Abstract
Purpose: Positive results have appeared among nonmetastatic breast cancer patients with the use of cognitive behavioral therapy (CBT). However, earlier stage patient results have been mixed. This novelty of this study was the focus on stage I and II breast cancer patients. The objective of the current study was to conduct a meta-analysis of psychosocial functions in early-stage breast cancer survivors to determine its efficacy. Methods: A search of Cochrane Library, EMBASE, MEDLINE, PsycInfo, and PubMed yielded 3237 abstracts, which were independently evaluated by research pairs. Meta-analysis was conducted on 8 studies that included a total of 1053 patients. Psychosocial functions were categorized according to 3 domains: (1) anxiety, (2) depression, and (3) quality of life. Results: Improvement in anxiety was observed in patients treated with CBT relative to controls without CBT (P = .04). Depression and quality of life improvement was not observed in the CBT group within or after 4 months of treatment (P > .05). Conclusions: The results indicated that observed improvements in anxiety in patients with early-stage breast cancer were moderate. The effectiveness of CBT for the improvement of patient outcomes could not be determined, given the methodological and clinical shortcomings of the included trials.
Keywords: anxiety, breast neoplasms, cognitive therapy, depression, quality of life
Introduction
Breast cancer is the most common cancer in women, comprising 30% of all types of cancer in women. Approximately 160 000 people were diagnosed, and 40 000 died, from breast cancer each year in China in 2008.1 Owing to the development of a combination of radiation therapy, chemotherapy, and endocrine therapy, the survival of breast cancer patients has risen from 74.8% to 90.8% during the past 3 decades (1970s to 2000s).2 However, half of all cancer patients suffer from a psychiatric disorder because of the cancer diagnosis or the side effects of treatment; the highest prevalence of any mental disorder was found in patients with breast cancer. It has been reported that 40% to 50% of breast cancer patients have been diagnosed with mental health disorders, including anxiety disorder, adjustment disorder, mood disorder, somatoform/conversion disorder, nicotine dependence, alcohol abuse/dependence, mental disorders resulting from medical conditions, and eating disorders.3,4 The results provided strong evidence for the need for psycho-oncological interventions.
Cognitive behavioral therapy (CBT) is a psychosocial intervention that is the most widely used evidence-based practice for improving mental health.5 The CBT model is based on a combination of the basic principles of behavioral and cognitive psychology. It is reported that CBT shows a positive effect on breast cancer patients for the treatment of mental disorders.6-8 Mindfulness-based cognitive therapy, one type of CBT, proved to effectively reduce the posttreatment pain that breast cancer patients experienced.9
CBT has shown some benefits for women with metastatic breast cancer as well as nonmetastatic breast cancer.10,11 But most research included nonmetastatic breast cancer patients in stage III, a local advanced stage that needs more aggressive radiation therapy and chemotherapy. A growing body of research has identified cognitive dysfunction caused by the chemotherapies used to treat cancer.12,13 Possible explanations for this have included direct neurotoxic effects, oxidative stress and DNA damage, induced hormonal changes, immune dysregulation and/or release of cytokines, and blood clots in peripheral vessels of the central nervous system.14 These pathological changes may be chronic and potentially could obscure any positive effects of CBT. Therefore, patients with diagnoses of stage III or IV breast cancers were excluded from this study.
Methods
Search Strategy
We collected search results from 5 databases: Cochrane Library (2017), EMBASE (Excluding MEDLINE Journals [1974 to June 2017]), MEDLINE (1946 to June 2017), PsycINFO (1806 to June 2017), and PubMed (Excluding MEDLINE [1946 to June 2017]). The search strategies for each are illustrated in Online Appendices 1 to 5. Duplicates were removed. Gray literature was included. Although CBT was developed in the 1960s by Aaron Temkin Beck,15 studies employed cognitive behavioral techniques prior to the 1960s. Therefore, the search encompassed all literature from 1806 through June 2017. The search was limited to studies published in English.
