Abstract
Specialists, who represent 60% of physicians in the United States, are consolidating into large group practices, but the degree to which group practice type facilitates the delivery of high quality of care in specialty settings is unknown. We conducted a systematic literature review to identify the impact of group practice type on the quality of care among specialty providers. The search resulted in 913 articles, of which only 4 met inclusion criteria. Studies were of moderate methodological quality. From the limited evidence available, we hypothesize that solo specialists deliver care that is inferior to their peers in group practice, whether measured by patient satisfaction ratings or adherence to guideline-based care. However, solo specialists and multidisciplinary group specialists may be more likely to provide some specialized services compared with their single-specialty group peers. Insufficient research compares quality of care among different practice types in specialty care. Substantial opportunity exists to test the degree to which organizational factors, whether size of practice or the mix of providers within the practice, influence quality of care in specialty settings.
Keywords: specialization, group practice, private practice, quality of health care, specialty, multispecialty, specialty care, single specialty, solo practice
What do we already know about this topic?
Practice type is a commonly used organizational characteristic in studies of health care delivery. Its impact on quality of care varies based on how quality is defined.
How does your research contribute to the field?
This is the first study to isolate the effect of practice type in specialty care settings and highlights the limited research conducted on quality of care in specialty care settings.
What are your research’s implications toward theory, practice, or policy?
Too few studies consider practice type to determine whether it is an important construct in influencing quality of care in specialty settings. Thus, policy imperatives for practice consolidation to improve quality may be ill founded.
Introduction
Physicians have been increasingly impelled in recent decades, to consolidate—either into single-specialty groups or multispecialty groups—by market forces, reimbursement policy, geographic trends, and physician’s own preferences.1 While consolidation affords physicians greater market power to negotiate price with payers2 and new physicians are attracted into larger group practices by the benefits afforded by these practice models,1 payment models based on accountable care organizations, bundled payments, and medical homes promote consolidation and incentivize physicians to consolidate under the presumption that integration will improve quality of care.1 Despite this encouragement, little empirical evidence exists to suggest that practice consolidation improves quality of care2 and the exact mechanism by which practice structure brings about improvements is unclear. Some observational evidence suggests that physicians in group practice may deliver higher quality processes of care than solo practitioners.3 However, most research on factors influencing quality of care has been limited to primary care settings.4
Although most physician visits are with primary care providers, approximately 60% of the 685 000 physicians in the United States are specialists,5 and a disproportionate amount of health care spending is for specialty care.6 Specialty group practice dominates as the most common type of practice arrangement,5 largely because US health policy has privileged specialty care over primary care.7 Societal support of specialty training programs, hospital infrastructure, disparate reimbursement strategies, and the development and evolution of academic medical centers over the last century have led to specialists’ growth in number, status, and wealth relative to primary care providers.7,8 Furthermore, a longstanding assumption that specialists deliver higher quality of care than their nonspecialist counterparts persists,9 but whether purported differences in quality stem from training differences, variation in the types of conditions treated, or organizational differences between primary and specialty practice is unknown.4 Thus, identifying whether organizational features produce similar results in specialty care as they do in primary care will help to narrow the potential causes of this variation.
Unfortunately, few studies invest in primary data collection of validated organizational measures and rather rely on extant organizational characteristics found in secondary data sets. One of the most prevalent constructs used in secondary analysis and some surveys is “practice type,” derived from insurance claims and codified in the National Plan & Provider Enumeration System.10 In this context, practice type refers to solo specialty, single-specialty group, or multispecialty group.10
Because little is known about the effect of physician consolidation on quality of care among specialists, we sought to isolate and synthesize the current literature regarding the influence of practice type on quality of care among specialists. This review is intended to form the evidence base that might be insightful for researchers and policy makers concerned about health care delivery system reform through physician group organization.
Conceptual Framework
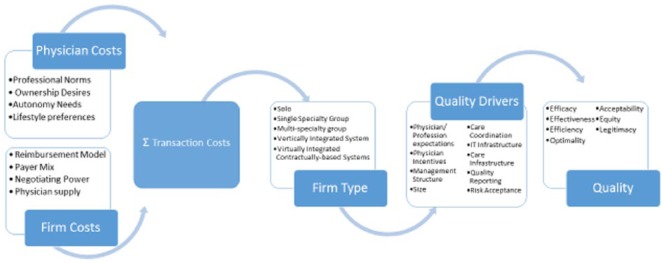
The conceptual framework for organizing this review (Figure 1) is derived from the transaction cost approach as a means to understand the structure of an organization.11 This theory suggests that transactional costs within the market will drive the boundaries of the organization (ie, the size and composition) as well as the employment relations within the organization.11 We highlight potential intrapersonal and organizational level transaction cost drivers which, as a whole, have a total transaction cost which can drive individual physicians’ entry into a particular organization or motivate existing firms to change their structure. Thus, these drivers produce health care practices organized by size and provider mix, resulting in practice types ranging from solo practice, group practice, and mixed specialty group practice. These organizational structures simultaneously shape the quality resources within the organization, ultimately influencing quality of care, and, along with internal transaction cost drivers, influence the “costliness” of transactions required to deliver high-quality care, Nonetheless, within each of these organizational types, there are factors independent of practice type that influence quality, including the size of the group practice (beyond the 1 versus many distinction implied by solo versus group), the quality of the management, influence of the members’ profession, and the degree of risk the firm accepts in delivering quality outcomes.12-14
Figure 1.
