Introduction
An extra-uterine abdominal pregnancy is a very rare form of ectopic pregnancy where implantation occurs within the peritoneal cavity excluding ovary, fallopian tube and broad ligament. It is estimated to occur in 1 out of 10,000 to 30,000 pregnancies [1, 2]. Despite the use of routine antenatal ultrasound, its diagnosis is frequently missed [3]. However, it is extremely important to detect an extra-uterine abdominal pregnancy because the associated maternal mortality rate is 5 out of 1000 cases which is approximately seven times higher than ectopic pregnancy and about 90 times higher than intrauterine pregnancy. The site of implantation and availability of vascular supply are believed to be factors that may influence the possibility of fetal survival. Advanced abdominal pregnancy carries a risk of hemorrhage, disseminated intravascular coagulation, bowel obstruction and fistula formation. Survival of new born is also affected with a perinatal mortality rate of 40–95%.
Case Report
A 20 year old patient was admitted to emergency room at our tertiary care hospital with complaints of 9-month amenorrhea, pain abdomen and bleeding per vagina since morning. Patient was a primigravida who was referred from primary health center for oblique presentation. Patient was admitted around 12.30 am midnight.
On examination her general condition was good. Her pulse was 98 beats per min, BP—100/70 mm of Hg Patient did not know her LMP, and her menstrual history was not significant. She had past history of vague dull pain abdomen. On per abdomen examination uterine height was 36 weeks, lie was oblique head was on maternal left side and fetal heart rate was irregular (106 beats per minute). On per vaginal examination cervix was one finger dilated, uneffaced, midline in position and medium consistency, presenting part could not made out, pelvis was adequate. All the blood and urine investigations were within normal limit. Her last USG showed single live fetus of 32 weeks, in oblique lie with head on maternal left side, fundo-anterior placenta and adequate liquor. This USG corresponded to current gestational age of 37 weeks and 1 day.
Due to oblique lie and irregular fetal heart rate, decision of emergency LSCS was taken. Blood was sent for grouping and cross-matching before the patient was taken to operation theater with written and informed consent. Patient was given spinal anesthesia, and self-retaining catheter was inserted. After opening the abdomen, amniotic sac was seen protruding in peritoneal cavity.
Membrane was ruptured and baby male child of 2.45 kg was delivered as breech and handed over to Pediatrician.
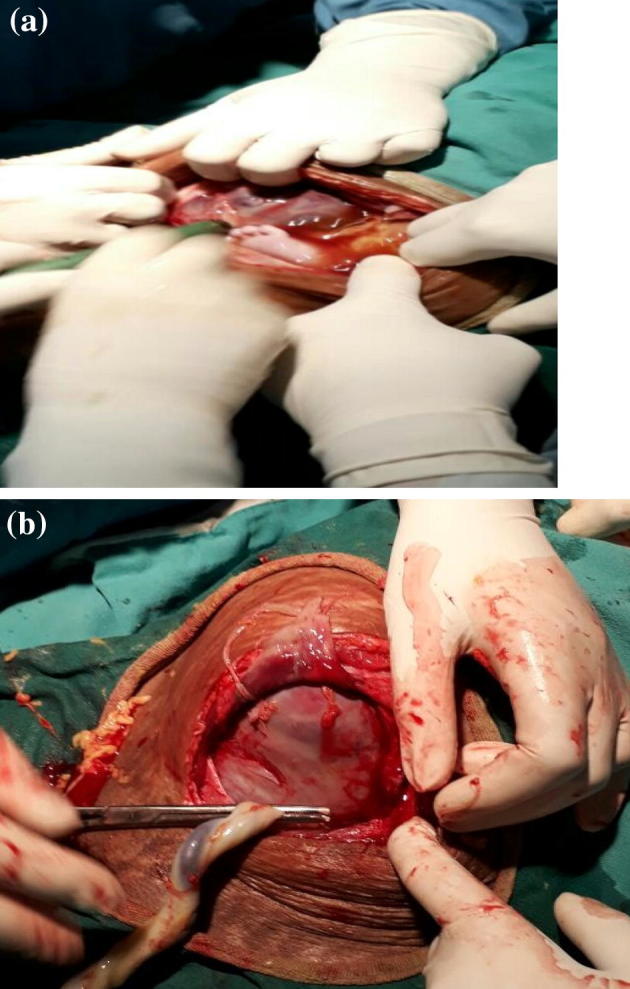
a Fetus in abdominal cavity after opening amniotic sac. b Placenta adherent on vital organs
There was profuse hemorrhage just after delivery of baby. After exploration, placenta was found adherent to omentum and intestine. Fortunately, senior gynecologist and senior surgeon were present in nearby operation theater attending another case. They immediately joined the case. Demand of blood products was sent to blood bank. Placenta was separated from omentum and intestine as much as possible by surgeon and hemostasis achieved by application of multiple hemostatic sutures. Pelvis was explored, uterus was 6–8 weeks size and intact, and placenta was originating from junction of isthmus and ampullary portion of right fallopian tube. Left side tube and both ovaries were healthy. Intra-operative 2 unit packed cell were transfused. Drain was inserted and abdomen was closed. Patient withstood the procedure well. Patient and healthy baby were discharged at day 10 postoperatively.

