Abstract
INTRODUCTION:
The inappropriate use of drugs is a global health problem, especially in developing country like India. Irrational prescriptions have an ill effect on health as well as health-care expenditure. Prescription auditing is an important tool to improve the quality of prescriptions, which in turn improves the quality of health care provided. The present study was conducted to investigate the rational use of drugs for completeness, legibility, and against the World Health Organization (WHO)-recommended core drug use indicators.
MATERIALS AND METHODS:
A cross-sectional, outpatient department-based study was carried out in a rural hospital of Delhi wherein 120 prescriptions were randomly sampled, irrespective of patient characteristics and diagnosis over a period of 1 month. All the prescriptions were analyzed for general details, medical components, and WHO core drug use indicators. The data obtained were summed up and presented as descriptive statistics using the Microsoft Excel and were analyzed using SPSS version 16.
RESULTS:
All the prescriptions had general details mentioned in it. The diagnosis was mentioned in 64.2% of prescriptions, and 85.8% of drugs were prescribed by generic name. An average of 3.02 drugs per encounter was prescribed. The average consultation time and dispensing time were 2.8 min and 1.2 min, respectively. Only half of the patients had correct knowledge of dose.
CONCLUSIONS:
Our study highlights the need to train our prescribing doctors on writing rational prescriptions for quality improvement.
Keywords: Core indicators, prescription audit, quality, rational prescription, World Health Organization
Introduction
Prescription is a written medicolegal document by an authorized person for the treatment of the patient and is a reflection of the quality of health-care service being delivered to the patient. It is a skill acquired through training. Prescribing errors promote the irrational use of drugs and decrease the patient compliance.[1] Irrational prescriptions unnecessarily increase the cost and duration of the treatment. Such practices also lead to the emergence of drug interactions, drug resistance, and adverse drug reactions. It ultimately increases the mortality, morbidity, and financial burden on the patient.[2]
The World Health Organization (WHO) stated the rational use of drugs requires that patients receive medication appropriate to their clinical needs, in doses that meet their own individual requirement for an adequate period of time and at the lowest cost to them and their community.[3] The WHO has reported that around 50% of all medicines are inappropriately prescribed, dispensed, or sold.[4] Inappropriate use of medicines is deemed to be more of a problem in the Global South. This is seen to have potential implications on health-care budgets as almost 25%–70% of worldwide health-care expenditure is spent on medicines.[5]
To investigate the rational use of drugs, the WHO in collaboration with the International Network for Rational Use of Drugs developed a set of “core drug use indicators.” The indicators measure performance in three related areas of prescribing practices, patient care, and facility-specific factors. The core drug use indicators have come to be recognized as objective measures that can describe the drug use situation in a country, region, or individual health facility. Prescribing indicators include the number of drugs prescribing per encounter, the percentage of drugs prescribed by generic name, the percentage of encounter by injection and antibiotics prescription, and the percentage of drugs prescribed from essential drug list (EDL).[6]
Prescription audit is a part of the holistic clinical audit and is a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change.[7] Prescription auditing is also an educational activity, and if regularly done, can aid in improving the prescription quality and thus can enable the patient to receive high standard and best-quality care.[8]
This study was conducted to audit the quality of outpatient department (OPD) prescriptions at a rural government hospital of Delhi to investigate the rational use of drugs for completeness, legibility, and against the WHO-recommended core drug use indicators.
Materials and Methods
A cross-sectional, OPD-based study was carried out in a rural hospital of Delhi after taking ethical clearance from the institutional ethics committee. Complete confidentiality of patients was maintained throughout the research after taking informed written consent. The study was carried out over a period of 1 month in August 2016. A total of 120 outpatient prescriptions were randomly sampled, irrespective of patient characteristics, diagnosis, and department.
