Abstract
We conducted a survey of pulmonary arterial hypertension (PAH) patients and healthy controls who use either a smartphone or wearable fitness device that tracks daily step count. We found that PAH patients have markedly reduced activity levels compared to controls, after controlling for confounders.
Keywords: accelerometry, wearable electronic devices, smartphone
Introduction
Pulmonary arterial hypertension (PAH) is characterized by progressive obliteration of the pulmonary arterioles, leading to increased pulmonary vascular resistance and right heart failure. This manifests in patients as dyspnea and fatigue, diminished exercise capacity, and premature death. Despite recent advances in treatment options for PAH, many patients remain burdened by daily symptoms, and mortality remains unacceptably high.1
Most evaluations of exercise capacity are performed in the clinic, but a few small studies have also shown that PAH patients are less active than healthy controls using accelerometers worn for short observational periods.2–5 Studies such as these may provide better insight into patients’ “free-living activity,” which is defined as the level of activity that the patients typically perform, within their physical limitations, and in their own environment. In these studies, daily activity levels also correlate moderately with clinical outcomes such as 6-min walk distance, invasive hemodynamics, and mortality, despite the limited observational periods, and potential susceptibility to the Hawthorne effect, wherein the behavior of individuals changes due to awareness that they are being observed.2,4,5 Given the widespread use and availability of smartphones and wearable fitness devices, many people now carry commercial accelerometers on a daily basis. To our knowledge, no one has investigated the daily activity levels of PAH patients using these increasingly ubiquitous devices. We designed this proof-of-concept study to determine if commercially available and routinely used devices with accelerometers detect differences in daily step counts between PAH patients and controls.
Methods
We conducted a survey of PAH patients (n = 37) attending the Pulmonary Hypertension Association International Conference from 29 June–1 July 2018 (VU IRB #180738), where a voluntary Research Room facilitated patient enrollment in multiple studies. All participants completed a universal demographic form, which included questions about PAH diagnosis, family history, etiology of PAH, anthropometric data, functional class (FC), and medications. Informed written consent was obtained before enrolling in our study. Volunteers without PAH attending the research room (n = 16) were also invited to participate and completed a separate demographic survey. We separately obtained demographic and daily step count data from a cohort of healthy volunteers (n = 24) (VU IRB #172129). All participants were asked what type of device they used and to provide their average daily step count over the longest available period (at least one week, up to one year). For the purposes of this study, daily step count was the only variable obtained from these devices.
Descriptive statistics are reported as median and interquartile range, or number and percent. Variables are compared between PAH patients and healthy controls by Chi-square test or Mann–Whitney U test, as appropriate. To examine the effect of PAH on daily step count, a regression model of average daily step count was developed with PAH status as the main predictor, and adjusted for the confounders age, body mass index (BMI), sex, and device (smartphone/wearable). Confounders were pre-specified based on clinical knowledge. Patients with missing data were excluded in the regression model. Analysis was performed using Stata version 15.1 for Mac (StataCorp, College Station, TX, USA).
Results
Complete demographics and clinical characteristics of the study population are provided in Supplementary Table 1. PAH patients were older than controls (56 years vs. 35 years, P = 0.0004); 89% were women compared to 73% of controls (P = 0.065). The two groups had similar racial and ethnic composition (86% vs. 80% white in PAH patients vs. controls, P = 0.448), as well as BMI (26.4 vs. 26.0 in PAH patients vs. controls, P = 0.6746). Idiopathic PAH was the most common etiology of PAH (70%), followed by connective tissue disease-associated PAH (22%) and heritable PAH (8%). The PAH patients were World Health Organization FC I (26%), II (57%), and III (17%). Medication information was obtained from 30/37 (81%) PAH patients, 90% of whom were on combination therapy, 30% were on parenteral prostanoids, and 46% were on diuretics.
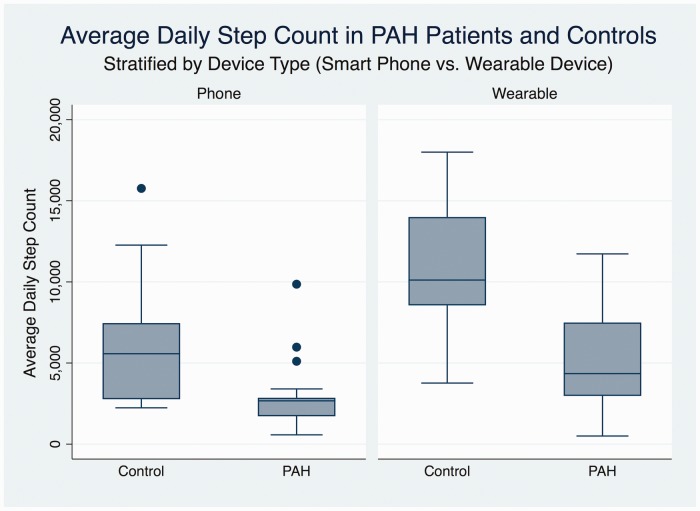
Step count data were derived from commercially available wrist-worn fitness devices in 43/77 (56%) of participants, and from a smartphone in the remainder. This was similar in PAH patients (57%) and controls (55%). Recorded average daily step counts were significantly lower in PAH patients than controls (2681 vs. 5573 for smartphones; 4901 vs. 10114 for wearable devices; P = 0.0001; Fig. 1).
Fig. 1.
Box plot displaying median, interquartile range, and 95% confidence interval of average daily step count as recorded by smartphones and wearable devices in pulmonary arterial hypertension (PAH) patients and controls. Dots represent outliers.
