Abstract
Purpose
To explore the availability and utilization of workplace health supports by employees of small and large-sized employers.
Design
Cross-sectional telephone-based interviews collected on 16 workplace health supports for physical activity and diet.
Setting
Participants selected by random-digit-dialing from four metropolitan areas of Missouri employees from 2012-2013.
Participants
2,015 working adults.
Methods
We explored the availability and use of supports by employer size (<100 employees versus ≥100 employees), accounting for industry and personal factors.
Analysis
We examined distributions and Poisson regression models of availability of supports by employer size and by industry, and use of supports by employer size and personal factors.
Results
One-fifth of the 1,796 employees were employed by small-sized employers. Large employers offered more supports than small (mean: 6 versus 3); but a higher proportion of employees of small-sized employers used supports when available (59% versus 47%). The differences in offered supports between industries were not due to size alone. In regards to the determinants of participation, the personal factors of gender, age, weight, and income were associated with participation in ten of the supports. Employer size was also associated with participation in ten supports. No associations were found between personal factors or workplace size and participation for three supports.
Conclusion
A higher proportion of employees working for smaller businesses use available supports than employees of larger businesses. Supports offered by employers should target the needs and interests of the workforce, particularly for the higher risk low-income employees.
Keywords: Health behaviors, small businesses, health disparities, supportive environments, workplace
In Brief
This paper explores the availability and utilization of workplace health supports by employees of small (<100 employees) and large-sized employers (≥100 employees). Survey data was collected on 1,796 employees randomly selected from four metropolitan areas of Missouri on 16 workplace health supports for physical activity and diet. Employee responses were evaluated by employer size based on overall company size and size at the work location. Large employers offered more supports than small (mean: 6 versus 3); but a higher proportion of employees of small-sized employers used supports when available (59% versus 47%). Personal factors of gender, age, weight, and income were independently associated with participation in ten of the supports. Participation availability and use also differed by the type of industry. These data may guide employers toward tailoring health promotion programs based on their company size, industry, and personal characteristics of their workforce to improve participation and better promote health.
PURPOSE
With more than one-third of current U.S. employees’ suffering from one or more chronic diseases including heart disease, cancer, diabetes, stroke, and musculoskeletal disorders,1,2 the worksite has been recognized as an appropriate and cost-effective setting for conducting preventive health interventions among large and diverse populations. Working Americans spend much of their time at the workplace, which can provide convenient access to working adults and regular opportunities to communicate through existing channels.3
The majority of small business owners (93%) report that the health of their employees is very important to their bottom line, yet most (78%) offer no health promotion programs4,5 or limit their programs to “awareness” supports such as web-based resources and wellness newsletters.6,7 These owners cite lack of program expertise, lack of employee interest, and uncertain return on investment 8 as common barriers to developing more comprehensive programs. In addition, many small companies struggle with their financial security and have limited resources for activities not directly related to their business.9 Yet, there are advantages to working within a smaller, more intimate work group. The few organizational levels between owner and employee creates a more casual environment, greater familiarity between employees, a more visible senior leadership, and less formality of rules so changes to policies and the workplace environment can be executed more easily.10 Program participation could potentially be enhanced by co-worker support in a smaller setting.
Many workplace health promotion programs report positive results for improving employee health,11 increasing physical activity,3,12 improving weight status13, and improving dietary behaviors.14 These programs also describe benefits for employers through decreased work absences,15 increased work ability,16 and lower turnover rates.17 Workplace health promotion programs are common in large businesses8 who have the financial means to hire consultants or designate employees to develop and implement health promotion programs.18 These programs are often described in companies from the education and healthcare industry8 but less is known about other industries. Although these programs have been growing in popularity in large workplaces, managers of these programs report that awareness and participation by employees is generally low.19,20 A systematic review of the determinants of participation in health promotion programs showed that the influence of personal factors on participation varied by the type of health support; many of these programs did not account for the effects of work factors on participation of employees.21
Even though health promotion programs may reduce the health risks for some chronic disorders, little is known about the type of programs offered by different industries, and if programs are offered, to what degree work and personal characteristics influence participation in the programs. The purpose of this study was to examine the availability and use of workplace health promotion supports by employees from various sized employers, across various industries, and across different personal factors. We hypothesized that more employees of larger employers would report having more supports available, but that a higher proportion of employees’ of smaller employers would report use of available supports, regardless of personal factors.