Conceptual model of firm integration’s effects on quality.
The quality of care outcomes which may or may not result from the care delivered are drawn from the Donabedian characterization of how quality is produced. This definition of quality has been utilized for many studies focusing on quality improvement15 and formed the basis for the Health and Medicine Division of the National Academy of Medicine (formerly Institute of Medicine) definition of quality put forth in the seminal work Crossing the Quality Chasm.16 As with the National Academy of Medicine, the outcomes specified by Donabedian15 are defined from the patient perspective.16 Efficacy refers to the ability of health science and technology to bring about improvements in health. Effectiveness is the degree to which attainable improvements in health are attained and is dependent on the extent to which available knowledge and technology are used or misused in the management of illness.17 This is often measured by the level of guideline adherence.16 Thus, we considered delivery of a guideline-based procedure as a proxy for the effectiveness of care. Efficiency is the ability to lower care costs without diminishing attainable improvements in health. Optimality is the balancing of improvements in health against the costs of improvements. Acceptability assesses the degree to which care confirms to the wishes, desires, and expectations of patients and their families. Equity, the lone societal outcome, is the degree to which care conforms to a principle that determines what is just and fair in the distribution of health and its benefits among members of the population. Legitimacy measures conformity to social preferences expressed by ethical principles, values, norms, mores, laws, and regulations.15
New Contribution
This review comprehensively examines the literature assessing the influence of physician group practice type on quality of care in specialty practice. Despite the acknowledged influence of practice organization on care delivery and adoption of quality initiatives, most research has focused on individual physicians’ characteristics and ignored organizational factors which influence physician behavior.18 This previous literature has focused on medicine as a profession,19 individual physician attitudes,20 demographic characteristics of individual physicians,21,22 or training characteristics.23,24 Moreover, when physician organization has been studied, the outcomes of interest have rarely included quality of care but have been limited to cost (absent any assessment of benefits), provider efficiency, payment, and provider productivity.19 Finally, the research upon which assumptions about the effect of practice organization type on quality of care have been formed has been limited to primary care settings.3
Methods
This systematic review was designed to conform to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria.25 A review protocol was published in the PROSPERO registry prior to its initiation.
Data Sources and Searches
PubMed/MEDLINE, CINAHL, PsycINFO, Health Business Fulltext Elite, Web of Science, and Cochrane Library were used to identify eligible studies (Figure 2). All databases were searched from their inception through February 2016. The initial search strategy (Figure 3) was designed for PubMed/MEDLINE using both natural language keywords and MEDLINE’s authority controlled Medical Subject Headings (MeSH). The databases were searched for terms describing specialty physician practice, both solo and group practices, including multispecialty groups and excluding group dental practices, combined with terms for health care quality, outcome assessment, and guideline adherence. As relevant articles were identified, their keywords and MeSH headings were examined, and new terms were added to the search strategy. The initial MEDLINE search results were assessed for face validity, and the search was repeated in each of the other 5 databases after each search iteration. To avoid missing relevant literature, both the Surveillance, Epidemiology, and End Results (SEER)-Medicare website and the reference sections of retrieved articles were manually searched for additional references. No publication date restrictions were applied. Studies published in languages other than English were excluded.
Figure 2.
PubMed search terms.
Figure 3.
Search strategy and terminology.
Eligibility Criteria
References from the electronic and manual searches were compiled and assessed to determine eligibility for further review. Three criteria guided the initial eligibility assessment: (1) quality of care as an outcome, (2) assessment of specialty practice, and (3) reporting empirical results. The screening criteria required that studies report quality of care outcomes as described by the conceptual model, ie, efficacy, effectiveness, efficiency, optimality, acceptability, legitimacy, or equity.15 Studies that reported guideline adherence, guideline adoption, and use of evidence-based processes of care were considered to represent effective care. Studies measuring patient satisfaction were considered to represent acceptability. Physician specialty practice was defined as single specialty, multispecialty, or solo specialty, as self-defined by the study authors. Studies were excluded from further review if they focused on primary care (family medicine or general internal medicine), pediatric care, dental care, or hospital care delivery. Subspecialties of internal medicine (eg, gastroenterology) were considered specialties. Editorials, newspaper articles, and any form of popular media publications were also excluded from review.
Initial Screening
During the initial screening, the title and abstract of all references were evaluated to identify potential studies meeting the eligibility criteria. To facilitate this phase of screening, 2 teams, each consisting of 2 investigators, were formed. For training purposes, the title and abstract of 50 articles were reviewed independently by the 2 teams. Team members independently determined whether to “keep,” “drop,” or “discuss” each article or study. Results from team members were compared. Articles designated “discuss,” or for which the ratings were inconsistent between reviewers, were discussed among the entire team to clarify eligibility criteria. As discrepancies were resolved, criteria were revised, and investigators received additional training on coding rules. When abstracts were not available, investigators applied inclusion and exclusion criteria to the title and keywords of the study. Due to the limited information available in the title, abstract, and keywords, studies were retained for further review if reviewers were unable to find evidence for exclusion. Two investigators reviewed the titles and abstracts of the remaining articles. The initial screening yielded 154 studies for the second phase of screening.