Selection Strategy
The selection of research abstracts was conducted by 3 raters. Most of the studies could be judged by their titles and abstracts. An examination of entire articles was necessary when there was disagreement among the researchers with regard to their inclusion. Four inclusion criteria were applied to the studies retrieved:
Patients with pathologically confirmed early-stage breast cancer (stages I and II) were included. Patients had completed medical treatment for breast cancer (surgery, radiotherapy, or chemotherapy) and had no evidence of other cancers or metastases. Women taking adjuvant endocrine treatment were eligible. Patients diagnosed with metastasis breast cancer and those who had severe mental disorders and/or a recurrence of cancer were excluded from the study.
Patients who received CBT were included. CBT is defined as a psychosocial intervention that aims to improve mental health.16 A reading of entire articles was necessary to determine what type of CBT was used in each study. The selection strategy was not limited to standard CBT. For example, we also included studies that employed cognitive and/or behavioral techniques to help individuals replace maladaptive thinking by challenging an individual’s way of thinking, as well as challenging the way in which one reacts to certain habits or behaviors. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders is a form of CBT and includes the following common set of components: psychoeducation, cognitive reappraisal, emotion regulation, and changing behavior.17 Based on previous opinions, we considered active psychoeducation—but not passive psychoeducation (eg, videotape intervention)—as a form of CBT.18 Patients who received treatment with mindfulness-based stress reduction were excluded from the study because mindfulness-based cognitive therapy incorporates mindfulness-based stress reduction into CBT.19
-
Results of the studies had to include data on at least one of the following: anxiety, depression, or quality of life (QoL). These outcomes were measured by a variety of scales. Duplicate results and studies that only reported changes with incomparable parameters—such as “improvement” and “relief”—were excluded. If a standard deviation was only reported for the intervention group, the standard deviation could be used for the control group. If a t value was used, standard deviation could be calculated by
All studies had to have included measures for both before and after interventions. The studies had to be randomized controlled trials (RCTs). Studies that did not define the methodology utilized were excluded. Quasi-experimental studies were also excluded.
Inclusion criteria are illustrated in Table 1.
Table 1.
PICOs of Including Studies in the Meta-Analysis.
| Inclusion | Exclusion | |
|---|---|---|
| Population | Patients with early-stage breast cancer (stages I and II), pathologically confirmed | Patient diagnosis of stage III or IV breast cancer, severe mental disorder, and/or cancer recurrence |
| Intervention | Patients who received CBT | Patients who received psychosocial therapy without using CBT technics (eg, mindfulness-based stress reduction) |
| Comparison/control group | Patients who received therapy without CBT | — |
| Outcomes | 1. Anxiety 2. Depression 3. QoL |
Duplicate results and studies that only reported changes with incomparable parameters, such as improve and relief, were excluded |
| Study design | RCTs | Case studies, quasi-experimental studies, and studies that did not define the methodology utilized were excluded |
Abbreviations: PICO, patient/problem, intervention, comparison, outcome; CBT, cognitive behavioral therapy; QoL, quality of life; RCTs, randomized controlled trials.
Data Collection and Analysis
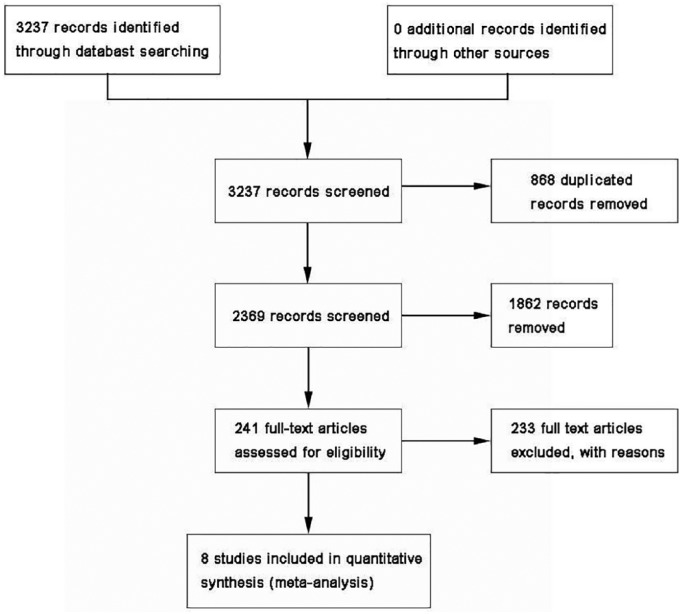
The selection of publications from the search results was undertaken independently by 2 review authors (HS and HH). Figure 1 illustrates the selection process. Disagreements over selection were resolved by discussion between the 2 researchers. A third researcher participated in the discussion, when necessary.
