Abstract
INTRODUCTION:
Oral health is an important component of general health. The World Health Organization has highly recommended the integration of oral health promotion into general health care. In majority of the cases, patients visit their physicians with simultaneous oral and systemic complaints, and primary oral complaints are more frequently encountered. Therefore, primary care physicians can play an expanded role within oral health care to raise the overall health of the patients.
AIM:
This study aimed to assess the knowledge and awareness of family physicians regarding oral health.
MATERIALS AND METHODS:
An observational (cross-sectional) study was conducted among 250 family physicians who are practicing in Tricity. A self-structured questionnaire (close-ended) prepared by a panel of oral health experts in English language (close-ended) was administered to the study participants. The questionnaire which was divided into two parts, A and B, contained 15 questions on knowledge and awareness regarding oral health. Categorization of knowledge scores was done at three levels: low, medium, and high. Statistical analysis was performed using analysis of variance and Student's t-test.
RESULTS:
Males comprised 72.8% (182) of the study population and 55.2% (138) of the participants were doing combined practice (academic and private both). Low knowledge scores were reported in 47.2% (118) of the participants whereas only 22.4% (56) of participants had a high score. The mean knowledge score according to educational level and working profile was statistically significant (P < 0.05).
CONCLUSION:
The results of our study showed a considerable lack of knowledge among family physicians regarding connection of oral health with general health. Therefore, there is an urgent need to increase their knowledge by various continued medical education and training programs.
Keywords: Knowledge, oral health, physicians, primary health care, private practice
Introduction
One of the main public health concerns in a country like India is emergence of oral health-related problems. Oral problems not only cause pain, agony, and functional and esthetic problems but also lead to loss of working man-hours. Hence, in the long run, they are bound to have a significant impact on our economy.[1] Oral health is also an essential and leading component of individual's overall health, functional capacity, and social welfare.[2] In developing countries, there is a vast difference in oral health status between urban and rural populations, with enormous and widening disparities in access to quality care, predominantly in rural areas.[3] The physician's office is considered an opportune site to reach a large population who make a visit for their nondental problems. It has been emphasized that family physicians and other primary care providers can play an important role in improving oral health of the population.[4,5] Many physicians are less familiar with the oral diseases and their systemic origin. They may not be effectively able to correlate systemic etiology of diseases with their oral manifestations.[6] Integrating oral health disease prevention strategies into these health-care professionals’ practices would help improve access to oral health care for poor and weakened sections of the society.
Physicians who have received training in oral health are more likely to provide not only more comprehensive emergency care but also more appropriate and thorough counseling to their patients experiencing orodental problems.[7,8,9] Family physicians and other primary care providers must understand their role in oral health integration and must receive appropriate training for oral health care. Therefore, the present study was conducted to:
Assess the dental knowledge of family physicians as well as their awareness regarding various dental problems that are frequently encountered
If required, suggest possible measures to increase oral health knowledge among them.
Materials and Methods
Ethical clearance and informed consent
The present study was conducted after obtaining ethical clearance from the institutional review board of the college. Prior permission was obtained from the concerned health department, and informed consent was obtained from the participants for their willingness to participate in the study.
Study population
A descriptive cross-sectional study was carried out among family physicians who are currently practicing in Chandigarh, Panchkula, and Mohali (Tricity). The list of practicing physicians was obtained from the local Indian Medical Association bodies. A second list was also prepared selecting only those physicians involved in family practice. The feasibility of the study was checked based on the results of the pilot study which was conducted on 35 participants.
Study sample
The required sample size for the study was determined on the basis of results of the pilot study. After doing all the calculations, a sample size of 225 was obtained. A total of 250 participants were finally chosen for the study by adding 10% of nonresponders and then rounding off. Simple random sampling was done to select the study participants from our target population.
Research instrument (questionnaire)
The instrument for the study was a self-made comprehensive questionnaire written in English language. The questionnaire was prepared by a panel of oral health experts. The questionnaire was handed over personally to the study participants after visiting them and was collected the next day, so that the participants get adequate time to fill. Direct mailing of the questionnaire was not done because participants might not return the questionnaire by mail because of time constraints. The validity of the questionnaire was then analyzed and confirmed. The mean score of validity for the questionnaire (including its relevance, clarity, and simplicity) was 0.82. The final version of the questionnaire was distributed among 25 study participants for measuring its reliability. Internal consistency (reliability) of the questionnaire was assessed using Cronbach's alpha, which was obtained as 0.765 for the 15 items of the questionnaire. The questionnaire was divided into two sections – section A was “general section” containing sociodemographic details of the participants and section B comprised 15 close-ended questions on their knowledge regarding oral health [Figure 1]. We have tried to incorporate all important aspects relating to dentistry such as knowledge regarding brushing technique, relation of oral health to systemic health, oral manifestations of sexually transmitted diseases (STDs), and importance of maintaining oral health during pregnancy. Incomplete questionnaires were not included in the study. Total knowledge/awareness score was calculated according to the participants’ response. Each positive response was scored as “1” and negative as “0.” The total score (sum of all responses) awarded ranged from 1 to 15, the answers of which were graded on a 15-point Likert Scale. Categorization of scores was done at three levels: low (0–5), medium (6–10), and high (11–15).