Full Article Screening
In the second phase of screening, full articles of studies selected by title/abstract review in the initial screening were reviewed to more adequately assess whether studies met the a priori inclusion eligibility criteria: (1) quality of care as an outcome, (2) assessment of specialty practice, and (3) reporting empirical results. Studies were moved to the third phase if at least 1 reviewer determined it worthy of methodological scrutiny. Upon further review of the full text of articles, 129 studies were excluded, leaving 25 studies potentially relevant for inclusion.
Study Design and Outcome Measurement Assessment
Although some studies described differences in practice organization type, not all studies were designed to compare these differences in the specialty setting. Likewise, although all studies described quality of care, not all studies measured a quality of care outcome meeting the definitions put forth in our conceptual model. Thus, a third, more rigorous screening following the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (MAStARI)26 was conducted to ensure the design of included studies met 2 essential core inclusion criteria. At this step, the full text articles were reviewed by 2 senior investigators to verify whether they (1) considered practice type (ie, solo, group, or multispecialty group) as a comparison in the analysis; and (2) whether at least 1 study outcome aligned with 1 of the 7 outcomes defined by the Donabedian model. All 25 studies identified for this phase of screening were reviewed. Studies which passed this stage of review were deemed appropriate for inclusion in the full methodological review. This final phase of screening yielded a total of 4 studies.
Methodological Quality Determination and Data Extraction
Studies selected for inclusion in the final review were further assessed for methodological quality using the 7 remaining MAStARI criteria.26 These additional criteria include the use of random or pseudorandom sample, clear criteria for inclusion, identification of and adjustment for confounding factors, both an objective and reliable measure of quality (outcome measure), follow-up over a sufficient time period, inclusion of outcomes of people who withdrew from the study, and appropriate statistical analysis.26 Each item was scored qualitatively as “yes,” “no,” “unclear,” or “not applicable.” Studies were considered low quality if they met 4 or fewer criteria, moderate quality if they met 5 to 7 criteria, and high quality if they met 8 or more of the 9 criteria.
The 2 investigators were blinded to each other’s assessment. Upon completion of the appraisal of all studies, assessments were compared between the 2 investigators. Disagreements were discussed in light of the select appraisal criteria to achieve consensus. Because the studies were heterogeneous and could not be subjected to meta-analysis, extracted data were synthesized qualitatively and study findings were described narratively.26 Key details about the study design, methods, and findings were abstracted from published manuscripts for all studies deemed eligible for inclusion. In particular, patient-, physician- and practice-level covariates were identified and efforts made to assess whether these effects moderated the effects of practice organization.
Results
Less than 1% of studies reviewed (4 of 913) met our review criteria for assessing the influence of practice type on quality of care in a specialty setting (Figure 4). A large number of the 913 articles identified from the initial database search were either (1) opinion or consensus advice pieces lacking measurement of observed constructs published in trade journals/magazines (eg, “Specialists ventures: new business partnerships with hospitals” in Medical Network Strategy Report27); (2) focused on primary care practices or pediatric specialty practices (eg, “High immunization rates versus missed immunization opportunities in a private pediatric office”28); or (3) focused on nonquality of care outcomes (eg, “Reimbursement denial and reversal by health plans at a university hospital29).
Figure 4.
Search results.
Although 154 studies were identified in the title/abstract screening, 129 were excluded in the full article screening for the following nonmutually exclusive reasons: 54% did not actually assess practice type; 47% did not investigate an aspect of quality; and 34% did not address a specialty setting. For example, a study describing the demand for physician services was initially identified for inclusion, but was excluded in the second round as the study did not focus on any aspect of quality, did not address practice type, and did not focus on a specialty setting.30
Further scrutiny of study methods based on the 2 essential MAStARI criteria excluded an additional 21 studies because they did not adequately compare solo or group practice types (n = 15) or did not measure quality of care as defined a priori by our conceptual model (n = 6). The outcomes of studies excluded focused on practice’s scale efficiencies without corresponding assessment of potential impacts on quality15 or solely on provider outcomes,31 without a link to attainable improvements in patient health. Thus, our systematic review yielded 4 articles19,32-34 published through June 2015, which made at least 1 comparison among solo specialty practitioners, single-specialty group practitioners, and multispecialty group practitioners on a quality of care outcome.
Table 1 summarizes the design, methods, and findings for each study. All study designs were retrospective observational studies. Three of the 4 were cross-sectional.19,32,34 Only 1 of the study cohorts was selected randomly, but sample inclusion criteria were defined clearly in all 4 studies. The methodological quality of the included observational studies was considered moderate. Scores ranged from 5 to 7 out of 9 possible points (Table 2). Although it is not feasible to randomize practices to a practice type, no study used a quasi-experimental design to strengthen its findings, although the survey relied on a random sample of patients. Nonetheless, statistical analyses appear to be appropriate for the observational studies, and the Lin et al study, in particular, appears to be based on well-validated measures.
Table 1.