METHODS
Design
Cross-sectional, telephone-based interview data on 2,015 participants were collected as part of the Supports at Home and Work for Maintaining Energy Balance (SHOW-ME) study. The SHOW-ME study explored associations between workplace environmental and policy influences on individual physical activity and nutrition behaviors.22 The design and conduct of the SHOW-ME study are described in detail elsewhere.7,23
Study sample
The SHOW-ME study recruited participants living within four metropolitan areas of Missouri (St. Louis, Kansas City, Columbia, and Springfield) based on home census tracts. A multistage, stratified sampling procedure was used to sample participants within census tracts from seven strata: metro size (large vs. small), and within large metro areas walkability (low, moderate, and high), and percent racial/ethnic minority (low vs. high).7
Participants were recruited through random-digit-dialing of resident landline telephone numbers purchased from a commercial marketing group in Missouri and interviews were conducted between April 2012 and April 2013. The first eligible adult to volunteer from each household was recruited to participate. Eligible participants were between 21 and 65 years of age, employed at least 20 hours per week at a single worksite outside the home by an employer with at least five employees. Participants were not pregnant, nor had any physical limitations that inhibited walking or bicycling in the past week. Participants provided verbal informed consent and were compensated for their participation. The Institutional Review Board of Washington University in St. Louis approved the study.
Measures
SHOW-ME Survey.
The survey captured individual, environmental, and organizational items pertaining to diet and physical activity around and within the workplace. The measure covered personal demographics including age, weight, and comorbid conditions; employment information including job title, industry, work hours, breaks, and number of employees at the work location; self-reported diet and physical activity behaviors; and a list of workplace supports. Self-reported height and weight were used to calculate body mass index (BMI) and to determine obesity status as normal (BMI ≤ 25), overweight (BMI >25 to < 30), or obese (BMI ≥ 30).The survey included 31 workplace supports that addressed physical activity, nutrition, and health behaviors. The support items were either new or adapted from existing instruments that had acceptable reliability.24,25
Participants were asked to report on the availability of 31 health-related supports at their workplace (yes, no, don’t know/not sure). For 16 of these supports, participants were also asked to report on their use of the support if it was available. The time frame for use differed by support with reference to the “past two months” for most supports; “ever” for use of the cafeteria, use of personal services, or participation in a health fair or challenge event; and “at least once a week” for vending machine purchases. The 16 workplace supports assessed for use were categorized into four groups: informational, wellness initiatives, environmental, and workplace policy.
Industry and Employer size.
Using the employer information including self-reported industry, occupation, and employer name and work address, each employer was assigned a standard industry code from the North American Industry Classification System (NAICS) and an employer size. The data was extracted using a publically available online tool, Reference USA (Ref-USA) that provides business-related data on more than 45 million companies.26 Using Ref-USA, two of the authors knowledgeable about job codes (AMD, CE) independently assigned the primary NAICS code and recorded the reported number of employees for both the overall company and for the location corresponding to the participant provided work address. For employers not found in Ref-USA, other web-based resources were used (NAICS code look-up, company website, LinkedIn, Manta).27 Discrepancies between the independent coders were resolved by consensus.
Employer size was dichotomized as less than 100 employees (small) versus 100 or more employees (large) for the overall size, as well as for the employer size at each work location or address. Each participant was assigned a combination employer size category based on overall company size, and by size by the work location: large company/large location (LL), large company/small location (LS), small company/small location (SS).
Analysis
We examined distributions of the availability and use of each workplace health promotion support by employer size using the combination employer size variable (LL, LS, SS). We also examined the availability of each support by 10 industry groups. Then we assessed the use of each support in separate Poisson regression models to examine the effects of employer size after adjusting for the individual factors of age, gender, body mass index, and income. All analyses were conducted using SPSS 23.0.28
RESULTS
Of the 2,015 participants who completed the SHOW-ME survey, 219 participants were excluded from analysis due to lack of job information, providing 1,796 participants for the analytic sample. Most of the participants (n=1,728) were assigned a NAICS code. The sample was predominately female, Caucasian, had a mean age of 48 years (SD 11), and was evenly distributed across the three BMI categories (Table 1). Most participants worked for a large-sized employer (80.5%) and many of these participants worked at locations considered large-sized (LL = 951, 52.95%) with fewer working at locations considered small (LS= 495, 27.5%). The smallest proportion of the sample worked for small companies at small locations (SS= 350, 19.5%). There was no difference in employee’s pre-existing medical conditions by the size of the business, but there were more current daily smokers employed by small employers (SS= 21.4%) than large (LL=10.1%; LS= 13.1%). Racial distributions were similar across company size groupings. Approximately twenty percent of the sample had a high school education or less and/or an annual income of less than $30,000. Lower incomes were most common among employees who worked in the food industry (52%) followed by the service (33%) and trade (26%) industries. Healthcare and social assistance industry employed the largest portion of the sample (21.5%) followed by educational services (16.4%). The fewest number of employees were employed by blue collar and agricultural jobs (4.8%), manufacturing (4.9%), and food services (5.0%). Most participants in each industry reported working for a large-sized employer at a large location, except for participants in the trade industry (46% employed by large-sized employers), service industry (34% employed by large-sized employers), and accommodation / food service (17% employed by large-sized employers).
Table 1.