Healthy baby at the time of delivery
Discussion
Extra-uterine abdominal pregnancy beyond second trimester with a viable fetus is an extremely rare condition.
It is classified into two types. Primary abdominal pregnancy refers to pregnancy where implantation of the fertilized ovum occurs directly in the abdominal cavity. In such cases, the fallopian tubes and ovaries are intact. There were only 24 cases of primary abdominal pregnancy reported up to 2007 [4]. In contrast, secondary abdominal pregnancy accounts for most cases of advanced extra-uterine pregnancy. It occurs following an extra-uterine tubal pregnancy that ruptures or aborts and gets re-implanted within the abdomen. Patients with an extra-uterine abdominal pregnancy typically have persistent abdominal and/or gastrointestinal symptoms during their pregnancy. Diagnosis of this condition is frequently missed, with only about 45% of cases diagnosed during the antenatal period. In our case, diagnosis was missed and misinterpretated as intrauterine pregnancy [5]. Ultrasonography remains the main method for the diagnosis of extra-uterine pregnancy. It usually shows no uterine wall surrounding the fetus, fetal parts that are very close to the abdominal wall, abnormal lie and no or decreased amniotic fluid between the placenta and the fetus [6].
Magnetic resonance imaging and serum a-fetoprotein have been used to diagnose abdominal pregnancy [7, 8]. However, there was no justification to perform these tests in our patient as the diagnosis was not suspected. In poor resourced centers, high index of suspicion is the key for prompt diagnosis and timely intervention to prevent life-threatening complications.
About 21% of babies born after an extra-uterine abdominal pregnancy have birth defects [9], presumably due to compression of the fetus in the absence of the amniotic fluid buffer. Typical deformities include limb defects, facial and cranial asymmetry, joint abnormalities and central nervous malformation. In this case, the baby was protected by the surrounding amniotic fluid and sac which could explain the absence of deformities in the baby. The massive bleeding that occurred from detached part of placenta was due to the adherence of the placenta to the abdominal viscera which, unlike the uterus, does not contract. It has been reported that, unless the placenta can be easily tied off or removed, it may be preferable to leave it in place and allow its natural regression. In our opinion, bleeding from placental implantation site is the most life-threatening complication during laparotomy. The decision to remove the placenta or not can be a determining factor for the survival or otherwise of the woman and this decision is subject to the surgeon’s expertise and the particular case in question. It is generally recommended to leave the placenta in situ and follow-up with USG and human chorionic gonadotropin levels. In this case, there was significant bleeding from some detached portions of the placenta that prompted removal of these portions to secure hemostasis.