Summary of Included Studies.
| Article | Description | Objectively assessed quality of care measure(s) | Quality of care measure description | Overall design | Sample size, type, and selection criteria | Patient-level covariates | Physician- and practice-level covariates | Practice type comparison | Distinguishes multispecialty practice from single-specialty group | Statistical analysis | Key results | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ellis et al33 | Conducted a retrospective analysis of administrative claims data for 2138 urologists to assess factors associated with inappropriate use of nonguideline recommended treatment in localized prostate cancer patients. The study included all urologists, who provided the majority of treatment to men aged 65 years or older with localized prostate cancer, and met clinical criteria. Used linked cancer registry data to identify a patient subpopulation for whom hormone therapy was not indicated, then used treatment claims to identify whether those patients received the treatment. The explanatory variable of interest, the practice type, was identified through linkage to American Medical Association physician data obtained from physician self-report. | Effectiveness | Appropriate use of androgen deprivation therapy (ADT) | Retrospective secondary analysis of claims data | 2138 urologists treating low and intermediate risk prostate cancer patients in the SEER registries | Cancer grade, stage, age, comorbidities, marital status, race/ethnicity, proclivity to seek care, use of consultations in the prostate cancer treatment decision, SEER region; rurality of the patient’s community at diagnosis, median income of the patients’ residential zip code and proportion of adults without high-school education in the patients’ residential zip code | Time in practice, physician gender, board certification, training location, medical school affiliation, Panel size, proportion of minority Medicare patients | Solo vs group practice vs missing practice type | No | Mixed effect logistic regression, controlling for clustering by provider | Solo practice type was associated with overuse of ADT | Only applies to age >65, care provided by urologist, not by midlevels |
| Lin et al34 | Used a validated instrument to collect primary data from patients in a sample of 17 new solo and group practices in Taiwan. Every third patient who attended the clinics was sampled for survey participation until the target sample size was achieved, yielding a 100% response rate among those asked to participate. The survey assessed patient perceptions of 5 domains of service delivery: practices’ facilities, reliability, responsiveness, assurance, and empathy. The manner in which practice type was defined was not described but appears to have been defined a priori by the study investigators. | Effectiveness Acceptability | Tangibles, reliability, responsiveness, assurance, empathy and potential patient loyalty | Retrospective patient survey | 1250 clinic outpatients from 17 newly established Taiwanese clinics | Patient age, gender, education, marital status and type of illness specialty category | Solo vs group practice | No | Hierarchal linear regression modeling controlling for clustering | Group practice patients score significantly higher than solo practice patients on the tangibles, reliability, responsiveness, assurance, and empathy dimensions of service quality and potential patient loyalty | The study did not control for important confounders such as self-reported health status, illness severity, and physician characteristics, which could impact quality perceptions due to potential attribution effects | |
| Shortell et al19 | Conducted a national survey of large physician organizations. Of the 1104 organizations in the sampling frame (70% response rate), they analyzed a subset of 693 medical groups that treated chronic conditions to assess the degree to which environmental forces, resource acquisition capabilities, resource deployment capabilities, and presence of a quality-oriented culture were associated with clinical quality performance, organizational learning, and financial performance. The study assessed 1 structural outcome, use of clinical information technology; 3 process outcomes, including physician turnover, availability of health promotion programs, and using care management protocols; and 1 global index of overall quality, which mixed process and outcome measures: public recognition for quality performance. Practice type was self-reported by survey respondents. | Effectiveness Acceptability Efficiency | Overall quality indicator, patient satisfaction measurement, care management index, health promotion index, information technology index, physician turnover and profitability | Retrospective organizational survey | National sample of 693 physician organizations with 20 or more physicians treating patients with chronic illness; 70% response rate | Practice size, ownership, years in existence, type of practice, governance and management, financial management, relationships with health plans, degree of risk assumption, compensation models, external incentives, use of information technology, care management processes, and quality improvement approaches | single-specialty group vs multispecialty group | Yes | Multiple logistic regression with multiple imputation for missing key explanatory variables | Multispecialty group practice performs better than single group specialty on health promotion index, but less efficient because significantly associated with physician turnover; no effect detected on overall quality, care management, technology or profitability | No direct measure of patient satisfaction or patient outcomes | |
| Walley et al32 | Identified a cohort of 356 Massachusetts physicians certified to administer office-based opioid treatment and used self-reported prescription of opioids as the quality outcome. Physicians were identified from federal records of waiver approvals, 235 of whom responded to the study questionnaire (66% response rate). The questionnaire asked physicians about processes for and barriers to prescribing the recommended treatment for opioid dependence. Practice type was self-reported by survey respondents. | Effectiveness | Prescribing practices, utilization of buprenorphine to treat opioid dependence | Retrospective provider survey | Primary care, psychiatrists and other physicians with licensing to prescribe; 75% response rate | Medical specialty, practice setting, addiction society certification, and 7 potential barriers to prescribing (insufficient nursing/office support, lack of institutional support, low demand, insufficient physician knowledge, insufficient staff knowledge, payment issues, and pharmacy issues). | Group vs solo | No | Multiple logistic regression modeling | Solo providers were 3 times more likely to prescribe buprenorphine treatment | Self-report; limited to those with licenses to prescribe; don’t know anything about interaction of specialty care and practice setting |
Table 2.