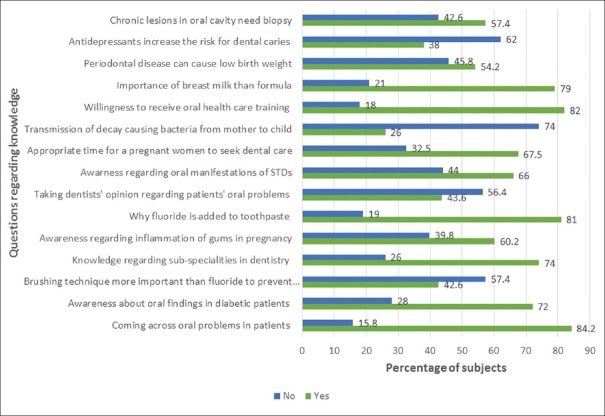
Figure 1.
Participants’ response of various questions regarding oral health
Statistical analysis
A descriptive statistical analysis was performed. The number and percentages were used to compute results on categorical measurements. The results were statistically analyzed using SPSS package version 15.0 (SPSS, Chicago, IL, USA). Analysis of variance was employed to find the significance of study parameters between three or more groups of participants, and Student's t-test was used to find significance between the two groups. The significance was set at <0.05.
Results
Sociodemographic characteristics of the study participants
Various sociodemographic details of the study participants such as gender, education level, and working profile are depicted in Table 1. A clear majority of family physicians were male (182, 72.8%) as compared to female participants (68, 27.2%). Furthermore, majority of the participants were graduates (145, 58%) and were doing private practice and academic teaching (combined) (138, 55.2%) as compared to postgraduates and private practitioners, respectively.
Table 1.
Various sociodemographic characteristics of study participants
| Characteristics | n (%) |
|---|---|
| Gender | |
| Male | 182 (72.8) |
| Female | 68 (27.2) |
| Educational status | |
| Graduate (MBBS) | 145 (58) |
| Postgraduate (MD) | 105 (42) |
| Working profile | |
| Private | 112 (44.8) |
| Combined (private and academic) | 138 (55.2) |
Participants’ response to various questions on oral health
Participants’ response to various questions regarding oral health is depicted in Figure 1. In reply to the question regarding coming across dental problems in their patients, 84.2% of participants gave a positive reply. Surprisingly, only 43.6% of participants reported that they would take dentist's opinion regarding their patients’ oral problems. Knowledge regarding correct time for pregnant women to seek dental care was reported by 67.5% of physicians; however, more than 70% of participants were unaware regarding transmission of caries causing bacteria from mother to child. Almost one-fourths (26%) of participants were unaware regarding various subspecialties in dentistry. When asked to their willingness to receive training in oral health, 82% of participants gave a positive reply.
Knowledge/awareness scores
Among the study participants, 47.2% (118) had low knowledge scores, 30.4% (76) had a medium score, and 22.4% (56) had a high score [Table 2].
Table 2.
Knowledge scores regarding oral health among study participants (according to Likert score)
| Knowledge score | Number of participants (%) |
|---|---|
| Low | 118 (47.2) |
| Medium | 76 (30.4) |
| High | 56 (22.4) |
| Total | 250 (100) |
When education level of the study participants was compared with their oral health knowledge, it was seen that 56.2% of the graduates had low knowledge scores and only 14.4% had high scores. Surprisingly, high knowledge scores were reported in less than one-third (31.4%) of the postgraduates [Figure 2]. The mean knowledge scores according to different sociodemographic characteristics are summarized in Table 3. The mean knowledge score according to educational level and the type of practice were statistically significant (P < 0.05), whereas there was no significant difference in case of gender (P > 0.05).
Figure 2.
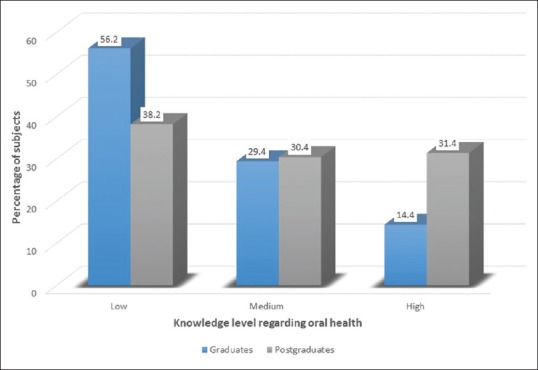
Knowledge level regarding oral health among graduates and postgraduates
Table 3.
