Abstract
Religious Freedom Restoration Acts and sexual minority population health in the United States ABSTRACT: Religious Freedom Restoration Acts (RFRAs) in the United States (US) potentially facilitate discrimination against lesbian, gay, and bisexual individuals (i.e., sexual minorities). This investigation explored whether a population health metric among sexual minority adults changed over time based on the presence, absence, or introduction of a state RFRA. Data are from 21 US states that gathered sexual orientation data from population-based samples of non-institutionalized adults in the 2015 Behavioral Risk Factor Surveillance System. The analytic sample included 4,911 sexual minority individuals. Time was measured in four 3-month quarters (i.e., Q1, Q2, Q3, Q4). For each state, the prevalence of sexual minority adults reporting ≥14 unhealthy days/30 days was calculated. Only Indiana (the only state in the sample that passed a RFRA in 2015) exhibited significant increasing proportions over time of sexual minority adults reporting ≥14 unhealthy days (Q1=24.5%, Q2=34.8%, Q3=41.2%, Q4=59.5%) (ß=0.50, SE=0.23, P=.037). Post hoc analyses revealed that unhealthy days did not increase for heterosexual adults in Indiana. Indiana’s RFRA could have contributed to the increasing prevalence of unhealthy days among sexual minority adults in that state during 2015. Public health surveillance tools are needed to facilitate expeditious analysis of the impact of laws on minority population health.
Keywords: sexual orientation, policy, health equity, public health, discrimination
The National Academy of Medicine issued a consensus report calling for greater attention to health disparities among individuals with minority sexual orientation (i.e., lesbian, gay, and bisexual sexual identity or sexual minority) (Institute of Medicine, 2011). Health disparities have been identified across the spectrum from risk behaviors (e.g., smoking, attempted suicide), to mental and physical conditions (e.g., depression, HIV) (Institute of Medicine, 2011), to nascent research that suggests sexual orientation-based differences in mortality (Cochran, Björkenstam, & Mays, 2016). More recently, investigations have focused on the potent, complex role that toxic social environmental exposures, such as discrimination (Bostwick, Boyd, Hughes, West, & McCabe, 2014), play in the etiology of sexual orientation-based health disparities. Key among these toxic social environmental exposures are laws that directly and indirectly promote discrimination against sexual minority communities.
Fundamental Cause Theory is one framework through which social factors (e.g., stigma, discrimination) are organized as ‘fundamental causes’ of poor health (Link & Phelan, 1995), and scholars continue to identify mechanisms by which social determinants affect biological health (Hatzenbuehler, Phelan, & Link, 2013). For example, Hatzenbuehler, Keyes, and Hasin (2009) found that sexual minorities who lived in states without hate crime or employment discrimination protections had over 4 times the odds of a comorbid psychiatric disorder than participants living in states with these protections. Additionally, before same-sex marriage was legalized throughout the U.S. in 2015, Hatzenbuehler et al. examined longitudinal data from the National Epidemiologic Survey on Alcohol and Related Conditions before and after state constitutional amendments prohibiting same-sex marriage in 16 states (Hatzenbuehler, McLaughlin, Keyes, & Hasin, 2010). The authors found that sexual minorities in states where these amendments passed experienced significant increases in mood, anxiety, and alcohol use disorders, whereas sexual minorities in states without these amendments did not have significant increases in psychiatric disorders. Although these previous studies established the importance of socio-political stressors on sexual minority health, research in this area has not considered whether Religious Freedom Restoration Acts (RFRAs) may be similarly detrimental to sexual minority health.
Congress enacted the federal RFRA in 1993 in response to a series of Supreme Court decisions that did not apply a standard of strict scrutiny in religious liberty cases (Chemerinsky, 1997; Katz, 2015). Although cases regarding the freedom of religious practice typically were examined under the strict scrutiny standard, the Court was increasingly opting not to employ this standard for rules of “general applicability,” meaning laws that are applied the same way to all citizens, regardless of their religious beliefs, with no exceptions or exemptions. The purpose of the federal RFRA was to restore strict scrutiny as the standard for judicial review, with the goal of sensitizing government officials to the ways that the uniform enforcement of laws sometimes burdens private citizens’ exercise of religion. Under the federal RFRA, government needed to provide a compelling interest in order to burden religious exercise, even for rules of general applicability.
