Introduction
The term fetus papyraceous is used when intrauterine fetal demise of a twin occurs early in pregnancy, with retention of the fetus for a minimum of 10 weeks resulting in mechanical compression of the small fetus and loss of fluid such that it resembles parchment paper. It is rare complication with incidence of 1:12,000 pregnancies and between 1:184 and 1:200 twin pregnancies. It results from failure to completely reabsorb the dead fetus. The cause is usually unknown, but is associated with twin-to-twin transfusion (TTTS), fetal genetic or chromosomal abnormalities and improper cord implantation such as velamentous cord insertion. There can be maternal and fetal complications.
Case History
An unbooked 25 yrs female was admitted on May 11, 2018 with H/O 8 months and 25 days amenorrhea for routine checkup. LMP was on 16.08.17 hence her EDD was calculated to be on 23.5.18. Here obstetric score was G2P1L1A0. In her first pregnancy a full term cesarean section was done—2 years 4 months back for transverse lie, 2.62 kg. In this pregnancy, she was booked elsewhere. She was diagnosed to have monochorionic monoamniotic twin gestation, with one foetus papyraceous and other foetus alive. There was no H/O pain or bleeding during early gestational period or other symptoms.
Her general examination was within normal limits. On per abdomen examination uterus was 34 weeks of gestation, relaxed, cephalic presentation, FHS 138/min regular, no scar tenderness, On per vaginal examination os was closed.
Investigations—Hb—12.2 g %, TWBC:7700/cu mm, platelet—1.93 lakh/cu mm, Blood group—B +ve, HIV, HBSAg, RPR—nonreactive, urine—WNL, GCT-WNL. PT—10.1, control—11.5, INR—0.87. She had serial USGs done. The reports are shown in Table 1.
Table 1.
Serial USG reports
| Gestational age in weeks and days | Fetus 1 | Fetus 2 | Placenta, chorionicity | Liquor, amnionicity |
|---|---|---|---|---|
| 13 and 0 | 11 weeks 5 days | 11 weeks 1 day | – | – |
| 19 and 1 | 13 weeks 1 day, dead | 18 weeks, live | Monochorionic | Monoamniotic |
| 23 and 5 | 11 weeks 5 days, dead | 22 weeks, live | Posterior | Adequate |
| 32 and 6 | Not mentioned | 30 weeks 2 days EFW*—1468 g |
Posterior | Adequate |
| 37 and 5 | Not mentioned | 33 weeks 3 days | Posterior | Adequate |
*EFW expected foetal weight
Provisional diagnosis was 38 weeks 2 days gestation with fetal growth restriction (FGR) with previous LSCS with fetus papyraceous.
She was admitted and elective LSCS was done in view of FGR with previous LSCS.
Intraoperative findings First baby was delivered by vertex and cried immediately. A fetus papyraceous, 3–4 cm in length, flattened, yellowish with an identifiable head and eye, was attached to the placenta with a very thin, thready umbilical cord. The corresponding placenta was very small and calcified. The healthy fetus weighing 2.03 kg had a healthy cord attached to the healthy counterpart of the same placenta. A separating membrane was seen in between the two placental counterparts suggesting diamnionicity as against the USG report of monoamnionicity (Figs. 1, 2).
Fig. 1.

Intraoperative Picture showing foetus papyraceous with thin umbilical cord & a healthy umbilical cord
Fig. 2.
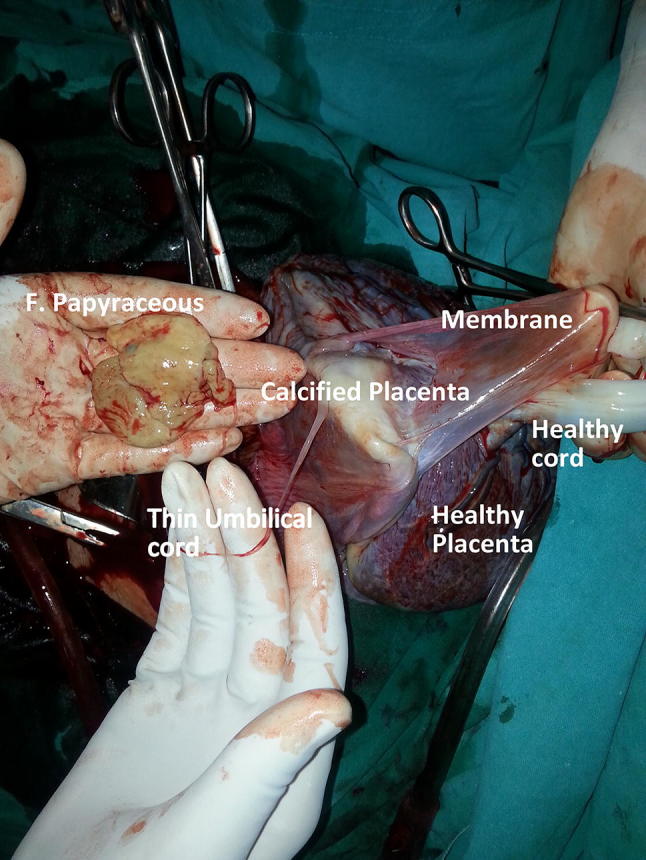
The Monochorionic placenta showing dividing membrane, foetus papuraceous with thin cord & healthy cord with healthy counterpart of placenta
Discussion
Frequently papyraceous twin is a blighted ovum, one that is never developed beyond the earliest stages of embryogenesis. In pregnancies achieved by IVF, it frequently happens that more than one amniotic sac can be seen in early pregnancy, whereas a few weeks later there is only one sac seen and the other has vanished. Hence, the rate of multi-fetal gestation is higher at conception, than at the time of birth. Fetus papyraceous has become quite common due to the practice of “fetal reduction” used after fertilization via assisted reproductive technology. With vanishing twin syndrome, there may be complete reabsorption of the fetus or formation of a mummified, compressed papyraceus and development of a subtle placental abnormality like placental cyst, subchorionic fibrin, amorphous material.