Characteristics of participants and Employment by Industry and Employer size*, n=1,796: Supports at Home and Work for Maintaining Energy Balance (SHOW-ME) study, Missouri, USA, 2012-2013
| Characteristics | No. | % | SS % (n=350) |
LS % (n=495) |
LL % (n=951) |
|---|---|---|---|---|---|
| Age (years) | |||||
| 21-34 | 265 | 14.8 | 15.2 | 18.5 | 12.7 |
| 35-44 | 363 | 20.2 | 18.9 | 18.7 | 21.6 |
| 45-54 | 585 | 32.6 | 32.1 | 30.5 | 34.0 |
| 55+ | 568 | 31.6 | 33.8 | 32.3 | 30.5 |
| Gender | |||||
| Male | 583 | 32.5 | 37.4 | 30.1 | 31.9 |
| Female | 1211 | 67.4 | 62.6 | 69.9 | 67.9 |
| BMI (kg/cm2) | |||||
| Normal (≤25) | 576 | 32.1 | 39.4 | 29.7 | 30.6 |
| Overweight (26-29) | 556 | 31.0 | 29.7 | 32.1 | 30.8 |
| Obese (≥30) | 579 | 32.2 | 27.4 | 34.1 | 33.0 |
| Race | |||||
| Caucasian | 1139 | 63.4 | 67.7 | 62.0 | 62.6 |
| African American | 523 | 29.1 | 23.1 | 29.5 | 31.1 |
| Other^ | 116 | 6.5 | 8.0 | 7.7 | 5.3 |
| Education | |||||
| High School or less | 379 | 21.1 | 29.4 | 24.8 | 16.1 |
| Some college or graduated | 1023 | 57.0 | 56.9 | 52.1 | 59.5 |
| Postgraduate | 389 | 21.7 | 14.0 | 22.6 | 24.3 |
| Income | |||||
| Less than 30k | 333 | 18.5 | 25.4 | 24.2 | 13.0 |
| 30-59k | 589 | 32.8 | 33.4 | 30.3 | 33.9 |
| 60k or more | 773 | 43.0 | 36.0 | 39.0 | 47.7 |
| NAICS Sector | SS % (n=308)** |
LS % (n=475)** |
LL % (n=856)** |
||
| Health Care and Social Assistance | 387 | 21.5 | 23.7 | 17.1 | 27.2 |
| Educational Services | 295 | 16.4 | 6.5 | 25.7 | 17.9 |
| Public Administration | 98 | 5.5 | 1.6 | 6.1 | 7.5 |
| Trade | 202 | 11.2 | 14.3 | 13.7 | 10.9 |
| Finance and Insurance | 101 | 5.6 | 3.6 | 5.9 | 7.2 |
| Manufacturing | 88 | 4.9 | 6.2 | 2.7 | 6.5 |
| Accommodation and Food Services | 89 | 5.0 | 7.8 | 10.5 | 1.8 |
| Blue collar and Agriculture | 87 | 4.8 | 8.1 | 3.6 | 5.3 |
| Professional | 180 | 10.0 | 13.3 | 8.8 | 11.3 |
| Service | 112 | 6.2 | 14.9 | 5.9 | 4.4 |
Small defined as < 100 employees; SS= small company/small location, LS= large company/small location, LL=large company/large location
American Indian, Alaskan Native, Native Hawiian or other Pacific Island, Asian, other
missing values due to incomplete job information for NAICS code assignment
NAICS: Industry NAICS codes: Healthcare and Social Assistance (62); Educational Services (61); Public Administration (92); Trade (Wholesale (42), Retail (44,45)); Finance and Insurance (52); Manufacturing (31,32,33); Accommodation and Food Services (72), Blue Collar and Agriculture (Agriculture, Forestry, Fishing and Hunting (11), Mining (21), Utilities (22), Construction (23), Transportation and Warehousing (48,49)); Professional (Information (51), Real Estate Rental and Leasing (53), Professional, Scientific, and Technical Services (54), Management of Companies and Enterprises (55), Arts, Entertainment, and Recreation (71)); Service (Administrative and Support and Waste Management and Remediation Services (56), Other Services (except Public Administration) (81)).
Participants reported the availability of an average of six workplace supports (SD 4) at their work location, with a range from 0 to 31 supports. On average, participants reported using three of the available supports (SD 2) at their work location, with a range from 0 to 16 supports. The most commonly available supports reported by employees were vending machines (76.1%), area to lock bikes (56.3%), health fairs (50.6%), and cafeterias (50.3%) (Table 2). Supports that were reported available at their workplace by the lowest number of participants were incentives to bike or walk (8.2%), or to take public transportation (18.1%) to work, availability of maps for walking (18.2%), and policies for physical activity breaks (14.4%).
Table 2.
