Abstract
The paper outlines the achievements and challenges in the additive manufacturing (AM) application to veterinary practice. The state-of-the-art in AM application to the veterinary surgery is presented, with the focus of AM for patient-specific implants manufacturing. It also provides critical discussion on some of the potential issues design and technology should overcome for wider and more effective implementation of additively manufactured parts in veterinary practices. Most of the discussions in present paper are related to the metallic implants, manufactured in this case using so-called powder bed additive manufacturing (PB-AM) in titanium alloy Ti–6AL–4V, and to the corresponding process of their design, manufacturing and implementation in veterinary surgery. Procedures of the implant design and individualization for veterinary surgery are illustrated basing on the four performed surgery cases with dog patients. Results of the replacement surgery in dogs indicate that individualized additively manufactured metallic implants significantly increase chances for successful recovery process, and AM techniques present a viable alternative to amputation in a large number of veterinary cases. The same time overcoming challenges of implant individualization in veterinary practice significantly contributes to the knowledge directly relevant to the modern medical practice. An experience from veterinary cases where organ-preserving surgery with 3D-printed patient-specific implants is performed provides a unique opportunity for future development of better human implants.
Keywords: Additive manufacturing, Ti–6Al–4V, Implants, Veterinary applications of 3D printing, Clinical cases, Osteosarcoma, Dogs
Introduction
Socio-economic value of the pets in human society is well recognized [1–4]. The benefits range from increased mobility of pet owners [5], to the significant contribution into stress management [6, 7] and even to the practice of so-called animal-assisted therapy [8]. All this leads to the strengthening of general animal care and veterinary, supported by increasing penetration of modern technologies into these application areas. For example, veterinary practice is rapidly becoming a beneficiary of additive manufacturing (AM), commonly known as 3D printing or rapid prototyping. It is following the success of AM applications in automotive and aerospace industry and engineering, but especially in biomedicine. Replacement surgery in larger animals like dogs can already successfully use the expertise from the field of human implant design, manufacturing and individualization. Application of AM in veterinary also presents additional challenges, for example a smaller amount of tissue surrounding bones even in larger animals like dogs, which is critical for recovery process. Overcoming such challenges demands not only rethinking of many traditional veterinary-surgical procedures taking into account new possibilities and specifics of AM, as it already happened with human medicine. But it also needs further development of implant and orthoses design and manufacturing process fitting the specifics of veterinary patients. Thus wider applications of AM in veterinary practice will not only benefit our pets but will strengthen the developments in implant and orthoses design and manufacturing methods in the widest sense.
Present paper analyzes the state-of-the-art in the area of AM applications to the veterinary, and discusses specifics and possibilities for additively manufactured items (preoperational models, special tooling for surgery, individualized implants) in veterinary surgery using examples of four surgical cases with larger dogs. It also provides critical discussion on some of the potential problems related technology should overcome for wider and more effective implementation of AM technologies in veterinary practices. Most of the discussions in present paper are related to the metallic implants, manufactured in this case using so-called powder bed additive manufacturing (PB-AM), and to the corresponding process of their design, manufacturing and implementation in veterinary surgery.
State of the art: AM in veterinary
PB-AM representing a wide range of fabrication techniques commonly known as 3D-printing is already successfully used in industry, for example in aerospace and automotive applications, and in bio-medicine [9–12]. However, despite increasing interest the use of this technique specifically for veterinary, applications like veterinary orthotics, prosthetics, reconstructive and bone replacement surgery are just developing, which is reflected in relatively small number of publications describing comparatively small number of veterinary cases [13–17]. The same time, prospects of veterinary AM applications are very wide, especially for so-called organ-sparing surgery. Osteosarcoma is one of the most common tumors of appendicular skeleton in canines. The aim of present research was in identifying the potential of the individualized additive manufactured titanium implants in keeping life quality level of the large-breed dogs after organ-sparing operations, and analyzing the specifics of design for AM and additive manufacturing approaches for veterinary applications.
AM technology is a promising alternative for producing endoprosthesis implants. The use of AM manufactured implants has been actively discussed and practically examined through last years, but mainly in biomedical applications related to humans, and only few publications contain analysis of its potential for the veterinary practice. One of the examples is a publication by Harrysson et al. [13] discussing applications of metal PB-AM in veterinary orthopedic surgery. The authors establish that geometry- and functionality individualization achieved at the implant design stage together with AM can provide effective therapeutic solutions supporting the treatment of working animals and pets with complex medical problems. The authors also conclude that use of metal additive manufacturing is rapidly increasing in veterinary orthopedic surgery. The authors reviewed, described and discussed current and potential applications of metal AM in veterinary orthopedic surgery. Customization and individualization of the implants can play an even larger role in veterinary practice in comparison with human medicine due to the larger variety in bone size and shapes between species and individual animals as compared to human patients. For example, human hip stems usually come in 6 or 7 sizes, as compared to 12 or more sizes with canines to cover for the dogs of different breeds. Also, in many cases there are no off-the-shelf implant solutions for veterinary applications, and custom-made implants are the only available option. Furthermore, in many cases needed implants with complex shapes would be impossible or prohibitively expensive to manufacture using the methods other than AM.
Song et al. [14] reported on the design and fabrication of titanium alloy beak for Grus Japonensis bird. Detailed geometric and structural analysis of the metallic substitute for an upper beak has been performed and AM techniques were used for manufacturing a suitable replacement. The combination of computer based design methods with fused deposition modeling (FDM) and selective laser melting (SLM) manufacturing allowed a quick response time in the challenging production of desired beak- replacement part. A short time after the operation the bird was able to move freely. Analysis showed that FDM and SLM additive manufacturing methods are quite complementary and very relevant to the customized medicine.
Nickels [15] discussed a capability of AM methods in manufacturing lightweight, detailed custom parts. Conclusions indicate that AM could be an ideal process for making certain implants for animals. The author mentioned a perfect fit which can be achieved only by using AM techniques to produce implants. However, in biomedical and veterinary applications the larger future may be with manufacturing one-of-a kind (customized, individualized) parts uniquely designed for a particular case and patient, as compared to the industry, which targets larger scale production. Thus AM is more suitable for the further progress of individualized medicine, as it allows for complex, case- and patient specific solutions leading to improved clinical outcomes, as well as providing cost savings for the healthcare sector.
