Abstract
An 86-year-old Asian man with asteroid hyalosis presented with decreased vision in the left eye. He underwent phacoemulsification and implantation of silicone intraocular lens (IOL) in the left eye 18 years ago, and also received neodymium:yttrium–aluminum–garnet (Nd:YAG) laser 3 years ago. At presentation, his corrected visual acuity (CVA) was 20/1000 in the left eye. Slit-lamp examination showed white-gray membranous deposits on the posterior IOL surface. The deposits were removed using Nd:YAG laser treatment. One week later, his CVA improved to 20/30, and opacity of the posterior IOL surface was removed. Six months later, his CVA was 20/30, and visual axis was clear. This case suggests that Nd:YAG laser treatment can be a viable option in some patients with posterior surface opacification of silicone IOL associated with asteroid hyalosis, especially in those who are a poor candidate for IOL exchange due to old age or compromised general condition.
Keywords: Asteroid hyalosis, calcification, neodymium:yttrium–aluminum–garnet laser, opacification, silicone intraocular lens
Introduction
Posterior surface opacification of silicone intraocular lens (IOL) associated with asteroid hyalosis, which was first reported in 2004,[1,2] is a rare but well-described late complication after cataract surgery.[1,2,3,4] The opacification is characterized by progressive accumulation of white granular or fleck-like deposits that is localized to the posterior optic surface of the silicone IOL.[5] Although removal the calcification deposits using neodymium:yttrium–aluminum–garnet (Nd:YAG) laser is simple and safe, attempts to use Nd:YAG laser treatment have often been associated with unsatisfactory results or immediate re-accumulation of the deposits on the posterior surface of the IOL[1,2,6] IOL exchange have been considered the definitive treatment for the silicone IOL opacification.[1,4,6,7] However, the method is technically difficult and associated with increased risk of complications.[5]
Herein, we report our recent experience with a case of posterior surface opacification of silicone IOL associated with asteroid hyalosis that was successfully treated with Nd:YAG laser.
Case Report
An 86-year-old Asian man with asteroid hyalosis presented with decreased vision in the left eye. His medical history was unremarkable except depression. He underwent uneventful phacoemulsification and implantation of silicone IOL in the left eye 18 years ago. In addition, he received Nd:YAG laser posterior capsulotomy 3 years ago. One week after the posterior capsulotomy, the corrected visual acuity (CVA) was 20/30 in the left eye. Since then, he was lost to follow-up for 3 years.
At presentation, his CVA was 20/1000 and intraocular pressure (IOP) measured with Goldmann applanation tonometry was 12 mmHg in his left eye. Slit-lamp examination showed white-gray membranous deposits and Nd:YAG pits occluding the posterior capsular opening on the posterior surface of IOL [Figure 1]. A Nd:YAG laser was used to remove the deposits and clear the visual axis. The membranous deposits were removed with a total of 80 mJ (50 shots × 1.6 mJ) Nd:YAG laser. Topical prednisolone acetate 1.0% 4 times daily for 1 month was prescribed to prevent intraocular inflammation.
Figure 1.
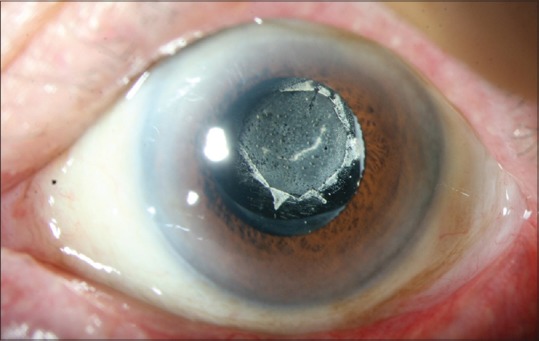
Anterior segment examination of the left eye showed white-gray membranous deposit on the posterior surface of the silicone intraocular lens occluding the posterior capsular opening
At 1 week, his CVA improved to 20/30 and IOP was 13 mmHg in the left eye. Anterior segment examination showed the successful removal of the membranous opacity, although mild opacification and Nd:YAG pits on the posterior IOL surface were observed [Figure 2a and b]. Anterior segment optical coherence tomography (Carl Zeiss Meditec, Oberkochen, Germany) confirmed the same findings [Figure 2c].
Figure 2.