Methodological Quality Assessment.
| Random Sample | Criteria for inclusion clearly defined | Confounding factors identified and addressed | Outcomes assessed using objective criteria | Sufficient descriptions of comparison groups | Adequate follow-up | Outcomes of those who withdrew described and included | Outcomes measured in a reliable way | Appropriate statistical analysis used | Total score | |
|---|---|---|---|---|---|---|---|---|---|---|
| Ellis et al33 | No | Yes | Yes | Yes | Yes | NA | No | Yes | Yes | 6 |
| Lin et al34 | Yes | Yes | Yes | Yes | Yes | NA | No | Yes | Yes | 7 |
| Shortell et al19 | No | Yes | Yes | No | Yes | NA | No | Yes | Yes | 5 |
| Walley et al32 | No | Yes | Yes | No | Yes | NA | No | Yes | Yes | 5 |
Studies could not be combined because quality of care was measured differently in each of the studies reviewed. One used patient self-report via survey34; 2 used provider self-report via survey19,32; and 1 used patient-level administrative data submitted by practices for payment.33 Outcomes assessed in the included studies included effectiveness,19,32-34 patient acceptability,34 and efficiency.19 No study directly included any of the other 4 dimensions of quality of care (efficacy, legitimacy optimality, or equity). In addition, the study settings were heterogeneous. Three of the 4 studies compared solo providers to single-specialty group practice in the fields of urology,33 psychiatry,32 and across multiple specialties, including primary care.34 One study compared single-specialty group practice and multispecialty group practice across specialty settings.19
Two studies controlled for covariates at the physician or practice level only.19,32 One study controlled only for patient characteristics.34 Only 1 study controlled for patient-, physician-, and practice-level characteristics.33 Neither patient-level study included payer-mix, ownership status, or total full-time equivalent medical professionals in the practice as covariates. Among the physician surveys, none of the studies were designed to assess the potentially moderating influence of multispecialty practice on the effect of group practice on quality.
Study Results
All 3 studies comparing solo to group practice specialists demonstrated a significant association between group practice type and quality. The direction of effect differed based on the quality measure used. Compared with solo providers, group practice providers performed better on measures of acceptability and patient assessment of quality, after adjusting for patient demographics and medical specialty. Patients rated group practice providers more highly on tangibles, such as the physical facilities, equipment, and appearance of personnel (regression coefficients: 0.30, P = .004); reliability, inclusive of timeliness and accuracy (0.25, P = .037); responsiveness to patients (0.31, P = .001); assurance, including courtesy and inspiring trust and confidence (0.26, P = .008); and empathy (0.28, P = .021).34 Similarly, group practice specialists were more likely than solo specialists to provide appropriate prostate cancer treatment, all else equal: being a solo practitioner was significantly associated with overuse of nonguideline recommended gonadotropin-releasing hormone agonists (multilevel mixed effects odds ratio [OR]: 1.65; 95% confidence interval [CI]: 1.34-2.02) after adjusting for tumor, patient demographic, physician personal characteristics, and practice characteristics.33
In contrast, solo providers were more likely to offer recommended opioid treatment than group practice providers controlling for specialty, certification status, and several staffing and organizational barriers (adjusted odds ratio [AOR]: 3.01, 95% CI: 1.23-7.35). Based on the 1 study that assessed differences between single-specialty group providers and multispecialty group providers, effects were mixed.19 Multispecialty groups were more efficient; they had significantly less voluntary turnover than single-specialty groups (OR: 0.23, 95% CI: 0.09-0.60). However, there were no significant differences in availability of clinical information technology (OR: 0.73, 95% CI: 0.35-1.5) or use of care management processes (AOR: 0.16, 95% CI: 0.02-1.2) between single-specialty and multispecialty groups. Multispecialty groups performed better than single-specialty groups on offering health promotion and promoting preventive services (AOR: 19.0, 95% CI: 4.8-73.9) but were not significantly different from single-specialty group physicians on receiving public recognition for quality (AOR: 2.8, 95% CI: 0.77-10.2).19
Discussion
We conducted a comprehensive, systematic review to identify empirical research that compared the quality of care among specialists of different practice types. Despite thorough, iterative and exhaustive attempts, we identified only 4 observational studies which addressed this issue.
The paucity of data and heterogeneity in practice setting, comparisons made, and outcomes measured prohibited data synthesis. Qualitative synthesis of these few observational studies provide only hypotheses for further study. All studies found a significant relationship between group practice type and at least 1 measure of quality. Thus, it could be hypothesized that specialists practicing in groups deliver care that is of higher technical quality and more patient-centered than their peers in solo practice, but solo specialists are more likely to offer access to specialty services that can improve quality of care for users of those services. With regard to single specialty and multispecialty differences in quality, it could be hypothesized that single-specialty and multispecialty group practices provide similar levels of clinical effectiveness and that multispecialty groups are better able to provide access to preventive services.
