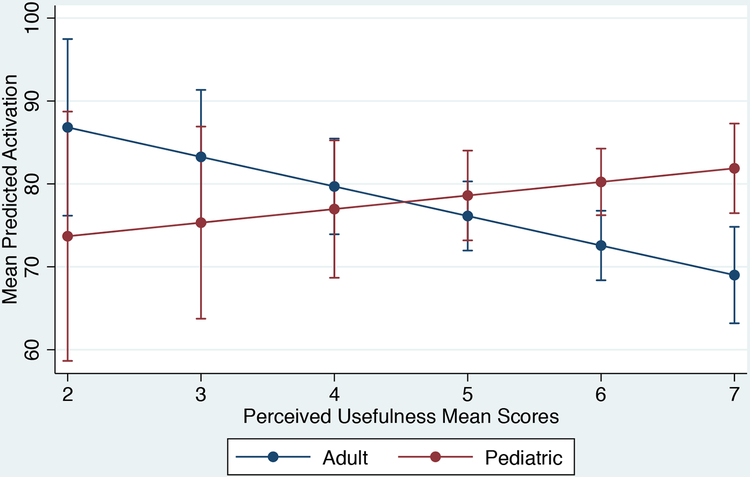
Next, a linear mixed model was fitted to identify determinants of activation by caregiver group over time, controlling for vigor and perceived usefulness (Table 4). Activation increased from baseline to discharge and remained stable at D100, and increased as vigor increased in pediatric caregivers. However, at lower levels of perceived usefulness (i.e., higher perceived usefulness mean scores), adult caregivers reported lower activation (Figure 3).
Table 4.
Determinants of Activation
| Activation† | ||
|---|---|---|
| Parameter | Estimate(SE) p | |
| Group‡ | ||
| Adult Caregivers | 23.7(14.7) | 0.12 |
| Time§ | ||
| Discharge | 8.3(2.5) | 0.001 |
| Day 100 | 5.4(2.6) | 0.04 |
| Group x Perceived Usefulness¶ | ||
| Adult Caregivers x Perceived Usefulness | −5.2(2.5) | 0.04 |
| Vigor | 0.5(0.2) | 0.001 |
| Perceived Usefulness†† | 1.7(4.0) | |
| Wald Chi2 | 37.1 | <0.0001 |
SE = Standard Error
Higher score is more desirable;
Reference: Pediatric Caregivers;
Reference: Baseline;
Reference: Pediatric Caregivers;
Lower score is more desirable
Figure 3.
Mean Predicted Activation by Care Role and Perceived Usefulness
Quality-of-Life.
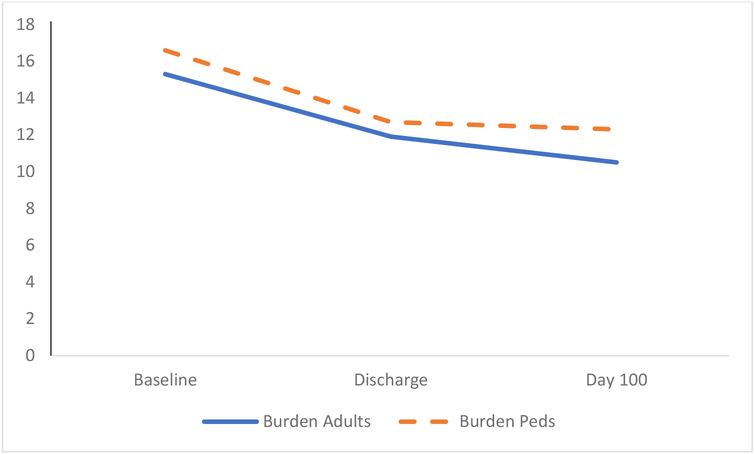
On a univariate level, the quality-of-life did not change over time (ST8; Figure 2H). However, the CQOLC–burden subscale decreased in caregivers from baseline to discharge (both p=0.007; ST8). Not surprisingly, quality-of-life correlated with depression, state anxiety, and fatigue at all-time points (ST5–ST7), but did not correlate with age and education. Thus, we performed a linear mixed model to identify the determinants of quality-of-life. Accounting for BMT Roadmap use, depression, anxiety, and fatigue, quality-of-life lowered at discharge and remained stable at D100. BMT Roadmap use and anxiety and fatigue were significantly associated with quality-of-life when caregiver group and time were accounted for (Table 5).
