Abstract
Objective:
To evaluate the efficacy of a paraprofessional-delivered, home-visiting intervention among young, reservation-based American Indian (AI) mothers on parenting knowledge, involvement, and maternal and infant outcomes.
Method:
From 2002 to 2004, expectant AI women aged 12 to 22 years (n = 167) were randomized (1:1) to one of two paraprofessional-delivered, home-visiting interventions: the 25-visit “Family Spirit” intervention addressing prenatal and newborn care and maternal life skills (treatment) or a 23-visit breast-feeding/nutrition education intervention (active control). The interventions began during pregnancy and continued to 6 months postpartum. Mothers and children were evaluated at baseline and 2, 6, and 12 months postpartum. Primary outcomes included changes in mothers’ parenting knowledge and involvement. Secondary outcomes included infants’ social and emotional behavior; the home environment; and mothers’ stress, social support, depression, and substance use.
Results:
Participants were mostly teenaged, first-time, unmarried mothers living in reservation communities. At 6 and 12 months postpartum, treatment mothers compared with control mothers had greater parenting knowledge gains, 13.5 (p < .0001) and 13.9 (p < .0001) points higher, respectively (100-point scale). At 12 months postpartum, treatment mothers reported their infants to have significantly lower scores on the externalizing domain (β = −.17, p < .05) and less separation distress in the internalizing domain (β = −.17, p < .05). No between-group differences were found for maternal involvement, home environment, or mothers’ stress, social support, depression, or substance use.
Conclusions:
This study supports the efficacy of the paraprofessional-delivered Family Spirit home-visiting intervention for young AI mothers on maternal knowledge and infant behavior outcomes. A longer, larger study is needed to replicate results and evaluate the durability of child behavior outcomes.
Keywords: American Indian, home visiting, parenting, infant development
Home-visiting interventions have shown a range of positive maternal and child health and behavior outcomes for young, black, Hispanic, and white unmarried, low-income mothers and their children. However, rigorous home-visiting trials have not yet demonstrated impacts on infant behavior outcomes1–3 or the use of paraprofessionals as home visitors.1,4
A variety of factors suggest paraprofessional-delivered, home-visiting interventions may be a viable public health strategy to prevent behavioral health problems among American Indian (AI) mothers and their children. First, the risk profile for AI mothers and children is similar or greater in magnitude to that of mothers and children who have responded to previous home-visiting interventions. American Indian teens bear children at twice the rate of U.S. all races and have more parity during adolescence.5American Indian mothers receive fewer prenatal and well-baby visits compared with U.S. all races mothers6–8 and thus experience less clinic-based education about prenatal and well-child care, child development, and parenting. Environmental and behavioral risks are also greater for young AI mothers and offspring living on reservations, including higher rates of poverty, substandard housing, unemployment, school dropout, alcohol and drug use, childhood injuries, suicide, disrupted family relationships, and domestic violence, compared with U.S. all races.5,9–12 Second, behavior problems that arise in infancy are known to track to negative behavioral outcomes in later childhood13,14 and adolescence.15 Theoretical models that underpin early childhood interventions posit effective parenting as the link between maternal factors and child outcomes and therefore center on parent training as the means for affecting positive outcomes for children.16,17 Specific to Indian communities, potent home-based parent education for AI teen parents could prevent the transmission of risk between teen mothers and their children by promoting effective parenting, while mitigating maternal and environmental risk factors that are associated with behavior problems and substance abuse in later childhood and adolescence.18 Third, home-visiting interventions in Indian communities overcome known transportation and cultural barriers to routine health care.19 Fourth, family and home-based interventions attract strong tribal community support as they resonate with native traditions that favor family-centered approaches to health and well-being.20 Fifth, well-trained AI paraprofessionals who speak their native languages and naturally navigate local social mores are inherently more culturally competent than non-Indian home visitors. The training and employment of native paraprofessionals also builds human capital in communities where there is a shortage of nurses and other providers to address behavioral health disparities.
Despite the potential use of paraprofessional home visitors in Indian communities, previous trials in the United States have suggested that nurse home visitors versus paraprofessionals were associated with more positive participant outcomes.4 However, these trials had notable methodological limitations. For example, one comparison of nurse and paraprofessional home visitors excluded paraprofessionals if they had any college preparation in the helping professions or a bachelors’ degree in any field.4 In the same study, it is not clear whether the intervention protocol relied on a manual-based curriculum for both interventionists,4 whether the content was the same, or whether both types of interventionists had to demonstrate mastery of their respective interventions before seeing participants. In addition, although preliminary results of this study favored nurse home visitors, in a subsequent publication of the same trial, the paraprofessional-visited mothers were found 2 years after the end of the intervention to have better mental health, greater sense of personal mastery, fewer subsequent miscarriages, and fewer low-birth-weight babies versus mothers visited by nurses, who had greater birth spacing, less domestic violence, and some indication of better child outcomes.1 Thus, it is difficult to know what the key intervention components (provider type and experience, intervention content, training, etc.) were in affecting participants’ specific outcomes. In the meantime, the use of paraprofessional home visitors is well supported by the international literature, which indicates well-trained lay health workers are effective21–24; avoid the cultural pitfalls of dispatching nonindigenous people into the home22; are more persuasive regarding risky attitudes and behaviors22; are more readily available than professional health educators25; and are more cost effective in impoverished or underresourced communities.21
The study described within is the second to evaluate the impact of the paraprofessional-delivered Family Spirit home-visiting intervention with young reservation-based AI mothers. The first-trial randomized young mothers from the Navajo and White Mountain Apache reservations to one of two home-visiting interventions: the Family Spirit intervention or a breast-feeding/nutrition education program from 28 weeks’ gestation to 6 months postpartum. Assessments occurred until 6 months postpartum and demonstrated improvements in mothers’ knowledge and involvement at 2 and 6 months postpartum.1 However, the duration of the first study did not allow for assessment of infant outcomes. The present study, although similar in design, extends the assessment period to 12 months postpartum and reports infant health and behavior outcomes at 1 year of age.
