Abstract
Purpose Evidence for the superiority of in situ simple decompression (SD) versus ulnar nerve transposition (UNT) for cubital tunnel syndrome remains controversial. The purpose of this study was to compare the clinical improvement, complication rate, and revision rate of SD versus UNT using the available evidence.
Materials and Methods We performed a literature search of relevant publications using PubMed, SCOPUS, Cochrane Library, and Springer Link. Inclusion criteria included (1) adult patients >18 years of age, (2) idiopathic cubital tunnel syndrome, (3) primary comparison studies including both SD versus UNT with discrete data for each procedure, (4) average follow-up of at least 2 months, and (5) a full English language manuscript available. Odds ratios of improvement, complications, and revision surgery after SD compared with UNT were calculated. Data were analyzed using both fixed and random effects models, and studies were assessed for publication bias and heterogeneity.
Results A total of 1,511 articles from 1970 to 2017 were identified before inclusion, and exclusion criteria were applied. Ultimately 17 studies met the inclusion criteria and included 2,154 procedures. Of these, 1,040 were SD, and 1,114 were UNT procedures. Study heterogeneity was low. Odds ratios of clinical improvement and revision surgery with SD versus UNT were not significantly different. The odds ratio of complications with SD versus UNT was 0.449 (95% confidence interval [CI] of 0.290–0.695) and 0.469 (95% CI of 0.297–0.738) for fixed and random effect models, respectively. The difference in complications between SD versus UNT was significant ( P < 0.001).
Conclusion There is no statistically significant difference in clinical outcomes or rate of revision surgery between SD versus UNT. However, there were significantly more complications with UNT. The current body of evidence regarding cubital tunnel syndrome lacks prospective, randomized, controlled trials, uniform reporting of indications, and standardized outcome scoring.
Keywords: cubital tunnel, simple decompression, subcutaneous transposition, submuscular transposition, ulnar nerve
Introduction
Cubital tunnel syndrome is the second most common peripheral neuropathy of the upper extremity after carpal tunnel syndrome, with an estimate incidence of 21 cases per 100,000 people. 1 2 3 Despite this, there remains controversy in the optimal surgical treatment of cubital tunnel syndrome. Surgical options include simple decompression (SD) with or without medial epicondylectomy, and an ulnar nerve transposition (UNT), either in a subcutaneous (SC) transposition or intra- and submuscular (SM) transposition. The literature currently lacks sufficient evidence of the superiority of in situ decompression versus transposition due to conflicting reports. 1 2 3
UNT is primarily indicated for acute traumatic ulnar neuropathy, idiopathic ulnar neuropathy with pre- or perioperative nerve instability, recurrent or persistent ulnar neuropathy, and ulnar neuropathy with hardware or lesions within the cubital tunnel. However, for idiopathic cubital tunnel syndrome, surgeon preference has generally dictated the choice of procedure between SD and UNT. Advocates for SD highlight its technical ease, less ulnar nerve manipulation, and less risk of vascular insult to the ulnar nerve. Advocates for UNT argue that SD addresses only ulnar nerve compression but not the effects of traction on the ulnar nerve across the medial epicondyle, where UNT addresses both compression and traction. Traction on the nerve during elbow range of motion may increase compression by raising intraneural pressure, and transposition may relieve it. 4
Since Macadam et al presented their meta-analysis findings 10 years ago that identified a trend, but not statistically significant superior outcomes with UNT rather than SD for cubital tunnel syndrome, several more comparative studies have been published. 5 Therefore, the purpose of this study was to provide an updated meta-analysis comparing clinical improvement of SD versus UNT for idiopathic cubital tunnel syndrome using pooled data of comparison studies. Moreover, while previous meta-analyses have not evaluated complication or revision rates, we also sought to evaluate complication rates and reoperation rates along with the outcome improvement advantages of each procedure.
Materials and Methods
Literature Review
The methods of this meta-analysis emulate that of Macadam et al. 5 We performed a literature search of SD versus UNT comparison studies using PubMed, SCOPUS, Cochrane Library, and Springer Link between from 1970 until 2017. Search terms included “cubital tunnel syndrome,” “ulnar nerve transposition,” “in situ decompression,” and “simple decompression.” Two of the authors (J.S. and D.V.N.) reviewed the abstracts separately for relevancy. If the abstract suggested inclusion in our study, the full manuscript was retrieved and reviewed. We then applied inclusion and exclusion criteria.
Inclusion Criteria
Inclusion criteria included (1) adult patients >18 years of age, (2) idiopathic cubital tunnel syndrome, (3) primary comparison study which included SD versus UNT with discrete data for each procedure, (4) average follow up of at least 2 months, and (5) a full English language manuscript available. Exclusion criteria included (1) incomplete data or outcomes or (2) inclusion of endoscopic cubital tunnel release or medial epicondylectomy in place of open simple decompression.
Data Extraction
For each study that met the inclusion criteria, the intervention, the number of patients in each intervention, gender, mean age, average follow-up time, and outcome measurement were collected and reviewed by two reviewers. Because of variable reporting of outcomes, clinical improvement after intervention was converted to a simplified binary system of “improved” or “not improved.” Improvement was defined as “excellent” or “good” when used by the study's authors as in the Wilson and Krout system, Bishop score, or similar criteria. 1 6 No improvement was defined as “fair” or “poor.” Otherwise, study-specific definitions of improved or not improved were used. When reported in each study, individual complications were summarized for SD and UNT procedures. Reoperation rates were collected for revision surgery performed for persistent or recurrent ulnar nerve neuropathy symptoms or instability only, and not for infection or wound complications.