Availability of workplace supports overall and by industry: Supports at Home and Work for Maintaining Energy Balance (SHOW-ME) study, Missouri, USA, 2012-2013
| Type of support | Overall (N=1796) |
Health Care and Social Assistance (N = 387) |
Educational Services (N = 295) |
Public Administration (N = 98) |
Trade (N = 202) |
Finance and Insurance (N = 101) |
Manufacturing (N = 88) |
Accommodation and Food Services (N = 89) |
Blue collar and Agriculture (N = 87) |
Professional (N = 180) |
Service (N = 112) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Informational Supports | |||||||||||
| Maps for Walking % | 18.2 | 24.7 | 20.6 | 25.0 | 12.1 | 15.5 | 15.1 | 20.2 | 15.1 | 14.9 | 12.3 |
| Health Fairs % | 50.6 | 65.3 | 71.1 | 68.0 | 29.9 | 59.8 | 50.6 | 19.3 | 38.6 | 42.4 | 26.4 |
| Wellness Initiatives | |||||||||||
| Challenge Events % | 47.6 | 61.2 | 61.0 | 67.0 | 35.2 | 57.7 | 44.2 | 16.9 | 37.2 | 39.7 | 28.2 |
| Exercise Programs % | 36.6 | 47.3 | 54.5 | 62.8 | 19.4 | 37.9 | 34.5 | 11.4 | 23.3 | 29.6 | 22.5 |
| Free/Reduced Cost | 30.5 | 39.5 | 35.0 | 35.6 | 25.3 | 47.3 | 30.9 | 9.1 | 32.2 | 42.2 | 14.0 |
| Gym Membership % | |||||||||||
| Incentives to Bike/Walk to Work % | 8.2 | 9.0 | 8.5 | 9.5 | 8.6 | 6.3 | 5.8 | 6.9 | 12.6 | 5.6 | 10.2 |
| Incentives for Public Transit % | 18.1 | 29.3 | 14.9 | 39.4 | 6.1 | 20.2 | 7.1 | 14.9 | 17.9 | 20.7 | 10.3 |
| Personal Services for Fitness & Nutrition % | 47.9 | 62.9 | 55.7 | 70.8 | 36.7 | 55.7 | 48.8 | 21.3 | 43.5 | 42.0 | 27.0 |
| Environmental Supports | |||||||||||
| Indoor Exercise Facilities % | 35.9 | 47.7 | 54.1 | 56.1 | 12.9 | 38.6 | 31.8 | 12.4 | 27.6 | 23.3 | 18.9 |
| Outdoor Exercise Facilities % | 29.1 | 29.4 | 66.4 | 24.0 | 10.9 | 27.0 | 26.1 | 8.0 | 18.4 | 20.6 | 16.5 |
| Shower Facilities % | 33.7 | 38.2 | 44.1 | 50.5 | 18.1 | 35.0 | 44.3 | 13.6 | 35.6 | 30.2 | 22.3 |
| Area to Lock Bike % | 56.3 | 58.3 | 72.7 | 71.1 | 55.6 | 48.9 | 51.2 | 54.1 | 55.3 | 53.8 | 52.8 |
| Cafeteria % | 50.3 | 61.5 | 68.5 | 46.9 | 26.7 | 63.4 | 42.0 | 49.4 | 34.5 | 44.4 | 28.8 |
| Vending Machines % | 76.1 | 80.2 | 88.1 | 88.8 | 73.8 | 85.1 | 87.5 | 29.2 | 69.0 | 75.6 | 63.1 |
| Policy Supports | |||||||||||
| Flextime for PA % | 36.1 | 34.2 | 38.9 | 48.5 | 26.6 | 45.5 | 33.7 | 26.1 | 32.9 | 44.6 | 34.5 |
| PA Breaks % | 14.4 | 17.9 | 12.4 | 17.0 | 14.3 | 11.2 | 12.8 | 14.6 | 16.1 | 11.2 | 13.4 |
Industry NAICS codes: Healthcare and Social Assistance (62); Educational Services (61); Public Administration (92); Trade (Wholesale (42), Retail (44,45)); Finance and Insurance (52); Manufacturing (31,32,33); Accommodation and Food Services (72), Blue Collar and Agriculture (Agriculture, Forestry, Fishing and Hunting (11), Mining (21), Utilities (22), Construction (23), Transportation and Warehousing (48,49)); Professional (Information (51), Real Estate Rental and Leasing (53), Professional, Scientific, and Technical Services (54), Management of Companies and Enterprises (55), Arts, Entertainment, and Recreation (71)); Service (Administrative and Support and Waste Management and Remediation Services (56), Other Services (except Public Administration) (81)).