METHOD
Study Design
The study was designed through a long formative development phase that engaged local and cross-tribal advisory boards and a pilot study that proved the intervention feasible and relevant to the target populations.19 Expectant young AI mothers were randomized (1:1) to one of two home-visiting interventions: the Family Spirit intervention versus a breast-feeding/nutrition education program. Mothers received home-visiting lessons from 28 weeks’ gestation to 6 months postpartum and were evaluated with their children at baseline and 2, 6, and 12 months postpartum. Primary outcomes included mothers’ parenting knowledge and involvement. Secondary outcomes included infants’ social, emotional, and behavioral outcomes at age 1 year; mothers’ provision of a stimulating home environment; and mothers’ stress, social support, depression, and substance use. We hypothesized that the Family Spirit intervention would increase mothers’ parenting knowledge, involvement, and stimulation of the child in the home environment, which over time would positively have an impact on children’s social, emotional, and behavioral development.
The study protocol was approved by the Johns Hopkins institutional review board, the Navajo Nation Human Research Review Board and appropriate Navajo community health boards, the White Mountain Apache Health Board and Tribal Council, and the Phoenix Area Indian Health Service institutional review board. This article was reviewed and approved by the White Mountain Apache Tribal Council and the Navajo Nation Human Research Review Board.
Participants
Expectant AI mothers aged 12 to 22 years and with 28 weeks or lesser of gestation were eligible for participation. If the prospective participant was younger than 18 years, informed consent was obtained from the parent or guardian, and assent was obtained from the participant. If the participant was 18 years or older, consent was obtained from the participant alone. Mothers were ineligible if they had extreme medical, legal, or social problems that precluded their ability to participate in visits or assessments, for example, mothers with medical, psychiatric, or substance abuse problems that required extended hospitalization or residential care off the reservation or legal problems that resulted in incarceration. Also, mothers who were at acute risk for self or others at the time of consent were not eligible.
Mothers were recruited from prenatal and school-based clinics in four Indian Health Service catchment areas on the Navajo and White Mountain Apache reservations in New Mexico and Arizona between May 2002 and May 2004. Follow-up of study participants was completed in May 2005. Incentives in the form of gift cards to a local grocery store were provided to all participants on completion of study assessments.
Sample Size
With power set at 80%, α = .05, and two-tailed tests, the study is able to detect a minimum 5% difference in parenting knowledge scores, the primary outcome, between study groups with a total sample size of 167. Based on our previous study19 a 5% difference was selected as the minimal accepted threshold of success.
Randomization
The randomization sequence, generated by the Web site http://randomization.com was stored confidentially by the data manager in Baltimore, MD. Randomization was revealed to participants after the baseline assessment. Neither the participants nor the interventionists were blind to study group assignment.
Treatment and Control Conditions
The home-visiting procedures for the treatment and control conditions were similar and based on the “Critical Elements” of home visiting put forth by the “Healthy Families America/Indiana” (Healthy Families) protocol.26 “Critical Elements” include early, intensive, and culturally competent services provided by staff who are well trained and supervised; have manageable caseloads; and who are compassionate, nonjudgmental, and interpersonally effective.3,26 All lessons were delivered by well-trained native paraprofessionals using tabletop flip charts to participants in their homes or a confidential setting of the participant’s choice.
Family Spirit Intervention.
The curricular content for the Family Spirit intervention was based on recommendations and standards documented in the American Academy of Pediatrics’ Caring for Your Baby and Child: Birth to Age 5.27 The curriculum includes developmentally timed prenatal and infant-care parenting lessons, as well as family planning, substance abuse prevention, and problem-solving and coping-skills lessons. Mothers were expected to receive 25 home visits, each lasting approximately 1 hour. The Family Spirit curriculum was carefully crafted to reflect local native practices but not community-specific traditions or spiritual beliefs. Tribal stakeholders emphasized that there is a broad spectrum of cultural beliefs and practices within and across tribal sites and supported that the Family Spirit curriculum address the shared needs of all of the participants. In addition, the interventionists were trained to interact in ways that respected the participants’ cultural orientation and living situation. For example, some participants preferred to do the lesson in their native language, whereas others preferred English. Some participants expressed interest in traditional ceremonies and practices covered in the curriculum, whereas others preferred more Western approaches.
Breast-Feeding Nutrition Control Group.
The control group’s curricular content included a previously developed breast-feeding/nutrition education program.28 Mothers were to receive 23 home visits, each lasting approximately 1 hour. The control condition was selected to provide participants a valuable home-visiting experience and hold constant the amount of supportive contact for mothers, so between-group differences could be linked to intervention content.
Interventionists.
Study interventionists were AI women from the local community, bilingual in their native language and English, with at least a high school degree and work experience in health or human services. Interventionists delivered both the Family Spirit intervention and the breast-feeding/nutrition intervention, after receiving approximately 500 hours of training in home-visiting methods and curricular content and demonstrating mastery and fidelity to the study protocol on oral and written examinations. Interventionists also served as evaluators and were specifically trained to administer self-report and observational assessments with objectivity. Appendix A, the Family Spirit Intervention Curriculum Lessons, can be found in the supplemental digital content (online-only) materials at http://admin.links.lww.com/A987. The investigator team worked extensively with the evaluators to develop anchors to standardize observational assessments. Evaluators were approved to administer observational measures when they received an 85% consistency score with anchors. Supervision of the curriculum implementation and assessments occurred daily on site and through weekly conference calls. Quality assurance procedures included direct observation of study interventionists and evaluators quarterly to ensure adherence to the protocol.