Figure 2H.
Quality of Life (Lower more desirable)
Table 5.
Determinants of Quality-of-Life
| Quality-of-Life† | ||
|---|---|---|
| Parameter | Estimate(SE) p | |
| Group‡ | ||
| Adult Caregivers | −3.9(2.6) | 0.14 |
| Time§ | ||
| Discharge | 3.2(1.5) | 0.04 |
| Day 100 | 3.3(1.7) | 0.05 |
| Depression† | 1.2(0.3) | 0.001 |
| State-Anxiety† | 5.8(1.1) | 0.001 |
| Fatigue† | 0.3(0.1) | 0.01 |
| Average daily use (minutes/days) | 1.4(0.6) | 0.02 |
| Wald Chi2 | 262.8 | <0.0001 |
SE = Standard Error
Lower score is more desirable;
Reference: Pediatric Caregivers;
Reference: Baseline
DISCUSSION
To our knowledge, this is the first study to investigate the feasibility and impact of a user-centered HIT application addressing informational needs of both adult and pediatric caregivers of HSCT patients. The feasibility of deploying BMT Roadmap was indicated by all eligible caregivers adhering to study procedures throughout patient hospitalization unless their patient relapsed or died. Indeed, we found that both caregiver groups perceived BMT Roadmap as useful and also reported increased activation. We speculate this was due to emphasis on patient-specific informational resources being made available to caregivers in a self-directed medium when and as often as they felt the need for it. We were encouraged by the association of increased vigor (e.g., high energy, positive affect) with activation. After accounting for vigor, we found a notable difference in activation between caregiver groups. Only adult caregivers who perceived BMT Roadmap as less useful exhibited decreased activation, but higher perceived usefulness was not associated with higher activation. Notably, among adult caregivers, greater perceived usefulness of BMT Roadmap correlated with lower quality-of-life and more depression, fatigue, and distress. These findings suggest, therefore, that BMT Roadmap was perceived to be more useful by adult caregivers who were struggling, and consequently, were more reliant on viewing the application repeatedly for information that was not well-understood or remembered. Why this might not be so for pediatric caregivers is worthy of future study. Although the application was a resource for patient-specific information, BMT Roadmap could be further enhanced with new caregiver-specific resources (e.g., peer-to-peer contact, coping techniques, problem-solving skills) that may further enhance caregiver well-being and their ability to care for the patient [21,22]. At this point, adult-specific vs. pediatric-specific caregiver resources could be further developed.
In this study, we found no significant differences in BMT Roadmap use between caregiver groups. Consistent with our previous findings in adult HSCT patients [23], the laboratory module was the most viewed and discharge checklist was the least viewed. Interestingly, adult caregivers spent significantly more time utilizing the medication and phases-of-care modules than pediatric caregivers. It is possible that adult caregivers (mostly spouses) spent less time in the hospital with patients, compared with pediatric caregivers (mostly parents who remained at bedside 24/7), and were not as well-acquainted with HSCT-related medications and phases-of-care.
Univariate analyses indicated that over time, overall quality-of-life did not vary, although burden decreased significantly in both adult and pediatric caregivers. Our speculative hope, that this reflects benefits of patient-specific information and education provided by BMT Roadmap, can only be definitively determined with further investigation. Recognizing that differences in caregiver quality-of-life likely reflect differences in patient and caregiver characteristics and response to BMT Roadmap, we controlled for mental health variables and BMT Roadmap use in linear mixed models, and found that quality-of-life lowered over time, consistent with other reports of low quality-of-life in caregivers of HSCT patients across the transplant trajectory [3,24,25]. In contrast to conventional denotations of the term ‘quality-of-life’ (i.e., physical, emotional, social, functional well-being), CQOLC subscales (i.e., disruptiveness, financial concerns, burden, positive adaptation [reverse scored]) suggest the CQOLC might be indicative, rather, of caregiver strain/onus/hardship. BMT Roadmap was not designed to specifically address disruptiveness, financial concerns, or positive adaptation, but future iterations of the application could. Further, in our study, BMT Roadmap was available only inpatient, not in the outpatient setting to help navigate the new-unknown outpatient caregiving role. Our previous qualitative work indicates that caregivers desire caregiver-specific modules in the outpatient setting, too [12]. Thus, future design should focus on developing these new modules, which is possible with a flexible HIT system.