Osmar [16] described a particular case with designing and manufacturing of part of a toucan’s bill, damaged by a gun shot. Combining different technologies such as plaster casting, optical 3D scanning, reverse engineering, virtual modeling and two different AM technologies it was possible to produce a prototype which would become the prosthesis of toucan´s bill. This research confirms the importance of synergy between different design, modeling and manufacturing approaches in production of prosthesis, and the applicability of many technologies, approaches and even particular design solutions to both human medicine and veterinary. Among such common areas one can mention 3D scanning of the body parts and body part imprints; computer-aided design of the whole implants, fixation plates and their elements; functional modeling of the implants and their interaction with the host; shape- and functional optimization of the implants; customization of the implants and medical tooling for the particular host and medical case; digitally-enhanced manufacturing of the prototypes for the pre-operational planning and final products. Paper also outlines a vast spectrum of possibilities involving both advanced design concepts and “digitally enhanced” production such as AM for different applications, including complicated veterinary cases such as prosthesis of a toucan’s bill.
Paper by Horal [17] describes applications of the additively manufactured implants for studies of fractures in rats and describes the potential of such artificial bodies implanted into bones of small animals. One of the study aims was investigation of inexpensive but stable non-metallic materials for biomedical application. Three point bending tests have been carried out to study how subjecting special polymer-made structures to wet and warm environment affected their properties. The examined nails demonstrated proper mechanical properties, a production of the screws with satisfactory properties using this specific printer was impossible. The PLA and PHA samples were stiff enough even after the exposure to saline. It was concluded that so far it is not yet possible to manufacture the implants from tested materials using chosen type of printer for in vivo studies.
At present there are not many options veterinary surgeons have in the osteosarcoma cases. The most common one is an amputation of the affected limb followed by an endoprosthesis implantation of standard metal plates. Boston and Skinner [18] described a standard resection of the distal radius as a strategy to salvage the limb. Instead of replacing the 6-cm bone defect with an endoprosthesis, the limb was acutely shortened and a carpal arthrodesis plate was applied. The continuation of the treatment included a use of standard fixation plate. This procedure is technically feasible and can save good limb functionality, even with significant limb shortening. A limb lengthening external prosthesis could be considered for cases where the limb length discrepancy created by this technique is thought to result in unacceptable lameness and may be prudent to protect the construct until arthrodesis.
Mitchell et al. [19] reported on the study with forty-five dogs treated using special first- and second generation endoprosthesis (GEN1 and GEN2) basing on medical and radiography records. Surgical outcome studies included assessment of the postoperative lameness and the presence, severity, and time onset of the complications. Oncologic outcomes studies included the monitoring of local metastasis recurrence and time to metastasis recurrence, metastasis free interval, and survival time. The frequency of implant-related complications, including infections, remained unacceptably high for both generations of endoprosthesis.
Seguin et al. [20] reported data on limb-sparing treatment of distal radial osteosarcoma at twenty-six dogs. The authors presented description of full cases, including analysis of defected limb function, challenges of the proposed implantation method, and follow-up period after surgery. This procedure was very complicated, however it allows to keep acceptable limb function. For the surgery were used standard limb-sparing plates. The results showed that local recurrence has not been too high in comparison with alternative limb-sparing approaches.
MacDonald and Schiller [21] reported on a dog with lameness of left forelimb. The limb-sparing surgery was done using a tantalum metal—DCP endoprosthesis. Trabecular tantalum implant was produced by machining. This production method is relatively expensive because of challenging tantalum machining. It was concluded, that tantalum endo-prosthesis, from material point of view, is a competitive implant for limb-sparing surgery.
Nazarali et al. [22] investigated the adhesion effect between the dog’s limb and implant made of stainless steel or tantalum. The performed study highlights the need to evaluate implant surface characteristics in addition to material properties. The authors concluded that porous trabecular structure of tantalum implant is beneficial for recovery process, and even more biocompatible than standard stainless steel limb-sparing plates.
Quinn-Gorham and Khan [23] considered a perspective of AM applications enabling better operation planning and shorter operation times in veterinary surgery. However the investigation was devoted to “printing” of standard fixing plates, not to patient-specific implants. These plates were scanned and then manufactured from aluminum using laser printing. Additively manufactured components had higher accuracy than the original ones. Also, following possibilities for AM applications in veterinary and private medical practice follow from the conclusions of this paper:
Manufacturing of specific medical instruments, cutting and drilling guides becomes feasible and economically viable;
Combination of computed tomography, three-dimensional scanning, and fast prototyping for pre-surgical procedures and surgery conducting becomes much more effective;
Design and manufacturing of patient-specific and individualized implants, tissue and organs using bio-printing is becoming available;
Production of physical models of bone and tissue structures for anatomical study, educational needs, and complex pathological cases is becoming easily available;
Using AM becomes easily available a production of physical models of bone and tissue structures for practical surgery teaching, when trainee can “operate” with the models of the bones and tissues representing certain “standard” or actually happened cases.
The authors mention that the main benefit of the 3D-printing technology is a creative approach to biomedical application [23].
Paper of Koptyug et al. [24] overviewed AM technologies in their applications benefiting orthopedics and prosthetics. To the opinion of the authors, unique and wide possibilities offered by these technologies are yet not properly comprehend and adopted by modern medicine. Indeed, a lot of the advantages of AM have been already experimentally examined and their effectiveness was successfully proven, and they are presently used. On the other hand, many novel properly proven methods are still await to be implemented in the modern medicine practice. Advantages of the AM technologies are not restricted by printing of geometrically complicated solid objects matching biological image-defined shapes. For example, the EBM technique can provide high quality bulk metal parts manufacturing together with shape flexibility. It also allows to produce components with variable density of lattice structures through providing control of the printed component accuracy within a tolerance less than millimeter.