Figure 1.
Flow diagram.
The following information was documented in a data extraction list for each article:
General information that included title, authors, year of publication, country of origin, ethical approval, funding, and duration.
Eligibility information that included whether the study was an RCT or not, addressed women with early-stage breast cancer or not, and the type of CBT intervention and CBT.
Participant information that included the sample size, method of recruitment, inclusion and exclusion criteria, demographic characteristics, descriptors, and characteristics prior to CBT intervention.
Intervention information that included description, setting, type of provider, and a description of the control group.
Outcome measures that included primary and secondary outcomes as reported in the study, methods and timeframes for assessments of effects, validity of outcome measurement tools used, and follow-up details.
Verification of the study’s inclusion of statistical data, research results, and whether criteria used to determine risk of bias.
Assessment of Risk of Bias
The methodological quality of the studies was analyzed according to the Cochrane Collaboration’s tool for assessing risk of bias. The following elements of each domain of bias were rated as “low risk,” “high risk,” or “unclear risk”:
Random sequence generation (selection bias): assessment of the method used to generate the allocation sequence to produce groups for comparison.
Allocation concealment (selection bias): assessment of the method used to conceal the allocation sequence to determine whether intervention allocations could have been foreseen prior to, or during, enrollment.
Blinding of participants and personnel (performance bias) and blinding of outcome assessment (detection bias): assessment of measures used to blind study participants and personnel from knowledge of interventions received by participants and their effectiveness.
Incomplete outcome data (attrition bias): assessment of the completeness of outcome data for each main outcome, including reporting of and reasons for attrition and exclusions from the analysis, as well as data on any re-inclusions.
Selective outcome reporting (reporting bias): assessment of the possibility of selective outcome reporting by the authors.
Other sources of bias.
Statistical Analysis
The studies were first examined for descriptions of the interventions and qualitative synthesis. The data from 3 or more studies were then examined for meta-analyses.
Authors were contacted for data that could not be determined from the published reports. If no additional information was made available, the study was not included in the analysis.
Statistical heterogeneity was assessed using the I2 statistic. An I2 value >50% suggests substantial heterogeneity. In cases of substantial heterogeneity, an attempt was made to explain the variation, and a random-effects model was employed.
For meta-analyses, all data from 3 or more RCTs were examined together if measures appropriate for comparison were used. Because the studies utilized different measurement tools, the effect size for the studies was summarized as a standard mean difference (SMD). P values <.05 were regarded as significant for all analyses. Review Manager 5.3 software was used to generate statistics and maps.
Subgroup Analysis and Investigation of Heterogeneity
Potential clinical variations that could result in heterogeneity were explored using subgroup analysis. The results of the intervention were evaluated at different time points (≤4 months or >4 months).
Sensitivity Analysis
Sensitivity analyses were applied to assess the robustness of the polled results. Where heterogeneity existed, studies that led to a different effect were removed. Additionally, studies with a high risk of bias were removed.
Results
We retrieved a total of 3237 references to studies. After examination of the titles and abstracts of these references, we deleted duplicates and eliminated all of those that did not match our inclusion criteria and those that were clearly ineligible. We obtained full-text copies of the remaining 241 potentially eligible studies for further evaluation. Eight studies proved to be eligible for inclusion in accordance with the established criteria. We included 8 randomized controlled clinical trials that included a total of 1053 participants.20-27 The publication date for these studies ranged from 1999 to 2012. Three of the studies were from the United States,24-26 2 from Australia,21,22 1 from Canada,20 and 1 from Turkey.28 More than 70% of all patients had undergone surgery and adjuvant therapies, and >50% of all patients were receiving endocrine therapy at the time of the study. All 8 studies had tested scales both before and after therapy. The baseline of the sociodemographic characteristics of the participants in the other 7 studies were all comparable. Dastan and Buzlu’s work demonstrated that only the age differences were statistically significant and the control group patients were younger than the experimental group patients.28 The psychosocial characteristics of patients in the 7 studies were all comparable, except for those from one study: Stanton et al’s article reported that participants demonstrated significantly greater vitality and psychological well-being as well as fewer depressive symptoms than the 2 intervention groups at baseline.26 Details of the included individual studies are summarized in Table 2.