In 1997, the Supreme Court ruling in City of Boerne v. Flores declared the federal RFRA an unconstitutional extension of Congressional authority over the states, in violation of the 14th Amendment. The decision was perceived as judicial activism and a major detriment to efforts at reducing burdens on religious freedom (Chemerinsky, 1997), and it spurred many state legislatures to pursue their own version of the law (Hamilton, 2015). Currently 21 states have RFRAs (National Conference of State Legislatures, 2015), and there is significant variation in the character of the laws across states. Some states have included civil rights protections, ensuring that RFRAs cannot be invoked to justify discriminatory treatment, but others passed versions that expanded provisions for religious liberty (Hamilton, 2015), which can pose a significant challenge to sexual minority civil rights.
Legal scholars have argued that the ambiguity and broad scope of RFRAs create a significant potential for harm to sexual minorities (Griffin, 2015; Hamilton, 2015). For instance, businesses have invoked a RFRA in the courts to challenge public accommodation laws based on sexual orientation and to justify discrimination against lesbian, gay or bisexual customers (“Elane Photography, LLC v. Willock,” 2013; Guo, 2015). Thus in the absence of explicit civil protections for sexual minority status, RFRAs pose a threat to equal protection and the civil rights of sexual minority Americans (Hamilton, 2015). Consequently, RFRAs may be associated with sexual minority health in a similar manner observed in previous research about discriminatory legislation and sexual minority health.
Because sexual orientation is not yet collected systematically on most federal health surveys, there are few, if any, datasets in the US that facilitate examining the potential impact of policies and laws on sexual minority health (Sell & Holliday, 2014). In the rare instances that sexual orientation data are included, the sample size of sexual minority individuals tends to be small, limiting statistical power. Furthermore, sexual orientation questions on federal health surveys are recent additions, resulting in a limited number of time periods for trend analyses. However, the recent addition of sexual orientation measures in an optional module of the Behavioral Risk Factor Surveillance System (BRFSS) presents a cursory opportunity because it is the largest survey conducted in the US and data can be examined by month over the course of a survey year. Thus, these data facilitated an exploratory analysis of whether a population health indicator (i.e., the CDC’s measure of healthy days (Moriarty, Zack, & Kobau, 2003)) among sexual minority individuals increased or decreased during 2015 based on the RFRA status of the states in which they resided.
METHOD
Data
Conducted by the Centers for Disease Control and Prevention (CDC), the BRFSS is the largest ongoing survey in the US, gathering annual cross-sectional data from probability-based samples of non-institutionalized adults over the age of 18 throughout the calendar year (Centers for Disease Control and Prevention, 2016). This project was approved by the institutional review board of the VA Pittsburgh Healthcare System; Protocol 880 “Behavioral Risk Factor Surveillance System (BRFSS) and health disparities”
Each US state and territory administers a standardized core survey, which they can supplement with optional modules. In 2015, 21 states elected to administer the Sexual Orientation and Gender Identity module (see Table 1 for a list of states). The survey response rates for the 21 states ranged from 34.4% for Texas to 57.6% for Ohio, resulting in a median response rate was 45.0% (the overall BRFSS median response rate was 47.2%) (Centers for Disease Control and Prevention, 2015). The survey is administered through computer-assisted telephone interviews, and participants are selected through disproportionate stratified sample design for landline phone samples and random sample design for cellular phone samples. The BRFSS data and detailed information about the survey and methodology are publicly accessible through the CDC (Centers for Disease Control and Prevention, 2015). BRFSS data are not longitudinal (i.e., no repeated measures), however it is possible to examine the data in a serial cross-sectional manner because the CDC provides data about the month in which each respondent was interviewed.
Table 1.