Findings from this review are similar to those reported in primary care in at least 1 regard. Studies comparing care processes, in particular appropriate prescribing, consistently report that primary care providers in group practice perform better than primary care providers in solo practice.3 Potential reasons for demonstrated differences between solo and group practices could equally apply to primary care or specialty care providers. High physician workload in solo practice may lead to less attention given to each patient and greater potential for medical error or inattention to standards of care. Physicians who prefer a greater proportion of time spent on direct patient contact, consistent with solo practice, may also resist the perceived lack of autonomy provided by guidelines. Alternatively, physicians in solo practice may have fewer referral resources or more vulnerable patient panels than those in group practice, resulting in poorer care processes.33,35
Specialists in solo practice may be more likely to offer some unique guideline-based services to patients, an outcome not directly assessed in other reviews focusing on primary care.3 Although solo primary physicians may be more likely to establish practices in rural areas, increasing overall access to care,36 recent evidence suggests that solo primary physicians may have more limited service offerings than their small and medium group practice counterparts.36 Thus, further attention to service offerings, in addition to geographic distribution, is needed in both primary care and specialty settings.
Our review sheds no light on the degree to which practice type affects patient satisfaction in the specialty setting as the only study which assessed patient satisfaction was conducted in a mix of primary and specialty care settings.34 In the primary care setting, studies assessing the impact of practice type on patients’ satisfaction provide conflicting results.3 However, patient satisfaction may be more directly impacted by the array of services offered, the amenities provided, the time spent with the provider, and the quality of the patient-provider interaction than by the practice type itself.
We analyzed reasons for exclusion at each step of the review and found that despite concerns for the demise of solo specialty practice, a modest trade literature on the benefits and challenges of integrating practices, and wide-spread assumption that integration will improve quality, there is little empirical research to provide an evidence base on how variations in specialty practice organizational structure affect quality. The evidence is limited for a number of reasons, all of which should be addressed in future research and research policy. Foremost, very few empirical studies addressing the issue of practice organization exist. Although physician productivity and efficiency has been studied from an organizational perspective, quality of care has not. Thus, opportunities to explore this issue are vast.
The lack of research partly arises because few studies include more than 1 practice type in their sampling strategy, preventing comparison. For example, quality may be studied in a single integrated delivery system or even across integrated systems, but studies are rarely designed to compare integrated systems with single group practice, often conflating payment model with practice type. Although secondary data are often limited with regard to what practice-level characteristics are available to be included, some data sets do offer the opportunity to make the comparison. However, investigators have not taken full advantage of the opportunity. For example, SEER-linked Medicare claims provide practice type, but many studies using this data source do not include the variable in the analysis and reasons for exclusion are not apparent.37 Few other current data sources offer organizational characteristics together with sufficient data to explore quality of care. The Community Tracking Study, the National Study of Physician Organizations, the National Ambulatory Medical Care Survey, and the American Medical Association group practice file are promising data sources, but either have limited capacity to measure clinical aspects of quality among specialists, have not been updated in recent years, or have not been validated.38-40 Investments should be made in making these data linkable with other clinical data sources or enhancing the information collected within them.
Efforts to include similar organizational level variables in primary data collection should be undertaken. Specifically, research examining quality of care should consider not only practice type, but other organizational features which drive quality of care such as group size, access to quality improvement technology (eg, decision support, clinical pathways, quality reporting, Lean Six Sigma infrastructure), and organizational culture. Furthermore, primary data collection may be needed to investigate specific features of specialty care organization which may influence quality of care, whether they be physician philosophy and style, practice leadership, clarity of staff roles, or communication patterns among physicians and staff41 of payment arrangements. These relationships should be examined with theoretically informed and validated measures and could be tested for their applicability within primary care practice as well. To further clarify relationships, different measures of quality should be assessed to shed light on which aspects of quality are influenced by practice type and clear definitions of specialties should be used in future studies. Study authors did not report whether “internal medicine” or “primary care” included the subspecialties of internal medicine, for example. Nor did studies define thresholds for defining multispecialty (ie, how many specialists are required).
The literature represents a high risk of selection and performance bias due to the limited number of study designs available. Whether higher performing physicians are more likely to choose group practice is unknown. Thus, studies which address potential selection bias are needed. When collected in samples of sufficient size, interaction terms should be considered for inclusion to potentially assess the mediating and moderating effect of these factors on quality of care.
Coordination of care, particularly in complex conditions, is a high priority for achieving high quality of care,16 and specialist collaboration has been demonstrated to lower mortality in some clinical conditions.42 But whether care coordination depends on the organization of different specialties into a single practice remains unknown based on the limited evidence available. Some forms of multispecialty care, such as intensity modulated radiation treatment (IMRT) centers, are suspected of encouraging overuse of services rather than improving overall quality.43 Thus, other modes of care coordination such as tumor boards may be preferable. In addition, multispecialty practices may be less efficient with regard to overall cost savings.31 However, if multispecialty practice organization can be demonstrated to consistently improve quality of care, inefficient care delivery may be worth the increased cost. Additional research to isolate the effect of group organization is needed.
Understanding the contribution of practice type to variations in quality is important. Specialists provide a significant proportion of care in the United States, but there remains a dearth of information on specialty care.44 Practice organization is one aspect of care that may influence its delivery of quality care. Multispecialty group practice may wax and wane with different payment models,5 but their presence is expected to remain.45 Although solo specialists may be decreasing in number,5,46 they remain a sizable cohort of specialty care providers. Almost 20% of all physicians are solo practitioners, with solo specialists ranging from 7% of radiologists to 30% of psychologists.5,47 Solo specialists provide access to care for many patients, especially those in rural areas, and deliver care for costly chronic conditions, providing care that is integral to the population’s health. Thus, solo providers still need support,48 but lacking an understanding of the features of group practice which may foster higher quality may limit our ability to do so.
