Abstract
Objectives
Molecular profiling of tumours has become the mainstay of diagnostics for metastasised solid malignancies and guides personalised treatment, especially in nonsmall cell lung cancer (NSCLC). In current practice, it is often challenging to obtain sufficient tumour material for reliable molecular analysis. Cell-free DNA (cfDNA) in blood or other bio-sources could present an alternative approach to obtain genetic information from the tumour. In a retrospective cohort we analysed the added value of cfDNA analysis in pleural effusions for molecular profiling.
Methods
We retrospectively analysed both the supernatant and the cell pellet of 44 pleural effusions sampled from 39 stage IV patients with KRAS (n=23) or EGFR (n=16) mutated tumours to detect the original driver mutation as well as for EGFR T790M resistance mutations. Patients were diagnosed with either NSCLC (n=32), colon carcinoma (n=4), appendiceal carcinoma (n=2) or adenocarcinoma of unknown primary (n=1). Samples collected in the context of routine clinical care were stored at the Netherlands Cancer Institute biobank. We used droplet digital PCR for analysis.
Results
The driver mutation could be detected in 36 of the 44 pleural effusions by analysis of both the supernatant (35 out of 44 positive) and the cell pellet (31 out of 44 positive). In seven out of 20 pleural effusions from patients with EGFR mutation-positive tumours, a T790M mutation was detected. All seven supernatants and cell pellets were positive.
Conclusions
cfDNA in pleural effusion can be used to detect driver mutations as well as resistance mechanisms like EGFR T790M in pleural effusion with high accuracy and is therefore a valuable bio-source.
Short abstract
Cell-free DNA in the supernatant of pleural effusion is a valuable bio-source and can be used to detect driver mutations as well as resistance mechanisms like EGFR T790M in pleural effusion http://ow.ly/Z16830nxxti
Introduction
In current practice, molecular profiling of tumours has become essential to offer targeted therapy for several types of metastasised malignancies. Especially in nonsmall cell lung cancer (NSCLC), targeted therapy has been shown to be highly effective, and multiple tyrosine kinase inhibitors (TKIs) for activating mutations or rearrangements in genes like EGFR (epidermal growth factor receptor), BRAF (B-Raf proto-oncogene serine/threonine kinase), ALK (anaplastic lymphoma kinase) and ROS1 (Ros oncogene 1 receptor tyrosine kinase) have become available [1]. Also, early detection of resistance mutations like EGFR T790M is important as they can guide the next line of therapy [2].
Unfortunately, obtaining tumour tissue for molecular analysis can be challenging. The site of the tumour can be difficult to reach and it often requires invasive procedures to obtain adequate amounts of vital tumour. In this respect, pleural effusion could be an attractive alternative bio-source for molecular analysis, especially as ∼30% of NSCLC patients develop pleural effusion [3]. Usually, DNA is isolated from a cell block or a Giemsa slide, but analysis of cell-free DNA (cfDNA) in the supernatant has shown promising results [4–9]. Moreover, since the amount of tumour cells or the tumour cell percentage is often insufficient for analysis, this cell-free compartment is highly interesting.
Here, we explore the diagnostic yield of cfDNA analysis in pleural effusion samples from patients with NSCLC and other cancer types for EGFR and KRAS (KRAS proto-oncogene GTPase) driver mutation detection, as well as for EGFR resistance mutations. Analyses of cfDNA from the supernatant were compared head to head with analyses of the cell pellets (figure 1).
FIGURE 1.
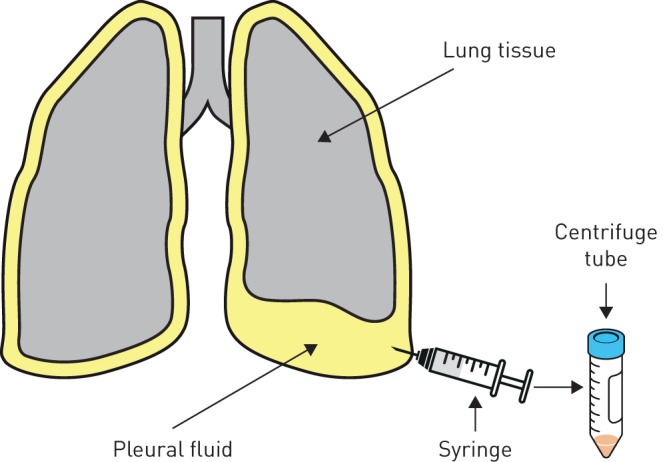
A schematic overview of the collection of pleural effusion. After pleurocentesis the fluid was centrifuged in order to separate the supernatant from the cell pellet.