Table 2.
Characteristics of Included Studies.
| Studies | Patients | Cases (I/C) | Intervention | Control | Follow-up | Scales |
|---|---|---|---|---|---|---|
| Edelman et al22 | 49 | 23/24 | CBT intervention | Supportive therapy | Pre-therapy Post-therapy 4-month follow-up |
POMS Functional Living Index Rosenberg Self-Esteem Scale Social Support |
| Sandgren et al25 | 62 | 24/29 | Telephone therapy assistance with relaxation | — | 4-month follow-up 10-month follow-up |
Coping Response Indices–Revised Scale POMS MOS |
| Simpson et al20 | 315 | 46/43 | Psychosocial support intervention | — | Pre-therapy Post-therapy 1-year follow-up 2-year follow-up |
SCL-90-R BDI MAC POMS QLI DWII SCID |
| Kissane et al21 | 303 | 154/149 | CEGT plus 3 relaxation classes | 3 relaxation classes | 6-month follow-up 12-month follow-up |
MILP ABS HADS MAC FAD |
| Stanton et al26 | 558 | 143/136 | EDU | CTL | 6-month follow-up 12-month follow-up |
4-Item SF-36 Vitality Subscale IES-R CES-D PTGI |
| Scheier et al24 | 252 | 69/76 | Education sessions | — | Pre-therapy 4-month follow-up 13-month follow-up |
10-item version of the CES-D 36-item SF-36 |
| Beatty et al23 | 49 | 25/24 | Self-help workbook | Workbook without suggestions, worksheets, or compact disc | 3-month follow-up 6-month follow-up |
21-Item Depression Anxiety Stress Scales 17-Item Posttraumatic Stress Diagnostic Scale Global QoL Mini-MAC |
| Dastan and Buzlu28 | 123 | 44/44 | Psychoeducation program | No program | Pre-therapy 6-week follow-up 6-month follow-up |
HADS KPS MAC |
Abbreviations: I/C, intervention/control; CBT, cognitive behavioral therapy; POMS, Profile of Mood States; MOS, Medical Outcome Scale; SCL-90-R, Symptom Checklist-90-R; BDI, Beck Depression Inventory; MAC, Mental Adjustment to Cancer Scale; QLI, Quality of Life Index; DWII, Dealing With Illness Inventory; SCID, structured clinical interview for DSM (Diagnostic and Statistical Manual of Mental Disorders)-III-R; CEGT, Cognitive-Existential Group Therapy; MILP, Monash Interview for Liaison Psychiatry; ABS, Affects Balance Scale; HADS, Hospital Anxiety and Depression Scale; FAD, Family Assessment Device; EDU, psychoeducational counseling; CTL, standard print control; SF-36, Short Form-36; IES-R, Impact of Events Scale; CES-D, Center for Epidemiologic Studies–Depression Scale; PTGI, Posttraumatic Growth Inventory; QoL, quality of life; KPS, Karnofsky Performance Scale.
Characteristics of the Outcome Measures
A variety of tools were used to determine outcomes measures. Anxiety was measured using the Profile of Mood States, the Hospital Anxiety Depression Scale, the 21-Item Depression Anxiety Stress Scales, and the Mental Adjustment to Cancer Scale.
Depression was measured with tools such as the Beck Depression Inventory, the Profile of Mood States, the Hospital Anxiety Depression Scale, the Center for Epidemiologic Studies–Depression Scale, and the 21-Item Depression Anxiety Stress Scales.
QoL outcomes were measured using Functional Living Index, the Quality of life Index, the Short-Form Health Survey, Global QoL (36).
Table 3 illustrates the scales used in the individual studies.
Table 3.