Analysis
Anterior subcutaneous transposition, submuscular, and intramuscular transposition were grouped together as UNT. Odds ratios of improvement, complications, and revision surgery were calculated for both SD and UNT patients. Dividing the number of “improved” patients by the total number of patients in each intervention generated the odds ratio of improvement. Similarly, dividing the number of patients undergoing revision surgery and number of complications by the total number of patients in each intervention generated odds ratios of revision and complications, respectively. With UNT as the denominator, a ratio < 1 would indicate greater odds of improvement, complication, or revision surgery with UNT. The odds ratios were compared using both fixed effects and random effects models. Effect size is often used in meta-analyses and describes the difference between groups in terms of standard deviations. A fixed effects model assumes no variation in the effect of treatment between groups. A random effects model assumes that the intervention varies between studies because of differences in study methodologies and sample sizes.
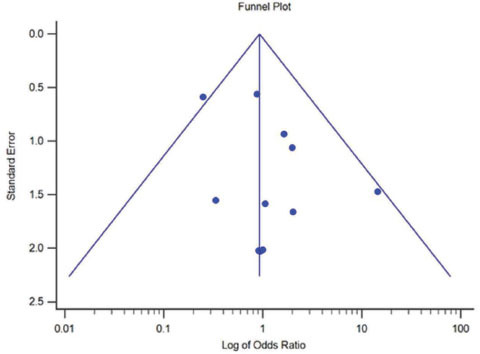
Publication bias was assessed using a funnel plot of the log of the odds ratio versus standard error. Each study represents a circle on the plot. The vertical line represents the pooled odds ratio, and studies to the left of it indicate those that favor UNT. Studies to the right favor SD. The sides of the funnel represent the 95% confidence interval (CI) for a given standard error. An asymmetric plot would suggest missing data points, that is, publication bias.
Statistical analysis was performed using MedCalc Statistical Software version 17.5.5 (MedCalc Software, Ostend, Belgium)
We referred to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. This 27-item checklist is intended to improve transparency and quality reporting in systematic reviews and meta-analyses. 7
Results
Literature Review
A total of 1,511 articles from 1970 to 2017 were identified during the initial search. After title review for relevance, 32 studies were identified ( Fig. 1 ). From these 32 studies, 3 were excluded for lacking a full English text available for review. 8 9 10 Three other studies were excluded for including post-traumatic cubital tunnel syndrome in their analysis. 11 12 13 Two studies were excluded for including medial epicondylectomy in place of SD. 14 15 Twenty-four studies were excluded for lacking discrete data or outcome reporting to compare SD versus UNT.
Fig. 1.
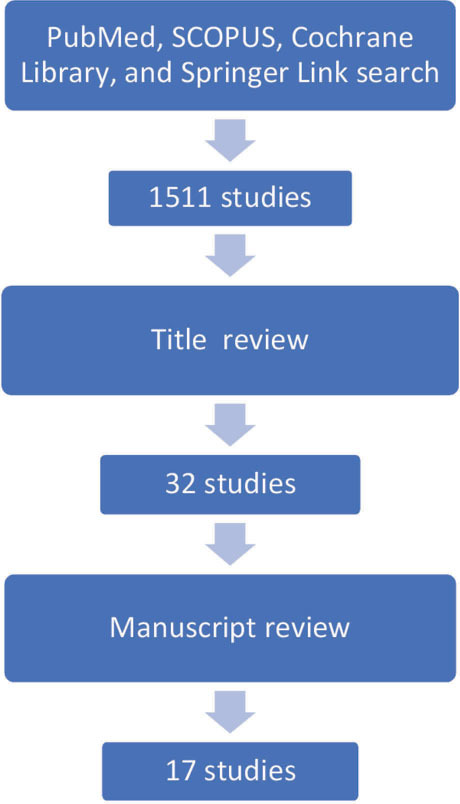
Flow chart of literature review including the number of studies identified at each stage.
Description of Included Studies
Ultimately, 17 studies met the inclusion and exclusion criteria. 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 The included studies are summarized in reverse chronological order in Table 1 . One study included 103 endoscopic patients in a prospective comparison study along with SD and UNT procedures. These 103 patients were excluded from our analysis. Only three prospective randomized trials met our inclusion criteria, with the remainder being retrospective comparisons. 19 20 25 Study dates ranged from 1970 to 2017. Average patient age ranged from 46 to 63 years. In the majority of studies, patients were male. The sample sizes ranged from 33 to 480. Average follow-up period ranged from 2 months to 92 months. A total of 2,154 procedures were included in the analysis. Of these, 1,040 were SD, and 1,114 were UNT. Of the UNT group, 848 were SC, 266 were SM. Measures of improvement varied between studies with some using ad hoc, ordinal rating scales.