Proportions of sexual minority adults having ≥14 unhealthy days/30 days among states that collected sexual orientation data in the 2015 BRFSS, by Religious Freedom Restoration Act (RFRA) status in 2015
| Time (3-month quarters) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |||||||||
| No. | % | (SE) | No. | % | (SE) | No. | % | (SE) | No. | % | (SE) | |
|
|
||||||||||||
| RFRA prior to 2015 | 456 | 29.5 | (3.7) | 420 | 23.1 | (3.5) | 463 | 28.4 | (4.2) | 537 | 35.4 | (3.8) |
| Connecticut | 64 | 47.7 | (9.7) | 46 | 28.6 | (12.2) | 120 | 28.2 | (6.4) | 115 | 26.5 | (5.1) |
| Idaho | 19 | 13.2 | (6.5) | 27 | 38.9 | (12.7) | 18 | 36.0 | (17.8) | 27 | 20.2 | (8.5) |
| Illinois | 38 | 28.8 | (9.7) | 43 | 12.8 | (5.8) | 29 | 36.4 | (12.5) | 41 | 22.5 | (7.0) |
| Kansas | 97 | 22.4 | (5.8) | 114 | 33.9 | (5.5) | 120 | 33.7 | (5.6) | 120 | 33.0 | (5.4) |
| Missouri | 50 | 26.2 | (9.6) | 31 | 39.2 | (13.3) | 35 | 16.1 | (7.2) | 55 | 57.4 | (11.1) |
| Pennsylvania | 62 | 34.4 | (7.5) | 39 | 34.7 | (11.7) | 23 | 18.9 | (9.3) | 24 | 61.9 | (12.6) |
| Virginia | 49 | 35.1 | (9.5) | 56 | 15.0 | (5.6) | 40 | 24.5 | (10.2) | 55 | 37.3 | (9.1) |
| Texas | 77 | 22.5 | (7.9) | 64 | 22.3 | (6.4) | 78 | 29.4 | (8.1) | 100 | 28.4 | (7.0) |
| No RFRA in 2015 | 704 | 28.0 | (2.9) | 593 | 29.5 | (3.3) | 405 | 32.7 | (4.2) | 342 | 31.5 | (4.4) |
| Delaware | 44 | 40.2 | (9.6) | 27 | 21.0 | (11.9) | 44 | 55.5 | (10.9) | 37 | 23.6 | (7.9) |
| Maryland* | 59 | 25.1 | (12.6) | 67 | 27.8 | (14.1) | 60 | 30.9 | (12.7) | 57 | 41.0 | (11.9) |
| Massachusetts | 144 | 21.5 | (4.3) | 75 | 29.4 | (7.1) | 74 | 31.6 | (8.2) | 63 | 30.4 | (8.0) |
| Minnesota | 167 | 37.7 | (4.7) | 189 | 32.8 | (4.9) | 64 | 21.7 | (6.0) | 36 | 35.6 | (10.3) |
| New York | 177 | 29.5 | (4.6) | 85 | 19.7 | (6.1) | 55 | 36.2 | (9.0) | 69 | 36.5 | (8.8) |
| Ohio | 70 | 25.9 | (10.8) | 80 | 49.7 | (9.1) | 58 | 29.8 | (11.1) | 58 | 24.5 | (8.9) |
| Wisconsin | 43 | 21.8 | (6.9) | 70 | 27.9 | (7.4) | 50 | 30.1 | (9.7) | 22 | 14.2 | (9.8) |
| RFRA introduced in 2015 | 227 | 31.1 | (6.6) | 229 | 37.1 | (5.9) | 264 | 30.0 | (5.3) | 271 | 47.4 | (6.1) |
| Colorado | 65 | 25.3 | (6.4) | 83 | 43.7 | (8.9) | 84 | 21.1 | (6.2) | 101 | 38.8 | (8.7) |
| Georgia | 18 | 39.2 | (16.9) | 23 | 29.6 | (12.8) | 33 | 23.8 | (10.4) | 19 | 50.8 | (13.7) |
| Hawaii | 50 | 27.0 | (10.0) | 69 | 24.7 | (7.9) | 78 | 25.5 | (7.6) | 47 | 28.1 | (9.2) |
| Indiana1* | 35 | 24.5 | (11.1) | 19 | 34.8 | (16.2) | 25 | 41.2 | (13.9) | 39 | 59.5 | (11.9) |
| Nevada | 29 | 29.1 | (12.5) | 16 | 51.9 | (12.0) | 24 | 43.4 | (13.5) | 25 | 38.6 | (15.6) |
| West Virginia | 30 | 40.8 | (10.5) | 19 | 58.2 | (12.6) | 20 | 48.0 | (14.0) | 40 | 43.2 | (9.5) |
| Overall (excluding Indiana) | 1,352 | 29.1 | (2.2) | 1,223 | 27.8 | (2.3) | 1,107 | 29.8 | (2.6) | 1,111 | 35.3 | (2.6) |
Note: Frequencies are unweighted; percentages and standard errors are weighted; Q1=January, February, March; Q2=April, May, June;
Q3=July, August, September; Q4=October, November, December; data were collected in the United States from January 1, 2015 through December 31, 2015.
=passed RFRA in 2015
=increasing prevalence across the year
Variables
Within the Sexual Orientation and Gender Identity module, respondents are asked, “Do you consider yourself to be: 1-straight, 2-lesbian or gay, 3-bisexual.” Respondents could indicate “other,” and, for the purposes of this study, these respondents were classified as sexual minority.
A three-category variable was created to classify states by whether they (1) had RFRAs in place prior to 2015, (2) had no RFRAs in place (and did not introduce RFRAs) in 2015, or (3) introduced or passed RFRAs in 2015. Among the 21 states included in the present analysis, eight states had RFRAs in place prior to 2015, seven had no RFRAs (and did not introduce RFRAs) in 2015, and six states introduced a RFRA in their state legislatures in 2015. Of these six states, Indiana was the only state to pass a RFRA on March 26, 2015 (National Conference of State Legislatures, 2015).