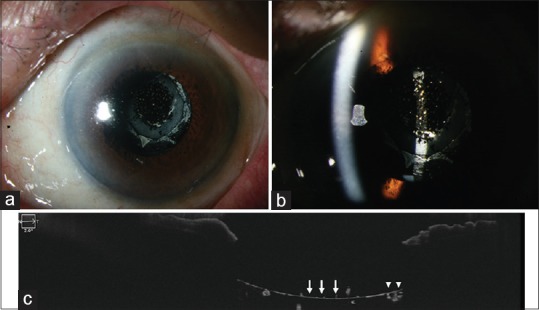
One week after the neodymium:yttrium–aluminum–garnet laser treatment, anterior segment examination of the left eye demonstrated successful removal of the deposit and clear visual axis (a), although mild opacification and neodymium:yttrium–aluminum–garnet laser pit remained (b). An anterior segment optical coherence tomography image confirmed removal of the deposit (white arrow) surrounded by thick membranous opacification (white arrowhead) (c)
Six months later, his CVA was 20/30 in the left eye, and slit lamp examination showed a clear visual axis.
Discussion
In this report, we introduce a case of posterior surface opacification of silicone IOL associated with asteroid hyalosis that was successfully treated using Nd:YAG laser.
Previous studies showed that it took an average of 8 years for the calcium deposits to accumulate on the posterior surface of the silicone IOL and cause a significant visual disturbance.[4,7] Werner et al.[4] revealed that in the case of bilateral asteroid hyalosis, the posterior surface opacification was found only in the eye with a silicone IOL implantation, whereas no opacification was found in the eye with hydrophobic acrylic lens implantation. These findings suggest that opacification might be associated with an interaction between the silicone IOL and asteroid hyalosis.[4]
Asteroid hyalosis is characterized by bright asteroid bodies floating in the vitreous body.[6] Its prevalence is approximately 1% and increases with aging.[8] Analysis of the asteroid bodies demonstrated that calcium and phosphorus were its main components.[6,9] The deposits on posterior IOL surface might be directly derived from the asteroid bodies, or produced by a similar process that leads to asteroid hyalosis,[6] as it is also composed of calcium phosphate hydroxyapatite.[1,3,6,7,9] Opacification is often accelerated after Nd:YAG laser posterior capsulotomy, because disruption of the posterior capsule results in direct contact between the vitreous and IOL, promoting the accumulation of the calcium deposits on the posterior IOL surface.[4] These findings suggest that implantation of silicone IOL in patients with asteroid hyalosis should be discouraged, and special attention should be paid when considering Nd:YAG laser posterior capsulotomy in these patients.[7] In the present case, although the typical granular or fleck-like calcium deposit was not clearly demonstrated, accumulation of the deposits on the previous Nd:YAG laser posterior capsulotomy opening suggests that the calcification was associated with asteroid hyalosis in the vitreous cavity. The previous Nd:YAG laser posterior capsulotomy led to break of the barrier between the IOL and vitreous cavity, which might accelerated the accumulation of the calcium deposit.[4]
Although this phenomenon appears to occur in association with silicone IOL, it is unclear why only a few cases develop IOL opacification despite the large number of silicone IOLs that have been implanted in patients with asteroid hyalosis.[6] We believe further studies are needed to elucidate the mechanism of the pathologic process.