Although our adult caregivers were significantly older and more educated than pediatric caregivers, age and education were not correlated with perceived usefulness of BMT Roadmap, activation, mental health PROMs, or quality-of-life. Our older adult caregivers expressed no more difficulties or barriers in using BMT Roadmap than younger pediatric caregivers. This suggests the digital divide is narrowing [26], which is important for technology-related solutions. Interestingly, more highly educated caregivers used the laboratory module more. However, examining BMT Roadmap in caregivers with wider range of education will be needed in future work. Additionally, our sample contained few male caregivers, thus precluding gender-specific comparisons. Given the importance of gender differences in caregiving [27], future studies should examine the impact of BMT Roadmap on male caregiving experiences.
Our study has important notable strengths. First, this was a prospective multi-component intervention conducted in caregivers of both adult and pediatric HSCT patients. Second, all of the caregivers approached to participate in the study, consented; only one adult caregiver (2% of those approached) withdrew from the study. We found caregivers eager and willing to participate in this technology-related intervention. Third, the study included longitudinal assessment using multi-dimensional PROMs with high-response rate, and the analyses included linear mixed models that adjust for small sample size as well as with-in participant correlation over time.
Study Limitations
Nonetheless, we recognize the limitations of our work. As previously reported in adult HSCT patients [23], caregivers also faced technological barriers related to logging into the secure hospital wireless network, which was a security requirement (i.e., being timed-out after 10 minutes and having to re-log into the application). The study population was homogeneous, including mostly female, white/Caucasian, and highly educated caregivers from a single institution. In addition, our eligibility requirement of English proficiency reduces generalizability. Thus, we are unable to generalize our findings to caregivers of HSCT patients who are not proficient in English, and caregivers of patients receiving care outside of our institution. However, the purpose of this feasibility study was to examine a preliminary effect of BMT Roadmap on perceived usefulness, activation, and quality-of-life. We found that BMT Roadmap was feasible to investigate among our sample of HSCT caregivers. Future iterations of this work will include a larger efficacy study design to assess the effect of BMT Roadmap on HSCT caregiver mental health outcomes with steps taken to achieve high internal validity and generalizability. The study was also limited by the lack of control groups: adult and pediatric caregivers who did not receive BMT Roadmap throughout HSCT. We accounted for this limitation by employing linear mixed regression models utilizing well-validated and clinically-relevant PROMs to account for the effects of multiple influences on activation and quality-of-life.
CONCLUSIONS
In summary, this study showed that our HIT application, BMT Roadmap, was perceived useful and associated with increased caregiver activation across time. The application was embedded within the standard hospital work flow and there were no unintended consequences. We found that HIT provided a flexible platform to deliver a scalable caregiving intervention, spanning adult and pediatric HSCT caregivers, to address unmet needs for information and support from medical providers. As more caregiving activities are taking place outpatient, our data support the need to further develop caregiver-specific resources and provide the application across the HSCT trajectory (i.e., across inpatient and outpatient settings).
Supplementary Material
Figure 2B.
Distress T Scores (Lower more desirable)
Figure 2C.
Depression T Scores (Lower more desirable)
Figure 2D.
Vigor T Scores (Higher more desirable)
Figure 2E.
Fatigue T Scores (Lower more desirable)
Figure 2F.
Percent of caregivers with clinically significant distress
Figure 2I.
Burden (Lower more desirable)
Figure 2J.
Disruptiveness (Lower more desirable)
Figure 2K.
Positive Adaptation (Lower more desirable)
ACKNOWLEDGEMENTS
This work was supported by AHRQ (R21HS23613), Fostering Innovations Grant, Gracie Leukemia Grant, and the Rita & Alex Hillman Foundation. This work was presented at the Tandem Meeting (02/2018: Salt Lake City, UT) and the Society of Behavioral Medicine Annual Meeting (04/2018: New Orleans, LA). We wish to thank the patients and families who participated in this clinical research study.
Footnotes
CONFLICTS-OF-INTEREST
The authors have no conflicts-of-interest to disclose.