Heinl et al. [25] reported on successfully use of selective electron beam melting (SEBM) for fabrication of novel cellular bodies made of Ti–6Al–4V for orthopedic use. Micro-computed tomography (μCT) analysis demonstrated a possibility to manufacture three-dimensional structures with open porosity, while the pore sizes are beneficial for tissue ingrowth and osseointegration. The authors reported that the mechanical properties of these manufactured porous structures were close to properties of the real human bone, which might minimize stress-shielding effects. It was also reported that chemically improved surface with the use of HCl and NaOH can provide a better connection of implant with the bone and improve by this way implant’s long-term stability.
Renishaw [26] described a case study done on 7-years old big dog with a tumor on the left side maxilla with only option of total excision of the growth which should be followed by a reconstruction. The complexity of the case made, personally patient customized laser 3D-printed titanium implant supporting the bone structure the most reliable treatment. That required a significant freedom of design and manufacturing. The procedure was performed in Canada through use of additively manufactured titanium alloy based implant designed by Voxelmed (Germany). A custom implant with input from the veterinary surgeon was designed using a special model. One day after the surgery, the dog breathed normally through his nose and then leaved the hospital through taking pain medication and antibiotics until a full recovery.
Aikman et al. [27] described a case of dog’s 3D printed prosthetic limb implantation. A patient—25 kg, 4-years old dog—had the right hind limb amputated when it was a puppy due to neglect and injury. The presented how design, modelling and 3D printing of a prosthetic leg for this dog can improve its life quality. The design included a flexible brace that wraps around her thigh to support the majority of the dog’s weight on that leg. The residual limb was placed on a foam and neoprene surface and secured with soft Velcro to the mount. The 3D-production method provides opportunity to replace the spare parts of the prosthetic. Finite element analysis (FEA) was performed on the load bearing parts of the prosthetic leg design. System level testing was also performed on the second prototype of the prosthetic.
Bachman et al. [28] reviewed the current market, of prosthetics for dogs with amputations. Since a high variety in limb deformities, the solution should be a customizable one. Therefore, AM techniques may be successfully applicable for such patient specially tailored solutions. The authors discussed various anatomic features of the dog bone diseases as well after-surgery recovering therapy. The authors described their trials to design and produce low-cost devices that would increase mobility and then life quality of such dogs.
In other work [29] the authors investigated the effect of surface roughness/texture on osseointegration process. The EBM-manufactured and machine-threaded implants were compared. The performed research demonstrated that EBM produced textured surfaces provide enhanced mechanical stability compared to those produced by machine threading.
Basing on the achievements listed above, the main goal of described research was in developing a novel promising approach to designing and manufacturing of veterinary patient-specific implants using modern digital technology and AM. As it was mentioned above, this technique enables to design patient-specific implants and produce them from biocompatible or at least bioinert material with relatively short lead-time from design to surgery. Present paper describes four veterinary surgical cases when additively manufactured case- and patient-specific titanium alloy implants were successfully used in large dogs. All the implants have been manufactured by PB-AM from Ti–6Al–4V powder.
Materials and methods
The surgery procedures with four large breed dogs with osteogenic sarcoma have been performed in the period November 2017–May 2018. The age of the animals ranged from 5 to 9 years. In all four cases it was necessary to substitute large sections of the bone that should be removed during surgery, and provide adequate implant stability allowing for restoring proper dog- patient movement. The weight, sex and other relevant data for the dog- patients are presented in the Table 1. General clinical examination of the animals was performed to establish a correct diagnosis. X-ray examination, fine-needle and core biopsy of their lesions, as well as of regional lymph nodes have been carried out during the preoperative planning process. The tumor had typical locations, which for these cases were: distal forelimb—cases 2 and 3 (see Figs. 4, 6), and distal portion of the hind limb—cases 1 and 4, (see Figs. 2, 8). All animals underwent contrast-enhanced computed tomography in search of metastases and for the purpose of operation planning and implant design. All animals received 1–2 chemotherapy sessions using carboplatin while waiting for the customized implant to be designed and manufactured. The chemotherapy was continued 10–14 days postoperatively to reach the total of 5–6 sessions. 3D-planning and 3D-modelling of the implants, preoperational models and special surgery support tooling was performed using Polygon Medical Engineering (PME) Software. The cases 1–3 were operated by a surgeon Stas Usov at veterinary clinic Ortho-Vet (Russia). The surgery for the 4th case was performed by a chief surgeon Dr. Jorge Leite, veterinary hospital Bone Matrix (Portugal). Corresponding procedures related to pre-operative planning were led by the veterinary surgeons with the support of designers and AM specialists. All procedures related to the surgery were carried out by the veterinary clinics.
Table 1.
Data of dog-patients
| Name | Breed of dog | Sex | Age | Weight (kg) | Diagnosis | |
|---|---|---|---|---|---|---|
| 1 case | Baron | Watch-dog | Male | 9 | 50 | Osteosarcoma |
| 2 case | Keirat | Central asian shepherd dog | Male | 9 | 68 | Osteosarcoma of radial bone |
| 3 case | Yulik | Half-breed | Male | 7 | 56 | Osteosarcoma |
| 4 case | Pipa | Labrador retriever | Female | 5 | 42 | Osteosarcoma |
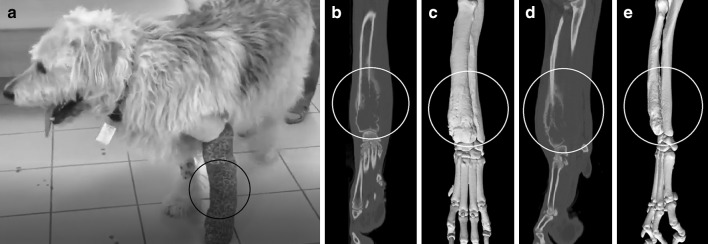
Fig. 4.