Data Collection
Intervention and control groups were assessed at four intervals: baseline (~28 weeks’ gestation), and 2, 6, and 12 months postpartum. Sociodemographic characteristics were gathered in the baseline assessment. Outcome data collected at all four assessment points included maternal self-reports on parenting knowledge, involvement, social support, depression, stress, and substance abuse. Infants’ social and behavioral outcomes and quality/quantity of parent-child interactions were measured in two ways. At 6 and 12 months postpartum, evaluators administered an observational measure of the home environment.29 At 12 months postpartum, mothers completed a parent report questionnaire on their infant’s social and emotional behavior.30
Outcome Measures
Based on our theoretical model, which hypothesized that parenting is the critical link between parent domains and child domains and mediates children’s outcomes,31 primary study outcomes were selected to measure parent’s knowledge gains related to the curriculum and parent involvement, and secondary outcomes included children’s behavior outcomes and maternal factors that could interfere with parent efficacy. The primary and secondary outcome measures were all reviewed and approved by the participating communities and are described below.
Primary Outcome Measures.
Parenting Knowledge (range 0%–100%, Cronbach α = .95). A 76-item multiple-choice self-report test designed by the study team to assess participants’ general knowledge on pregnancy, infant care, and parenting skills. Appendix B, the Parenting Knowledge Test, can be found in the supplemental digital content (online-only) materials at http://admin.links.lww.com/A987.
Parent Involvement (range 5–20, Cronbach α = .65). A 5-item self-report scored on a 4-point scale adapted from Substance Abuse and Mental Health Services Administration measures32 to assess participants’ level of direct involvement in infant care and support. Appendix C, the Parent Involvement Measure, can be found in the supplemental digital content (online-only) materials at http://admin.links.lww.com/A987.
Secondary Outcome Measures.
Home Observation for Measurement of the Environment (HOME) (range 0–45, Cronbach α = .89).29 A 45-item observational checklist that assesses parent support and stimulation of the child in the home environment. Six subscales include Maternal Responsivity, Acceptance, Organization of the Home, Learning Materials, Maternal Involvement, and Variety (i.e. life experiences). It is intended for use at 6-month intervals from 6 to 36 months postpartum and was used at 6 and 12 months in this study. For some study participants, the HOME was completed as interview outside of the home environment because of participant refusal to allow staff in the home or staff safety concerns.
Infant Toddler Social Emotional Assessment (ITSEA) (range 0–2 for individual items and 0–2 for domains; Cronbach α range 0.71–0.83).30 A 126-item parent report that assesses four primary domains of child behavior for ages 12 to 36 months including Externalizing, Internalizing, Dysregulation, and Competence. It was conducted at 12 months postpartum and was the first use of the ITSEA within our participant populations.
The Center for Epidemiological Studies–Depression (range 0–60, Cronbach α = .88).33 A 20-item self-report scored on a 4-point scale to measure participants’ level of depressive symptoms.
Substance Use (not applicable—proportions are reported). Three self-report items developed by Substance Abuse and Mental Health Services Administration regarding participants’ use of alcohol, cigarettes, or illegal substances in the previous month.34
Social Support (range 20–100, Cronbach α = .93).35 A 20-item self-report scored on a 5-point scale designed to measure participants’ perceived support from family, friends, and community.
Parenting Stress Index (range 30–150, Cronbach α = .80).36 A 30-item self-report scored on a 5-point scale measuring participants’ level of stress associated with parenting. As this index is only relevant after the child’s birth, it was not collected at baseline.
Data Analysis
Multivariate generalized linear mixed models (GLMMs) were used to determine whether study outcomes were associated with intervention receipt. The GLMMs allow repeated measures for each individual to be modeled simultaneously such that the estimated SEs are fully efficient, and the treatment effect for each change because baseline can be estimated. Each regression model was adjusted for any variables found to be imbalanced between intervention and control groups at baseline and potential confounders, as suggested by comparable studies1,37 (including age, parity, gestational age, educational status, whether the participant resided with her partner, whether her partner was also enrolled in the Family Spirit program, and study site). Regression models also examined site-by-treatment interactions, which were inconclusive. Unstandardized β regression coefficients are presented for continuous outcomes, which represent the amount of difference in the outcome value seen between those who received the intervention versus those in the control group. Adjusted odds ratios are reported for binary outcomes. All analyses followed an intent-to-treat approach, irrespective of the actual amount of intervention received. The GLMMs allowed for the inclusion of individuals who lacked complete data for all three follow-up time points. For example, if an individual was missing the 6-month time point but had data for the 2- and 12-month time point, they were included in the analysis for the 2- and 12-month analysis, but their data were considered missing for the 6-month time point.
Rates of attrition were compared across study group at each time point using χ2 tests. At each time point, those lost to follow-up were compared with those remaining in the study, by study group and for the entire sample. Exploratory stratified analyses examined the two major demographic variables shown in previous home-visiting trials2 to moderate intervention outcome: age (younger [14–17 years] versus older [18–22 years]) and educational status (not completed versus completed high school or equivalent).
With the exception of the ITSEA outcomes, p values adjusted for multiple comparisons using the false discovery rate correction are reported. Because this was the first time we had used the ITSEA instrument in this population, we treated the ITSEA outcomes as pilot data and did not adjust for multiple comparisons. The GLMMs and multiple corrections were conducted using SAS 9.1. The ITSEA analysis and all other analyses were conducted using Stata 8.2 (Stata Corporation, College Station, TX).