We explored differences in the availability of workplace health supports by type and size of industry. Employees of small businesses were less likely to report availability of most workplace supports compared to employees of large businesses, and were more likely to report having no workplace supports available (14.6% versus 3.2%). Many differences were reported in availability of supports across industries (Table 2), in part associated with employer size, with lower availability among those industries with more small sized employers. However, there were notable differences in the number of supports offered between industries, even among those industries with more than 20% of workers in small sized employers. For example, supports were more common in Manufacturing compared to Accommodation/Food Service for health fairs (51% vs 19%), gym memberships (31% vs 9%), personal services (49% vs 21%), and shower facilities (44% vs 14%).
While employees of small businesses were less likely to report availability of most workplace supports than employees of large businesses, we found that a higher proportion of employees of small businesses reported using available supports than employees of large businesses, as shown in Figure 1. Compared to employees of large businesses, more small business employees used the available supports for exercise programs (54% vs 31%), free/reduced gym membership (49% vs 22%), incentives to bike/walk to work (43% vs 19%), and incentives for public transportation (57% vs 25%). Only one support, health fairs, showed a lower participation for small business employees compared to large (65% vs 75%). Most workplace supports for the mixed employer group (large sized parent company but small sized by location) were offered nearly twice as often as at small businesses but not as often as large employers at large location (LL). Use of the available workplace supports by employees of these large employers at small locations was intermediate between use by employees of small businesses and use by employees at large work locations.
Figure 1:
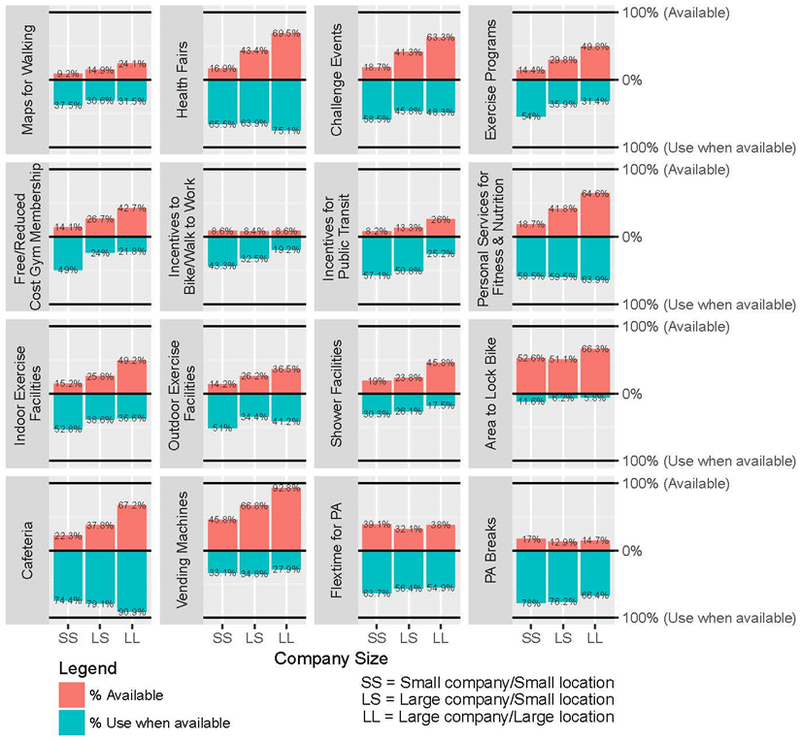
Availability and use of workplace supports based on employer size of the overall company and work location, n=1,796: Supports at Home and Work for Maintaining Energy Balance (SHOW–ME) study, Missouri, USA, 2012–2013
We evaluated other determinants of employees’ use of available workplace supports in separate regression models evaluating the use of supports by the size of employer, adjusted for individual factors (age, gender, BMI, and income) as shown in Table 3. In seven of the 16 workplace support models, employees of small employers reported greater likelihood of using available supports compared to employees of larger employers. For example, relative to employees at large locations, employees at small employers and locations are 31% more likely to use challenge events, 75% more likely to use exercise programs, 157% more likely to use free or reduced gym memberships, 86% more likely to use incentives for public transportation, 40% more likely to use indoor exercise equipment, 67% more likely to use available showers, and 19% more likely to use flextime for physical activity for supports that are available. In addition to greater participation related to employer’s small-size, use of some supports was also related to employee characteristics. For example, challenge events were more commonly used by females, employees of overweight and obese categories, and those with higher income. A higher proportion of lower income workers used incentives for biking/walking to work, use of public transportation, and vending machine purchases than employees with higher incomes. A lower proportion of participants in the oldest age group (55 years and older) reported using indoor exercise facilities compared to the youngest. Fewer men reported using supports than women (shower facilities, free gym membership, vending machines, and areas to lock bikes). Employer size and individual factors had no effect on the use of five supports (maps for walking, personal services for fitness and nutrition, and physical activity breaks).
Table 3.