Time was measured by the month in which respondents completed the survey in 2015. However, because of small monthly totals of sexual minority individuals within some states, time was aggregated into four 3-month quarters (e.g., quarter 1 = January, February, March).
The criterion variable of interest was the CDC-calculated measure of unhealthy days (Moriarty et al., 2003), which is comprised of two BRFSS core survey questions: “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?” and “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” The respondent answered each question with a number from 0-30. The responses to both items are added together with a ceiling of 30 days (Moriarty et al., 2003). The unhealthy days measure has been shown to be a reliable and valid measure of population health-related quality of life (Andresen, Catlin, Wyrwich, & Jackson-Thompson, 2003; Barile et al., 2016; Jia, Lubetkin, Moriarty, & Zack, 2007). Because the variable tends to be non-normally distributed (as it was in the present study; kurtosis=3.87), we followed previous research that dichotomized the measure to ≥14 unhealthy days/30 days vs. <14 days (D. R. Brown, Carroll, Workman, Carlson, & Brown, 2014; D. W. Brown et al., 2004; Ford, Moriarty, Zack, Mokdad, & Chapman, 2001).
Analyses
First, the proportion of sexual minority individuals reporting ≥14 unhealthy days/30 days were calculated and plotted by quarter for each state and for the 3 categories of RFRA states. Next, for any state that showed a consistent increasing prevalence in the proportion of sexual minority individuals reporting ≥14 unhealthy days/30 days over the year (i.e., prevalence increased in all four quarters), a logistic regression model was used to test the association of time with the criterion variable (i.e., testing whether the increase over time was significant). All analyses were conducted using Stata/SE Version 13, and all estimates, standard errors, and confidence intervals were weighted to account for stratification, clustering, and weighting in the complex sampling design of the BRFSS. The Institutional Review Board of [institution name masked for review] approved this secondary data analysis.
RESULTS
Across the 21 states that used the Sexual Orientation and Gender Identity module, 166,997 respondents answered the sexual orientation question. Because this study is focused solely on sexual minority populations, persons who indicated “heterosexual” (n=157,199), “don’t know” (n=1,759), or who refused to answer (n=2,951) were excluded from a priori analyses. We also excluded 177 participants who did not answer one or both of the two measures necessary for the composite unhealthy days variable. Our analytic sample contained 4,911 sexual-minority adults: 2,192 gay/lesbian individuals, 2,189 bisexual individuals, and 530 individuals who indicated “other” sexual orientation.
Among the three categories of states (i.e., had a RFRA in place prior to 2015, had no RFRA in place in 2015, and introduced a RFRA in 2015), no consistent increasing pattern was observed of proportions of sexual minority individuals reporting ≥14 unhealthy days/30 days over the year (Table 1 and 2). Among individual states, Maryland and Indiana exhibited increasing proportions over the year of sexual minority adults reporting ≥14 unhealthy days/30 days. Regressing the proportion of sexual minority individuals reporting ≥14 unhealthy days/30 days on time for Maryland did not show a significant increase (ß=0.13, SE=0.25, P=.617), however for Indiana, there was a significant increase over time in the proportion of sexual minorities reporting ≥14 unhealthy days/30 days (ß=0.50, SE=0.23, P=.037) (Table 2). Because only two statistical tests for significance needed to be conducted (i.e., one for Maryland and one for Indiana), the <.05 p-value for statistical significance was not adjusted for multiple testing.
Table 2.
Association of time with proportion of adults reporting ≥14 unhealthy days/30 days in 2015
| States by Religious Freedom Restoration Act (RFRA) status | Time1 | ||
|---|---|---|---|
| ß | (SE) | P | |
|
|
|||
| Without RFRAs (n=2,044) | 0.07 | (.07) | .354 |
| With RFRAs (n=1.876) | 0.11 | (.08) | .189 |
| Introduced RFRAs (n=991) | 0.19 | (.12) | .117 |
| Individual states | |||
| Sexual minority adults in Indiana (n=118) | 0.50 | (0.23) | .037 |
| Sexual minority adults in Maryland (n=94) | 0.13 | (0.25) | .617 |
Note: all analyses are weighted;
= time defined as four 3-month quarters across 2015; data were collected in the United States from January 1, 2015 through December 31, 2015.