Table 1. Study characteristics.
| Study | Year | Journal | Design | N | Gender (% male) | Mean age | Average follow-up (months) | Outcome measure | |
|---|---|---|---|---|---|---|---|---|---|
| Abbreviations: N/A, not applicable; SC, subcutaneous transposition; SD, simple decompression; SM, submuscular transposition. | |||||||||
| Zhang et al | 2017 | J Hand Surg | Retrospective review | 247 | 157 (SD) | 42.6 | 51 | >3 | Complications |
| 29 (SC) | Revisions | ||||||||
| 61 (SM) | |||||||||
| Kamat et al | 2014 | Acta Neurochirur | Retrospective review | 480 | 179 (SD) | 47 (SD) | 51 (SD) | 3 | McGowan score |
| 301 (SC) | 33 (SC) | 49 (SC) | |||||||
| Bacle et al | 2014 | Ortho Traumatol Surg Res | Retrospective review | 409 | 44 (SD) | N/A | 54 (SD) | 92 | Patient satisfaction |
| 178 (SC) | 54 (SQ) | ||||||||
| 103 (endo) | |||||||||
| 84 (SM) | 61 (SM) | ||||||||
| Sousa et al | 2014 | Rev Bras Ortop | Retrospective review | 97 | 64 (SD) | 60.3 (SD) | 51.2 (SD) | 10.3 | Wilson and Kout score |
| 33 (SC) | 54.5 (SC) | 53.3 (SC) | |||||||
| Mitsionis et al | 2010 | J Shoulder Elbow Surg | Retrospective review | 73 | 34 (SD) | N/A | 51 | 37 | McGowan score |
| 39 (SC) | Patient satisfaction | ||||||||
| Keiner et al | 2009 | Acta Neurochir | Prospective | 33 | 17 (SD) | 50 (SD) | 52 (SD) | 63 | |
| 16 (SM) | 70 (SM) | 46 (SM) | |||||||
| Biggs and Curtis | 2006 | Neurosurgery | Prospective randomized | 44 | 23 (SD) | 69 (SD) | 56.7 (SD) | 42 | McGowan score |
| 21 (SM) | 80 (SM) | 61.1 (SM) | Louisiana State University score | ||||||
| Bartels et al | 2005 | Neurosurgery | Prospective randomized | 152 | 75 (SD) | 61 (SD) | 47 | 12 | McGill Pain Questionnaire |
| 77 (SC) | 62 (SC) | Improved/not improved | |||||||
| Asamoto et al | 2005 | Neurol Med Chir | Retrospective review | 72 | 12 (SD) | 69 | 52.3 | 2.2 | Improved/not improved |
| 51 (SC) | |||||||||
| 9 (SM) | |||||||||
| Gervasio et al | 2005 | Neurosurgery | Prospective randomized | 70 | 35 (SD) | 71 (SD) | 53 (SD) | 47 | Bishop score |
| 35 (SM) | 65 (SM) | 52 (SM) | |||||||
| Taha et al | 2004 | Neurosurgery | Retrospective review | 38 | 21 (SD) | 71 | 63 | 48 | Gabel score |
| 17 (SC) | |||||||||
| Bimmler and Meyer | 1996 | Ann Chir Main Memb Super | Retrospective review | 79 | 31 (SD) | 69 | 45 | 76 | McGowan score |
| 48 (SM) | |||||||||
| Adelaar et al | 1984 | J Hand Surg | Prospective | 37 | 7 (SD) | N/A | 51 | 13 | Improved/not improved |
| 22 (SC) | |||||||||
| 8 (SM) | |||||||||
| Foster and Edshage | 1981 | J Hand Surg | Retrospective review | 48 | 29 (SD) | 56 | N/A | 50 | Improved/not improved |
| 19 (SC) | |||||||||
| Chan et al | 1980 | Neurosurgery | Retrospective Review | 235 | 115 (SD) | 75 | 54 | 22 | Improved/not improved |
| 71 (SC) | |||||||||
| 49 (SM) | |||||||||
| MacNicol | 1979 | J Bone Joint Surg | Retrospective review | 80 | 42 (SD) | N/A | 50 | 53 | Improved/not improved |
| 38 (SM) | |||||||||
| Paine | 1970 | Can J Surg | Retrospective review | 63 | 52 (SD) | 81 | 51 | min 12 | Improved/not improved |
| 11 (SC) | |||||||||
Meta-Analysis of Clinical Improvement
The results of the improvement with SD versus UNT meta-analysis and test for heterogeneity are shown in Table 2 . Both fixed and random effects models failed to detect a difference between SD versus UNT, suggesting low heterogeneity. Odds ratio of improvement of SD versus UNT was 0.928 (95% CI of 0.725–1.188) and 0.916 (95% CI of 0.712–1.180) using fixed and random effects models, respectively. The Q test for heterogeneity was 12.45 with a P -value of 0.772. The I 2 value was 0% indicating low heterogeneity.
Table 2. Results for improvement of SD versus UNT.