Limitations
We conducted a comprehensive search of the literature and applied systematic review criteria to identify studies that could inform this relationship. Still, our study has limitations. We searched the literature based on a defined set of terms, but may have missed studies due to incomplete MeSH coding. We also may have missed studies which made comparisons of practice type, but which did not emphasize those findings in their study conclusions. Our study is limited to the study of practice type, a single and potentially flawed organizational factor which may influence quality. However, the purpose of our study is to assess this widely available construct, often used in the existing quality of care literature. Better constructs which do not conflate group size and specialty mix should be used in future research.
Conclusion
We conducted a systematic and comprehensive review of the existing literature to summarize the impact of group practice structure on quality of care in specialty practice. Existing literature to address this question is scant and heterogeneous. There is a great opportunity for systematic research to assess not only the degree to which practice type influences a variety of quality of care indicators but also the specific features inherent to group practice that may facilitate the delivery of high quality care.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported in part by National Cancer Institute of the National Institutes of Health under award number R25CA171994. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ORCID iD: Shellie D. Ellis  https://orcid.org/0000-0002-3599-0804
https://orcid.org/0000-0002-3599-0804
References
- 1. Welch WP, Cuellar AE, Stearns SC, Bindman AB. Proportion of physicians in large group practices continued to grow in 2009-11. Health Aff (Millwood). 2013;32(9):1659-1666. [DOI] [PubMed] [Google Scholar]
- 2. Conti RM, Landrum MB, Jacobson M. The Impact of Provider Consolidation on Outpatient Prescription Drug-Based Cancer Care Spending. Portland, ME: National Academy for State Health; 2016. [Google Scholar]
- 3. Damiani G, Silvestrini G, Federico B, et al. A systematic review on the effectiveness of group versus single-handed practice. Health Policy. 2013;113(1-2):180-187. [DOI] [PubMed] [Google Scholar]
- 4. Audet AM, Doty MM, Shamasdin J, Schoenbaum SC. Measure, learn, and improve: physicians’ involvement in quality improvement. Health Aff (Millwood). 2005;24(3):843-853. [DOI] [PubMed] [Google Scholar]
- 5. Kane CK, Emmons DW. Policy Research Perspectives: New Data on Physician Practice Arrangements: Private Practice Remains Strong Despite Shifts Toward Hospital Employment. Chicago, IL: American Medical Association; 2013. [Google Scholar]
- 6. Indiana University Heath Care Reform Faculty Study Group. Overuse of Specialty Care Increases Healthcare Costs in Indiana. Indianapolis, IN; Indiana University Public Policy Institute; 2008. [Google Scholar]
- 7. Sandy LG, Bodenheimer T, Pawlson LG, Starfield B. The political economy of U.S. primary care. Health Aff (Millwood). 2009;28(4):1136-1145. [DOI] [PubMed] [Google Scholar]
- 8. Brooks JV. Hostility during training: historical roots of primary care disparagement. Ann Fam Med. 2016;14(5):446-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smetana GW, Landon BE, Bindman AB, et al. A comparison of outcomes resulting from generalist vs specialist care for a single discrete medical condition: a systematic review and methodologic critique. Arch Intern Med. 2007;167(1):10-20. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Medicare & Medicaid Services. National plan and provider enumeration system. In: Centers for Medicare & Medicaid Services, ed. Taxonomy. Baltimore, MD: Health and Human Services; 2016. https://nppes.cms.hhs.gov/webhelp/nppeshelp/TAXONOMY%20PAGE.html [Google Scholar]
- 11. Williamson OE. The economics of organization—The transaction cost approach. Am J Sociol. 1981;87(3):548-577. [Google Scholar]
- 12. Burns LR, Goldsmith JC, Sen A. Horizontal and vertical integration of physicians: a tale of two tails. Adv Health Care Manag. 2013;15:39-117. [DOI] [PubMed] [Google Scholar]
- 13. Hearld LR, Alexander JA, Fraser I, Jiang HJ. Review: how do hospital organizational structure and processes affect quality of care? a critical review of research methods. Med Care Res Rev. 2008;65(3):259-299. [DOI] [PubMed] [Google Scholar]
- 14. Barber B. Some problems in the sociology of the professions. Daedalus. 1963;92(4):669-688. [Google Scholar]
- 15. Donabedian A. An Introduction to Quality Assurance in Health Care. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 16. Committee on the Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 17. Aday LA, Begley CE, Lairson DR, Balkrishnan R. Evaluating the Healthcare System: Effectiveness, Efficiency and Equity. 3rd ed. Chicago, IL: Health Administration Press; 2004. [Google Scholar]
- 18. Francke AL, Smit MC, de Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak. 2008;8:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shortell SM, Schmittdiel J, Wang MC, et al. An empirical assessment of high-performing medical groups: results from a national study. Med Care Res Rev. 2005;62(4):407-434. [DOI] [PubMed] [Google Scholar]