Because Indiana was the only state with a statistically significant increase in the proportion of sexual minority individuals reporting ≥14 unhealthy days/30 days over the year, two post hoc analyses were conducted to specifically compare heterosexual and sexual minority Indianans. First, there was no significant increase over time in the proportion of heterosexual Indianans reporting ≥14 unhealthy days/30 days (ß=0.02, SE=0.05, P=.727) (data not shown). Second, a logistic regression model showed that there was a significant interaction between sexual minority status and time in reporting ≥14 unhealthy days/30 days in the fourth quarter of 2015 (ß=1.48, SE=0.75, P=.048) in contrast to the interaction of sexual minority adults and time in the first quarter of 2015 (referent) (Table 3). Interactions between sexual identity and time for the second or third quarters of 2015 were not significant. Plots of the proportions and 95% confidence intervals of heterosexual and sexual minority adults in Indiana reporting ≥14 unhealthy days/30 days showed a clear divergence at the Quarter 4 time point (Figure 1).
Table 3.
Post hoc analysis of interaction between sexual orientation and time among adults in Indiana reporting ≥14 unhealthy days/30 days in 2015
| ≥14 unhealthy days/30 days (n=4,850) | ||||
|---|---|---|---|---|
| Independent Variables | ß | (SE) | P | |
|
|
||||
| Time | ||||
| Quarter 1 | Ref | - | ||
| Quarter 2 | -0.05 | (0.15) | .732 | |
| Quarter 3 | 0.02 | (0.15) | .878 | |
| Quarter 4 | 0.03 | (0.14) | .830 | |
| Sexual identity | ||||
| Heterosexual | Ref | - | ||
| Sexual minority | 0.18 | (0.52) | .724 | |
| Interaction | ||||
| Sexual identity × Q1 | Ref | - | ||
| Sexual identity × Q2 | 0.55 | (0.90) | .542 | |
| Sexual identity × Q3 | 0.75 | (0.78) | .343 | |
| Sexual identity × Q4 | 1.48 | (0.75) | .048 | |
Data were collected in the United States from January 1, 2015 through December 31, 2015.
Figure 1.
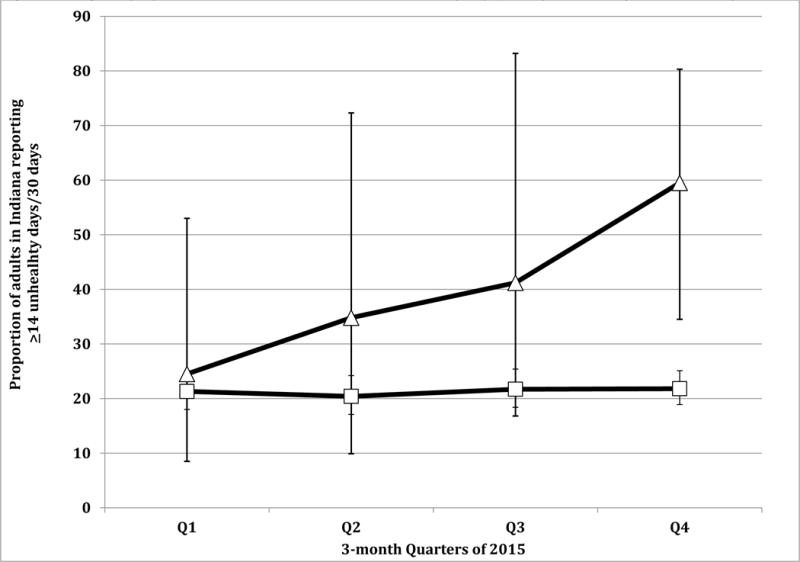
Weighted proportion of adults in Indiana with ≥14 unhealthy days/30 days in 2015, by sexual minority status
Δ=Indiana Sexual Minority; □=Indiana Heterosexual
DISCUSSION
Though previous studies have examine other policies and sexual minority health, principally same-sex marriage bans ((Hatzenbuehler et al., 2013), this analysis is one of the few to examine RFRAs. The results suggest that, among the 21 states for which sexual orientation data were available, Indiana was the only state with a significant increase in the proportion of sexual minority adults reporting ≥14 unhealthy days/30 days during 2015. This finding is remarkable in that it was detected even with hampered statistical power due to the relatively small sample of sexual minority adults in Indiana (n=119). Increases in the proportion of sexual minority adults reporting ≥14 unhealthy days/30 days were not observed in the groups of states that had RFRAs prior to 2015, states that did not have RFRAs in 2015, or even amongst other states that introduced (but did not enact) RFRAs in 2015.