All the prescriptions were analyzed on the following parameters:
Prescription format and its completeness with regard to:
General details (name, age, sex, OPD registration number, date of consultation, and legible handwriting)
Medical components (history, examination, presumptive/definite diagnosis, investigations, correct dose and dosage, duration of treatment, follow-up advice, referral details, do's and don’ts, legible signature, and medical council registration number).
The WHO core drug use indicators[6] which include three groups:
-
Prescribing indicators
- Average number of drugs per prescription
- Percentage of drugs prescribed by generic name
- Percentage of prescriptions containing antimicrobial agents (antibiotics)
- Percentage of injections per prescription
- Percentage of drugs prescribed from the EDL.
-
Patient-care indicators
- Average consultation time
- Average dispensing time
- Percentage of drugs actually dispensed
- Percentage of drugs adequately labeled
- Patients’ knowledge of correct dosage.
-
Health facility indicators.
- Availability of copy of EDL in all OPDs
- Availability of key drugs.
The WHO core drug use indicators include five questions each on prescribing and patient care indicators and two questions related to health facility. The patient care indicators included average consultation and dispensing time, which excludes the waiting time. Availability of a copy of EDL in all OPDs and in-stock availability of 18 key drugs identified by hospital authorities was checked for health facility indicator.
The data obtained were summed up and presented as descriptive statistics using the Microsoft Excel. The data were analyzed using SPSS version 16 (SPSS for Windows, Version 16.0. Chicago, SPSS Inc.).
Results
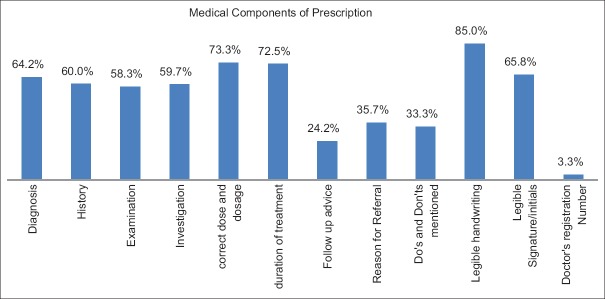
Among the 120 prescriptions analyzed, all (100%) of them had the general details, i.e. name, age, sex, and OPD registration number. Date of consultation was mentioned in 98.3% of prescriptions and 95.8% had legible handwriting. In the medical component, diagnosis was mentioned in 64.2% of prescriptions. Out of 72 prescriptions which required investigations, 59.7% had been advised investigations, and out of 14 prescriptions which required referral, only 35.7% had mentioned reason for referral. Legible signature was found in 65.8% of prescriptions, but doctor's registration number was mentioned in hardly few of them [Figure 1].
Figure 1.
Bar graph showing completeness of prescriptions
The average waiting time was found to be 17.6 min. An average of 3.02 drugs per encounter was prescribed. A total of 85.8% of drugs were prescribed by generic name and 88.3% of drugs were prescribed from EDL of the hospital. The patients spent an average of 2.8 min with doctors in the consultation room and an average of 1.2 min in receiving their drugs. Only 51.7% of patients were able to repeat the correct dosage schedule of the drugs they had received. Out of eight OPDs checked, 87.5% had a copy of the EDL. In the hospital, 93.3% of the 18 key essential drugs were actually in stock [Table 1].
Table 1.
The World Health Organization core drug use indicators
| Core Drug use Indicators | Frequency/percentage |
|---|---|
| Prescribing indicators | |
| Average number of drugs per encounter | 3.02±0.81 |
| Percentage of drugs prescribed by generic name | 85.8 |
| Percentage of encounters with an antibiotic prescribed | 52.5 |
| Percentage of encounters with an injection prescribed | 10.8 |
| Percentage of drugs prescribed from essential drugs list of hospital | 88.3 |
| Patient care indicators | |
| Average consultation time | 2.8 min |
| Average dispensing time | 1.2 min |
| Percentage of drugs actually dispensed | 86.7 |
| Percentage of drugs adequately labeled | 73.3 |
| Patients’ knowledge of correct dosage | 51.7 |
| Health facility indicators | |
| Availability of copy of essential drugs list in all OPDs | 87.5 |
| Availability of key drugs | 93.3 |
OPDs – Outpatient departments
Discussion
Prescription is an important intervention by the physician, and it is the ethical and legal duty of the practitioner to write complete and legible prescriptions. In our study, we found that the date of prescription and patient's details (name, age, sex, and address) were complete in all the prescriptions. This was because these details were printed at the time of registration itself. Studies auditing handwritten prescriptions have found that patient details were usually incomplete in almost all prescriptions.[9] It is important to mention the correct patient details for medicolegal purpose and also to ensure patient receives correct treatment for his/her diagnosis.