| Study | Intervention | Controls | Odds ratio | 95% CI | z | p -Value | Weight (%) | ||
|---|---|---|---|---|---|---|---|---|---|
| Fixed | Random | ||||||||
| Abbreviations: CI, confidence interval; DF, degree of freedom; SD, simple decompression; UNT, ulnar nerve transposition. | |||||||||
| Kamat | 161/179 | 266/301 | 1.177 | 0.645–2.147 | 17.67 | 17.67 | |||
| Bacle | 42/44 | 238/262 | 2.118 | 0.482–9.297 | 2.92 | 2.92 | |||
| Sousa | 43/64 | 23/33 | 0.890 | 0.359–2.206 | 7.76 | 7.76 | |||
| Mitsionis | 26/31 | 23/37 | 3.165 | 0.987–10.149 | 4.70 | 4.70 | |||
| Keiner | 16/17 | 14/16 | 2.286 | 0.187–27.996 | 1.02 | 1.02 | |||
| Biggs | 17/23 | 19/21 | 0.298 | 0.0529–1.681 | 2.14 | 2.14 | |||
| Bartels | 49/75 | 54/77 | 0.803 | 0.406–1.587 | 13.75 | 13.75 | |||
| Asamoto | 11/12 | 52/60 | 1.692 | 0.192–14.945 | 1.35 | 1.35 | |||
| Gervasio | 28/35 | 29/35 | 0.828 | 0.247–2.769 | 4.38 | 4.38 | |||
| Taha | 10/21 | 10/17 | 0.636 | 0.175–2.314 | 3.83 | 3.83 | |||
| Bimmler | 17/31 | 35/48 | 0.451 | 0.174–1.168 | 7.05 | 7.05 | |||
| Davies | 49/54 | 71/76 | 0.690 | 0.190–2.512 | 3.83 | 3.83 | |||
| Barrios | 5/7 | 34/46 | 0.882 | 0.151–5.165 | 2.05 | 2.05 | |||
| Adelaar | 1/7 | 7/30 | 0.548 | 0.0560–5.353 | 1.23 | 1.23 | |||
| Foster | 27/29 | 17/19 | 1.588 | 0.204–12.359 | 1.52 | 1.52 | |||
| Chan | 94/115 | 99/120 | 0.949 | 0.487–1.851 | 14.33 | 14.33 | |||
| MacNicol | 18/42 | 20/38 | 0.675 | 0.279–1.632 | 8.20 | 8.20 | |||
| Paine | 41/52 | 9/11 | 0.828 | 0.156–4.402 | 2.29 | 2.29 | |||
| Total (fixed effects) | 655/838 | 1020/1247 | 0.928 | 0.725–1.188 | –0.592 | 0.554 | 100.0 | 100.0 | |
| Total (random effects) | 655/838 | 1020/1247 | 0.916 | 0.712–1.180 | –0.679 | 0.497 | 100.0 | 100.0 | |
| Test for heterogeneity | |||||||||
| Q | 12.4499 | ||||||||
| DF | 17 | ||||||||
| Significance level | p = 0.7722 | ||||||||
| I 2 (inconsistency) | 0.00% | ||||||||
| 95% CI for I 2 | 0.00–31.74 | ||||||||
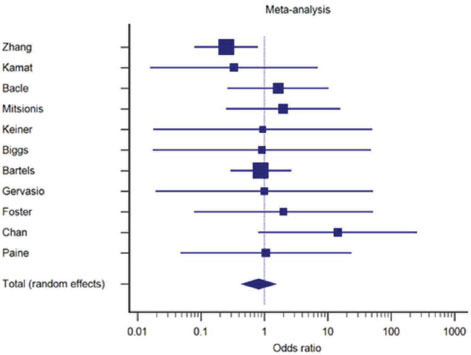
The forest plot and funnel plot for the odds ratio of improvement are shown in ( Figs. 2 3 ), respectively. Depicted in the forest plot, relative clustering of studies toward an odds ratio of 1.0 represent low study heterogeneity. The overall result's confidence interval intersects 1.0 indicating failure to detect a difference.
Fig. 2.
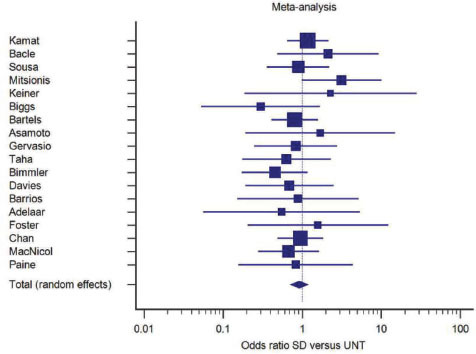
Forest plot of improvement of SD versus UNT. SD, simple decompression; UNT, ulnar nerve transposition.
Fig. 3.
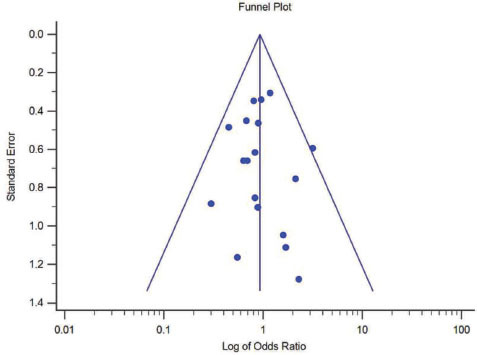
Funnel plot of improvement of simple decompression versus ulnar nerve transposition.
Meta-Analysis of Complications
The results of the complications with SD versusUNT meta-analysis and test for heterogeneity are shown in Table 3 . The odds ratio of complications with SD versus UNT was 0.449 (95% CI of 0.290–0.695) and 0.469 (95% CI of 0.297–0.738) for fixed and random effect models, respectively. This indicates greater odds of complications with UNT. The difference was significant ( P < 0.001) using both fixed and random effects, suggesting low heterogeneity. The Q test for heterogeneity was 6.17 with a P -value of 0.732. The I 2 value was 0% indicating low heterogeneity.