RESULTS
Participant Flow
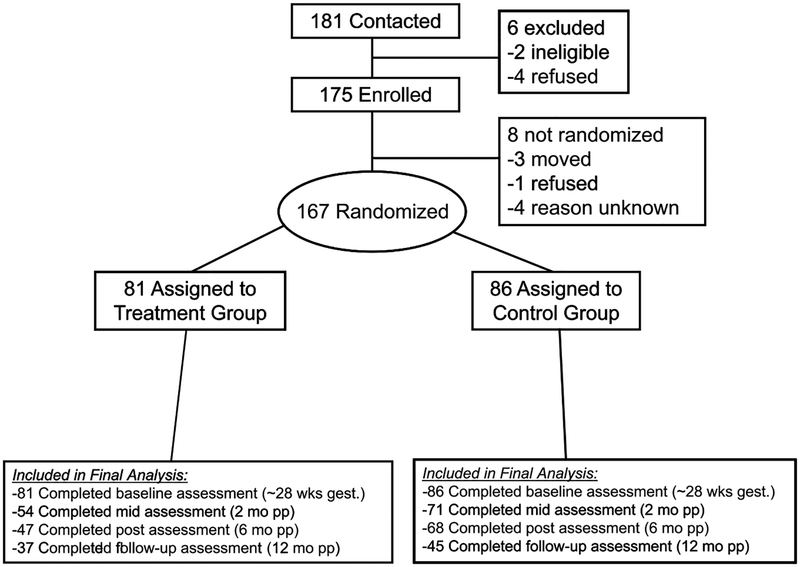
Of the 181 women initially contacted, 175 (97%) were eligible and agreed to enroll (Fig. 1).38 Of the 175 enrolled, 167 (95%) were randomized, with 81 participants assigned to the Family Spirit arm and 86 to the control arm. Attrition rates were significantly higher among treatment versus control group mothers at 2 months (33% versus 17%, p < .05) and 6 months (42% versus 21%, p < .01). Rates of attrition were similar for both groups at 12 months (54% versus 48%, p = .39). For the entire sample and within each study group, participants lost to follow-up at 2, 6, or 12 months were not different in baseline demographic characteristics or outcome variables from those still in the study at these time points.
Fig. 1.
Flow of participants through the study.
Participant Characteristics
Randomized participants ranged in age from 14 to 22 years, with a median age of 18.0 years. All were AI, primarily Navajo (65%), White Mountain Apache (18%), or from mixed tribes. The majority of mothers (87%) were less than 20 years old at the time of conception. The majority of women (84%) had gestational ages of less than 28 weeks at the time of enrollment. Subsequent to enrollment, 16% of the participants were found to have gestational ages older than 28 weeks (range 29–35 weeks) because of corrections in their expected due dates. At enrollment, 8% were married, and 10% had one or more children. Slightly more than one third (39%) of the sample had completed high school, a general equivalency diploma, or some college, and 12% were employed. At baseline, 68% of the participants were living with their male partners, and 72% were living with their parents or the baby’s father’s parents (Table 1).
TABLE 1.
Selected Sociodemographic Characteristics of Participants at Baseline, by Study Group
| Sociodemographic Characteristics | Control (n = 86) n (%) | Treatment (n = 81) n (%) | Total (n = 167) n (%) |
|---|---|---|---|
| Age at time of conception (range 14–22 y) | |||
| 14–17y | 43 (50) | 36 (44) | 79 (47) |
| 18+ y | 43 (50) | 45 (56) | 88 (53) |
| Parity: ≥1 | 8 (9) | 8 (10) | 16 (10) |
| Education: high school/general equivalency diploma/some college | 35 (41) | 31 (38) | 66 (39) |
| Currently married | 5 (6) | 9 (11) | 14 (8) |
| Male partner enrolled in program | 45 (52) | 35 (43) | 80 (48) |
| Living situation | |||
| Live in same household as parents | 58 (67) | 63 (78) | 121 (72) |
| Live in same household as partner | 63 (73) | 50 (62) | 113 (68) |
| Gestational age (range 3–35 wk) | |||
| ≤20 wk | 53 (62) | 39 (48) | 92 (55) |
| 21–28 wk | 19 (22) | 30 (37) | 49 (29) |
| 29+ wk | 14 (16) | 12 (15) | 26 (16) |
| Currently employed | 11 (13) | 9 (11) | 20 (12) |
Intervention and control participants were similar with respect to all baseline demographic characteristics (Table 1), and all outcome variables except intervention mothers had slightly higher baseline parenting knowledge (mean 45.4 versus 42.0, p < .05). Baseline demographic characteristics and outcome scores did not vary across sites.
Dose of Intervention
Treatment group mothers completed a median of 20 of 25 (80%) expected home visits. Control group mothers completed a median of 21 (91%) of 23 expected home visits.
Primary Outcomes
Adjusting for potential confounders and for multiple comparisons, treatment mothers’ mean increase in parenting knowledge at 6 and 12 months was 13.5 (p < .0001) and 13.9 (p < .0001) points higher, respectively, than mothers in the control group (Table 2). Knowledge gains among treatment mothers at 2 months post-partum trended positively (β = 3.1, p = .07). No significant differences between study groups were seen for maternal involvement at any time point.
TABLE 2.