Case 2: a the photo of the dog with the limb prepared for surgery; b, d X-ray images of the limb; c, e images of the digital model of the damaged limb
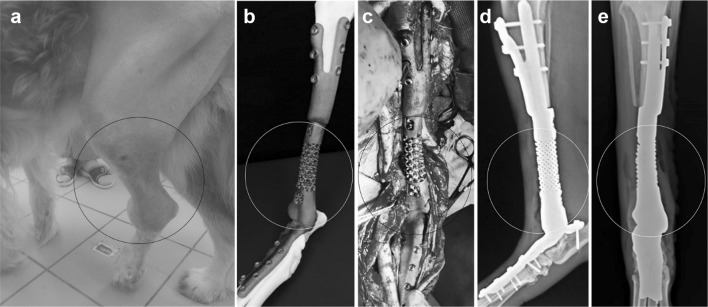
Fig. 6.
Case 3: a the photo of the dog with the limb prepared for surgery; b, d X-ray images of the limb; c, e images of the digital models of the defected limb
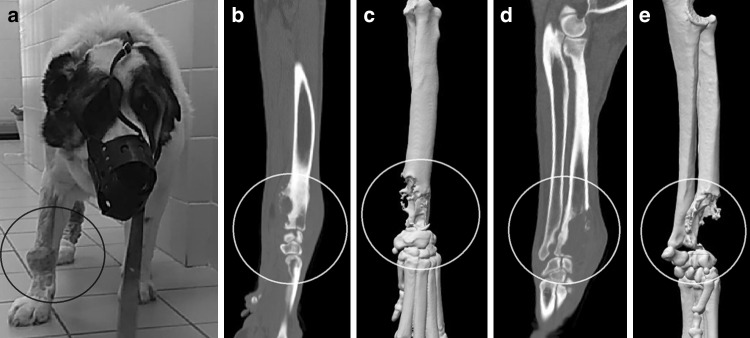
Fig. 2.
Case 1: a the photo of the dog with the limb prepared for surgery; b, d X-ray images of the limb; c, e corresponding images of the digital models of the defected limb
Fig. 8.
Case 4: a the photo of the dog with the limb prepared for surgery; b, d, e X-ray images of the defected limb; c, f digital model of the defected limb and joint
The CT scans in DICOM format were imported to the PME Planner software. Based on these data digital 3D models of the damaged bones were constructed, and basing on these digital models for the custom-made cutting and drilling guides and individualized titanium implants needed to restore the defect were prepared. After that 3D models were processed and sent to corresponding 3D-printing devices for manufacturing.
The use and application of custom-made cutting/drilling guides are illustrated on Fig. 1 from the case 2 study described further in more detail. One tool was designed for cutting and drilling the proximal part of the bones (Fig. 1a, b), whereas the other—for the distal parts (Fig. 1c, d). Stereolithographic (SLA) technique was used to produce the cutting and drilling guides from a Nextdent Dental SG material. The cutting and drilling guides had 3D-outlines reproducing the shape of the bones ensuring their proper fit for high precision in positioning and angles of the cutting tools and drills, thus preparing best possible fit of customized implants and their osseointegration.
Fig. 1.
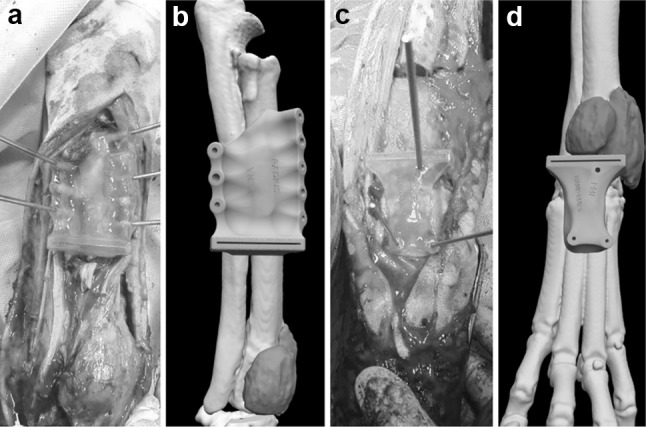
Case 2: a, c photographic images of application of cutting/drilling guides during the surgery; b, d digital images of the defected limb with the tumor and cutting/drilling guides set into proper positions
During the first phase of the intervention the proximal portion of the bone was accessed, its surface was prepared for the cutting/drilling guides’ placement, and for the installation and temporary fixation of the guide using the guide pins. At the second phase the bone was drilled, followed with oscillation saw osteotomy and excision of the affected area. At the third phase the distal portions of the limbs were accessed, their surface was prepared for cutting/drilling guide placement, as well as replacement and temporary fixation of the guides with the pins (see Fig. 1a, c). The fourth phase included cutting the bone and the placement of custom-made titanium implant.
Titanium implants came in two designs following what can be called a “bionic” and “quasi-classic” approach. Implants of the “bionic” design (case 1, see Fig. 3) used fixation plates conformal to the outlines of remaining bones, and a stem following the outlines of a healthy bone containing lattice structure on part of its surface. Implants of the “classical” design (cases 2–4, see Figs. 5, 7, 9) were built with two fixating elements (upper- “fork” and lower- plate) connected with a central cylinder that is thinner as compared to the outline of a healthy bone. With both design approaches the proximal and distal parts of the implants contacting with the bone had osseointegration- friendly surface (see Fig. 5c). Custom-made titanium implants were produced using two PB-AM techniques: Electron Beam Melting (EBM) and Selective Laser Melting (SLM) from the Ti–6Al–4V alloy specified by ASTM standards and US FDA [30] for surgical implants. The SLM implants (cases 2 and 3) and EBM implants (cases 1 and 4) were attached to the bone with traditional locking screws.