REFERENCES
- 1.Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med 2006;354(17):1813–1826. [DOI] [PubMed] [Google Scholar]
- 2.Simoneau TL, Mikulich-Gilbertson SK, Natvig C, Kilbourn K, Spradley J, Grzywa-Cobb R et al. Elevated peri-transplant distress in caregivers of allogeneic blood or marrow transplant patients. Psychooncology 2013; 22(9):2064–2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Jawahri AR, Traeger LN, Kuzmuk K, Eusebio JR, Vandusen HB, Shin JA et al. Quality of life and mood of patients and family caregivers during hospitalization for hematopoietic stem cell transplantation. Cancer 2015;121(6): 951–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. Jama 2012;307(4):398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Northouse LL, Katapodi MC, Schafenacker AM, Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin Oncol Nurs 2012;28(4): 236–245. [DOI] [PubMed] [Google Scholar]
- 6.Kent EE, Rowland JH, Northouse L, Litzelman K, Chou WY, Shelburne N et al. Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer 2016;122(13):1987–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. 2012. Washington D.C: National Academy Press. [PubMed] [Google Scholar]
- 8.Abernethy AP, Etheredge LM, Ganz PA, Wallace P, German RR, Neti C et al. Rapid-learning system for cancer care. J Clin Oncol 2010;28(27):4268–4274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.e-Connected Family caregiver: Bring caregiving into the 21st Century. National Alliance for Caregiving. http://www.unitedhealthgroup.com/~/media/UHG/PDF/2011/UHC-NAC-eConnected-Family-Caregiver.ashx?la=en. Accessed on 12/04/17.
- 10.Maher M, Kaziunas E, Ackerman M, Derry H, Forringer R, Miller K et al. User-Centered Design Groups to Engage Patients and Caregivers with a Personalized Health Information Technology Tool. Biol Blood Marrow Transplant 2016;22(2): 349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maher M, Hanauer DA, Kaziunas E, Ackerman MS, Derry H, Forringer R et al. A Novel Health Information Technology Communication System to Increase Caregiver Activation in the Context of Hospital-Based Pediatric Hematopoietic Cell Transplantation: A Pilot Study. JMIR Res Protoc 2015;4(4):e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Runaas L, Hanauer D, Maher M, Bischoff E, Fauer A, Hoang T et al. BMT Roadmap: a User-Centered Design Health Information Technology Tool to Promote Patient-Centered Care in Pediatric HCT. Biol Blood Marrow Transplant 2017;23(5):813–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res 2005;40:1918–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weitzner MA, Jacobsen PB, Wagner H Jr., Friedland J, Cox C. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Quality of life research: an international journal of quality of life aspects of treatment, care and rehabilitation 1999;8:55–63. [DOI] [PubMed] [Google Scholar]
- 16.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 17.McNair DM, Loor M, Droppelman LF. Profile of mood states. San Diego, CA: Educational and Industrial Testing Service; 1981. [Google Scholar]
- 18.Davis F Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989; 13(3): 319–340. [Google Scholar]
- 19.West BT, Welch KB, Galecki AT Linear mixed models: a practical guide using statistical software. Second Edition CRC Press; 2014. [Google Scholar]
- 20.Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005;106(8): 2912–2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Q, Loke AY. The positive aspects of caregiving for cancer patients: a critical review of the literature and directions for future research. Psychooncology 2013;22(11):2399–2407. [DOI] [PubMed] [Google Scholar]
- 22.DuBenske LL, Gustafson DH, Namkoong K, Hawkins RP, Atwood AK, Brown RL et al. CHESS improves cancer caregivers’ burden and mood: results of an eHealth RCT. Health psychology 2014; 33(10):1261–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Runaas L, Hoodin F, Munaco A, Fauer A, Sankaran R, Churay T et al. Journal of Clinical Oncology Clinical Cancer Informatics. Accepted, In Press; 2017. [Google Scholar]
- 24.Bevans MF, Mitchell SA, Marden S. The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT). Supportive care in cancer 2008;16(11):1243–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Von Ah D, Spath M, Nielsen A, Fife B. The Caregiver’s Role Across the Bone Marrow Transplantation Trajectory. Cancer nursing 2016;39(1):E12–19. [DOI] [PubMed] [Google Scholar]
- 26.Lopez L, Green AR, Tan-McGrory A, King R, Betancourt JR. Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. Jt Comm J Qual Patient Saf 2011;37(10):437–445. [DOI] [PubMed] [Google Scholar]
- 27.Kim Y, Loscalzo MJ, Wellisch DK, Spillers RL. Gender differences in caregiving stress among caregivers of cancer survivors. Psychooncology 2006;15(12):1086–1092. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.