There are several possible explanations for the results observed for Indiana. First, consistent with previous research showing associations between discriminatory laws and sexual minority health (Hatzenbuehler et al., 2009; Hatzenbuehler et al., 2010), it is possible that the RFRA may have contributed to sexual minorities’ poor self-rated health in Indiana. Indiana’s RFRA law (Senate Bill 101) was signed into law by then Governor Mike Pence on March 26, 2015 (i.e., within Quarter 1 of the present analysis), precipitating the steady increases in prevalence at each subsequent quarter.
Moreover, Indiana’s RFRA is qualitatively different from the federal RFRA and RFRAs passed previously in other states. In most states, RFRAs do not apply in litigation in which a government agency is not a party, meaning it cannot be invoked in disputes between private parties or between citizens and corporations. Indiana’s RFRA uses a broad and ambiguous definition of government entity that includes private parties acting under the color of law (Katz 2015). This means a RFRA defense can be used in private litigation, including cases where businesses wish to refuse services to members of the LGBT community. Legal scholars contend that the law will ultimately make it harder for parties in private litigation to win lawsuits that would result in any burden to the opposing party’s ability to exercise their religion (Griffin, 2015; Hamilton, 2015). It also enables to courts to grant compensatory damages and attorneys’ fees against the person or entity bringing the suit, meaning the risk of losing the suit may be prohibitively high for private parties (Katz, 2015). For these reasons, opponents of the bill have described it as providing a “license to discriminate”(Petri, 2015).
Consequently, these aspects of the Indiana’s RFRA law likely contributed to perceived discrimination among LGB individuals that was unique to Indiana. We did not observe a pattern of increasing unhealthy days among sexual minority residents of states that already had RFRA laws. We caution against drawing the conclusion that these other RFRA laws do no harm. RFRAs are interpreted on a case-by-case basis by the state courts, and many states have modified the standards of scrutiny applied to cases involving religious liberties through court decisions rather than making modifications directly to RFRA legislation (Hamilton, 2015). Thus, the absence of a RFRA does not necessarily imply a favorable legal climate for sexual minority individuals. Consequently, there is heterogeneity among states, RFRAs, and climate toward sexual and gender minority status that is unaccounted for in the present study, and further research is needed to operationalize these complexities to better explore ramifications of RFRAs on minority health.
A related explanation for the findings is that the media blitz surrounding Indiana’s RFRA heightened the salience of the threat it posed to sexual minority residents (Barbaro & Eckholm, 2015; Jones & Peters, 2015). For example, the executive editor for the Indianapolis Star stated publicly that the newspaper aggressively pushed back against RFRA in unprecedented kinds of ways (e.g. a front-page editorial), and the state governor wrote an editorial in the Wall Street Journal to defend the law (Pence, 2015). Moreover, opposition to the bill was organized relatively late (i.e., the bill had already passed the state legislature), though it was effective in forcing clarification preventing the RFRA from being used to discriminate based on sexual orientation (Davey, Robertson, & Perez-Pena, 2015). However, based on the results of the present study, one hypothesis is that the damage was already set in motion and persistently amplified by continual media coverage over the course of 2015. Further research is needed to develop nuanced measures of media exposure to political issues as a way of exploring potential meditational effects of how laws may impact minority health (Cassese & Hannagan, 2015; Flores, Hatzenbuehler, & Gates, 2018; Frost & Fingerhut, 2016; Maisel & Fingerhut, 2011).
The findings should be viewed in light of several limitations. Only 21 states included sexual orientation data in 2015, making it unclear whether similar trajectories of unhealthy days may have existed among sexual minority adults in other states. Arkansas was the only other state to pass a RFRA in 2015 (National Conference of State Legislatures, 2015), and it did not collect sexual orientation data in its 2015 BRFSS survey. Despite being a relatively large aggregate sample of sexual minority individuals, in some states there were small samples in each quarter, which reduced precision of estimates. We included those who responded “other” to sexual orientation as sexual minorities. Although we cannot know exactly how these respondents identify, literature suggests irrespective of sexual orientation, it is the inability to claim heterosexuality and its corresponding social privilege that can make persons vulnerable to health disparities (Matthews, Blosnich, Farmer, & Adams, 2014). Additionally, due to sample size limitations, transgender-specific analyses were not possible. Although the data show increases over time, the results cannot determine causality because there were no longitudinal data on individuals before vs. after the RFRA. Furthermore, sexual orientation data in the BRFSS are not available for all of these states for years prior to 2015, making it impossible to gauge whether the patterns observed in 2015 were unique (e.g., inability to assess seasonality). Lastly, the sample was restricted to adults, and it is unclear whether similar patterns would be observed among sexual minority youth in Indiana.