Fetus papyraceous can occur in both uniovular and binovular twins. Intrauterine death is three times more common in case of uniovular twin because of frequency of vascular connections (85–98%) and TTTS in monochorionic placenta [1]. In dichorionic twins, the prognosis for the surviving twin is relatively good and immaturity is the main risk factor. Death of one fetus can lead to ischemic brain damage of the other twin by causing sudden hypotension and hampering the blood supply to other twin. In diamniotic twins, death of one baby can cause sudden rupture of the thin membrane between them again leading to sudden hypotension and death of the other twin. Rarely, single-fetal death causes release of fibrin and tissue thromboplastins in circulation, causing disaminated intravascular coagulation which can also damage organs of surviving twin like brain, kidney & cause intrauterine death or premature birth (twin embolization syndrome). Though it is very uncommon, it can be fatal for both the mother and the fetus [2]. In general, chorionicity rather than zygosity determines the risk of mortality and the morbidity [2].
Loss of one twin in the first trimester does not appear to impair the development of the surviving twin. This may present as vaginal bleeding and mild abdominal pain, especially if the fetus is completely absorbed and mostly there are no complications afterward. Fetal death occurring after mid-gestation may increase the risk of IUGR to the surviving twin, cerebral palsy, preterm labor, preeclampsia, hemorrhage, sepsis as a result of a dead fetus, consumptive hemorrhage, labor dystocia and perinatal mortality.
Placental or fetal analysis frequently reveals chromosomal abnormalities, triploidy, abnormal sex chromosomes, which may be found in skin biopsies, placental pathology, chorionic villi sampling. Chromosomal analysis of the surviving twin is generally normal. Other complications can be aplasia cutis, microcephaly, hydrocephalus, eye anomalies, cleft lip/palate, cardiac anomalies.
A vanishing twin may cause an elevated maternal serum alpha-fetoprotein, an elevated amniotic alpha-fetoprotein level and a positive amniotic fluid acetylcholine esterase.
If fetus papyraceous is diagnosed antenatally, close monitoring is of utmost importance. Serial evaluation of the surviving fetus by sonography, biophysical profile, Doppler and maternal serial evaluation by coagulation profile, FDP and d-dimer should be done.
Our patient was booked elsewhere. She was continuously monitored by serial ultrasounds throughout the pregnancy once the vanishing twin was diagnosed. But there was no previous record of monitoring her BPP, Doppler, maternal coagulation profile, FDP and D-dimer. Although her INR on admission was within normal limits, the surviving twin had FGR, which can be identified by the serial ultrasound reports. As is evident from the picture, the pregnancy was diamniotic as against the early USG report of monoamniotic. The main problem with early ultrasound examination is the occasional difficulty in visualization of the interfetal membrane in some diamniotic pregnancies, leading to erroneous diagnosis of monoamniotic gestation.
Dahiya et al. [3] have reported two cases of fetus papyraceous delivered at term with no complications to the surviving fetus.
A case report is available depicting 35 weeks pregnancy with fetus papyraceous causing labor dystocia,(fetus + placenta weighing 200 g) requiring cesarean delivery [4].
A monochorionic monoamniotic twin pregnancy with demise of one twin at 27 weeks is reported, which was delivered at 37 weeks, and the mummified fetus weighed 700 g [1].
Conclusion
In the presence of fetus papyraceous, we are primarily concerned about the effect it can have on the surviving fetus and the mother. Carefully monitoring of the surviving fetus by serial ultrasound and monitoring the mother for possible complications are of paramount importance for a better outcome.
Prof. Sandhya Gadre
is working at Chirayu Medical College and Hospital, Bhopal. She has seven case studies and five case reports published in international and national journals. She has been awarded FICOG and is presently pursuing advanced course in medical education technology from MCI nodal center, Karamsad. She is a member and resource faculty of medical education technology of CMCH, Bhopal, and has participated in several RBCW workshops. Has a passion for implementing her own innovative methods for teaching students. The author has the experience of being speaker, panelist and moderator at AICOG, state- and local-level conferences. She has presented many research papers, posters at AICOG, state- and local-level conferences and won prize. She has written many fictions, poetries which have got published.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was taken.
Footnotes
Sandhya Gadre is a Professor of Department of Obstetrics and Gynaecology at Chirayu Medical College and Hospital, Bhopal. Reshika Gangatirkar is a Assistant Professor of Department of Obstetrics and Gynaecology at Chirayu Medical College and Hospital, Bhopal.
References
- 1.Rahman H, Pathak R, Dubey S, et al. Fetus papyraceous in uniovular twin; death of one twin in early third trimester and successful outcome of other twin at term: a rare case report. Gen Med (Los Angel) 2013;1:118. [Google Scholar]
- 2.Jain D, Purohit RC. Review of twin pregnancies with single foetal death: management, maternal and fetal outcome. J Obstet Gynecol India. 2014;64(3):180–183. doi: 10.1007/s13224-013-0500-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dahiya P, Bains R. Conservative management of fetus papyraceus: a report of two cases. Oman Med J. 2014;29(2):132–134. doi: 10.5001/omj.2014.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matovelo D, Ndaboine E. Fetus papyraceus causing dystocia in a rural setting: a case report. J Med Case Rep. 2015;9:178. doi: 10.1186/s13256-015-0666-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