In our institute, there was another case of abdominal pregnancy where there was no bleeding from placenta so the placenta was left in situ. No methotrexate was given because it may cause rapid necrosis of placenta, infection and abscess formation [10].
There are only very few case reports of advanced extra-uterine pregnancy that ended in a viable healthy fetus with no malformations and a healthy mother and hence this was a rare of the rarest case of secondary abdominal pregnancy. Abdominal pregnancy with resultant healthy newborn is very rare. Diagnosis of the condition can be difficult especially if the pregnancy is advanced. High level of suspicion, careful clinical and ultrasound examinations are the routine means of diagnosis though CT scan and MRI can be useful. Bleeding is the single most important life-threatening complication for the mother while fetal malformation is one of the numerous challenges that can confront the newborn.
Dr. Rajkumar Gurjar
is a third-year postgraduate student in the Department of Obstetrics and Gynecology, RNT Medical College, Udaipur. He has keen interest in high-risk cases and their management.
Conflict of interest
The authors declare that he has no conflict of interest.
Informed Consent
Informed consent was taken for publication of this case report from patient and institutional head.
Footnotes
Dr. Rajkumar Gurjar is third-year resident at RNT Medical College Udaipur in Department of Obstetrics and Gynecology. He has keen interest in high-risk cases and their management.
References
- 1.Atrash HK, Friede A, Hogue CJ. Abdominal pregnancy in the United States: frequency and maternal mortality. Obstet Gynecol. 1987;69:333–337. [PubMed] [Google Scholar]
- 2.Worley KC, Hnat MD, Cunningham FG. Advanced extrauterine pregnancy: diagnostic and therapeutic challenges. Am J Obstet Gynecol. 2008;198(3):297.e1–297.e7. doi: 10.1016/j.ajog.2007.09.044. [DOI] [PubMed] [Google Scholar]
- 3.Costa SD, Presley J, Bastert G. Advanced abdominal pregnancy. Obstet Gynecol Surv. 1991;46(8):515–525. doi: 10.1097/00006254-199108000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Yildizhan R, Kolusari A, Adali F. Primary abdominal ectopic pregnancy: a case report. Cases J. 2009;2:8485. doi: 10.4076/1757-1626-2-8485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dahab AA, Aburass R, Shawkat W. Full-term extrauterine abdominal pregnancy: a case report. J Med Case Rep. 2011;5:531. doi: 10.1186/1752-1947-5-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Opare-Addo HS, Daganus S. Advanced abdominal pregnancy: a study of 13 consecutive cases seen in 1993 and 1994 at Komfo Anokye Teaching Hospital, Kumasi. Ghana. Afr J Reprod Health. 2000;4(1):28–39. doi: 10.2307/3583240. [DOI] [PubMed] [Google Scholar]
- 7.Bertrand G, Le Ray C, Simard-Emond L, et al. Imaging in the management of abdominal pregnancy: a case report and review of the literature. J Obstet Gynaecol Can. 2009;31(1):57–62. doi: 10.1016/S1701-2163(16)34055-5. [DOI] [PubMed] [Google Scholar]
- 8.Mittal SK, Singh N, Verma AK, et al. Fetal MRI in the pre-operative diagnosis and assessment of secondary abdominal pregnancy: a rare sequela of a previous caesarean section. Diagn Interv Radiol. 2012;18(5):496–502. doi: 10.4261/1305-3825.DIR.5200-11.1. [DOI] [PubMed] [Google Scholar]
- 9.Stevens CA. Malformations and deformations in abdominal pregnancy. Am J Med Genet. 1993;47(8):1189–1195. doi: 10.1002/ajmg.1320470812. [DOI] [PubMed] [Google Scholar]
- 10.Rahman MS, Al-Suleiman SA, Rahman J, et al. Advanced abdominal pregnancy–observations in 10 cases. Obstet Gynecol. 1982;59(3):366–72. [PubMed] [Google Scholar]