Means, SDs, and Mean Differences in Maternal Study Outcomes Tretment and Control Groups at 2, 6, and 12 Months Postpartum, Adjusted for Covariated and for Multiple Comparison Testing
| 2 Months Postpartum (n = 71 Control, n = 54 Treatment) | 6 Months Postpartum (n = 68 Control, n = 47 Treatment) | 12 Months Postpartum (n = 45 Control, n = 37 Treatment) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Study Outcome | Control Mean (SD) |
Treatment Mean (SD) |
βa (95% CI) | Control Mean (SD) |
Treatment Mean (SD) |
βa (95% CI) | Control Mean (SD) |
Treatment Mean (SD) |
βa (95% CI) |
| Change in parenting knowledge | 2.6 (9.9) | 3.2 (10.4) | 3.10† (0.65–5.55) | 12.8 (14.3) | 23.8 (12.1) | 13.46** (9.28–17.65) | 15.2 (14.0) | 26.6 (12.1) | 13.92** (9.01–18.83) |
| Change in maternal involvement | 1.2 (2.3) | 1.1 (2.8) | −.06 (−1.04 to 0.93) | 1.2 (2.7) | 1.3 (3.4) | −.15 (−1.16 to 0.86) | 0.6 (2.3) | 1.0 (3.0) | .22 (−0.87 to 1.31) |
| Change in social support | −1.7 (19.1) | −0.4 (20.5) | −.21 (−7.63 to 7.20) | −2.5 (19.2) | −3.7 (21.0) | −.98 (−8.63 to 6.68) | −2.2 (19.6) | 0.5 (23.4) | 1.98 (−6.55 to 10.52) |
| Change in depressive symptoms | −3.3 (10.7) | −2.0 (11.8) | .05 (−3.99 to 4.09) | −4.0 (10.7) | −4.0 (12.2) | −.58 (−4.71 to 3.55) | −2.0 (11.8) | −3.1 (9.7) | −1.69 (−6.29 to 2.91) |
| Parenting stress index | 66.8 (17.9) | 62.3 (16.0) | −3.31 (−9.69 to 3.08) | 64.1 (17.2) | 63.3 (17.1) | 1.01 (−5.78 to 7.80) | 60.4 (15.2) | 62.6 (17.1) | 3.91 (−2.79 to 10.61) |
| Home observation for measurement of the environment | NA | NA | NA | 33.4 (7.2) | 32.5 (5.5) | −1.27 (−4.08 to 1.54) | 37.4 (6.2) | 37.1 (7.2) | −.04 (−3.15 to 3.08) |
| n (%) | n (%) | Odds Ratiosb (95% CI) | n (%) | n (%) | Odds Ratiosb (95% CI) | n (%) | n (%) | Odds Ratiosb (95% CI) | |
| Alcohol in last month | 5 (7) | 6 (11) | 1.52 (0.42–5.46) | 4 (6) | 5 (12) | 2.19 (0.55–8.78) | 6 (13) | 7 (19) | 1.54 (0.45–5.27) |
| Cigarette in last month | 12 (17) | 7 (13) | 0.74 (0.24–2.30) | 8 (13) | 9 (22) | 2.06 (0.64–6.62) | 7 (15) | 7 (19) | 1.27 (0.34–4.72) |
| Illegal substance in last month | 5 (7) | 7 (13) | 2.02 (0.51–7.92) | 2 (3) | 3 (7) | 2.57 (0.37–18.00) | 4 (9) | 6 (16) | 2.37 (0.51–10.99) |
Note: CI = confidence interval; NA = not applicable.
The unstandardized β regression coefficient represents the mean difference in the outcome value seen between those who received the intervention versus those who were in the control group.
The odds ratio represents the odds of outcome occurrence in the treatment group compared with the control group.
p < .01;
p < .1.
Secondary Outcomes
Family Spirit mothers reported their infants’ behavioral development as significantly better on several dimensions measured by the ITSEA (Table 3) including lower activity and impulsivity (β = −.27, p < .01), lower peer aggression (β = −.23, p < .01), lower overall externalizing behaviors (β = −.17, p < .05), and less separation distress (β = −.17, p < .05). No significant between-group differences were seen in HOME scores, maternal social support, depressive symptoms, substance abuse, or parenting stress at any time point.
TABLE 3.
Means, SDs, and Mean Differences in ITSEA Outcomes Between Treatment and Control Groups at 12 Months Postpartum, Adjusted for Covariates
| ITSEA Outcomes (Range for All 0–2) | 12 Months Postpartum | ||
|---|---|---|---|
| Control Mean (SD) (n = 30) | Treatment Mean (SD) (n = 35) | βa (95% CI) | |
| Externalizing domain | 0.57 (0.27) | 0.39 (0.29) | −.17 (−0.30 to −0.04)* |
| Activity/impulsivity | 0.98 (0.44) | 0.69 (0.44) | −.27 (−0.47 to −0.07)* |
| Aggression/defiance | 0.35 (0.26) | 0.27 (0.29) | −.06 (−0.19 to 0.08) |
| Peer aggression | 0.30 (0.29) | 0.13 (0.20) | −.23 (−0.40 to −0.07)* |
| Internalizing domain | 0.55 (0.23) | 0.48 (0.16) | −.06 (−0.16 to 0.04) |
| Depression/withdraw | 0.15 (0.21) | 0.12 (0.23) | .01 (−0.11 to 0.11) |
| General anxiety | 0.21 (0.23) | 0.20 (0.22) | .01 (−0.11 to 0.13) |
| Separation distress | 1.02 (0.39) | 0.84 (0.30) | −.17 (−0.33 to −0.02)* |
| Inhibition to novelty | 0.82 (0.38) | 0.73 (0.36) | −.09 (−0.28 to 0.11) |
| Dysregulation domain | 0.49 (0.26) | 0.43 (0.27) | −.05 (−0.18 to 0.08) |
| Sleep | 0.53 (0.39) | 0.44 (0.33) | −.06 (−0.24 to 0.13) |
| Negative emotionality | 0.48 (0.25) | 0.47 (0.32) | .02 (−0.13 to 0.17) |
| Eating | 0.44 (0.25) | 0.43 (0.30) | −.02 (−0.16 to 0.12) |
| Sensory sensitivity | 0.52 (0.42) | 0.37 (0.31) | −.14 (−0.30 to 0.02) |
| Competence domain | 0.95 (0.33) | 0.94 (0.36) | −.01 (−0.19 to 0.18) |
| Compliance | 0.84 (0.40) | 0.91 (0.38) | .10 (−0.11 to 0.31) |
| Attention | 1.07 (0.48) | 1.11 (0.51) | .05 (−0.21 to 0.32) |
| Imitation/play | 1.10 (0.42) | 1.08 (0.41) | −.03 (−0.26 to 0.20) |
| Mastery motivation | 1.34 (0.42) | 1.30 (0.51) | −.05 (−0.30 to 0.20) |
| Empathy | 0.59 (0.41) | 0.66 (0.52) | .09 (−0.15 to 0.33) |
| Prosocial peer relations | 0.79 (0.41) | 0.51 (0.40) | −.24 (−0.51 to 0.02) |
Note: CI = confidence interval; ITSEA = Infant Toddler Social Emotional Assessment.
The unstandardized β regression coefficient represents the mean difference in the outcome value between those who received the intervention versus those who were in the control group.
p < .05.