Multiple regression models of use of supports by employer size, adjusting for personal factors: Supports at Home and Work for Maintaining Energy Balance (SHOW-ME) study, Missouri, USA, 2012-2013
| Type of support | N | Employer size* |
Employer size RR (95% CI) |
Significant covariates |
|---|---|---|---|---|
| Informational Supports | ||||
| Maps | 293 | SS | 1.13 (0.68-1.88) | N/A |
| LS | 0.96 (0.63-1.45) | |||
| Health Fairs | 819 | SS | 0.96 (0.80-1.15) | age, gender, income |
| LS | 0.87 (0.77-0.97) | |||
| Wellness Initiatives | ||||
| Challenge Events | 772 | SS | 1.31 (1.04-1.65) | age, BMI, gender, income |
| LS | 0.95 (0.79-1.14) | |||
| Exercise Programs | 600 | SS | 1.75 (1.32-2.32) | age |
| LS | 1.09 (0.83-1.43) | |||
| Free/Reduced Cost Gym Membership | 494 | SS | 2.57 (1.80-3.65) | gender |
| LS | 1.14 (0.78-1.67) | |||
| Incentives to Bike/Walk to Work | 130 | SS | 1.74 (0.88-3.43) | income |
| LS | 1.32 (0.69-2.55) | |||
| Incentives for Public Transit | 279 | SS | 1.86 (1.23-2.80) | income |
| LS | 1.62 (1.12-2.35) | |||
| Personal Services for Fitness & Nutrition | 776 | SS | 0.98 (0.78-1.23) | N/A |
| LS | 0.96 (0.84-1.10) | |||
| Environmental Supports | ||||
| Indoor Exercise Facilities | 579 | SS | 1.40 (1.04-1.87) | age |
| LS | 1.08 (0.83-1.40) | |||
| Outdoor Exercise Facilities | 468 | SS | 1.33 (0.99-1.80) | income |
| LS | 0.84 (0.63-1.10) | |||
| Shower Facilities | 550 | SS | 1.67 (1.09-2.58) | gender, income |
| LS | 1.47 (1.00-2.18) | |||
| Area to Lock Bike | 907 | SS | 1.51 (0.88-2.61) | gender |
| LS | 0.79 (0.386-1.60) | |||
| Cafeteria | 814 | SS | 0.81 (0.696-0.93) | N/A |
| LS | 0.86 (0.792-0.94) | |||
| Vending Machines | 1242 | SS | 1.15 (0.90-1.48) | BMI, gender, income |
| LS | 1.20 (1.00-1.45) | |||
| Policy supports | ||||
| Flextime for Physical Activity | 591 | SS | 1.19 (1.01-1.41) | N/A |
| LS | 1.02 (0.85-1.22) | |||
| Physical Activity Breaks | 239 | SS | 1.17 (0.97-1.42) | N/A |
| LS | 1.10 (0.91-1.32) | |||
SS small employer/small location; LS large employer/small location; LL large employer/ large location; RR Relative Risk
Poisson regression models to show the prevalence ratio of employer size for each health support. Multivariable models adjusted for gender, bmi, age, and income.
Employer size reference: LL
DISCUSSION
Results from our study corroborate previous findings showing smaller businesses provide fewer workplace supports for their employees than larger businesses; our study also documented variation across industries in the number of workplace supports offered to employees. A new and important finding of this study is that a higher proportion of the employees of small businesses reported use of available supports than did employees of large companies. Employees’ reported use of many workplace supports was also associated with demographic factors, while use of some supports showed no association with either employer size or individual factors.
Our study found that company size was related to the number of health promotion initiatives offered to employees. Supports that require greater time and resources to implement were far less available at small businesses compared to large-sized businesses, similar to results of Hannon and colleagues.20 One novel aspect of the current study was the description of an intermediate employer group: small work locations of a larger parent company. At these companies, events that were linked to a larger parent company like health fairs and challenge events were more commonly available at small work locations than for small parent companies; perhaps because such programs, benefits, and events can be designed and funded at the corporate level of large companies and delivered at the local level. In contrast, environmental supports that required more equipment and space were less common in these intermediate employers.
Workplace health promotion programs and activities also differed by industry. Similar to past studies, the largest number of supports were offered in Education and Healthcare, and the lowest number of supports in Trade, Service, and Food industries.18,29 While some of these differences between industries are likely driven by employer size, we found differences in the type and availability of supports between similar sized employers across industries.
A unique contribution of this study was the collection of individual level data on use of available workplace supports in addition to the availability of supports. This allowed us to demonstrate that a higher proportion of employees of small businesses utilize available workplace supports than employees at larger employers. This effect has not previously been described across a range of workplace supports, though a few previous studies demonstrated an association between participation in a smoking cessation program and employer size and type of industry.30,31 As noted by McCoy,30 it may be the use of available supports is higher at small businesses since they have a greater ability to customize programs to meet their employee’s needs, implementation may be less bureaucratic in the smaller setting, management may be more visibly engaged, and there may be greater teamwork and co-worker support in smaller work settings. Understanding the reasons for this observed effect may lead to strategies to increase participation in available workplace health supports; relatively low participation is an issue across programs at most employers.