Table 3. Results for complications of SD versus UNT.
| Study | Intervention | Controls | Odds ratio | 95% CI | z | p -Value | Weight (%) | ||
|---|---|---|---|---|---|---|---|---|---|
| Fixed | Random | ||||||||
| Abbreviations: CI, confidence interval; DF, degree of freedom; SD, simple decompression; UNT, ulnar nerve transposition. | |||||||||
| Zhang | 6/157 | 2/90 | 1.512 | 0.343–6.656 | 9.41 | 9.41 | |||
| Kamat | 6/179 | 18/301 | 0.575 | 0.231–1.435 | 24.78 | 24.78 | |||
| Bacle | 0/44 | 22/262 | 0.122 | 0.00729–2.055 | 2.60 | 2.60 | |||
| Sousa | 0/64 | 0/33 | 0.512 | 0.00993–26.388 | 1.33 | 1.33 | |||
| Mitisonis | 0/34 | 1/39 | 0.373 | 0.0147–9.474 | 1.98 | 1.98 | |||
| Keiner | 0/17 | 0/16 | 0.939 | 0.0175–50.316 | 1.31 | 1.31 | |||
| Biggs | 6/23 | 10/21 | 0.394 | 0.113–1.371 | 13.30 | 13.30 | |||
| Bartels | 7/75 | 23/77 | 0.253 | 0.103–0.620 | 25.71 | 25.71 | |||
| Gervasio | 5/35 | 9/35 | 0.500 | 0.154–1.623 | 14.95 | 14.95 | |||
| Foster | 2/29 | 1/19 | 1.101 | 0.133–9.100 | 4.64 | 4.64 | |||
| Total (fixed effects) | 32/657 | 86/893 | 0.449 | 0.290–0.695 | –3.589 | <0.001 | 100.0 | 100.0 | |
| Total (random effects) | 32/657 | 86/893 | 0.469 | 0.297–0.738 | –3.268 | 0.001 | 100.0 | 100.0 | |
| Test for heterogeneity | |||||||||
| Q | 6.1655 | ||||||||
| DF | 9 | ||||||||
| Significance level | p = 0.7232 | ||||||||
| I 2 (inconsistency) | 0.00% | ||||||||
| 95% CI for I 2 | 0.00–45.35 | ||||||||
The forest plot and funnel plot for the odds ratio of complications are shown in ( Figs. 4 5 ), respectively. Depicted in the forest plot, the overall result is <1.0.
Fig. 4.

Forest plot of complications of simple decompression versus ulnar nerve transposition.
Fig. 5.
Funnel plot of complications of simple decompression versus ulnar nerve transposition.
A list of all complications is shown in Table 4 . There were 88 complications in the UNT group and 32 complications in the SD group. The most common complication was scar sensitivity (36 in UNT group and 4 in SD group), infection (25 in UNT group and 11 in SD group) and wound complications (9 in UNT group, 5 in SD group).
Table 4. List of complications of SD and UNT.
| Complication | SD | UNT | Total |
|---|---|---|---|
| Abbreviations: CRPS, complex regional pain syndrome; SD, simple decompression; UNT, ulnar nerve transposition. | |||
| Sensitive scar | 4 | 36 | 40 |
| Infection | 11 | 25 | 36 |
| Wound complication (keloid and dehiscence) | 5 | 9 | 14 |
| CRPS | 2 | 11 | 9 |
| Seroma/hematoma | 4 | 3 | 7 |
| Elbow pain | 2 | 1 | 3 |
| Instability | 3 | 0 | 3 |
| Nerve injury | 1 | 2 | 3 |
| Stiffness | 0 | 1 | 1 |
| Total | 32 | 88 | 116 |
Meta-Analysis of Revision Surgery
The results of the revision surgery with SD versus UNT meta-analysis and test for heterogeneity are shown in Table 5 . Both fixed and random effects models failed to detect a difference between SD versus UNT, suggesting low heterogeneity. The odds ratio of revision surgery with SD versus UNT was 0.930 (95% CI of 0.537–1.609) and 0.809 (95% CI of 0.441–1.484) for fixed and random effect models, respectively. The Q test for heterogeneity was 9.9983 with a P -value of 0.4406. The I 2 value was 0% indicating low heterogeneity. The forest plot and funnel plot for the odds ratio of revision surgery are shown in ( Figs. 6 7 ), respectively. Depicted in the forest plot, relative clustering of studies toward an odds ratio of 1.0 represent low study heterogeneity. The overall result's confidence interval intersects 1.0 indicating failure to detect a difference.
Table 5. Results for revision surgery of SD versus UNT.
| Study | Intervention | Controls | Odds ratio | 95% CI | z | p- Value | Weight (%) | |
|---|---|---|---|---|---|---|---|---|
| Fixed | Random | |||||||
| Abbreviations: CI, confidence interval; DF, degree of freedom; SD, simple decompression; UNT, ulnar nerve transposition. | ||||||||
| Zhang | 4/157 | 9/90 | 0.250 | 0.0789–0.793 | 27.62 | 27.62 | ||
| Kamat | 0/179 | 2/301 | 0.334 | 0.0160–7.006 | 3.97 | 3.97 | ||
| Bacle | 1/44 | 5/262 | 1.646 | 0.263–10.306 | 10.93 | 10.93 | ||
| Mitsionis | 2/34 | 1/39 | 1.984 | 0.248–15.865 | 8.51 | 8.51 | ||
| Keiner | 0/17 | 0/16 | 0.939 | 0.0175–50.316 | 2.32 | 2.32 | ||
| Biggs | 0/23 | 0/21 | 0.911 | 0.0173–48.054 | 2.34 | 2.34 | ||
| Bartels | 6/75 | 7/77 | 0.879 | 0.292–2.647 | 30.27 | 30.27 | ||
| Gervasio | 0/35 | 0/35 | 1.000 | 0.0193–51.847 | 2.36 | 2.36 | ||
| Foster | 1/29 | 0/19 | 2.018 | 0.0779–52.283 | 3.47 | 3.47 | ||
| Chan | 6/114 | 0/120 | 14.451 | 0.805–259.575 | 4.41 | 4.41 | ||
| Paine | 2/52 | 0/11 | 1.061 | 0.0474–23.746 | 3.80 | 3.80 | ||
| Total (fixed effects) | 22/759 | 24/991 | 0.930 | 0.537–1.609 | –0.260 | 0.795 | 100.00 | 100.00 |
| Total (random effects) | 22/759 | 24/991 | 0.809 | 0.441–1.484 | –0.685 | 0.493 | 100.00 | 100.00 |
| Test for heterogeneity | ||||||||
| Q | 9.9983 | |||||||
| DF | 10 | |||||||
| Significance level | p = 0.4406 | |||||||
| I 2 (inconsistency) | 0.00% | |||||||
| 95% CI for I 2 | 0.00–60.37 | |||||||
Fig. 6.