Exploratory Stratified Analyses
Subsequent analyses explored if age or educational status modified intervention outcomes. Older treatment group mothers (i.e., 18–22 years) experienced significant increases in parenting knowledge at all three time points 2 months (β = 4.71, p < .01); 6 months (β = 16.28, p < .001); and 12 months (β = 14.62, p < .001) and significantly less parenting stress at 2 months postpartum (β = −10.39, p < .05). In addition, older treatment mothers had significantly fewer depressive symptoms at 6 months postpartum (β = −4.14, p < .05). Similarly, among more educated mothers (i.e., completed high school or equivalent) regardless of age, treatment mothers reported significantly fewer depressive symptoms (β = −6.60, p < .05) and less parenting stress (β = −19.55, p < .001) at 2 months postpartum.
DISCUSSION
This study had several potential limitations. First, attrition rates particularly among treatment group mothers were higher than anticipated. High attrition rates were likely related to participant factors such as Family Spirit intervention time burden and transient living status postdelivery. Also, the attrition prevention protocol for this study did not include maintaining contact with participants or reengaging mothers who missed multiple consecutive sessions. Although mothers lost to follow-up were similar in observed baseline characteristics and outcome variables from those still in the study at all assessment time points, the imbalance in attrition rates between study groups may have biased results if mothers lost to follow-up had between-group differences that we did not measure. Second, there were also some limitations in our assessments and assessment administration. Primarily, we relied largely on maternal self-reports and parent reports on children for outcome measures and did not engage additional informants. In addition, the parenting knowledge test was designed for this and our previous pilot study to ascertain knowledge gains specific to curricular content. We did not evaluate the psychometric properties of the knowledge test. We also did not use independent evaluators for the HOME observational measure because of resource limitations and our preference for maintaining trust with enrolled mothers for this first-ever use of a home-based observational measures within the participating communities. Finally, we did not implement an interrater reliability check among those who scored the HOME because of resource constraints. Third, several assessments, including maternal self-reports and the HOME, seemed to have ceiling effects. Ceiling effects on self-reports may be due to participant bias to provide socially or culturally conforming responses. Ceiling effects on the HOME may be linked to the fact that evaluators scored HOME items based on their perception of community norms rather than comparison to suggested norms for HOME items.29
Choice of control condition was both a weakness and strength in this study. From a clinical trials perspective, the home-visiting, breast-feeding/nutrition education program may have positively benefitted outcomes targeted by the Family Spirit intervention, making treatment effects more difficult to detect. From a Community-Based Participatory Research perspective, the inclusion of an active control condition was positive because it assured all participants meaningful and appropriate services. The control condition was highly valued in the participating communities where needs are prevalent and a history of exploitative research predominates collective memory. In subsequent studies, the control group must be designed to both provide a meaningful experience for participants while allowing for clear inferences about the Family Spirit intervention benefit.
Primary Outcomes
Mothers in the treatment group experienced greater knowledge gains than mothers in the control group at 6 and 12 months postpartum with a positive trend at 2 months. These significant between-group differences replicate findings from our earlier study and confirm the capacity of AI paraprofessionals to engage and educate a sample of AI teen mothers. Higher knowledge scores in the treatment group also provide evidence that the treatment and control conditions were appropriately differentiated from each other in implementation. Furthermore, knowledge scores were inversely correlated with infant behavioral outcomes (Pearson r range of −0.2 to −0.5), such that the higher the knowledge score, the fewer infant behavioral problems. Future studies with longer term follow-up will be required to determine whether mothers’ early knowledge gains are proximal markers for distal health and behavior changes for them and their children.
No differences in parent involvement were seen at any time point. Involvement scores at baseline were higher than anticipated for all participants, making it difficult to detect significant gains over time or identify between-group differences.
Secondary Outcomes
Treatment mothers compared with control mothers reported via the ITSEA that their infants had significantly fewer behavioral difficulties at 1 year of age, including lower activity/impulsivity and peer aggression; lower overall externalizing behavior; and less separation distress in the internalizing domain. To our knowledge, this is the first report of positive infant behavior outcomes in the home-visiting literature. Given the validity of the ITSEA to identify externalizing problems in infancy39 that persist in later childhood13,14 and the consistent link of externalizing problems to early parenting practices,17,31,40 this low-cost, paraprofessional-delivered, home-visiting intervention holds promise for reducing important behavioral health disparities for AI children.20,41
Because the HOME has been a primary outcome measure in many home-visiting studies, the lack of between-group differences in HOME scores at 6 and 12 months postpartum is important to consider. First, other large home-visiting studies have not been able to identify positive impacts in HOME scores until children were at least 2 years of age.1,4 The lack of HOME findings among the 1-year-olds in these studies as well as our own may suggest that many HOME items may not be developmentally relevant to infants (e.g. “[does child have] toys for literature and music”). Second, HOME scores for both groups (~73% at 6 months and ~82% at 12 months) were high, given the disadvantaged circumstances of the participants. During training, study evaluators expressed discomfort with evaluating parent-child interactions and home environments negatively for what is considered normative for their communities. For example, they noted that some items were culturally irrelevant (e.g., the HOME scores positively for pets in the home, but pets are preferentially kept outside in the participating communities) and may be biased against economically depressed families (e.g., “Child has a special place for toys and treasures”). To address these challenges in future studies, we recommend collecting HOME data over a longer period of early childhood (up to 48 months postpartum); employing independent raters who are well trained in the use of culturally, socioeconomically, and developmentally appropriate anchors for HOME ratings and who undergo regular interrater reliability checks; and including adaptations of the HOME for socioeconomically disadvantaged families such as the Supplement to the HOME for Impoverished Families.42
Although the trend for decreased depression scores for all treatment mothers in our previous study was not replicated, we observed lower depression scores among older and more educated treatment mothers in this study. We hypothesize that older and more educated AI mothers may respond more readily to core treatment components and/or relate better to measures of mood and stress than younger, less educated mothers. Potential moderator effects of age and education warrant more formal investigation in future research.