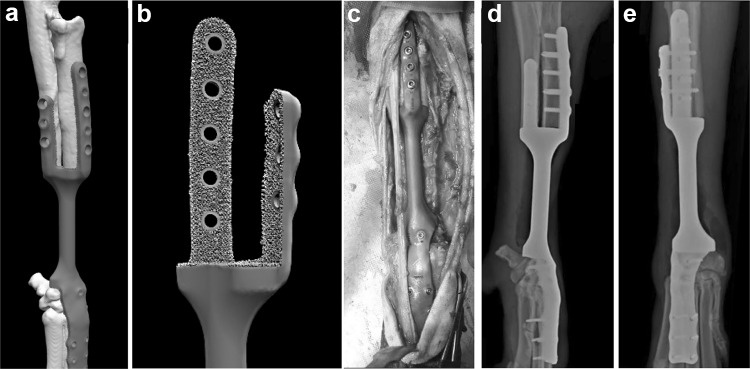
Fig. 3.
Case 1: a the photo of the dog with the limb prepared for surgery; b image of the final EBM-manufactured titanium implant with the preoperational bone model additively manufactured from a polymer; c surgical placement of the implant; d, e final CT images after surgery
Fig. 5.
Case 2: a, b image of the digital model of titanium implant with the bone; c surgical replacement of the implant; d, e CT 2 days after surgery
Fig. 7.

Case 3: a digital model of the titanium implant with the bone; b surgical placement of the implant; c, d CT after several days after surgery
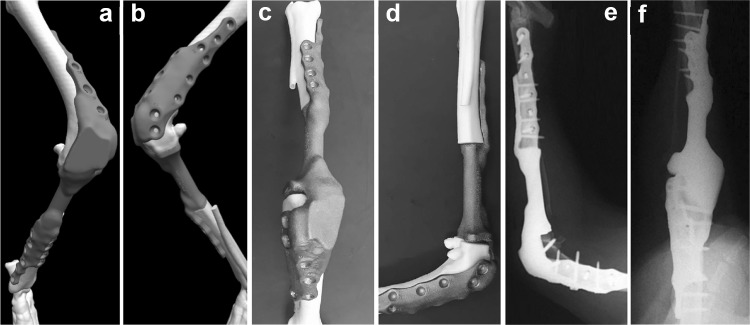
Fig. 9.
Case 4: a, b digital models of the bones and virtually installed implant; c, d images of the final 3D-printed models of the bones and installed titanium implant; e, f final CT after surgery
All the additively manufactured implants were passed the necessary post-processing—polishing of outer surface and machining of locking screw seats.
EBM manufacturing and mechanical properties investigation was carried out by TechMed laboratory of Israel Institute of Metals. To determine the mechanical characteristics of the material, fatigue and impact tests were carried out. Fatigue strength examination was performed for 5 test specimens manufactured with the same technology (EBM), from the same material (Ti–6Al–4V). Specimens were prepared according to the requirements of ASTM E466 Standard [31] with a diameter D = 6.0 mm (stress area ~ 28.3 mm2). The fatigue test was performed according to ASTM E466 Standard with a focus on high cycle number stability.
The impact test was carried out according to ASTM E23 - 12c Standard Test Methods for Notched Bar Impact Testing of Metallic Materials [32] using Wolpert impact testing machine (available energy 150 J). The force controlled constant amplitude uniaxial loading was carried out using an Instron 8801 testing machine (Dynacell, Dynamic Load Cell ± 100 kN) under load control with a sinusoidal waveform of a loading force. Three sets of standard (10 × 10 × 55 mm) V-notch impact Ti–6Al–4V specimens were prepared by EBM according to the requirements of ASTM E23 - 12c Standard Test Methods for Notched Bar Impact Testing of Metallic Materials. All material tests were performed at 23 ± 2 °C temperature.
Results and discussion
Case 1
For the first investigated case (Fig. 2) implant with a large lattice-structured area in the middle part designed following the “bionic” approach was manufactured using EBM-technology (see Fig. 3). Figure 2 illustrates the medical condition of the dog with the hind limb osteosarcoma in this case. On Fig. 2b, d, the cancer tumor is shown. The bone damage is easily visible in the images of digital models generated from CT scan data (see Fig. 2c, e).
The goal in this case was helping a dog-patient targeting restoring the damaged limb functionality, and investigating the main benefits of PB-AM implementing net-shape structures and patient specific geometries. However, the approach when the implant reproduces the outlines of the healthy bones is not universal, and for this case it was not correct solution as followed from the post-operational assessment. Following issues were outlined:
Patient-specific shape of the implant (Fig. 3b): because of the attempt to reproduce the exact bone shape, the implant diameter was too large, and it was hard to close the implant by the existing tissue. The lack of tissue was a result of highly progressed cancer (besides the fact that metallic rod of the same diameter as a bone is by far too rigid);
Lattice structured area: the open-cellular geometry was chosen basing on the suggestions that it promotes vascularization and supposedly improves recovery process, promoting joining of the live tissue with implant surface [12, 33]. However, open lattice area of the implant resulted in a big amount of air trapped in it, leading to the growth of aerobic bacteria, which led to an inflammatory process.
Figure 3a–e illustrate the preoperative planning, surgery and its results in case 1 (final titanium EBM-manufactured implant with diamond lattice structure; surgical replacement of the implant; and CT-images taken days after surgery). Because of the issues explained above, to prevent the advance of inflammatory process the limb with implant was later amputated.
Case 2
The Fig. 4 presents the condition of the dog bones in the case 2, the large- breed dog with damaged forelimb. The part of the bone lost to a progressing cancer is clearly visible in the images on Fig. 4b–e.
For the case 2 the previous experience was taken into account and the cylindrical part of the implant was implemented without lattice and not following the outline of the healthy bone. However the cellular trabecular structures were used at the inner surface of the implant contacting the bone (see Fig. 5b). Followed approach can be called “quasi-classic”; as such strategy and application of trabecular surfaces are well developed with the biomedical implants for human (e.g. [34]). Such solutions commonly result in relatively fast and efficient patient recovery.
Figure 5 presents the process steps for the case 2 from model-image of the implant to surgery, and post-surgery CT-images. The CT-images (Fig. 5d, e) were taken 6 weeks after the surgery. From Fig. 5d, e it is clear that the osseointegration process is going on adequately already after 6 weeks after the surgery. More than that, 5 weeks after surgery the dog ceased to limp for the first time since the formation of the tumor.