In the regression model, PAH status was significantly related to daily average step count (β = −3030.475, P = 0.01), after adjusting for confounders, including type of device. PAH patients on average walked 3030 (95% confidence interval = 759–5302) fewer steps than healthy people did.
Discussion
Our survey of PAH patients and healthy controls shows that routinely used devices detect a significantly lower daily step count in PAH patients, whether measured by wearable fitness device or smartphone, in an observational study free from the Hawthorne effect. The step counts recorded by control participants using wearable fitness devices are in the middle of the range reported in studies using clinical pedometers in this age group, suggesting that this group is representative of a healthy population, and wearable fitness devices capture similar step counts to previously studied pedometers.6
The finding that PAH patients have a lower average daily step count than healthy controls confirms previous findings and suggests that these devices could potentially be used to track clinical status and symptom burden in between office visits and formal exercise capacity testing.4 Some patients already use these devices to track response to therapy and set daily activity goals; clinicians may wish to utilize this information when available. Daily activity level, as measured by clinical accelerometers, is under investigation as a potential end point in adult and pediatric PAH clinical trials (ClinicalTrials.gov Identifier NCT03078907).7 There are also ongoing clinical trials to investigate whether wearable fitness devices can serve as an intervention to improve daily activity and clinical outcomes in PAH patients (ClinicalTrials.gov Identifiers NCT03069716 and NCT03043976).
There are a number of reasons why smartphones may record fewer average daily steps than wearable fitness devices; this finding raises important caveats that must be used in comparing step counts between devices. It may be that individuals who wear fitness devices do, in fact, have higher daily activity levels than those who track their steps using a smartphone because they are a self-selected and motivated group. However, it is also possible that smartphones failure to capture as many steps because they are left behind for short trips around the home, office, or while exercising. Furthermore, the accelerometer in a smartphone carried in a bag or purse may not be as sensitive as one worn on a wrist. Previous studies have shown that smartphone apps (while carried in a pocket) and wearable devices perform similarly in providing step counts under direct observation conditions, with some inter-device variation, but we are unaware of any studies comparing the two classes of devices under free-living conditions.8 Further research, including direct comparison of smartphones and wearable devices within the same individuals, would be required before concluding that smartphones are inferior to wearable devices in this regard.
This study has multiple limitations. It is a small, cross-sectional, observational study of PAH patients that may not be representative of a national or international cohort. Furthermore, the self-reported variables, such as diagnosis and etiology of PAH on the demographic questionnaire, were not independently validated by clinicians. The observational nature of this study does not allow for controlling of many potential confounders in determinates of measured daily activity levels. There is also a significant imbalance in age and gender between PAH patients and controls, and despite controlling for this in our regression model, residual confounding is likely. However, this is the first study we are aware of to report daily activity levels in PAH patients using common commercial devices, and the significant differences found between PAH patients and healthy controls, and between different devices may have implications for clinical care given the rapid emergence and availability of these technologies.
Supplementary Material
Acknowledgments
The authors thank Dr. Kara Goss, the leadership of the Pulmonary Hypertension Association, and all of the research room participants and volunteers at the PHA Conference in 2018.
Conflict of interest
ARH has served as a consultant to Actelion, Bayer, GSK, Accleron, United Therapeutics, and Pfizer. She has received research/grant support from the NIH and Cardiovascular Medical Research and Education Fund. ELB has served as a consultant for Hovione Pharmaceuticals.
Funding
SJH is supported by NIH grant T32 HL087738-12; ELB is supported by NIH grant R34HL136989-01, the American Heart Association (13FTF16070002), and Gilead Sciences Scholars Program in Pulmonary Arterial Hypertension. ARH is supported by NIH grant UO1HL125212-01.
Ethical approval
This study was approved by the Vanderbilt University Internal Review Board (IRBs #172129 and #180738) and the Pulmonary Hypertension Association Research Room Committee (RR18).
References
- 1.Farber HW, Miller DP, Poms AD, et al. Five-Year outcomes of patients enrolled in the REVEAL Registry. Chest 2015; 148(4): 1043–1054. [DOI] [PubMed] [Google Scholar]
- 2.Mainguy V, Provencher S, Maltais F, et al. Assessment of daily life physical activities in pulmonary arterial hypertension. PLoS One 2011; 6(11): e27993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matura LA, Shou H, Fritz JS, et al. Physical activity and symptoms in pulmonary arterial hypertension. Chest 2016; 150(1): 46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pugh ME, Buchowski MS, Robbins IM, et al. Physical activity limitation as measured by accelerometry in pulmonary arterial hypertension. Chest 2012; 142(6): 1391–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ulrich S, Fischler M, Speich R, et al. Wrist actigraphy predicts outcome in patients with pulmonary hypertension. Respiration 2013; 86(1): 45–51. [DOI] [PubMed] [Google Scholar]
- 6.Tudor-Locke CE, Myers AM. Methodological considerations for researchers and practitioners using pedometers to measure physical (ambulatory) activity. Res Q Exerc Sport 2001; 72(1): 1–12. [DOI] [PubMed] [Google Scholar]
- 7.Zijlstra WMH, Ploegstra MJ, Vissia-Kazemier T, et al. Physical activity in pediatric pulmonary arterial hypertension measured by accelerometry. A candidate clinical endpoint. Am J Respir Crit Care Med 2017; 196(2): 220–227. [DOI] [PubMed] [Google Scholar]
- 8.Case MA, Burwick HA, Volpp KG, et al. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA 2015; 313(6): 625–626. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.