On analyzing the prescriptions, it was found that the prescriptions were incomplete with regard to history, examination, diagnosis, and investigations. The reasons could be heavy OPD load, nonspecific complaints, or verbal communication by doctors, rather than writing in detail.
The prescriptions were incomplete with regard to follow-up advice, reasons for referrals, dos and don’ts, drug formulation, and direction of administration. Dosing errors and omitting the duration of treatment were also common prescribing errors in 26.7% and 27.5%, respectively. Most drugs are available in variable strengths and dosage forms and thus it poses problems for dispensing. It can also lead to issues such as treatment failure, antibiotic resistance, and adverse drug reaction which are associated with underdosing or overdosing. Wrong dose, dose omission, and wrong duration were the most common types of prescribing errors found in many studies worldwide.[10,11,12]
The doctors are infamous for their illegible handwriting, and this can cause medication errors, dispensing of wrong drugs, and can lead to adverse drug reactions. We found that 15% of prescribing doctors had illegible handwriting. In our study, the prescribing doctor's signature or initials were legible in 65.8% of the prescriptions and doctor's registration number was mentioned in only 3.3% of prescriptions. These details are important to identify the prescribing doctor and validate the authenticity of prescriptions. To avoid such errors, the use of capital letters while prescribing drugs should be encouraged and if possible switching to electronic prescribing system.
To investigate the drug use in health facilities, the WHO has recommended core prescribing indicators. These indicators aim to measure the performance of health-care providers in several important areas pertaining to appropriate or rational use of drugs. These indicators have been developed by the WHO after observing prescribing practices at outpatient facilities for the treatment of acute and chronic illnesses.[6] The average number of drugs per consultation in our study was 3.02 ± 0.81 drugs which was similar to drug use pattern in secondary level hospitals (3.1).[13] The purpose of this indicator is to measure polypharmacy, and the WHO recommends 2 drugs per encounter. Polypharmacy increases the cost of health care for patient as well as government and it can also result in adverse drug reaction due to drug–drug interaction. In our study, majority of the drugs were prescribed by generic names and were prescribed from the EDL available in the hospital. This could be due to repeated circulars from the hospital authorities and government to prescribe generic drugs and refrain from prescribing medicines, which are not mentioned in the current EDL. Furthermore, the hospital has been carrying out regular monitoring and reporting and surprise checks to ensure compliance. More than 50% of prescriptions had an antibiotic prescribed which was almost double of what the WHO recommends (20%–25.4%). The high prevalence of antibiotic prescriptions implies inappropriate use of antibiotics in our study setting. Overprescription of antibiotics by health workers and overuse of antibiotics by public are leading to a dangerous rise in antibiotic resistance and are threatening our ability to treat common infectious diseases. There should be a robust national action plan in place and regulation for appropriate use of antibiotics. To raise awareness among professionals, antimicrobial resistance should be made a part of their curriculum, and regular trainings and certifications like that used for biomedical waste should be carried out. General public should also be made aware to use antibiotics only when prescribed by certified doctors and not use over-the-counter prescriptions or use leftover antibiotics.
The average consulting time in our study was 2.8 min. This is the time between entering and leaving the consultation room and does not include waiting time. Such a short consulting time, during which the physician must make a complete evaluation of the patient, prescribe an appropriate drug, and have interaction, is insufficient.[6] This consultation time was as told by the patients and may be biased as the patients think that the doctors are not giving them enough of their time.
