Among patients with symptoms/signs of cardiac ischaemia referred for coronary angiography up to two-thirds of women and one-third of men have no obstructive coronary artery disease (CAD).1,2 These patients with ischaemia and no obstructive CAD (INOCA) have an almost two-fold higher risk of cardiovascular disease (CVD) compared with age- and sex-matched reference subjects, even after adjusting for traditional CVD risk factors.2 To identify specific prevention and treatment strategies for symptomatic patients with INOCA it is essential to explore the presence of novel risk variables.3 Little is known about differences in non-traditional factors and psychosocial well-being of these patients compared with those with stable angina due to stable obstructive CAD (further mentioned as CAD).
We studied 64 women with INOCA and 64 age-matched women with CAD, recruited from our specialised women’s heart outpatient clinic and regular outpatient clinic at the Radboud University Medical Center in The Netherlands, respectively. All participants had at least weekly occurring angina for at least three months. Patients with structural myocardial disease, significant valvular heart disease or significant psychiatric comorbidity were excluded. All patients completed an online survey with questions regarding sociodemographic factors, severity of symptoms, traditional CVD risk factors, non-traditional risk variables and four validated psychosocial questionnaires concerning fatigue, cardiac-related anxiety, quality of life and general anxiety and depression (Checklist Individual Strength,4 Cardiac Anxiety Questionnaire,5 Short Form 126 and Hospital Anxiety and Depression Scale).7 Comparisons were made using the appropriate tests. All reported p values are two-sided and p values < 0.05 were considered significant. The local Ethics Committee approved the study protocol and all patients gave written informed consent.
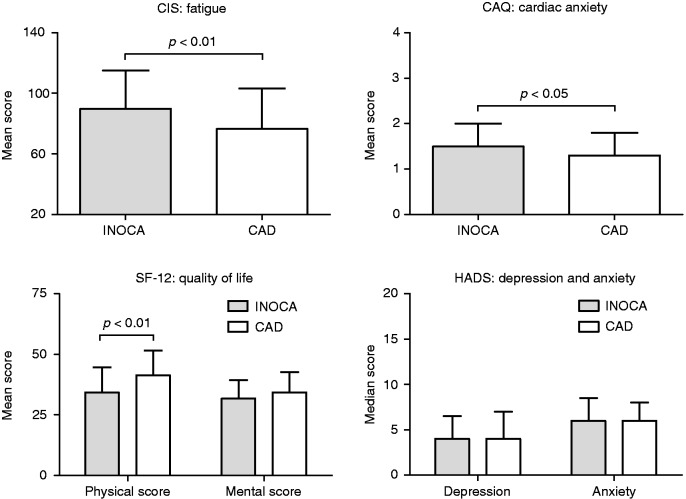
Results showed that the median age of women with INOCA and women with CAD was 57 and 56 years respectively (p = 0.46) and that most were postmenopausal (84% vs. 81%, p = 0.82). Women with INOCA had higher education levels compared with women with CAD. Other sociodemographic factors did not differ. Women with INOCA reported more severe and more frequent symptoms compared with women with CAD (angina CCS ≥ 3: 34% vs. 11%, p < 0.01; New York Heart Association class ≥ 3: 52% vs. 24%, p < 0.01, daily symptoms: 40% vs. 7%, p < 0.01). Regarding traditional CVD risk factors, women with INOCA were less frequently active smokers compared with women with CAD (8% vs. 23%, p = 0.02). There was a weak correlation between smoking behaviour and educational level (τb = 0.07, p < 0.01). There were no significant differences in the reported prevalence of traditional CVD risk factors (hypertension, hypercholesterolaemia, diabetes mellitus or a family history of CVD) between the two groups. Regarding non-traditional risk variables, women with INOCA more often reported rheumatic disorders (39% vs. 21%; p < 0.01) or a history of premenopausal migraine (52% vs. 31%; p = 0.02) compared with women with CAD. Female-related risk factors had a low prevalence in both groups with no differences. Outcomes of the psychosocial questionnaires are shown in Figure 1. Women with INOCA scored higher levels of fatigue and cardiac anxiety and a lower physical quality of life compared with women with CAD. Mental quality of life scores were comparable among both groups and levels of general anxiety and depression were overall low without significant differences. The frequency and severity of angina correlated with the level of fatigue, cardiac anxiety and physical quality of life in both groups (τb = 0.21, p < 0.01; τb = 0.22, p < 0.01; τb = –0.42, p < 0.01, respectively).
Figure 1.
Psychosocial factors in women with INOCA and CAD.
Values are presented as mean and SD for the CAQ, SF-12 and CIS; the HADS as median and interquartile range.
INOCA: ischaemia with no obstructive coronary arteries; CAD: stable obstructive coronary artery disease; CIS: Checklist Individual Strength; CAQ: Cardiac Anxiety Questionnaire; SF-12: Short Form 12; HADS; Hospital Anxiety and Depression Scale.
Our cross-sectional study demonstrates that women with INOCA have a different pattern of risk factors compared with women with stable obstructive CAD. These differences are mainly determined by non-traditional risk variables related to inflammation. Our data also show that women with INOCA experience more psychosocial distress – related to a higher symptom burden – but not higher levels of general anxiety or depression. Awareness of psychosocial distress in patients with ischaemic heart disease is important.8 Prospective longitudinal studies are warranted to explore the causality of the studied risk variables for INOCA.
Author contribution
AHEMM, CB, SEES and AL contributed to the conception and design. All authors contributed in the items acquisition, analysis and interpretation. REK and SEES drafted the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Johnston N, Schenck-Gustafsson K, Lagerqvist B. Are we using cardiovascular medications and coronary angiography appropriately in men and women with chest pain? Eur Heart J 2011; 32: 1331–1336. [DOI] [PubMed] [Google Scholar]
- 2.Jespersen L, Hvelplund A, Abildstrom SZ, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 2012; 33: 734–744. [DOI] [PubMed] [Google Scholar]
- 3.Bairey Merz CN, Pepine CJ, Walsh MN, et al. Ischemia and no obstructive coronary artery disease (INOCA): Developing evidence-based therapies and research agenda for the next decade. Circulation 2017; 135: 1075–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vercoulen JHMM, Alberts M and Bleijenberg G. De Checklist Individual Strength (CIS). Gedragstherapie 1999; 32: 131–136.
- 5.Eifert GH, Thompson RN, Zvolensky MJ, et al. The cardiac anxiety questionnaire: Development and preliminary validity. Behav Res Ther 2000; 38: 1039–1053. [DOI] [PubMed] [Google Scholar]
- 6.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–233. [DOI] [PubMed] [Google Scholar]
- 7.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 8.Pogosova N, Kotseva K, De Bacquer D, et al. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: Results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur J Prev Cardiol 2017; 24: 1371–1380. [DOI] [PubMed] [Google Scholar]