Participants’ mean oral health literacy score according to different sociodemographic variables
| Sociodemographic variable | Knowledge score | P | |
|---|---|---|---|
| Mean | SD | ||
| Gender | |||
| Male | 4.36 | 1.54 | F=1.254 |
| Female | 3.82 | 2.64 | P=0.082 |
| Total | 4.09 | 3.01 | |
| Education level | |||
| Graduate (BDS) | 5.01 | 2.65 | F=1.465 |
| Postgraduate (MDS) | 5.34 | 1.76 | P=0.018 |
| Total | 5.17 | 2.76 | |
| Working profile | |||
| Private | 4.15 | 2.32 | F=2.014 |
| Combined | 5.23 | 2.87 | P=0.027 |
| Total | 4.69 | 2.53 | |
P<0.05 (statistically significant), tests used student t-test, ANOVA. ANOVA=Analysis of variance, SD=Standard deviation
Discussion
Primary care providers, especially family physicians, could have a profound impact on the oral health of their patients by integrating oral health in their practices which can effectively address their oral health needs. The present study was conducted to assess the knowledge and awareness of family physicians regarding oral health and to find out areas in which they need to improve their knowledge. The authors have tried to gather vital information regarding oral health from the participants. For this reason, the questionnaire used in the present study was framed after consulting experts and specialists in oral care. Our study showed a considerable lack of knowledge among family physicians regarding oral health.
It has been documented in various studies that periodontal disease can lead to adverse pregnancy outcomes.[10,11] Therefore, physicians are expected to have a sound knowledge on the impact of oral health on pregnancy. However, in our study, only 54.2% of participants were aware of this fact. Similar findings were observed in some other studies conducted elsewhere on physicians and health-care providers.[12,13]
It is a common belief among some physicians that all the dental problems can be solved by a general dentist and are unaware about the existence of different subspecialties in the dentistry. This is evident from the results of the study where one-fourths of the participants were unaware regarding different specialties in dentistry. The results correlate with the findings of some other studies conducted on family physicians.[14] Moreover, more than 50% of participants were unwilling to seek dentist's opinion regarding their patients’ oral problems.
Early lesions of many STDs appear in the oral cavity that can be caused by fungal, bacterial, or viral infections.[15] The results of our study indicate that only 66% of participants were knowledgeable regarding oral manifestations of STDs in comparison to some other studies, in which more than 80% of participants looked into oral cavity when they encounter any patient with STD.[16] The results of another study conducted in Chennai among primary care physicians revealed that 86% of participants routinely examined the oral cavity of their patients.[17] It is necessary for a physician to know about oral health and to examine all patients’ oral cavity during their routine practice.
Training is critical to preparing physicians to take on new and expanded roles in oral health care.[18] Training provides an excellent basis for deepening their understanding of dental health and prevention. In the present study, 82% of the participants were willing to undergo training in oral health as compared to the findings of another study, in which willingness was shown by 92% of participants.[9] According to literature, some of the health centers in the US provided oral health content during training sessions for its primary care providers and physicians to embrace oral health care as an integral part of primary care.[5]
In the present study, 47.2% of the participants had low knowledge scores with more than 50% of participants possessing a graduate degree, and the findings were statistically significant (P = 0.018). These findings are in accordance with the results of some other studies conducted in southern part of India. This might be due to the reason that with increase in knowledge, awareness also increases. Moreover, participants doing combined practice had more knowledge as compared to those doing private practice (P = 0.027). This could be due to the reason that participants engaged in academic teaching are exposed to more learning experiences as compared to those doing only private practice.
There are some limitations in our study which are worth to mention. Surveys conducted with a self-administered questionnaire might also produce nonresponses, misconceptions, and errors;[19] these should be small in our survey since the participants were highly educated health professionals. Furthermore, the present study was conducted in a particular geographic region with a limited sample size; therefore, it is difficult to generalize the results for the entire country. Similar studies should be conducted in other parts of the country involving a larger sample.
Conclusion and Recommendations
Family practitioners and primary care providers must have the requisite knowledge regarding oral health and the ability to assume the necessary roles within models that integrate oral care and primary care. It is reflected from the results of the study that importance of oral health in relation to general health has been overlooked. Primary knowledge on dental health issues was relatively low among participants, so priming their information on diseases and supporting new practices might produce a significant effect. Based on the results of the study, some recommendations are put forth:
Continuing medical education programs should also include topics on oral health care as these can be effective in producing both short-term and long-term knowledge gains
A compulsory subject emphasizing on the influence of oral health on general health should be introduced in the undergraduate medical curriculum
Increasing awareness in the medical community about various roles primary care physicians can play for improvement of oral health of the population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the concerned health authorities for supporting us and giving the permission to conduct the study. Also, we also would like to thank our participants (family physicians) for taking out time from their busy schedule to participate in the study.