Summary of Scales Used in the Individual Studies for Analysis.
| Studies | Anxiety | Depression | QoL |
|---|---|---|---|
| Edelman et al22 | POMS | POMS | Functional Living Index |
| Sandgren et al25 | POMS | POMS | — |
| Simpson et al20 | POMS | POMS | QLI |
| Kissane et al21 | HADS | HADS | — |
| Stanton et al26 | — | CES-D | — |
| Scheier et al24 | — | CES-D | SF-36 Health Survey |
| Beatty et al23 | 21-Item Depression Anxiety Stress Scales | 21-Item Depression Anxiety Stress Scales | Global QoL |
| Dastan and Buzlu28 | MAC | — | — |
Characteristics of the Interventions
A wide range of interventions were evaluated. All of the interventions were based on cognitive behavioral theory using different techniques: CBT is a psychosocial intervention that is the most widely used evidence-based practice for improving mental health. Edelman et al, Simpson et al, and Kissane et al20-22 used group CBT (a common format for the delivery of therapy) to treat newly diagnosed primary breast cancer patients. Sandgren et al used cognitive-behavioral therapy administered by telephone in a study of patients with breast cancer.25 Stanton et al used psychoeducational counseling to treat women assigned to the psychoeducational group in one individually conducted in-person session, as well as in one telephone session with trained cancer educators.26 Scheier et al adopted 4 education sessions specifically designed to provide information about the psychosocial issues of concern to younger women with early-stage breast cancer.24 Dastan and Buzlu used an 8-session study of psychoeducational intervention to provide education and support.28 All 3 studies mentioned above used active psychoeducational interventions, which were all included based on our definition of CBT. Beatty et al’s study used a self-help workbook intervention, which contained cognitive restructuring and relaxation techniques. Thus, self-help workbook interventions were also considered as a form of CBT.23
Risk of Bias in Included Studies
We assessed the risk of bias for each included study (Table 4). Owing to the nature of the intervention studies, an assessment of the blinding of treatment assignments was not applicable. For example, Beatty et al presented a randomized trial of a workbook intervention for primary breast cancer patients without any information about randomization methods, which was determined to represent an unclear risk. Additionally, 2 studies with incomplete outcome data were determined to represent high risk.20,25
Table 4.
Risk of Bias of Included Studies.
| Studies | Random Sequence Generation | Allocation Concealment | Blinding | Incomplete Outcome Data | Selective Reporting | Other Bias |
|---|---|---|---|---|---|---|
| Edelman et al22 | Low risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Sandgren et al25 | Low risk | Unclear risk | Low risk | High risk | Low risk | Unclear risk |
| Simpson et al20 | Low risk | Low risk | Low risk | High risk | Low risk | Unclear risk |
| Kissane et al21 | Low risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Stanton et al26 | Low risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Scheier et al24 | Low risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Beatty et al23 | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Dastan and Buzlu28 | Low risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
Primary Outcomes
Mean Difference in Anxiety
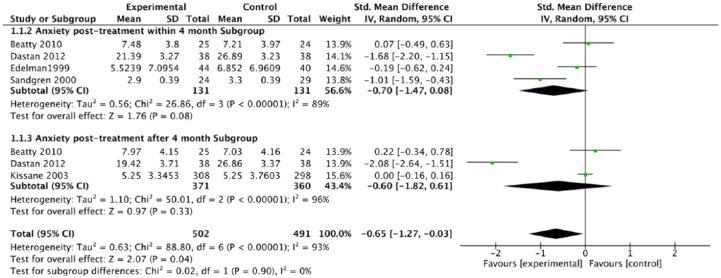
We identified 5 studies that included anxiety outcomes that were appropriate for analysis.21-23,25,28 The pooled change from baseline SMD that compared the group and individually delivered interventions of standard care was −0.65 (95% confidence interval [CI] = −1.27 to −0.03, P = .04, I2 = 93%; χ2 test P < .01). The estimate was analyzed by random effect due to heterogeneity. A sensitivity analysis was performed by removing data from 3 studies.20,23,25 Although the removal of data from the 3 studies weakened the overall treatment effect of anxiety, the SMD was −0.96 (95% CI = −1.94 to 0.02, P < .01, I2 = 96%; χ2 test P < .01). Nonsignificant statistical evidence indicated a subgroup reduction in anxiety from the baseline compared with the control group (Figure 2).
Figure 2.
Forest plot of comparison: CBT versus control groups and standardized mean difference for the change in anxiety levels from baseline.