In hydrophilic acrylic IOLs, calcium deposits cannot be mechanically removed because they are incorporated into the subsurface of the optic;[6,10,11,12] thus, IOL exchange is the only treatment option.[6,12,13] By contrast, in silico ne IOL, calcium deposits accumulate only on the posterior IOL surface and are amenable to direct mechanical removal, such as Nd:YAG laser treatment.[1,2,3,4] However, the displacement of calcium deposits from the IOL optic using Nd:YAG is often associated with unsatisfactory visual outcome or re-accumulation of the deposits.[1,2] Moreover, Nd:YAG laser treatment results in disruption of posterior capsule, which makes IOL exchange more difficult and increases the risk of complications.[5,14] Therefore, IOL exchange has been considered the only successful therapeutic option for silicone IOL opacification associated with asteroid hyalosis.[1,4,6,7,11,14]
However, the procedure of IOL explantation and exchange is technically difficult and associated with complications including corneal endothelial cell loss, aggravation of refractive error, zonular dehiscence, IOL tilting, and decentration.[15,16,17] The complication rate increases in the presence of an Nd:YAG capsulotomy opening.[5,14] Moreover, an anterior vitrectomy, which is often required for IOL exchange, also increases the risk of retinal tear or detachment.[3,17] IOL exchange also has a limitation that the new IOL must be implanted in the ciliary sulcus in most cases.[17]
Therefore, more simple methods for removal of the calcium deposits have been developed.[3,18] Moussa et al.[18] introduced a technique of manual removal of calcium deposits from the posterior surface of silicone IOL using a nickel-titanium loop, suggesting that mechanical displacement of calcium deposits might be a viable option. Platt et al.[3] recently demonstrated a surgical technique that uses pars plana vitrectomy (PPV) a lighted pick and a modified silicone-tipped cannula to remove calcium deposits from posterior IOL surface in a patient with asteroid hyalosis. Calcium deposits were removed, and clear IOL optic was maintained throughout the 6-month follow-up. CVA improved to 20/20. This case suggests that mechanical clearing of posterior IOL surface accompanied with PPV might avoid the need for IOL exchange.[3] In an effort to prevent IOL exchange, Ullman et al.[7] also attempted PPV to eliminate the source of the abnormal calcification and halt the progression of IOL opacification,[7] in which IOL opacification was stabilized, and good vision was maintained throughout the 16-month follow-up.[7] These results suggest that mechanical removal of the calcium deposit can be useful for visual recovery, and PPV might prevent the recurrence of the dystrophic calcification.[3,7,18] In our case, we attempted to mechanically remove the calcium deposits using Nd:YAG laser because the patient was a poor candidate for surgical options, including IOL exchange, due to old age. In addition, he previously received Nd:YAG posterior capsulotomy, which made the IOL exchange more difficult. We discussed the risk of the IOL exchange with the patient, and chose to perform the Nd:YAG laser treatment first as it was relatively simple and safe, and would not further increase the risk of IOL exchange as the posterior capsule was already disrupted due to the previous laser posterior capsulotomy. Calcium deposits were almost entirely removed, and his CVA was improved to 20/30 from 20/1000. Although we informed the patient that the results could be unsatisfactory, he was fortunate that the clear visual axis and improved vision was maintained throughout the 6-month follow-up. Although the mechanism underlying the good visual results is unclear, we believe that delayed accumulation of calcium deposits due to slow metabolism in old age might, at least in part, play a role.
However, we acknowledge that further follow-up is necessary as the possibility of re-accumulation of calcium deposits cannot be ignored. If the dystrophic calcification recurs, we believe the repetition of the Nd:YAG laser treatment can be helpful, especially given the old age of the patient. Otherwise, simple PPV can be considered to prevent re-accumulation of calcium deposit after mechanical clearing of the posterior IOL to avoid the need for an IOL exchange.[3,7]
This report suggests that Nd:YAG laser can sometimes be useful for the treatment of dystrophic calcification on the posterior surface of silicone IOL surface, particularly in patients with to old age or compromised general condition. If a patient previously received Nd:YAG posterior capsulotomy, Nd:YAG laser treatment can be attempted first as it does not further increase the risk of IOL exchange. Nd:YAG laser treatment can also be considered in patients with a history of PPV, as there is reduced risk of recurrence of the dystrophic calcification.[3,7] Even if the calcification recurs, IOL exchange can still be considered in these patients.