Case 3
The successful “quasi-classic” approach used in the case 2 was approved for the case 3, with the dog patient having same diagnosis (see Fig. 6).
Figure 7 presents the design of an SLM-manufactured implant and illustrates the process of surgery and its outcomes. The design implements the same principle as used in case 2. Figure 7c, d shows the CT images taken 2 weeks after surgery. To the moment the results of surgery are regarded as successful.
Case 4
Case 4 (Fig. 8) was rather specific and complicated, because of the damaged knee bone of a dog patient in the joint area (see Fig. 8b–f).
The titanium implant was manufactured by EBM using already proven trabecular inner surface of fixation elements and “quasi- classic” design approach (see Fig. 9c, d). The design of implant was performed using a “minimum contact” approach, when connecting plates are not contacting the bone over the whole surface, but only via special protruding spacers [35]. This is a well-known design element in bone fixation plates used in orthopedic surgery with human patients. However, there were not found any reported implementation of this approach for patient-specific implants, and specifically- in veterinary applications. Figure 9 illustrates the digital models of the implant and the bone (see Fig. 9a, b); the 3D-printed titanium implant with plastic printed bone (see Fig. 9c, d); and on the Fig. 9e, f present the CT-images of the installed implant after surgery. Two weeks after surgery the results are regarded as successful.
Mechanical property studies
To approve the high mechanical properties of the manufactured patient-specific implants, impact and fatigue strength tests have been conducted on the used titanium alloy samples made in the same technology. The results presented in Tables 2 and 3 show the fatigue and impact strength of EBM-manufactured Ti–6Al–4V made in the same machine, from the same material batch and using same process parameters. In the Table 2 are presented 4 examined samples, and is shown that fatigue strength results increased up to 4% in comparison with traditionally manufactured Ti–6Al–4V specimens [36–39].
Table 2.
Fatigue test results for EBM-manufactured Ti–6Al–4V specimens
| Specimen No. | Maximum load, Pmax (kN) | Corresponding maximum cycle stress (MPa) | Number of cycles to failure |
|---|---|---|---|
| 1 | 16.2 | 572 | 984,704 |
| 2 | 15.0 | 530 | 3,438,852 |
| 3 | 14.0 | 495 | 2,558,642 |
| 4 | 15.0 | 530 | 1,168,277 |
| Average | 531,75 |
Table 3.
Impact test results for EBM-manufactured Ti–6Al–4V specimens
| Sample ID | Specimen ID | Test piece dimensions (mm) | Impact energy (kV J) | ||
|---|---|---|---|---|---|
| Length, I | Height, h | Width, w | |||
| 1 | ZX-1 | 55.1 | 10.10 | 11.10 | 21 |
| ZX-2 | 55.2 | 10.10 | 11.10 | 18 | |
| ZX-3 | 55.2 | 10.10 | 11.10 | 18 | |
| Average | – | – | – | 19 | |
| 2 | ZY-1 | 55.2 | 10.20 | 11.10 | 16 |
| ZY-2 | 55.2 | 10.20 | 11.10 | 17 | |
| ZY-3 | 55.2 | 10.00 | 10.15 | 15 | |
| Average | – | – | – | 16 | |
| 3 | Z-1 | 54.4 | 10.25 | 11.10 | 26 |
| Z-2 | 54.3 | 10.10 | 11.00 | 26 | |
| Z-3 | 54.5 | 10.45 | 11.10 | 26 | |
| Average | – | – | – | 26 | |
Table 3 presents results for three sets of standard prism-like specimens. The specimens were printed in three directions—horizontal ZX, ZY, and vertical Z. Results for the 3rd set of specimens manufactured vertically in z-axis direction showed relatively better results, that confirmed sufficient melting ability of the material along this axis. Impact increased up to 15% according to Refs. [36–39].
The obtained results indicate better mechanical properties of additively manufactured Ti–6Al–4V samples, as compared to the ones made using traditionally methods [36–39]. Mechanical properties examination confirms high prospects of PB-AM technology and Ti–6Al–4V alloy for biomedical veterinary applications.
More than that it is already well-known that the fatigue resistance of AM parts could be additionally improved by hot isostatic pressure (HIP) treatment which reduces significantly the porosity level in additively manufactured components [40, 41]. Such treatment is relatively expensive and used mostly for human critical implants that undergo high cyclic fatigue loading like mandibular implants [12].
Conclusions
The use of AM technologies for restoring bone defects and substituting large sections of lost bones in organ-sparing operations is a promising veterinary approach which warrants further studies. In our case studies all operated animals began to actively use their restored limbs and showed good functional results. There was no need for the application of nonsteroidal anti-inflammatory drugs (NSAIDs). Seroma was observed only in the 1st case, presumably due to the onset of inflammatory process and presence of aerobic bacteria inside the lattice part of the implant. The outcomes of this case also outline the necessity of careful approach to designing metallic implants and integration of the medical specialists into this process. For example, the undesired long-term outcome in this case was caused by the desire to have implant following the shape of healthy bone, without considering the consequences of the disease process, such as a lack of soft tissue that should cover this implant, and corresponding complications for the surgery process.
All operated animals restored weight-bearing capacity early and showed good functional outcomes, which supports the efficiency of the implant individualization in veterinary. The described technique allows surgeon to accurately plan tumor resection in 3D and to translate it into the design of both custom-made implants and surgery supporting tools. This helps to shorten the time of the intervention lowering its cost, and improves post-operational prospects for the patients due to much better fit of the implants. This should provide faster and more effective recovery of the patient and reduced risk of implant failure. After several months all patients are alive and did not have metastatic lesions. However, long-term results of the cases warrant further examination.
The presented positive results of novel 3D-approach should promote development of this application for veterinary surgery. Simultaneously, studies of the outcomes in implant studies with canine patients can significantly help developing procedures and concepts relevant to human patients. Curing different bone defects of larger dogs with the sizes of needed implants similar to the ones used in orthopedic surgery, and with relatively fast healing process allowing fast result assessment, should allow for developing better implant design procedures.