Abbreviation: CBT, cognitive behavioral therapy.
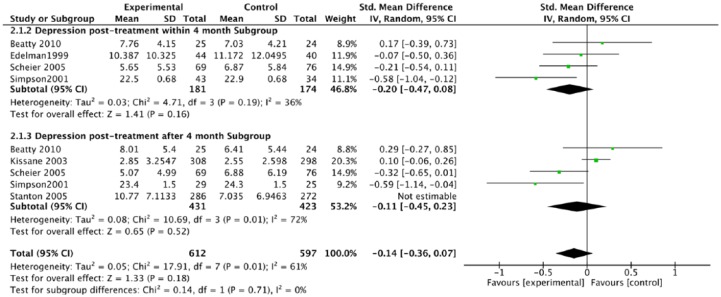
Mean Difference in Depression
Six of the studies determined the change in levels of depression.20-24,26 The change from the baseline pooled SMD between the intervention and control groups on the Depression Scale was −0.06 (95% CI = −0.32 to 0.21; P = .68; I2 = 84%; χ2 test P < .01; Figure 3). Following the removal of one study,26 a sensitivity analysis resulted in an SMD of −0.14 (95% CI = −0.36 to 0.07; P = .18; I2 = 61%; χ2 test P = .01). Depression in the CBT group was no lower than in the control group.
Figure 3.
Forest plot of comparison: CBT versus control and standardized mean difference for the change in depression levels from baseline.
Abbreviation: CBT, cognitive behavioral therapy.
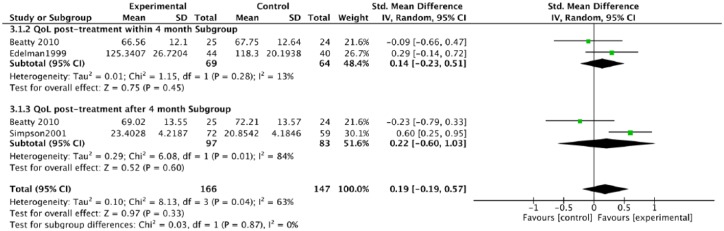
Mean Difference in QoL
Three studies were included to determine QoL levels.20,22,23 There appeared to be no difference between the groups for this outcome: 0.19 (95% CI = −0.19 to 0.57; P = .33; I2 = 63%; χ2 test P = .04; Figure 4). However, the estimate was associated with a high level of uncertainty due to severe heterogeneity.
Figure 4.
Forest plot of comparison: CBT versus control and standardized mean difference for the change from baseline in QoL.
Abbreviations: CBT, cognitive behavioral therapy; QoL, quality of life.
Discussion
The current meta-analysis synthesized data from 8 studies to examine the psychosocial functions of depression, anxiety, and QoL. The results indicated that patients who received CBT showed improvements with regard to anxiety. However, depression and QoL did not evidence improvements during a 4-month period or longer.
These findings were consistent with previous research on nonmetastatic breast cancer, and psychological outcomes became less evident when the disease had already metastasized to other parts of the body10,11; this study did not evidence much progress in depression and QoL in early-stage breast cancer patients either. The results could be explained by different inclusion criteria or specific aspects of the included studies. For example, Jassim et al11 found that group therapy proved more effective than individual therapy for the treatment of anxiety and depression. However, half of the studies included here focused on individual therapy. It is possible that the CBT could have been more effective if it had been utilized in the context of group therapies.
Multiple factors could have altered the risk of bias in this research. The inability to blind participants or investigators to the intervention also could have resulted in a bias that shaped the results. Moreover, Sandgren et al reported only the mean for the control group, while reporting the mean plus its standard deviation for the intervention group. Based on our selection strategy delineated in the Methods section, the standard deviation for the intervention group could be used for the control group.25 Simpson et al did not report standard deviation but, rather, reported the t value; standard deviation was calculated with the equation presented in the Methods section.20 The bias that possibly resulted would have to be eliminated to assure an adequate evaluation of the efficacy of CBT interventions.