Forest plot of revision surgery of simple decompression versus ulnar nerve transposition.
Fig. 7.
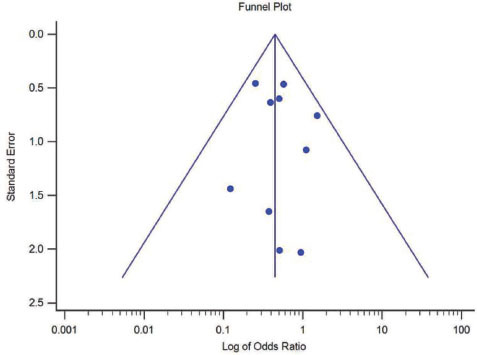
Funnel plot of revision surgery of simple decompression versus ulnar nerve transposition.
Discussion
Evidence for the superiority of UNT or SD for cubital tunnel syndrome has been lacking. Advocates for SD claim that it poses less risk of vascular insult to the nerve, has potentially fewer complications, and requires a smaller incision with potentially shorter surgical time. Advocates for UNT claim that SD addresses only ulnar nerve compression and not the effects of traction across the medial epicondyle. In addition, UNT has the potential benefits in the management of post-traumatic ulnar neuropathy, ulnar nerve instability or subluxation, triceps hypertrophy, and recurrent or persistent ulnar neuropathy post decompression.
The controversy is represented in the literature. Mowlavi et al performed a meta-analysis of 30 studies from 1945 to 1995 including 903 patients treated nonoperatively and operatively. 2 They used an outcome status determination algorithm applied to each study's patients and found that for mild-staged patients, all forms of management including nonoperative were effective. For moderate-staged patients, submuscular transposition produced the highest percentage of total relief and satisfaction and highest percentage of normal strength. For severe-staged patients, results were inconsistent with UNT having a greater percentage of patients without pain, but SD providing a greater percentage of normal strength.
Because a lack of clear advantage of one technique over another has not been identified, we performed an updated meta-analysis of all comparison studies of SD versus UNT for idiopathic cubital tunnel syndrome. Moreover, in addition to examining the rates of improvement, we examined complications and revision rates. This meta-analysis failed to detect a difference in clinical improvement between SD versus UNT after analyzing 2,154 procedures in 17 comparison studies with low heterogeneity. Rather, we found greater complications with UNT than SD (88 vs. 32). The difference in revision surgery for recurrent or persistent symptoms was not significantly different between the UNT and SD groups.
Equivalent clinical outcomes with SD or UNT has grounds in the literature. 3 5 33 34 In a previous meta-analysis, Macadam et al reviewed 10 studies between 1970 and 2006 involving 449 SD procedures and 457 UNT procedures. 5 Using an odds ratio of improvement as the metameter, they too found no statistically significant difference between procedures. In a Cochrane review in 2011 and updated in 2016, Caliandro et al concluded that SD and decompression with transposition are equally effective. Furthermore, transposition was associated with more deep and superficial wound infections. 33 34
UNT had more recorded complications than SD. Most notably, scar sensitivity, infection, and complex regional pain syndrome were greater in the UNT group than those in the SD group. These findings are consistent with using a larger incision, more nerve manipulation, and wider dissection required for transposition. 11 12 13 33 Bartels et al performed a randomized, prospective study and found a higher complication rate with UNT versus SD (31.1% vs. 9.6%) including more numbness (18.6% vs. 2.5%) and more infections (9.3% vs. 2.5%). 19 In another prospective, randomized trial comparing SD versus UNT, Biggs and Curtis found that UNT resulted in greater infection rates than SD. 20 In our analysis, the rate of revision for recurrent or persistent symptoms was not different between groups. This counters the purported advantage of UNT as the definitive treatment of cubital tunnel syndrome. However, this does not factor surgeons’ tendencies for revision or loss to follow-up in this largely retrospective collection of studies.
Strengths of this study include a large study population. Greater than 2,000 procedures were included, the largest sample size on the topic. Heterogeneity of the included studies was low. This was the only meta-analysis comparing SD versus UNT in the past decade. Since the last meta-analysis on the topic, several more comparison studies have been published. We expand on prior reports by comparing clinical improvement, complications, and revision to better guide decision-making. We were also able to isolate idiopathic cubital tunnel syndrome from post-traumatic etiologies and exclude revision surgeries, which eliminates a bias favoring UNT.