Similar to other studies, the current study showed the use of supports varied by personal and workplace characteristics. A systematic review on determinants of participation showed personal characteristics were important for participation in only some supports, but many of the studies had small samples sizes and did not account for type nor size of the business.21 Our study showed similar findings- personal factors were important for the use of some supports. For example lower income and obese participants tended to frequent the vending machines, and higher use of transportation incentives among participants with lower income. These health supports were used based on a personal need or behavior, but they may be used to promote physical activity and good nutrition.
This study had several limitations. Even though recruitment used random selection from a large market sample, the use of landline telephone numbers may have biased the sample. At the time of this study, approximately 22.4% of the Missouri population solely used cell phones, slightly lower than the US population (27.3%).32 Our study polled metropolitan areas of Missouri, and may not represent rural populations. Employees’ reports of the availability of workplace health supports may underreport their true availability by their employer, but instead represents workers’ knowledge of available benefits. Strengths of this study include the large sample, broad range of industries captured, and information about both the workplace supports that were offered as well as the employees’ self-reported use of the supports. This design allowed us to demonstrate the new findings that employees of some smaller businesses and smaller locations of larger employers are more likely to use available workplace supports when offered. In addition, our study was able to evaluate individual participation based on personal factors across a wide range of supports, demonstrating strong associations for some supports and no associations for others.
Future studies should explore how employers of different size, industry, and workplace demographics can tailor workplace-based prevention programs toward the personal factors of their workers and work organization. Smaller businesses may use their flatter organizational structure and informal communication lines to identify the unique needs and preferred supports of their workers, and means to implement them throughout the company. There is a public health need to provide greater health supports for employees in small establishments, particularly since other health disparities may be more prevalent in many small businesses. For larger employers, it is important to recognize that adding more supports does not guarantee successful healthy behaviors - much work remains to be done to understand workplace culture and increase participation rates in workplace based health promotion offerings. Designing health activities and programs with employee input will likely improve the relevance of the activities to the workgroup and support buy-in for participation.
So What?
What is already known on this topic?
Many workplace health promotion programs report positive results for improving employee health, yet most small business owners offer no or limited health promotion programs despite expressing concern for their employees health.
What does this article add?
These results add to the small body of literature describing the disparity in access to comprehensive workplace health promotion programs between small and large employers. Variation in use of available programs also differed by employer size, by industry, and by demographic factors.
What are the implications for health promotion practice or research?
Tailoring programs to meet the needs of different worker groups may improve participation and better promote health.
Acknowledgments
Funding:
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Transdisciplinary Research on Energetics and Cancer Center at Washington University in St. Louis, funded by the National Cancer Institute at the National Institutes of Health (U54 CA155496-01), Washington University in St. Louis, and the Alvin J. Siteman Cancer Center; and supported by the Healthier Workforce Center of the Midwest (NIOSH Grant No. U19OH008858).
Footnotes
Conflict of Interest Statement:
The Authors declares that there is no conflict of interest.
REFERENCES
- 1.Linnan LA, Sorensen G, Colditz G, Klar DN, Emmons KM. Using theory to understand the multiple determinants of low participation in worksite health promotion programs. Health education & behavior : the official publication of the Society for Public Health Education. 2001;28(5):591–607. [DOI] [PubMed] [Google Scholar]
- 2.Laing SS, Hannon PA, Talburt A, Kimpe S, Williams B, Harris JR. Increasing evidence-based workplace health promotion best practices in small and low-wage companies, Mason County, Washington, 2009. Prev Chronic Dis. 2012;9:E83. [PMC free article] [PubMed] [Google Scholar]
- 3.Katz DL, O’Connell M, Yeh MC, et al. Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recomm Rep. 2005;54(Rr-10):1–12. [PubMed] [Google Scholar]
- 4.Mattke S, Liu H, Caloyeras J, et al. Workplace Wellness Programs Study: Final Report. Rand health quarterly. 2013;3(2):7. [PMC free article] [PubMed] [Google Scholar]
- 5.National Small Business Association. Workplace wellness programs in small business: Impacting the bottom line. 2012. http://www.nsba.biz/wp-content/uploads/2012/09/wellness-survey-v3.pdf.