Methods
Supernatant and corresponding cell pellets from 39 stage IV patients, presented at the Netherlands Cancer Institute (Amsterdam, The Netherlands) between 2009 and 2016, with EGFR (n=16) or KRAS (n=23) mutation-positive tumours were obtained from the Netherlands Cancer Institute biobank. In total, 44 paired (supernatant and cell pellet) samples were available from 39 patients diagnosed with NSCLC (n=32), colon carcinoma (n=4), appendiceal carcinoma (n=2) and adenocarcinoma of unknown primary (n=1) (table 1). The reason for pleurocentesis was either diagnostic (n=16) or therapeutic (n=28). These samples were leftover material that had been stored as routine laboratory assessment after diagnostics.
TABLE 1.
Patient and sample characteristics
| All patients | All paired samples | Paired samples per tumour driver mutation | ||||
| EGFR exon 19 deletion | EGFR L858R | EGFR G719X | KRAS | |||
| Patients/samples | 39 | 44 | 15 | 4 | 1 | 24 |
| Tumour type | ||||||
| Nonsmall cell lung cancer | 32 | 35 | 15 | 4 | 1 | 17 |
| Colon carcinoma | 4 | 4 | 4 | |||
| Appendiceal carcinoma | 2 | 2 | 2 | |||
| Adenocarcinoma of unknown primary | 1 | 1 | 1 | |||
Data are presented as n.
This study was approved by the Institutional Research Board of the Netherlands Cancer Institute (CFMPB497).
All driver gene and EGFR T790M mutations were detected in tumour tissue or cytology samples with clinically validated assays using high-resolution melting, fragment analysis, Sanger sequence analysis, MassARRAY technology or next-generation sequencing (NGS) (data not shown). These analyses were done in multiple hospitals in the Netherlands.
The supernatant was separated from the cell pellet after centrifugation (1700×g for 10 min). The pellet was resuspended in 0.5 mL of 0.9% NaCl. Both samples were stored at −30°C. In total, 400 μL from the cell pellet was isolated using the QIAsymphony DSP DNA Midi Kit (Qiagen, Hilden, Germany). At least 10% from the sample was analysed, from a median eluted volume of 200 μL. cfDNA was isolated from a median (range) of 1 (0.75–4) mL pleural effusion using the QIAsymphony Circulating DNA kit (Qiagen). At least 20% of the sample was analysed, from a median eluted volume of 90 μL. The Bio-Rad (Hercules, CA, USA) QX200 droplet digital PCR (ddPCR) was used for mutation detection using Bio-Rad PrimePCR ddPCR mutation assays for KRAS (KRAS Screening Multiplex 186-3506), EGFR T790M (dHsaCP2000019 and dHsaCP2000020), EGFR exon 19 deletion screening assay [10], EGFR L858R (dHsaCP2000021 and dHsaCP2000022) and EGFR G719X (validated laboratory-developed method using IDT (Coralville, IA, USA) EGFR wild-type for G719 (HEX), EGFR G719S and EGFR G719A (both FAM)). The limit of blank and the limit of detection were determined for each individual assay using a Clinical and Laboratory Standards Institute (CLSI) EP17 protocol [11]. Results were analysed using Quantasoft version 1.6.6 (www.quantasoft.com). Supernatant results were normalised to the amount of cfDNA in 1 mL of fluid.
Results
The majority of the 44 paired samples were either both positive (30 out of 44) or both negative (eight out of 44) for the original driver mutation. In five cases the driver mutation was only detected in the supernatant and in one case only in the cell pellet (table 2). Thus, in 36 of the 44 paired samples a driver mutation was detected using both the supernatant and the cell pellet. Testing only the supernatant would detect 35 of the 36 drivers (97%) and analysis of only the cell pellet would detect 31 of the 36 drivers (86%). These results indicated that the supernatant was an excellent bio-source for ddPCR driver detection. Optimal sensitivity was reached when both the cell pellet and supernatant were analysed.