Severe heterogeneity could be observed in some areas. Various scales were used to measure the effects of treatment, especially on depression levels. Moreover, after checking Stanton et al’s original article,26 it was found that the control group reported significantly greater vitality and psychological well-being and fewer depressive symptoms than the 2 intervention groups at the baseline. The differences persisted with baseline Center for Epidemiologic Studies–Depression Scale scores utilized as a covariate to serve as a control. The differences that existed at the baseline comparison suggested that greater evidence would be needed to support more convincing results. The impact of the methodological quality on overall effect size was determined by sensitivity analyses. Potential clinical variations that could cause heterogeneity were explored through subgroup analysis. However, neither clinical heterogeneity (no decrease in statistical heterogeneity in subgroup analyses) nor methodological heterogeneity (no decrease in statistical heterogeneity in sensitivity analyses) explained the statistical heterogeneity of effects.
In conclusion, the results from this meta-analysis suggested that CBT potentially works to improve psychological disorders among early-stage breast cancer patients. However, the results could not be determined given the methodological and clinical shortcomings of the included trials. It could be argued that additional studies with methodologies more apt for comparison could provide evidence for a greater effectiveness of CBT for the treatment of psychological disorders among women with early-stage breast cancer.
Supplemental Material
Supplemental material, Appendices for The Efficacy of Cognitive Behavioral Therapy to Treat Depression and Anxiety and Improve Quality of Life Among Early-Stage Breast Cancer Patients by Haoyao Sun, Hualei Huang, Shengjun Ji, Xiaochen Chen, Yongqing Xu, Fenglan Zhu and Jinchang Wu in Integrative Cancer Therapies
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study received financial support from the Community Health Service Center of the Taicang Economic-Technical Development Zone (KFQKT2017002).
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Fan L, Strasser-Weippl K, Li JJ, et al. Breast cancer in China. Lancet Oncol. 2014;15:e279-e289. [DOI] [PubMed] [Google Scholar]
- 2. Jemal A, Ward EM, Johnson CJ, et al. Annual report to the nation on the status of cancer, 1975-2014, featuring survival. J Natl Cancer Inst. 2017;109(9). doi: 10.1093/jnci/djx030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mehnert A, Brähler E, Faller H, et al. Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J Clin Oncol. 2014;32:3540-3546. [DOI] [PubMed] [Google Scholar]
- 4. Kuhnt S, Brähler E, Faller H, et al. Twelve-month and lifetime prevalence of mental disorders in cancer patients. Psychother Psychosom. 2016;85:289-296. [DOI] [PubMed] [Google Scholar]
- 5. Musiat P, Tarrier N. Collateral outcomes in e-mental health: a systematic review of the evidence for added benefits of computerized cognitive behavior therapy interventions for mental health. Psychol Med. 2014;44:3137-3150. [DOI] [PubMed] [Google Scholar]
- 6. Xiao F, Song X, Chen Q, et al. Effectiveness of psychological interventions on depression in patients after breast cancer surgery: a meta-analysis of randomized controlled trials. Clin Breast Cancer. 2017;17:171-179. [DOI] [PubMed] [Google Scholar]
- 7. Aricò D, Raggi A, Ferri R. Cognitive behavioral therapy for insomnia in breast cancer survivors: a review of the literature. Front Psychol. 2016;7:1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang J, Xu R, Wang B, Wang J. Effects of mindfulness-based therapy for patients with breast cancer: a systematic review and meta-analysis. Complement Ther Med. 2016;26:1-10. [DOI] [PubMed] [Google Scholar]
- 9. Johannsen M, O’Connor M, O’Toole MS, Jensen AB, Højris I, Zachariae R. Efficacy of mindfulness-based cognitive therapy on late post-treatment pain in women treated for primary breast cancer: a randomized controlled trial. J Clin Oncol. 2016;34:3390-3399. [DOI] [PubMed] [Google Scholar]