AM sparing limbs approach provides comfortable rest life for a dog. However, in a case of progressing sarcoma, amputation can be performed anyway. That means that AM sparing limbs surgery may be a good solution for life quality, however, without effect on a dog’s lifetime.
Further work on the subject will include the analysis and revisions to the “bionic” approach including the integration of lattice structures into the implants for the veterinary applications, and long term monitoring of the already operated dog- patients. Additionally, the development of veterinary AM includes simulation of implants design which should approve the geometry, control stress points, and determine the necessary amount of screws and distance between them.
Acknowledgements
Authors want to thank Dr. Jorge Leite, Bonematrix (Portugal) for fruitful joint work on the 4th case and conducting the challenging surgery; Haim Rosenson and Dr. Jean Ramon for support of biomedical activities in Israel Institute of Metals (IIM); the IIM team for conducting all the necessary 3D printing and testing activities.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained in Russia (cases 1–3) and Portugal (case 4) according to the local guidelines for the care and use of animals.
Contributor Information
Vladimir V. Popov, Jr., Email: vvp@technion.ac.il
Gary Muller-Kamskii, Email: garym@technion.ac.il.
Alexander Katz-Demyanetz, Email: kalexand@trdf.technion.ac.il.
Aleksey Kovalevsky, Email: alekseyk@trdf.technion.ac.il.
Stas Usov, Email: stasusov@mail.ru.
Dmitrii Trofimcow, Email: trofimcow@bk.ru.
Georgy Dzhenzhera, Email: gdjenjera@gmail.com, https://www.polygonmed.ru.
Andrey Koptyug, Email: andrey.koptyug@miun.se.
References
- 1.The social and economic value of pets to human society, The Telegraph (UK). 2017. https://www.telegraph.co.uk/pets/news-features/social-economic-value-pets-human-society/.
- 2.Hall S, Dolling L, Bristow K, Fuller T, Mills D. Companion animal economics. The economic impact of companion animals in the UK. S CABI (Centre for Agriculture and Biosciences International), Paperback. 2017. 10.1079/9781786391728.0000.
- 3.Saunders J, Parast L, Babey SH, Miles JV. Exploring the differences between pet and non-pet owners: implications for human-animal interaction research and policy. PLoS ONE. 2017;12(6):e0179494. doi: 10.1371/journal.pone.0179494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herzog H. The impact of pets on human health and psychological well-being fact, fiction, or hypothesis? Curr Dir Psychol Sci. 2011;20(4):236–239. doi: 10.1177/0963721411415220. [DOI] [Google Scholar]
- 5.Cutt H, Giles-Corti B, Knuiman M, Timperio A, Bull F. Understanding dog owners’ increased levels of physical activity: results from RESIDE. Am J Public Health. 2008;98(1):66–69. doi: 10.2105/AJPH.2006.103499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shiloh S, Sorekt G, Terkel J. Reduction of state-anxiety by petting animals in a controlled laboratory experiment. Anxiety Stress Coping. 2010;16(4):387–395. doi: 10.1080/1061580031000091582. [DOI] [Google Scholar]
- 7.Beetz A, Uvnäs-Moberg K, Julius H, Kotrschal K. Psychosocial and psychophysiological effects of human–animal interactions: the possible role of oxytocin. Front Psychol. 2012;3:234. doi: 10.3389/fpsyg.2012.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nimer J, Lundahl B. Animal-assisted therapy: a meta-analysis. Anthrozoos. 2007;20(3):225–238. doi: 10.2752/089279307X224773. [DOI] [Google Scholar]
- 9.Herderick E. Additive manufacturing of metals: a review, vol 2; 2011. p. 1413–1425.
- 10.Koptyug A, Rännar L, Bäckström M, Cronskär M. Additive manufacturing for medical and biomedical applications: advances and challenges. In: Materials science forum; 2014. p. 1286–1291.
- 11.Kolomiets A, Popov V, Strokin E, Muller G, Kovalevsky A. Benefits of additive manufacturing for industrial design development. Trends, limitations and applications. Glob J Res Eng. 2018;18(2).
- 12.Popov VV, Muller-Kamskii G, Kovalevsky A, et al. Design and 3D-printing of titanium bone implants: brief review of approach and clinical cases. Biomed Eng Lett. 2018;8:337. doi: 10.1007/s13534-018-0080-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harrysson OLA, Marcellin-Little DJ, Horn TJ. Applications of metal additive manufacturing in veterinary orthopedic surgery. JOM J Miner Met Mater Soc. 2015;67(3):647–654. doi: 10.1007/s11837-015-1295-x. [DOI] [Google Scholar]
- 14.Song C, Wang A, Wu Z, Chen Z, Yang Y, Wang D. The design and manufacturing of a titanium alloy beak for Grus japonensis using additive manufacturing. Mater Des. 2016 [Google Scholar]
- 15.Nickels L. Positive prognosis for 3D printed animal implants. Metal Powder Rep. 2018 [Google Scholar]
- 16.Osmar R. Veterinary additive manufacturing: development of a prosthesis of a toucan’s bill. In: Conference: RAPID 2015; 2015.
- 17.Horal M. 3D printing implants for fracture healing studies in rats. Department of Biomedical Engineering. 2015. 10.5703/1288284315910. http://lup.lub.lu.se/luur/download?func=downloadFile&recordOId=8310516&fileOId=8310520.