TABLE 2.
Detection of original driver mutations by droplet digital PCR in paired samples (supernatant and cell pellet available) of pleural effusions
| Supernatant | Cell pellet | ||
| Driver positive | Driver negative | Total | |
| Driver positive | 30 | 5 | 35 |
| Driver negative | 1 | 8 | 9 |
| Total | 31 | 13 | 44 |
Data are presented as n.
In five paired samples the driver mutation was only detected in the supernatant. Reviewing the cytology reports for these cases showed that in two of these samples no tumour cells were seen, in two cases no cytologically analysis was performed and in one case the tumour cell percentage was only 1%. In four of these cell pellets no mutant copies were found and in one the amount was below the limit of detection. In one sample only the cell pellet was positive for the primary driver mutation. This cell pellet had a very low estimated tumour cell percentage and a borderline result of only 1 mutant copy·μL−1 in the cell pellet (supplementary table S1). No mutant copies were detected in the supernatant by ddPCR. The cfDNA was isolated from 0.75 mL of supernatant and showed a very low concentration of 0.005 ng·μL−1 measured by Qubit (Invitrogen, Carlsbad, CA, USA). Therefore, the mutation could easily be missed in our analysis.
To evaluate whether pleural effusion could be used as a bio-source for resistance analysis after progression on EGFR TKIs we analysed 20 paired pleural effusions sampled from the 16 patients with EGFR-positive tumours for the presence of EGFR T790M. EGFR T790M was detected in seven out of the 20 paired samples. All seven supernatants and cell pellets were positive (table 3). Four out of the seven EGFR T790M mutation-positive pleural effusion samples had very low estimated tumour cell percentages and in one case no tumour cells were seen by the pathologist (supplementary table S1). Five of the seven pleural effusions were sampled from patients progressing on first-generation EGFR TKIs (erlotinib, gefitinib). Furthermore, two cases with a positive supernatant, but with a cell pellet showing a borderline result of 1 copy·μL−1, identified two patients with a durable response to osimertinib. The cytology reports of these pleural effusion samples showed that in one sample no tumour cells were seen and in one sample the tumour cell percentage was very low (supplementary table S1). These results indicated that the supernatant is a good bio-source to detect EGFR T790M. In four patients EGFR T790M had already been detected in tumour tissue samples by clinically validated diagnostic assays. EGFR T790M was confirmed in all four matched supernatants and cell pellets. Two out of the seven samples were initially taken specifically for molecular resistance analysis by NGS/TSACP version 1.0 (MiSeq; Illumina, San Diego, CA, USA) using the cell pellet: in one of these samples NGS could be successfully performed but no T790M mutation was found, while for the other sample in the end no NGS was done due to a low estimated tumour cell percentage. Both samples had tumour cell percentages ≤5% (supplementary table S1).
TABLE 3.
Detection of EGFR T790M by droplet digital PCR in paired samples (supernatant and cell pellet available) of pleural effusions
| Supernatant | Cell pellet | ||
| T790M positive | T790M negative | Total | |
| T790M positive | 7 | 0 | 7 |
| T790M negative | 0 | 13 | 13 |
| Total | 7 | 13 | 20 |
Data are presented as n.
Discussion
This study investigated whether cfDNA from the supernatant of pleural effusions could be used for detecting driver mutations and EGFR resistance mutations. Our results clearly show that the cell-free fraction of pleural effusions is an excellent source for cfDNA and that it can be used to detect driver as well as resistance mutations effectively with ddPCR. We showed a high concordance rate between the supernatant and the cell pellet, which is in line with a previous study [6], but a slightly lower rate has been reported elsewhere [7]. Furthermore, our results suggest that by using cfDNA in pleural effusion as a bio-source, the molecular testing has gained in sensitivity, and that optimal sensitivity can be reached by analysing both the supernatant and the cell pellet. In addition to analysis of cfDNA in pleural effusion from NSCLC patients, we could also detect KRAS mutations in the supernatant samples from patients with colon carcinoma, appendiceal carcinoma and adenocarcinoma of unknown primary, which has not been reported before.