References
- 1.Nanda Kishore KM. Public health implications of oral health – Inequity in India. J Adv Dent Res. 2010;1:1–10. [Google Scholar]
- 2.Edelstein BL. Dental care considerations for young children. Spec Care Dentist. 2002;22:11S–25S. [PubMed] [Google Scholar]
- 3.Sivapathasundharam B. Dental education in India. Indian J Dent Res. 2007;18:93. [Google Scholar]
- 4.Kumari NR, Sheela S, Sarada PN. Knowledge and attitude on infant oral health among graduating medical students in Kerala. J Indian Soc Pedod Prev Dent. 2006;24:173–6. doi: 10.4103/0970-4388.28072. [DOI] [PubMed] [Google Scholar]
- 5.Maxey HL, Norwood CW, Weaver DL. Primary care physician roles in health centers with oral health care units. J Am Board Fam Med. 2017;30:491–504. doi: 10.3122/jabfm.2017.04.170106. [DOI] [PubMed] [Google Scholar]
- 6.McCarthy PL, Shklar G. 2nd ed. Philadelphia: Febiger; 1980. Diseases of the Oral Mucosa. [Google Scholar]
- 7.Mouradian WE, Schaad DC, Kim S, Leggott PJ, Domoto PS, Maier R, et al. Addressing disparities in children's oral health: A dental-medical partnership to train family practice residents. J Dent Educ. 2003;67:886–95. [PubMed] [Google Scholar]
- 8.Cohen LA. Expanding the physician's role in addressing the oral health of adults. Am J Public Health. 2013;103:408–12. doi: 10.2105/AJPH.2012.300990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nammalwar RB, Rangeeth P. Knowledge and attitude of pediatricians and family physicians in Chennai on pediatric dentistry: A survey. Dent Res J (Isfahan) 2012;9:561–6. doi: 10.4103/1735-3327.104874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tettamanti L, Lauritano D, Nardone M, Gargari M, Silvestre-Rangil J, Gavoglio P, et al. Pregnancy and periodontal disease: Does exist a two-way relationship? Oral Implantol (Rome) 2017;10:112–8. doi: 10.11138/orl/2017.10.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shenoy RP, Nayak DG, Sequeira PS. Periodontal disease as a risk factor in pre-term low birth weight – An assessment of gynecologists’ knowledge: A pilot study. Indian J Dent Res. 2009;20:13–6. doi: 10.4103/0970-9290.49049. [DOI] [PubMed] [Google Scholar]
- 12.Rabiei S, Mohebbi SZ, Patja K, Virtanen JI. Physicians’ knowledge of and adherence to improving oral health. BMC Public Health. 2012;12:855. doi: 10.1186/1471-2458-12-855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Habashneh R, Aljundi SH, Alwaeli HA. Survey of medical doctors’ attitudes and knowledge of the association between oral health and pregnancy outcomes. Int J Dent Hyg. 2008;6:214–20. doi: 10.1111/j.1601-5037.2008.00320.x. [DOI] [PubMed] [Google Scholar]
- 14.Prakash P, Lawrence HP, Harvey BJ, McIsaac WJ, Limeback H, Leake JL, et al. Early childhood caries and infant oral health: Paediatricians’ and family physicians’ knowledge, practices and training. Paediatr Child Health. 2006;11:151–7. doi: 10.1093/pch/11.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mastrolorenzo A, Giomi B, Tiradritti L, Zuccati G. Oral manifestations of sexually transmitted infections. G Ital Dermatol Venereol. 2012;147:373–88. [PubMed] [Google Scholar]
- 16.Chitta H, Chaitanya N, Lavanya R, Reddy MP, Mohammed I, Subramanyam K. Awareness of medical doctors on oral health: A cross sectional study. Oral Health Dent Manage. 2015;14:424–8. [Google Scholar]
- 17.Sarumathi T, Saravanakumar B, Datta M, Nagarathnam T. Awareness and knowledge of common oral diseases among primary care physicians. J Clin Diagn Res. 2013;7:768–71. doi: 10.7860/JCDR/2013/5419.2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edwards PC, Kanjirath P. Recognition and management of common acute conditions of the oral cavity resulting from tooth decay, periodontal disease, and trauma: An update for the family physician. J Am Board Fam Med. 2010;23:285–94. doi: 10.3122/jabfm.2010.03.090023. [DOI] [PubMed] [Google Scholar]
- 19.Sjöström O, Holst D, Lind SO. Validity of a questionnaire survey: The role of non-response and incorrect answers. Acta Odontol Scand. 1999;57:242–6. doi: 10.1080/000163599428643. [DOI] [PubMed] [Google Scholar]