This study has several limitations. We chose to include studies with at least 2 months follow-up to include more studies which we believe add value to the analysis despite the short time period. The majority of the studies included in our analysis were retrospective by design, posing potential selection bias. Patients with less severe symptoms are more likely to be treated with SD whereas more severe symptoms would be treated with UNT. Unfortunately, the current body of evidence regarding cubital tunnel syndrome lacks patient randomization or neuropathy severity stratification to counter this potential selection bias. A previous meta-analysis by Zlowodzki et al attempted to avoid the selection bias of surgeon preference for each procedure by including only prospective, randomized studies. 3 However, only four studies met that criteria. One study did not report discrete clinical outcome data, and three studies did not describe whether surgeons were blinded to each patients’ procedure allocation, thereby introducing potential selection bias. These limitations emphasize the variability in reporting outcomes and the difficulty analyzing that data. Lastly, we were unable to compare SM versus SC transposition groups because of underreporting of discrete data in the studies.
Conclusion
In conclusion, there is no statistically significant difference in clinical outcomes or rate of revision surgery between SD versus UNT. However, there were significantly more complications with UNT. Perhaps more important than the method of decompression is proper surgical technique with attention to avoiding iatrogenic injury, meticulous hemostasis, and adequate decompression. We observed that the current body of evidence regarding cubital tunnel syndrome lacks prospective randomized trials, uniform reporting of indications, and standardized outcome scoring. Future studies on the topic should consider accounting for preoperative nerve instability and symptom severity.
Footnotes
Conflict of Interest None.
References
- 1.Kleinman W B, Bishop A T. Anterior intramuscular transposition of the ulnar nerve. J Hand Surg Am. 1989;14(06):972–979. doi: 10.1016/s0363-5023(89)80046-2. [DOI] [PubMed] [Google Scholar]
- 2.Mowlavi A, Andrews K, Lille S, Verhulst S, Zook E G, Milner S. The management of cubital tunnel syndrome: a meta-analysis of clinical studies. Plast Reconstr Surg. 2000;106(02):327–334. doi: 10.1097/00006534-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007;89(12):2591–2598. doi: 10.2106/JBJS.G.00183. [DOI] [PubMed] [Google Scholar]
- 4.Gelberman R H, Yamaguchi K, Hollstien S B et al. Changes in interstitial pressure and cross-sectional area of the cubital tunnel and of the ulnar nerve with flexion of the elbow. An experimental study in human cadavera. J Bone Joint Surg Am. 1998;80(04):492–501. doi: 10.2106/00004623-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Macadam S A, Gandhi R, Bezuhly M, Lefaivre K A. Simple decompression versus anterior subcutaneous and submuscular transposition of the ulnar nerve for cubital tunnel syndrome: a meta-analysis. J Hand Surg Am. 2008;33(08):13140–1.314E15. doi: 10.1016/j.jhsa.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Wilson D H, Krout R. Surgery of ulnar neuropathy at the elbow: 16 cases treated by decompression without transposition. Technical note. J Neurosurg. 1973;38(06):780–785. doi: 10.3171/jns.1973.38.6.0780. [DOI] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman D G. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(04):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto K, Shishido T, Masaoka T, Katori Y, Tanaka S. Postoperative clinical results in cubital tunnel syndrome. Orthopedics. 2006;29(04):347–353. doi: 10.3928/01477447-20060401-14. [DOI] [PubMed] [Google Scholar]
- 9.Geutjens G G, Langstaff R J, Smith N J, Jefferson D, Howell C J, Barton N J. Medial epicondylectomy or ulnar-nerve transposition for ulnar neuropathy at the elbow? J Bone Joint Surg Br. 1996;78(05):777–779. [PubMed] [Google Scholar]
- 10.Seyfettinoğlu F, Karaer A, Sertöz Z, Dülgeroğlu A, Koruyucu M B, Bora O A. [Assessment of the effects of surgical treatment options for cubital tunnel syndrome on the ulnar nerve by USG and EMG] (article in Turkish) Eklem Hastalik Cerrahisi. 2012;23(02):88–93. [PubMed] [Google Scholar]
- 11.Barrios C, Ganoza C, de Pablos J, Cañadell J. Posttraumatic ulnar neuropathy versus non-traumatic cubital tunnel syndrome: clinical features and response to surgery. Acta Neurochir (Wien) 1991;110(01)(02):44–48. doi: 10.1007/BF01402047. [DOI] [PubMed] [Google Scholar]
- 12.Davies M A, Vonau M, Blum P W, Kwok B CT, Matheson J M, Stening W A. Results of ulnar neuropathy at the elbow treated by decompression or anterior transposition. Aust N Z J Surg. 1991;61(12):929–934. doi: 10.1111/j.1445-2197.1991.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 13.Bruder M, Dützmann S, Rekkab N, Quick J, Seifert V, Marquardt G. Muscular atrophy in severe cases of cubital tunnel syndrome: prognostic factors and outcome after surgical treatment. Acta Neurochir (Wien) 2017;159(03):537–542. doi: 10.1007/s00701-017-3086-3. [DOI] [PubMed] [Google Scholar]