- 10. Mustafa M, Carson-Stevens A, Gillespie D, Edwards AG. Psychological interventions for women with metastatic breast cancer. Cochrane Database Syst Rev. 2013;(6):CD004253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jassim GA, Whitford DL, Hickey A, Caryer B. Psychological interventions for women with non-metastatic breast cancer. Cochrane Database Syst Rev. 2015;(5):CD008729. [DOI] [PubMed] [Google Scholar]
- 12. Vardy J, Wefel JS, Ahles T, Tannock IF, Schagen SB. Cancer and cancer-therapy related cognitive dysfunction: an international perspective from the Venice cognitive workshop. Ann Oncol. 2008;19:623-629. [DOI] [PubMed] [Google Scholar]
- 13. Vardy J, Rourke S, Tannock IF. Evaluation of cognitive function associated with chemotherapy: a review of published studies and recommendations for future research. J Clin Oncol. 2007;25:2455-2463. [DOI] [PubMed] [Google Scholar]
- 14. Ahles TA, Saykin AJ. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer. 2007;7:192-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beck AT. The past and future of cognitive therapy. J Psychother Pract Res. 1997;6:276-284. [PMC free article] [PubMed] [Google Scholar]
- 16. Field TA, Beeson ET, Jones LK. The new ABCs: a practitioner’s guide to neuroscience-informed cognitive-behavior therapy. J Ment Health Couns. 2015;37:206-220. [Google Scholar]
- 17. Sauer-Zavala S, Cassiello-Robbins C, Conklin LR, Bullis JR, Thompson-Hollands J, Kennedy KA. Isolating the unique effects of the unified protocol treatment modules using single case experimental design. Behav Modif. 2017;41:286-307. [DOI] [PubMed] [Google Scholar]
- 18. Donker T, Griffiths KM, Cuijpers P, Christensen H. Psychoeducation for depression, anxiety and psychological distress: a meta-analysis. BMC Med. 2009;7:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alsubaie M, Abbott R, Dunn B, et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev. 2017;55:74-91. [DOI] [PubMed] [Google Scholar]
- 20. Simpson JS, Carlson LE, Trew ME. Effect of group therapy for breast cancer on healthcare utilization. Cancer Pract. 2001;9:19-26. [DOI] [PubMed] [Google Scholar]
- 21. Kissane DW, Bloch S, Smith GC, et al. Cognitive-existential group psychotherapy for women with primary breast cancer: a randomised controlled trial. Psychooncology. 2003;12:532-546. [DOI] [PubMed] [Google Scholar]
- 22. Edelman S, Bell DR, Kidman AD. Group CBT versus supportive therapy with patients who have primary breast cancer. J Cogn Psychother. 1999;13:189-202. [Google Scholar]
- 23. Beatty LJ, Koczwara B, Rice J, Wade TD. A randomised controlled trial to evaluate the effects of a self-help workbook intervention on distress, coping and quality of life after breast cancer diagnosis. Med J Aust. 2010;193(5 suppl):S68-S73. [DOI] [PubMed] [Google Scholar]
- 24. Scheier MF, Helgeson VS, Schulz R, et al. Interventions to enhance physical and psychological functioning among younger women who are ending nonhormonal adjuvant treatment for early-stage breast cancer. J Clin Oncol. 2005;23:4298-4311. [DOI] [PubMed] [Google Scholar]
- 25. Sandgren AK, McCaul KD, King B, O’Donnell S, Foreman G. Telephone therapy for patients with breast cancer. Oncol Nurs Forum. 2000;27:683-688. [PubMed] [Google Scholar]
- 26. Stanton AL, Ganz PA, Kwan L, et al. Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol. 2005;23:6009-6018. [DOI] [PubMed] [Google Scholar]
- 27. Ambler N, Rumsey N, Harcourt D, Khan F, Cawthorn S, Barker J. Specialist nurse counsellor interventions at the time of diagnosis of breast cancer: comparing “advocacy” with a conventional approach. J Adv Nurs. 1999;29:445-453. [DOI] [PubMed] [Google Scholar]
- 28. Dastan NB, Buzlu S. Psychoeducation intervention to improve adjustment to cancer among Turkish stage I-II breast cancer patients: a randomized controlled trial. Asian Pac J Cancer Prev. 2012;13:5313-5318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendices for The Efficacy of Cognitive Behavioral Therapy to Treat Depression and Anxiety and Improve Quality of Life Among Early-Stage Breast Cancer Patients by Haoyao Sun, Hualei Huang, Shengjun Ji, Xiaochen Chen, Yongqing Xu, Fenglan Zhu and Jinchang Wu in Integrative Cancer Therapies