In both groups, the participants’ substance use was consistent with national and local data suggesting that AI teens and young adults are vulnerable to substance use. At baseline, 13% of the participants had used alcohol or drugs within the past month, despite being pregnant. Alcohol use seemed to increase in both groups over time, which may be a result of the participants’ increasing comfort with revealing their substance use as the study progressed or the initiation/reinitiation of alcohol use postdelivery or as they aged. This trial points to the need for specifically targeting drug prevention for teen mothers in pregnancy and postpartum periods.
It is well established that AI communities are disparately challenged by behavioral health problems precipitated by a myriad of historical and environmental factors, and there are insufficient clinical resources or proven community-based interventions to address those problems.43 Demonstrating the effectiveness of paraprofessionals in rural U.S. communities that have nursing shortages and few trained professionals makes an important public health contribution, addresses behavioral health and clinical resource disparities in native communities, and counters concerns about the use of paraprofessionals as home visitors.
Although prevention research that uses evidence-based and culturally congruent solutions is desperately needed, Indian communities remain extremely cautious of research because of a history of abuses. Through the use of community-based participatory research methods, this study breaks new ground in designing, implementing, and evaluating paraprofessional delivered in-home interventions and supports future tribal-academic partnerships in behavioral intervention research.
Acknowledgments
Disclosure: Dr. Walkup has received research grant support from Eli Lilly, Pfizer, and Abbott. He has been a consultant to GlaxoSmithKline, Eli Lilly, and the Cliff’s Communities. He has received speaker’s honoraria from the Tourette Syndrome Association. The other authors report no conflicts of interest.
Financial support for this work was provided by the Substance Abuse Mental Health Services Administration (SAMHSA I: Grant No. UD1SP08860, SAMHSA II: Grant No. UD1SP09588), and the Ford Foundation, the Annie E. Casey Foundation, and the C.S. Mott Foundation. The PI for this work, John Walkup, M.D., had full access to the study data and takes responsibility for the data integrity and accuracy of the analyses.
The authors thank the Navajo and White Mountain Apache mothers, children, and families who participated in this study. The authors also thank the Navajo and White Mountain Apache leaders and community stakeholders who generously contributed time and wisdom to designing the Family Strengthening intervention and research protocol and reviewing the article. The authors also thank the Indian Health Service colleagues for their long-standing collaboration in health prevention research and service and for their review of the research and article.
Footnotes
This article was reviewed under and accepted by Ad Hoc Editor Bonnie T. Zima, M.D., M.P.H.
Supplemental digital content for this article can be found online only. See text for specific links.
This article is the subject of an editorial by Dr. Douglas K. Novins in this issue.
Clinical trial registry information—Family Spirit Study. URL: http://www.clinicaltrials.gov. Unique identifier: NCT00356551.
REFERENCES
- 1.Olds DL, Robinson J, Pettitt L et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics. 2004;114:1560–1568. [DOI] [PubMed] [Google Scholar]
- 2.Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. Am Psychol. 2003;58:457–465. [DOI] [PubMed] [Google Scholar]
- 3.Olds DL, Sadler L, Kitzman H. Programs for parents of infants and toddlers: recent evidence from randomized trials. J Child Psychol Psychiatry. 2007;48:355–391. [DOI] [PubMed] [Google Scholar]
- 4.Olds DL, Robinson J, O’Brien R et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002;110:486–496. [DOI] [PubMed] [Google Scholar]
- 5.US DHHS. Trends in Indian health, 2000–2001. 2004. Rockville, Public Health Service, Indian Health Service, US Government Printing Office. [Google Scholar]
- 6.Brink S, Martin R, Golden D, Smith L. Primary pediatric care: a comparison of use by adolescent and older mothers. J Adolesc Health Care. 1985;6:201–205. [DOI] [PubMed] [Google Scholar]
- 7.Bodurtha J Testimony of the American Academy of Pediatrics before the Senate Committee on Indian Affairs on “A Partnership for a New Millennium: Addressing the Unmet Health Care Needs in Indian Country.” 1998.
- 8.Liu LL, Slap GB, Kinsman SB, Khalid N. Pregnancy among American Indian adolescents; reactions and prenatal care. J Adolesc Health. 1994; 15:336–341. [DOI] [PubMed] [Google Scholar]
- 9.Blum RW, Harmon B, Harris L, Bergeisen L, Resnick MD. American Indian-Alaska Native youth health. JAMA. 1992;267:1637–1644. [DOI] [PubMed] [Google Scholar]
- 10.Beauvais F Trends in Indian adolescent drug and alcohol use. Am Indian Alask Native Ment Health Res. 1992;5:1–12. [DOI] [PubMed] [Google Scholar]
- 11.Hill A Treatment and prevention of alcoholism in the Native American family In: Larson GW, Lawson AW, eds. Alcoholism and Substance Abuse in Special Populations. Rockville: Aspen; 1989. [Google Scholar]
- 12.King J, Thayer JF. Examining conceptual models for understanding drug use behavior among American Indian youth In: Trimble JE, Padilla A, Bell CS, eds. Drug Abuse Among Ethnic Minorities. Rockville: US Department of Health and Human Services; 1987. [Google Scholar]
- 13.Briggs-Gowan MJ, Carter AS, Bosson-Heenan J, Guyer AE, Horwitz SM. Are infant-toddler social-emotional and behavioral problems transient? J Am Acad Child Adolesc Psychiatry. 2006;45:849–858. [DOI] [PubMed] [Google Scholar]