- 6.Claxton G, Rae M, Panchal N, et al. Health benefits in 2013: moderate premium increases in employer-sponsored plans. Health Aff (Millwood). 2013;32(9):1667–1676. [DOI] [PubMed] [Google Scholar]
- 7.Hipp JA, Reeds DN, van Bakergem MA, et al. Review of measures of worksite environmental and policy supports for physical activity and healthy eating. Prev Chronic Dis. 2015;12:E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linnan L, Bowling M, Childress J, et al. Results of the 2004 National Worksite Health Promotion Survey. Am J Public Health. 2008;98(8):1503–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Legg SJ, Olsen KB, Laird IS, Hasle P. Managing safety in small and medium enterprises. Safety Science. 2015;71, Part C:189–196. [Google Scholar]
- 10.Goetzel RZ, Liss-Levinson RC, Goodman N, Kennedy JX. Development of a community-wide cardiovascular risk reduction assessment tool for small rural employers in upstate New York. Prev Chronic Dis. 2009;6(2):A65. [PMC free article] [PubMed] [Google Scholar]
- 11.Hutchinson AD, Wilson C. Improving nutrition and physical activity in the workplace: a meta-analysis of intervention studies. Health Promot Int. 2012;27(2):238–249. [DOI] [PubMed] [Google Scholar]
- 12.Conn VS, Hafdahl AR, Mehr DR. Interventions to increase physical activity among healthy adults: meta-analysis of outcomes. Am J Public Health. 2011;101(4):751–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson LM, Quinn TA, Glanz K, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med. 2009;37(4):340–357. [DOI] [PubMed] [Google Scholar]
- 14.Maes L, Van Cauwenberghe E, Van Lippevelde W, et al. Effectiveness of workplace interventions in Europe promoting healthy eating: a systematic review. Eur J Public Health. 2012;22(5):677–683. [DOI] [PubMed] [Google Scholar]
- 15.Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta-analysis of workplace physical activity interventions. Am J Prev Med. 2009;37(4):330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuoppala J, Lamminpaa A, Husman P. Work health promotion, job well-being, and sickness absences--a systematic review and meta-analysis. J Occup Environ Med. 2008;50(11):1216–1227. [DOI] [PubMed] [Google Scholar]
- 17.Berry LL, Mirabito AM. Partnering for prevention with workplace health promotion programs. Mayo Clin Proc. 2011;86(4):335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hannon PA, Hammerback K, Garson G, Harris JR, Sopher CJ. Stakeholder perspectives on workplace health promotion: a qualitative study of midsized employers in low-wage industries. American journal of health promotion : AJHP. 2012;27(2):103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spence G Workplace wellbeing programs: If you build it they may not come...because it’s not what they really need! International Journal of Wellbeing. 2015;5(2):109–124. [Google Scholar]
- 20.Hannon P, Garson G, Harris J, Hammerback K, Sopher C, Clegg-Thorp C. Workplace health promotion implementation, readiness, and capacity among midsize employers in low-wage industries: A national survey. J Occup Environ Med. 2012;54(11):1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robroek S, van Lenthe F, van Empelen P, Burdorf A. Determinants of participation in worksite health promotion programmes: a systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2009;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoehner CM, Budd EL, Marx CM, Dodson EA, Brownson RC. Development and reliability testing of the Worksite and Energy Balance Survey. Journal of public health management and practice : JPHMP. 2013;19(3 Suppl 1):S105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang L, Hipp JA, Marx CM, Brownson RC. Occupational sitting and weight status in a diverse sample of employees in Midwest metropolitan cities, 2012-2013. Prev Chronic Dis. 2014;11:E203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frank LD, Sallis JF, Saelens BE, et al. The development of a walkability index: application to the Neighborhood Quality of Life Study. Br J Sports Med. 2010;44(13):924–933. [DOI] [PubMed] [Google Scholar]
- 25.DeJoy DM, Wilson MG, Goetzel RZ, et al. Development of the Environmental Assessment Tool (EAT) to measure organizational physical and social support for worksite obesity prevention programs. J Occup Environ Med. 2008;50(2):126–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.ReferenceUSA. 2017. http://www.referenceusa.com/Home/Home. Accessed March 08 2017.
- 27.United States Census Bureau. North American Industry Classification System. 2017; https://www.census.gov/eos/www/naics/. Accessed October 4, 2017.
- 28.IMB SPSS Statistics for Windows [computer program]. Version 23.0. Armonk, NY: 2015. [Google Scholar]
- 29.Tremblay PA, Nobrega S, Davis L, Erck E, Punnett L. Healthy workplaces? A survey of Massachusetts employers. American journal of health promotion : AJHP. 2013;27(6):390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCoy K, Stinson K, Scott K, Tenney L, Newman LS. Health promotion in small business: a systematic review of factors influencing adoption and effectiveness of worksite wellness programs. J Occup Environ Med. 2014;56(6):579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glasgow RE, McCaul KD, Fisher KJ. Participation in worksite health promotion: a critique of the literature and recommendations for future practice. Health education quarterly. 1993;20(3):391–408. [DOI] [PubMed] [Google Scholar]
- 32.Tabak RG, Hipp JA, Marx CM, Brownson RC. Workplace social and organizational environments and healthy-weight behaviors. PLoS One. 2015;10(4):e0125424. [DOI] [PMC free article] [PubMed] [Google Scholar]