The findings seem to align with prior research showing important associations between laws and policies and sexual minority population health (Hatzenbuehler et al., 2009; Hatzenbuehler et al., 2010). Feminist essayist Carol Hanisch is often credited with the statement “the personal is political”(Hanisch, 2000); apt words for sexual minority communities. Laws may intentionally or inadvertently give rise to minority health disparities or become the scaffolding by which disparities are upheld or amplified. Public health needs better, expeditious surveillance tools with which to gauge potential impacts of laws on minority population health. This is especially pertinent as religious-related issues related to sexual minorities continue to unfold in the US, (e.g., Masterpiece Cakeshop v. Colorado Civil Rights Commission) (Barnes & Marimow, 2017; Pierson & Wolfe, 2018).
PUBLIC POLICY RELEVANCE.
Legal scholars posit that religious freedom restoration acts (RFRAs) create a significant potential for discrimination against sexual minorities, which provides the scaffolding to uphold sexual minority health disparities. Taking advantage of a natural experimental phenomenon, the present results suggest the passage of a religious freedom restoration act in the U.S. state of Indiana in March 2015 may have been associated with increased poor self-reported overall health among sexual minorities in Indiana.
Acknowledgments
The authors thank J. Dan Harding at the Center for Health Equity and Promotion for his assistance in creating the graphs. This work was partially supported by a Career Development Award (CDA 14-408) to JRB from the Department of Veterans Affairs, Health Service Research & Development, by a pre-doctoral research award to RWSC from the National Institute on Drug Abuse (F31DA037647). The authors thank the Centers for Disease Control and Prevention for making the BRFSS data publicly available. The opinions expressed in this work are those of the authors and do not necessarily reflect those of the funders, institutions, the Department of Veterans Affairs, or The U.S. Government.
Footnotes
Conflict of interest: The authors have no conflicting interests to disclose.
References
- Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. Journal of Epidemiology and Community Health. 2003;57(5):339–343. doi: 10.1136/jech.57.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbaro M, Eckholm E. Indiana law denounced as invitation to discriminate against gays. 2015 Retrieved from http://www.nytimes.com/2015/03/28/us/politics/indiana-law-denounced-as-invitation-to-discriminate-against-gays.html.
- Barile JP, Horner-Johnson W, Krahn G, Zack M, Miranda D, DeMichele K, Thompson WW. Measurement characteristics for two health-related quality of life measures in older adults: The SF-36 and the CDC Healthy Days items. Disability and health journal. 2016 doi: 10.1016/j.dhjo.2016.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes R, Marimow AE. Supreme Court seems divided in case of baker who refused to create a wedding cake for a same-sex couple. Washington Post. 2017 Retrieved from https://www.washingtonpost.com/politics/courts_law/supreme-court-asked-if-wedding-cake-bakers-case-protects-religious-freedom-or-illegal-discrimination/2017/12/05/c73e6efa-d969-11e7-a841-2066faf731ef_story.html?noredirect=on&utm_term=.ab411989fcea.
- Bostwick WB, Boyd CJ, Hughes TL, West BT, McCabe SE. Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. American Journal of Orthopsychiatry. 2014;84(1):35. doi: 10.1037/h0098851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DR, Carroll DD, Workman LM, Carlson SA, Brown DW. Physical activity and health-related quality of life: US adults with and without limitations. Quality of life research. 2014;23(10):2673–2680. doi: 10.1007/s11136-014-0739-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DW, Balluz LS, Giles WH, Beckles GL, Moriarty DG, Ford ES, Mokdad AH. Diabetes mellitus and health-related quality of life among older adults: Findings from the behavioral risk factor surveillance system (BRFSS) Diabetes research and clinical practice. 2004;65(2):105–115. doi: 10.1016/j.diabres.2003.11.014. [DOI] [PubMed] [Google Scholar]
- Cassese EC, Hannagan R. Framing and Women’s Support for Government Spending on Breast Cancer Research and Treatment Programs. Analyses of Social Issues and Public Policy. 2015;15(1):69–88. [Google Scholar]
- Centers for Disease Control and Prevention. BRFSS: 2015 summary data quality report. 2015 Retrieved from http://www.cdc.gov/brfss/annual_data/2015/pdf/2015-sdqr.pdf.
- Centers for Disease Control and Prevention. BRFSS: Comparability of Data 2015. 2016 Retrieved from http://www.cdc.gov/brfss/annual_data/2015/pdf/compare_2015.pdf.