- 18.Boston SE, Skinner OT. Limb shortening as a strategy for limb sparing treatment of appendicular osteosarcoma of the distal radius in a dog. Vet Surg. 2018;47:136–145. doi: 10.1111/vsu.12726. [DOI] [PubMed] [Google Scholar]
- 19.Mitchell KE, Boston SE, Kung M, Dry S, Straw RC, Ehrhart NP, Ryan SD. Outcomes of limb-sparing surgery using two generations of metal endoprosthesis in 45 dogs with distal radial osteosarcoma. A veterinary society of surgical oncology retrospective study. Vet Surg. 2016;45:36–43. doi: 10.1111/vsu.12423. [DOI] [PubMed] [Google Scholar]
- 20.Seguin B, O’Donnell MD, Walsh PJ, Selmic LE. Long-term outcome of dogs treated with ulnar rollover transposition for limb-sparing of distal radial osteosarcoma: 27 limbs in 26 dogs. Vet Surg. 2017;46:1017–1024. doi: 10.1111/vsu.12698. [DOI] [PubMed] [Google Scholar]
- 21.MacDonald TL, Schiller TD. Limb-sparing surgery using tantalum metal endoprosthesis in a dog with osteosarcoma of the distal radius. Can Vet J. 2010;51:497–500. [PMC free article] [PubMed] [Google Scholar]
- 22.Nazarali A, Singh A, Morrison S, Gibson TWG, Rousseau J, Weese JS, Boston SE. Comparison of methicillin-resistant Staphylococcus pseudintermedius adherence to 2 canine limb salvage endoprosthesis implants. Can Vet J. 2017;58:964–966. [PMC free article] [PubMed] [Google Scholar]
- 23.Quinn-Gorham DM, Khan JM. Thinking outside of the box: the potential of 3D printing in veterinary medicine. J Vet Sci Technol. 2016;7:360. [Google Scholar]
- 24.Koptyug A, Rännar L, Bäckström M, Fager Franzén S, Dérand P. Additive manufacturing technology applications targeting practical surgery. Int J Life Sci Med Res. 2013;3(1):15–24. doi: 10.5963/LSMR0301003. [DOI] [Google Scholar]
- 25.Heinl P, Müller L, Körner C, Singer RF, Müller FA. Cellular Ti–6Al–4V structures with interconnected macro porosity for bone implants fabricated by selective electron beam melting. Acta Biomater. 2008;4(5):1536–1544. doi: 10.1016/j.actbio.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 26.Renishaw. Case study “Additive manufacturing in veterinary surgery—saving a well-loved member of the family”. http://resources.renishaw.com/en/download/case-study-additive-manufacturing-in-veterinary-surgery-saving-a-well-loved-member-of-the-family--98590.
- 27.Aikman S, McGee J, Meile A, Powell B, Gogard J, Bitter T. “Puppy prosthetic—custom 3D printed dog prosthetic”, P17061. http://edge.rit.edu/edge/P17061/public/Customer%20Handoff%20and%20Final%20Project%20Documentation/MSD_Final_Paper_ver2_4_25_17.pdf.
- 28.Bachman N, Lasso M, Olaode O, Walfield E, Zuhairi MA. Design of a prosthesis for canines with front limb deformities. A Major Qualifying Project Report submitted to the faculty of Worcester Polytechnic Institute in partial fulfillment of the requirements for the degree of Bachelor of Science. 2017. https://web.wpi.edu/Pubs/E-project/Available/E-project-042717-151238/unrestricted/MQPReport.pdf.
- 29.Ruppert DS, Harrysson OLA, Marcellin-Little DJ, Dahners LE, Weinhold PS. Improved osseointegration with as-built electron beam melted textured implants and improved peri-implant bone volume with whole body vibration. Med Eng Phys. 2018 doi: 10.1016/j.medengphy.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 30.ASTM F1472-14, Standard specification for wrought titanium–6aluminum–4vanadium alloy for surgical implant applications (UNS R56400). West Conshohocken: ASTM International; 2014. https://www.astm.org/Standards/F1472.htm.
- 31.ASTM E466 - 07, Standard practice for conducting force controlled constant amplitude axial fatigue tests of metallic materials. https://www.astm.org/DATABASE.CART/HISTORICAL/E466-07.htm.
- 32.ASTM E23 - Standard test methods for notched bar impact testing of metallic materials. https://www.astm.org/Standards/E23.
- 33.Surmeneva MA, Surmenev R, Chudinova EA, Koptioug A, Tkachev MS, Gorodzha SN, Rännar L. Fabrication of multiple-layered gradient cellular metal scaffold via electron beam melting for segmental bone reconstruction. Mater Des. 2017;133:195–204. doi: 10.1016/j.matdes.2017.07.059. [DOI] [Google Scholar]
- 34.Regis M, Marin E, Fedrizzi L, Pressacco M. Additive manufacturing of trabecular titanium orthopedic implants. MRS Bull. 2015;40(02):137–144. doi: 10.1557/mrs.2015.1. [DOI] [Google Scholar]
- 35.Xiong Y, Zhao Y, Wang Z, Du Q, Chen W, Wang A. Comparison of a new minimum contact locking plate and the limited contact dynamic compression plate in an osteoporotic fracture model. Int Orthop. 2009;33(5):1415–1419. doi: 10.1007/s00264-008-0713-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boyer R, Welsch G, Collings EW. Materials properties handbook: titanium alloys. Metals Park: ASM International; 1994. [Google Scholar]
- 37.Metals handbook, volume 2—properties and selection: nonferrous alloys and special-purpose materials, 10th edn. ASM International; 1990.
- 38.Metals handbook, volume 3, properties and selection: stainless steels, tool materials and special-purpose metals, ninth edition, ASM Handbook Committee. Materials Park: American Society for Metals; 1980.
- 39.Holt JM, Ho CY, editors. Structural alloys handbook, 1996 edition. West Lafayette: CINDAS/Purdue University; 1996. [Google Scholar]
- 40.Popov V, Katz-Demyanetz A, Garkun A, Muller G, Strokin E, Rosenson H. Effect of hot isostatic pressure treatment on the electron-beam melted Ti–6Al–4V specimens. Procedia Manuf. 2018;21:125–132. doi: 10.1016/j.promfg.2018.02.102. [DOI] [Google Scholar]
- 41.Popov VV, Jr, Katz-Demyanetz A, Garkun A, Bamberger M. The effect of powder recycling on the mechanical properties and microstructure of electron beam melted Ti–6Al–4V specimens. Addit Manuf. 2018;22:834–843. doi: 10.1016/j.addma.2018.06.003. [DOI] [Google Scholar]