- 20. Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? a framework for improvement. JAMA. 1999;282:1458-1465. [DOI] [PubMed] [Google Scholar]
- 21. Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142(4):260-273. [DOI] [PubMed] [Google Scholar]
- 22. Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756-764. [DOI] [PubMed] [Google Scholar]
- 23. Mick SS, Comfort ME. The quality of care of international medical graduates: how does it compare to that of U.S. medical graduates? Med Care Res Rev. 1997;54(4):379-413. [DOI] [PubMed] [Google Scholar]
- 24. Sutherland K, Leatherman S. Does certification improve medical standards? BMJ. 2006;333(7565):439-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65-94. [DOI] [PubMed] [Google Scholar]
- 26. Joanna Briggs Institute. Joanna Briggs Institute Reviewers’ Manual: 2014 Edition. Adelaide, Australia; Joanna Briggs Institute; 2014. [Google Scholar]
- 27. Berry K. Specialist ventures: new business partnerships with hospitals. Med Netw Strategy Rep. 1999;8(7):17-11. [PubMed] [Google Scholar]
- 28. Epstein D. High immunization rates versus missed immunization opportunities in a private pediatric office. Del Med J. 1998;70(8):361-366. [PubMed] [Google Scholar]
- 29. Greenberg JD, Hoover DR, Sharma R, Noveck H, Bueno M, Carson JL. Reimbursement denial and reversal by health plans at a university hospital. Am J Med. 2004;117(9):629-635. [DOI] [PubMed] [Google Scholar]
- 30. Weiner JP. The demand for physician services in a changing health care system: a synthesis. Med Care Rev. 1993;50(4):411-449. [DOI] [PubMed] [Google Scholar]
- 31. Rosenman R, Friesner D. Scope and scale inefficiencies in physician practices. Health Econ. 2004;13(11):1091-1116. [DOI] [PubMed] [Google Scholar]
- 32. Walley AY, Alperen JK, Cheng DM, et al. Office-based management of opioid dependence with buprenorphine: clinical practices and barriers. J Gen Intern Med. 2008;23(9):1393-1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ellis SD, Nielsen ME, Carpenter WR, et al. Gonadotropin-releasing hormone agonist overuse: urologists’ response to reimbursement and characteristics associated with persistent overuse. Prostate Cancer Prostatic Dis. 2015;18:173-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lin HC, Xirasagar S, Laditka JN. Patient perceptions of service quality in group versus solo practice clinics. Int J Qual Health Care. 2004;16(6):437-445. [DOI] [PubMed] [Google Scholar]
- 35. Kravitz RL, Greenfield S, Rogers W, et al. Differences in the mix of patients among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992;267(12):1617-1623. [PubMed] [Google Scholar]
- 36. Liaw WR, Jetty A, Petterson SM, Peterson LE, Bazemore AW. Solo and small practices: a vital, diverse part of primary care. Ann Fam Med. 2016;14(1):8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Quek RG, Master VA, Portier KM, et al. Association of reimbursement policy and urologists’ characteristics with the use of medical androgen deprivation therapy for clinically localized prostate cancer. Urol Oncol. 2014;32(6):748-760. [DOI] [PubMed] [Google Scholar]
- 38. Ramsay PP, Shortell SM, Casalino LP, Rodriguez HP, Rittenhouse DR. A longitudinal study of medical practices’ treatment of patients who use tobacco. Am J Prev Med. 2016;50(3):328-335. [DOI] [PubMed] [Google Scholar]
- 39. Hollingsworth JM, Sakshaug JW, Zhang Y, Hollenbeck BK. In-office imaging capabilities among procedure-based specialty practices. Surg Innov. 2014;21(4):403-408. [DOI] [PubMed] [Google Scholar]
- 40. Center for Studying Health System Change. Health Tracking Household Survey, 2010. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2012. [Google Scholar]
- 41. Crabtree BF, Miller WL, Aita VA, Flocke SA, Stange KC. Primary care practice organization and preventive services delivery: a qualitative analysis. J Fam Pract. 1998;46(5):403-409. [PubMed] [Google Scholar]
- 42. Hussain T, Chang HY, Veenstra CM, Pollack CE. Collaboration between surgeons and medical oncologists and outcomes for patients with stage III colon cancer. J Oncol Pract. 2015;11(3):e388-e397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schilling PJ. Formation of combined urology and radiation oncology practices: objective data from radiation oncologists for rationale. Am J Clin Oncol. 2011;34(3):289-291. [DOI] [PubMed] [Google Scholar]
- 44. Casalino LP, Pham H, Bazzoli G. Growth of single-specialty medical groups. Health Aff (Millwood). 2004;23(2):82-90. [DOI] [PubMed] [Google Scholar]
- 45. Terry K. Questions to ask before joining a multispecialty group. Medial Economics. May 2002;9:124. [PubMed] [Google Scholar]
- 46. Squires D, Blumenthal D. Do small physician practices have a future? To the Point: Quick Takes on Health Care Policy and Practice. The Commonwealth Fund; May 26, 2016. [Google Scholar]
- 47. Qessential Medical Market Research. Physician outlook: urology. Qessential Medical Market Research. Exeter, NH: Qessential Medical Market Research; 2013. [Google Scholar]
- 48. Young K. Medicare may soften impact of doctor pay rule on small practices. Washington Health Policy Week in Review. May 23, 2016. https://www.commonwealthfund.org/publications/newsletter/2016/may/medicare-may-soften-impact-doctor-pay-rule-small-practices