The average drug dispensing time, which is the average time that personnel dispensing drugs spend with patients, was 1.2 min. This is the time between arriving at the dispensary counter and leaving and does not include waiting time and this time needs to be more for pharmacists to explain the dosages, necessary precautions, and adverse reactions associated with any particular drug therapy. The availability of EDL enhances rational prescribing and quality of care, and it was encouraging to see that most of the OPDs in the hospital had a copy available at the time of the study.
The prescription audit should be carried out at regular intervals for rationalizing drug prescriptions and continuous quality improvement of any hospital.
Conclusions
Our study highlights the need to train our prescribing doctors to write rational prescriptions and adhere to the WHO standards for prescriptions for the quality improvement of hospitals.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are thankful to the medical superintendent of the hospital for his help. The authors are also thankful to all the participants for being a part of this study.
References
- 1.Fijn R, Van den Bemt PM, Chow M, De Blaey CJ, De Jong-Van den Berg LT, Brouwers JR, et al. Hospital prescribing errors: Epidemiological assessment of predictors. Br J Clin Pharmacol. 2002;53:326–31. doi: 10.1046/j.0306-5251.2001.bjcp1558.doc.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Introduction to Drug Utilization Research. OSLO: World Health Organization; 2003. [Google Scholar]
- 3.World Health Organization (WHO) The World Medicine Situation. Geneva: World Health Organization Press. World Health Organization; 2004. [Google Scholar]
- 4.World Health Organization. The World Medicines Situation. World Health Organization. [Last accessed on 2015 Jun 06]. Available from: http://www. apps.who.int/medicinedocs/en/d/Js6160e/
- 5.World Health Organization. Measuring Medicine Prices, Availability, Affordability and Price Components. 2008. [Last accessed on 2015 Mar 21]. Available from: http://www.who.int/medicines/areas/access/OMS_Medicine_prices.pdf .
- 6.World Health Organization. How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators – EDM Research Series No 007. 1993. [Last accessed on 2015 May 05]. Available from: http://www.apps.who.int/ medicinedocs/en/d/Js2289e/
- 7.National Institute for Clinical Excellence (NICE): Principles for Best Practice in Clinical Audit. Oxford: Radcliffe Publishing; 2002. [Google Scholar]
- 8.Ahsan M, Shaifali I, Mallick AK, Singh HK, Verma S, Shekhar A. Prescription auditing based on World Health Organization prescribing indicators in a teaching hospital in North India. Int J Med Res Rev. 2016;4:1847–52. [Google Scholar]
- 9.Shelat PR, Kumbar SK. Analysis of out door patients’ prescriptions according to world health organization (WHO) prescribing indicators among private hospitals in Western India. J Clin Diagn Res. 2015;9:FC01–4. doi: 10.7860/JCDR/2015/12724.5632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abidi A, Gupta S, Kansal S. Prescription auditing and drug utilization pattern in a tertiary care teaching hospital of western UP. Int J Basic Clin Pharmacol. 2012;1:184–90. [Google Scholar]
- 11.Seden K, Kirkham JJ, Kennedy T, Lloyd M, James S, McManus A, et al. Cross-sectional study of prescribing errors in patients admitted to nine hospitals across North West England. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-002036. pii: e002036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kiekkas P, Karga M, Lemonidou C, Aretha D, Karanikolas M. Medication errors in critically ill adults: A review of direct observation evidence. Am J Crit Care. 2011;20:36–44. doi: 10.4037/ajcc2011331. [DOI] [PubMed] [Google Scholar]
- 13.Potharaju HR, Kabra SG. Prescription audit of outpatient attendees of secondary level government hospitals in Maharashtra. Indian J Pharmacol. 2011;43:150–6. doi: 10.4103/0253-7613.77350. [DOI] [PMC free article] [PubMed] [Google Scholar]