- 14.Capo J T, Jacob G, Maurer R J, Nourbakhsh A, Preston J S. Subcutaneous anterior transposition versus decompression and medial epicondylectomy for the treatment of cubital tunnel syndrome. Orthopedics. 2011;34(11):e713–e717. doi: 10.3928/01477447-20110922-18. [DOI] [PubMed] [Google Scholar]
- 15.Hahn S B, Choi Y R, Kang H J, Kang E S. Decompression of the ulnar nerve and minimal medial epicondylectomy with a small incision for cubital tunnel syndrome: comparison with anterior subcutaneous transposition of the nerve. J Plast Reconstr Aesthet Surg. 2010;63(07):1150–1155. doi: 10.1016/j.bjps.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Adelaar R S, Foster W C, McDowell C. The treatment of the cubital tunnel syndrome. J Hand Surg Am. 1984;9A(01):90–95. doi: 10.1016/s0363-5023(84)80193-8. [DOI] [PubMed] [Google Scholar]
- 17.Asamoto S, Böker D K, Jödicke A. Surgical treatment for ulnar nerve entrapment at the elbow. Neurol Med Chir (Tokyo) 2005;45(05):240–244. doi: 10.2176/nmc.45.240. [DOI] [PubMed] [Google Scholar]
- 18.Bacle G, Marteau E, Freslon Met al. Cubital tunnel syndrome: comparative results of a multicenter study of 4 surgical techniques with a mean follow-up of 92 months Orthop Traumatol Surg Res 201410004SupplS205–S208. [DOI] [PubMed] [Google Scholar]
- 19.Bartels R HMA, Verhagen W I, van der Wilt G J, Meulstee J, van Rossum L GM, Grotenhuis J A. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery. 2005;56(03):522–530. doi: 10.1227/01.neu.0000154131.01167.03. [DOI] [PubMed] [Google Scholar]
- 20.Biggs M, Curtis J A. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery. 2006;58(02):296–304. doi: 10.1227/01.NEU.0000194847.04143.A1. [DOI] [PubMed] [Google Scholar]
- 21.Bimmler D, Meyer V E. Surgical treatment of the ulnar nerve entrapment neuropathy: submuscular anterior transposition or simple decompression of the ulnar nerve?. Long-term results in 79 cases. Ann Chir Main Memb Super. 1996;15(03):148–157. doi: 10.1016/s0753-9053(96)80004-4. [DOI] [PubMed] [Google Scholar]
- 22.Macnicol M F. The results of operation for ulnar neuritis. J Bone Joint Surg Br. 1979;61-B(02):159–164. doi: 10.1302/0301-620X.61B2.438266. [DOI] [PubMed] [Google Scholar]
- 23.Chan R C, Paine K W, Varughese G. Ulnar neuropathy at the elbow: comparison of simple decompression and anterior transposition. Neurosurgery. 1980;7(06):545–550. doi: 10.1227/00006123-198012000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Foster R J, Edshage S. Factors related to the outcome of surgically managed compressive ulnar neuropathy at the elbow level. J Hand Surg Am. 1981;6(02):181–192. doi: 10.1016/s0363-5023(81)80173-6. [DOI] [PubMed] [Google Scholar]
- 25.Gervasio O, Gambardella G, Zaccone C, Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56(01):108–117. doi: 10.1227/01.neu.0000145854.38234.81. [DOI] [PubMed] [Google Scholar]
- 26.Kamat A S, Jay S M, Benoiton L A, Correia J A, Woon K. Comparative outcomes of ulnar nerve transposition versus neurolysis in patients with entrapment neuropathy at the cubital tunnel: a 20-year analysis. Acta Neurochir (Wien) 2014;156(01):153–157. doi: 10.1007/s00701-013-1962-z. [DOI] [PubMed] [Google Scholar]
- 27.Keiner D, Gaab M R, Schroeder H W, Oertel J. Comparison of the long-term results of anterior transposition of the ulnar nerve or simple decompression in the treatment of cubital tunnel syndrome–a prospective study. Acta Neurochir (Wien) 2009;151(04):311–315. doi: 10.1007/s00701-009-0218-4. [DOI] [PubMed] [Google Scholar]
- 28.Mitsionis G I, Manoudis G N, Paschos N K, Korompilias A V, Beris A E. Comparative study of surgical treatment of ulnar nerve compression at the elbow. J Shoulder Elbow Surg. 2010;19(04):513–519. doi: 10.1016/j.jse.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 29.Zhang D, Earp B E, Blazar P. Rates of complications and secondary surgeries after in situ cubital tunnel release compared with ulnar nerve transposition: a retrospective review. J Hand Surg Am. 2017;42(04):2940–2.94E7. doi: 10.1016/j.jhsa.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 30.Paine K WE. Tardy ulnar palsy. Can J Surg. 1970;13(03):255–261. [PubMed] [Google Scholar]
- 31.Sousa M, Aido R, Trigueiros M, Lemos R, Silva C. Cubital compressive neuropathy in the elbow: in situ neurolysis versus anterior transposition - comparative study. Rev Bras Ortop. 2014;49(06):647–652. doi: 10.1016/j.rboe.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taha A, Galarza M, Zuccarello M, Taha J. Outcomes of cubital tunnel surgery among patients with absent sensory nerve conduction. Neurosurgery. 2004;54(04):891–895. doi: 10.1227/01.neu.0000115152.78918.61. [DOI] [PubMed] [Google Scholar]
- 33.Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2011;(02):CD006839. doi: 10.1002/14651858.CD006839.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2016;11:CD006839. doi: 10.1002/14651858.CD006839.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]