In five pleural effusion samples driver mutations were detected only in the supernatant even though no or very few tumour cells were seen in the cytopathological results. In our study, mutations were only called when the amount of copies found by ddPCR was above the limit of detection, determined according to the CLSI EP17 protocol [11]. The limit of detection was set with a confidence level of 99% to prevent false-positive results. Tumour DNA in the five corresponding cell pellets was not present or too low to detect the driver mutation. Importantly, since the detection of a driver mutation in the supernatant provides no proof of actual presence of tumour cells it can at present not be used for staging purposes. The origin of cfDNA in the supernatant has not been well studied, although several theories have been described [5, 8, 9]. Most likely this cfDNA is released from necrotic cells in the pleural cavity, but may also have been leaked from the circulation as a transudate. Alternatively, the cfDNA could have been derived from tumour cells damaged in the pre-analytical phase, e.g. by centrifugation [5], or from exosomes secreted by the tumour [8, 9]. Therefore, a high detection rate in the supernatant is expected and also observed in our study. In one pleural effusion sample only the cell pellet was positive for the driver mutation. Most likely too little tumour DNA was present in the supernatant.
Resistance mutations are subclonal events in the tumour that often occur during TKI treatment. The EGFR T790M mutation, for example, is common in tumours of patients progressing on first-generation EGFR TKIs (erlotinib, gefitinib) [2]. Osimertinib is frequently given as alternative treatment after this mutation is detected in a biopsy of a progressive lesion [2]. As obtaining tumour tissue is challenging and EGFR T790M is a subclonal event, sensitive techniques are needed for molecular testing. Plasma genotyping is an alternative approach, but the sensitivity of detecting EGFR T790M in plasma is only 70% [12]. Therefore, other bio-sources for molecular testing could be useful. In our study, seven paired samples were positive for EGFR T790M, of which all were concordant between the supernatant and the cell pellet. Based on these results, both the supernatant and the cell pellet performed equally well as bio-sources for detecting EGFR T790M. The pleural effusion samples from four of the five patients progressing on first-generation EGFR TKIs showed a higher amount of T790M copies in both the supernatant and cell pellet compared with the two patients showing a durable response to osimertinib. In prospective studies it will be interesting to see if the amount of EGFR T790M copies, measured by ddPCR in the supernatant and cell pellet of pleural effusions, correlates to outcome in patients with EGFR-positive tumours treated with osimertinib.
This study is limited by the small sample size. The supernatant performed better as a bio-source than the cell pellet for detecting EGFR or KRAS primary driver mutations, but not for detecting EGFR T790M. Studies with a larger sample size are needed to confirm our results. Besides this, we could only compare a subset of the paired samples with results obtained in molecular diagnostics with NGS/TSACP version 1.0 using the cell pellet. A direct comparison with a larger set of paired samples could confirm the additive value of using cfDNA in the supernatant as a bio-source for molecular profiling in a clinical setting.
In conclusion, we showed that analysis of cfDNA in pleural effusion can robustly detect EGFR and KRAS driver mutations and EGFR resistance mutations. Therefore, cfDNA is a valuable bio-source for molecular testing, even when tumour cell purity is low.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
TABLE S1 Sample characteristics with initial clinical application in molecular diagnostics and concentrations of the original driver mutation and EGFR T790M in supernatant and/or cell pellet measured by ddPCR 00016-2019.table_S1 (18.6KB, xlsx)
Acknowledgements
We would like to acknowledge the Netherlands Cancer Institute Core Facility Molecular Pathology and Biobanking (CFMPB; Amsterdam, The Netherlands) for supplying biobank material and laboratory support.
Footnotes
This article has supplementary material available from openres.ersjournals.com
Conflict of interest: K. Hummelink has nothing to disclose.
Conflict of interest: M. Muller has nothing to disclose.
Conflict of interest: T.C. Linders has nothing to disclose.
Conflict of interest: V. van der Noort has nothing to disclose.
Conflict of interest: P.M. Nederlof has nothing to disclose.
Conflict of interest: P. Baas has nothing to disclose.