- Chemerinsky E. The Religious Freedom Restoration Act Is a Constitutional Expansion of Rights. Wm & Mary L Rev. 1997;39:601. [Google Scholar]
- Cochran SD, Björkenstam C, Mays VM. Sexual Orientation and All-Cause Mortality Among US Adults Aged 18 to 59 Years, 2001–2011. American journal of public health. 2016;106(5):918–920. doi: 10.2105/AJPH.2016.303052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey M, Robertson C, Perez-Pena R. After rights clash, two states revise legislation. The New York Times. 2015:A12. [Google Scholar]
- Elane Photography, LLC v Willock. NM: Supreme Court; 2013. No. No. 33,687, 309 53. [Google Scholar]
- Flores AR, Hatzenbuehler ML, Gates GJ. Identifying psychological responses of stigmatized groups to referendums. Proceedings of the National Academy of Sciences. 2018 doi: 10.1073/pnas.1712897115. 201712897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES, Moriarty DG, Zack MM, Mokdad AH, Chapman DP. Self-Reported Body Mass Index and Health-Related Quality of Life: Findings from the Behavioral Risk Factor Surveillance System. Obesity Research. 2001;9(1):21–31. doi: 10.1038/oby.2001.4. [DOI] [PubMed] [Google Scholar]
- Frost DM, Fingerhut AW. Daily exposure to negative campaign messages decreases same-sex couples’ psychological and relational well-being. Group Processes & Intergroup Relations. 2016;19(4):477–492. [Google Scholar]
- Griffin LC. A Word of Warning from a Woman: Arbitrary, Categorical, and Hidden Religious Exemptions Threaten LGBT Rights. Alabama Civil Rights and Civil Liberties Law Review. 2015;7:97. [Google Scholar]
- Guo J. Here’s how to use religious freedom laws to fend off a gay discrimination suit. The Washington Post 2015 [Google Scholar]
- Hamilton MA. The case for evidence-based free exercise accomodation: Why the Religious Freedom Restoration Act is bad public policy. Harvard Law & Policy Review. 2015;9:129–160. [Google Scholar]
- Hanisch C. The personal is political. In: Crow BA, editor. Radical feminism: A documentary reader. New York, NY: New York University Press; 2000. pp. 113–116. [Google Scholar]
- Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. American journal of public health. 2009;99(12):2275–2281. doi: 10.2105/AJPH.2008.153510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: A prospective study. American journal of public health. 2010;100(3):452–459. doi: 10.2105/AJPH.2009.168815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American journal of public health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Jia H, Lubetkin EI, Moriarty DG, Zack MM. A comparison of healthy days and EuroQol EQ-5D measures in two US adult samples. Applied Research in Quality of Life. 2007;2(3):209–221. [Google Scholar]
- Jones A, Peters M. Indiana governor wants to clarify religious freedom law. 2015 Retrieved from http://www.wsj.com/articles/indiana-governor-wants-to-clarify-religious-freedom-law-1427817080.
- Katz R. Indiana’s Flawed Religious Freedom Law. Ind L Rev. 2015;49:37. [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Maisel NC, Fingerhut AW. California’s ban on same-sex marriage: The campaign and its effects on gay, lesbian, and bisexual individuals. Journal of Social issues. 2011;67(2):242–263. [Google Scholar]
- Matthews DD, Blosnich JR, Farmer GW, Adams BJ. Operational definitions of sexual orientation and estimates of adolescent health risk behaviors. LGBT health. 2014;1(1):42–49. doi: 10.1089/lgbt.2013.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures–Population tracking of perceived physical and mental health over time. Health and quality of life outcomes. 2003;1(1):1. doi: 10.1186/1477-7525-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Conference of State Legislatures. 2015 state religious freedom restoration legislation. 2015 Retrieved from http://www.ncsl.org/research/civil-and-criminal-justice/2015-state-rfra-legislation.aspx.
- Pence M. Ensuring religious freedom in Indiana. Wall Street Journal. 2015 Retrieved from http://www.wsj.com/articles/mike-pence-ensuring-religious-freedom-in-indiana-1427757799.
- Petri A. License to discriminate? The Washington Post. 2015 Retrieved from https://www.washingtonpost.com/blogs/compost/wp/2015/03/30/license-to-discriminate/?utm_term=.1421c70f2a2b.
- Pierson B, Wolfe J. Trump move on healthcare religious freedom prompts discrimination fears. 2018 Retrieved from https://www.reuters.com/article/us-usa-healthcare-religion-legal/trump-move-on-healthcare-religious-freedom-prompts-discrimination-fears-idUSKBN1F800L.
- Sell RL, Holliday ML. Sexual orientation data collection policy in the United States: public health malpractice. American journal of public health. 2014;104(6):967–969. doi: 10.2105/AJPH.2013.301814. [DOI] [PMC free article] [PubMed] [Google Scholar]