- 14.Van Zeijl J, Mesman J, Van IJzendoom MH et al. Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: a randomized controlled trial. J Consult Clin Psychol. 2006;74:994–1005. [DOI] [PubMed] [Google Scholar]
- 15.Shaw DS, Winslow EB, Owens EB, Vondra JI, Cohn JF, Bell RQ. The development of early externalizing problems among children from low-income families: a transformational perspective. J Abnorm Child Psych. 1998;26:95–107. [DOI] [PubMed] [Google Scholar]
- 16.Patterson GR. Continuities–a search for causal mechanisms: comment on the special section. Dev Psychol. 1998;34:1263–1268. [DOI] [PubMed] [Google Scholar]
- 17.Shaw DS, Bell RQ, Gilliom M. A truly early starter model of antisocial behavior revisited. Clin Child Fam Psychol Rev. 2000;3:155–172. [DOI] [PubMed] [Google Scholar]
- 18.Dishion TJ, Shaw D, Connell A, Gardner F, Weaver C, Wilson M. The family check-up with high-risk indigent families: preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Dev. 2008;79:1395–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barlow A, Varipatis-Baker E, Speakman K et al. Home-visiting intervention to improve child care among American Indian adolescent mothers. Arch Pediatr Adolesc Med. 2006;160:1101–1107. [DOI] [PubMed] [Google Scholar]
- 20.Barlow A, Walkup J. The First Americans have much to teach us. J Am Acad Child Adolesc Psychiatry. 2008;47:843–844. [DOI] [PubMed] [Google Scholar]
- 21.Emond A, Pollock J, Da CN, Maranhao T, Macedo A. The effectiveness of community-based interventions to improve maternal and infant health in the Northeast of Brazil. Rev Panam Salud Publica. 2002;12: 101–110. [DOI] [PubMed] [Google Scholar]
- 22.Walt G, Ross D, Gilson L, Owur-Omondi L, Knudsen T. Community health workers in national programmes: the case of the family welfare educators in Botswana . Trop R Soc Trop Med Hyg. 1989;83:49–55. [DOI] [PubMed] [Google Scholar]
- 23.Lam TK, McPhee SJ, Mock J et al. Encouraging Vietnamese-American women to obtain pap tests through lay health worker outreach and media education. J Gen Intern Med. 2003;18:516–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jack S, DiCenso A, Lohfield L. Opening doors: factors influencing the establishment of a working relationship between paraprofessional home visitors and at-risk families. Can J Nurs Res. 2002;34:59–69. [PubMed] [Google Scholar]
- 25.Barbosa RH, Cavalcanti C, Cabral CD et al. Urban women educate their community on HIV/STDs, family planning and reproductive health. Sex Health Exch. 1998;3:9–13. [PubMed] [Google Scholar]
- 26.Healthy Families America Web site. www.healthyfamiliesamerica.org. 2008.
- 27.Shelov SP, Hannemann RE, Trubo R, Agran PF, Altmann TR, Baker SS. Caring for Your Baby and Young Child: Birth to Age 5 Revised Edition New York: Bantam; 2004. [Google Scholar]
- 28.Barlow A, Varipatis-Baker E, Speakman K et al. Home-visiting intervention to improve child care among American Indian adolescent mothers. Arch Pediatr Adolesc Med. 2006;160:1101–1107. [DOI] [PubMed] [Google Scholar]
- 29.Caldwell BM, Bradley RH. Home Inventory Administration Manual. Little Rock: University of Arkansas for Medical Sciences and University of Arkansas at Little Rock; 1979. [Google Scholar]
- 30.Carter AS, Briggs-Gowan MJ. Infant-Toddler Social and Emotional Assessment (ITSEA) Manual. New Haven: Yale University, Department of Psychology; 1999. [Google Scholar]
- 31.Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. Am Psychol. 1989;44:329–335. [DOI] [PubMed] [Google Scholar]
- 32.SAMHSA. Mentoring and Family Strengthening Cross-Site Instrument Baseline Administration Guidelines SAMHSA. Rockville: US DHHS; 2002. [Google Scholar]
- 33.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychol Meas. 1977;1:385–401. [Google Scholar]
- 34.SAMHSA. Center for Substance Abuse and Prevention GPRA Attitudes and Beliefs–Youth (2005). Rockville: SAMHSA; 2005. [Google Scholar]
- 35.Moore KA, Zaslow MJ, Coiro MJ, Miller SM. How Well Are They Faring? AFDC Families With Preschool Aged Children in Atlanta at the Onset of the JOBS Evaluation. Washington: US Department of Health and Human Services and US Department of Education, 1995. [Google Scholar]
- 36.Abidin RR. Parenting Stress Index. 3rd ed Odessa: Psychological Assessment Resources; 1995. [Google Scholar]
- 37.Olds DL. Prenatal and infancy home visiting by nurses: from randomized trials to community replication. Prev Sci. 2002;3:153–172. [DOI] [PubMed] [Google Scholar]
- 38.Moher D, Schulz KF, Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–1991. [DOI] [PubMed] [Google Scholar]
- 39.Carter AS, Briggs-Gowan MJ, Davis NO. Assessment of young children’s social-emotional development and psychopathology: recent advances and recommendations for practice. J Child Psychol Psychiatry. 2004;45: 109–134. [DOI] [PubMed] [Google Scholar]
- 40.Shaw DS, Owens EB, Giovannelli J, Winslow EB. Infant and toddler pathways leading to early externalizing disorders. J Am Acad Child Adolesc Psychiatry. 2001;40:36–43. [DOI] [PubMed] [Google Scholar]
- 41.Whitbeck LB, Yu M, Johnson KD, Hoyt DR, Walls ML. Diagnostic prevalence rates from early to mid-adolescence among indigenous adolescents: first results from a longitudinal study. J Am Acad Child Adolesc Psychiatry. 2008;47:890–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ertem IO, Forsyth BW, vni-Singer AJ, Damour LK, Cicchetti DV. Development of a supplement to the HOME Scale for children living in impoverished urban environments. J Dev Behav Pediatr. 1997;18: 322–328. [DOI] [PubMed] [Google Scholar]
- 43.Barlow A, Walkup J. Developing mental health services for Native American children. Child Adolesc Psychiatr Clinics North Am. 1998;7: 555–577. [PubMed] [Google Scholar]