Conflict of interest: S. Burgers has nothing to disclose.
Conflict of interest: E.F. Smit has nothing to disclose.
Conflict of interest: G.A. Meijer reports patents pending on biomarkers and on the diagnosis and prognosis of colorectal cancer, and research collaborations with Exact Sciences and Sysmex in which the companies provide materials, equipment or (sample) analyses.
Conflict of interest: M.V. van den Heuvel has nothing to disclose.
Conflict of interest: D. van den Broek has nothing to disclose.
Conflict of interest: K. Monkhorst reports personal fees from Pfizer to attend ASCO 2016, personal fees from Roche Pharma to attend ASCO WCLC 2017, speaker's fees from Roche Diagnostics and Benecke, and has served on advisory boards for Pfizer, Roche, MSD, AbbVie and BMS, outside the submitted work.
References
- 1.Li T, Kung HJ, Mack PC, et al. . Genotyping and genomic profiling of non-small-cell lung cancer: implications for current and future therapies. J Clin Oncol 2013; 31: 1039–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cross DA, Ashton SE, Ghiorghiu S, et al. . AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov 2014; 4: 1046–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Froudarakis ME. Pleural effusion in lung cancer: more questions than answers. Respiration 2012; 83: 367–376. [DOI] [PubMed] [Google Scholar]
- 4.Liu D, Lu Y, Hu Z, et al. . Malignant pleural effusion supernatants are substitutes for metastatic pleural tumor tissues in EGFR mutation test in patients with advanced lung adenocarcinoma. PLoS One 2014; 9: e89946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin J, Gu Y, Du R, et al. . Detection of EGFR mutation in supernatant, cell pellets of pleural effusion and tumor tissues from non-small cell lung cancer patients by high resolution melting analysis and sequencing. Int J Clin Exp Pathol 2014; 7: 8813–8822. [PMC free article] [PubMed] [Google Scholar]
- 6.Asaka S, Yoshizawa A, Saito K, et al. . Rapid point-of-care testing for epidermal growth factor receptor gene mutations in patients with lung cancer using cell-free DNA from cytology specimen supernatants. Int J Oncol 2018; 52: 2110–2118. [DOI] [PubMed] [Google Scholar]
- 7.Kawahara A, Fukumitsu C, Azuma K, et al. . A combined test using both cell sediment and supernatant cell-free DNA in pleural effusion shows increased sensitivity in detecting activating EGFR mutation in lung cancer patients. Cytopathology 2018; 29: 150–155. [DOI] [PubMed] [Google Scholar]
- 8.Shin S, Kim J, Kim Y, et al. . Assessment of real-time PCR method for detection of EGFR mutation using both supernatant and cell pellet of malignant pleural effusion samples from non-small-cell lung cancer patients. Clin Chem Lab Med 2017; 55: 1962–1969. [DOI] [PubMed] [Google Scholar]
- 9.Lee J, Hur JY, Kim IA, et al. . Liquid biopsy using the supernatant of a pleural effusion for EGFR genotyping in pulmonary adenocarcinoma patients: a comparison between cell-free DNA and extracellular vesicle-derived DNA. BMC Cancer 2018; 18: 1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yung TK, Chan KC, Mok TS, et al. . Single-molecule detection of epidermal growth factor receptor mutations in plasma by microfluidics digital PCR in non-small cell lung cancer patients. Clin Cancer Res 2009; 15: 2076–2084. [DOI] [PubMed] [Google Scholar]
- 11.Clinical and Laboratory Standards Institute. EP17: Evaluation of Detection Capability for Clinical Laboratory Measurement Procedures. 2nd Edn Wayne, CLSI, 2012. [Google Scholar]
- 12.Oxnard GR, Thress KS, Alden RS, et al. . Association between plasma genotyping and outcomes of treatment with osimertinib (AZD9291) in advanced non-small-cell lung cancer. J Clin Oncol 2016; 334: 3375–3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
TABLE S1 Sample characteristics with initial clinical application in molecular diagnostics and concentrations of the original driver mutation and EGFR T790M in supernatant and/or cell pellet measured by ddPCR 00016-2019.table_S1 (18.6KB, xlsx)