In conclusion, we introduce a case of opacification of the posterior surface of silicone IOL associated with asteroid hyalosis. Removal of the calcium deposits from IOL surface using Nd:YAG laser might be a viable option in some patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by 2018 Research Grant from Kangwon National University.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Foot L, Werner L, Gills JP, Shoemaker DW, Phillips PS, Mamalis N, et al. Surface calcification of silicone plate intraocular lenses in patients with asteroid hyalosis. Am J Ophthalmol. 2004;137:979–87. doi: 10.1016/j.ajo.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 2.Wackernagel W, Ettinger K, Weitgasser U, Bakir BG, Schmut O, Goessler W, et al. Opacification of a silicone intraocular lens caused by calcium deposits on the optic. J Cataract Refract Surg. 2004;30:517–20. doi: 10.1016/S0886-3350(03)00672-2. [DOI] [PubMed] [Google Scholar]
- 3.Platt SM, Iezzi R, Mahr MA, Erie JC. Surgical removal of dystrophic calcification on a silicone intraocular lens in association with asteroid hyalosis. J Cataract Refract Surg. 2017;43:1608–10. doi: 10.1016/j.jcrs.2017.09.026. [DOI] [PubMed] [Google Scholar]
- 4.Werner L, Kollarits CR, Mamalis N, Olson RJ. Surface calcification of a 3-piece silicone intraocular lens in a patient with asteroid hyalosis: A clinicopathologic case report. Ophthalmology. 2005;112:447–52. doi: 10.1016/j.ophtha.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 5.Stringham J, Werner L, Monson B, Theodosis R, Mamalis N. Calcification of different designs of silicone intraocular lenses in eyes with asteroid hyalosis. Ophthalmology. 2010;117:1486–92. doi: 10.1016/j.ophtha.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 6.Espandar L, Mukherjee N, Werner L, Mamalis N, Kim T. Diagnosis and management of opacified silicone intraocular lenses in patients with asteroid hyalosis. J Cataract Refract Surg. 2015;41:222–5. doi: 10.1016/j.jcrs.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Ullman DI, Gupta S. Pars plana vitrectomy for dystrophic calcification of a silicone intraocular lens in association with asteroid hyalosis. J Cataract Refract Surg. 2014;40:1228–31. doi: 10.1016/j.jcrs.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell P, Wang MY, Wang JJ. Asteroid hyalosis in an older population: The blue mountains eye study. Ophthalmic Epidemiol. 2003;10:331–5. doi: 10.1076/opep.10.5.331.17324. [DOI] [PubMed] [Google Scholar]
- 9.Matsumura K, Takano M, Shimizu K, Nemoto N. Silicone intraocular lens surface calcification in a patient with asteroid hyalosis. Jpn J Ophthalmol. 2012;56:319–23. doi: 10.1007/s10384-012-0124-9. [DOI] [PubMed] [Google Scholar]
- 10.Werner L, Apple DJ, Escobar-Gomez M, Ohrström A, Crayford BB, Bianchi R, et al. Postoperative deposition of calcium on the surfaces of a hydrogel intraocular lens. Ophthalmology. 2000;107:2179–85. doi: 10.1016/s0161-6420(00)00416-4. [DOI] [PubMed] [Google Scholar]
- 11.Jones JJ, Jones YJ, Jin GJ. Indications and outcomes of intraocular lens exchange during a recent 5-year period. Am J Ophthalmol. 2014;157:154–62.e1. doi: 10.1016/j.ajo.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Werner L, Wilbanks G, Nieuwendaal CP, Dhital A, Waite A, Schmidinger G, et al. Localized opacification of hydrophilic acrylic intraocular lenses after procedures using intracameral injection of air or gas. J Cataract Refract Surg. 2015;41:199–207. doi: 10.1016/j.jcrs.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 13.Jorge Pde A, Jorge D, Ventura CV, Ventura BV, Lira W, Ventura MC, et al. Late opacification in hydrophilic acrylic intraocular lenses: Analysis of 87 eyes in a random sample of 102 patients. J Cataract Refract Surg. 2013;39:403–7. doi: 10.1016/j.jcrs.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 14.Leysen I, Bartholomeeusen E, Coeckelbergh T, Tassignon MJ. Surgical outcomes of intraocular lens exchange: Five-year study. J Cataract Refract Surg. 2009;35:1013–8. doi: 10.1016/j.jcrs.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 15.Mamalis N, Brubaker J, Davis D, Espandar L, Werner L. Complications of foldable intraocular lenses requiring explantation or secondary intervention--2007 survey update. J Cataract Refract Surg. 2008;34:1584–91. doi: 10.1016/j.jcrs.2008.05.046. [DOI] [PubMed] [Google Scholar]
- 16.Oh SY, Lee SJ, Park JM. Comparision of surgical outcomes of intraocular lens refixation and intraocular lens exchange with perfluorocarbon liquid and fibrin glue-assisted sutureless scleral fixation. Eye (Lond) 2015;29:757–63. doi: 10.1038/eye.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fernández-Buenaga R, Alió JL, Pinilla-Cortés L, Barraquer RI. Perioperative complications and clinical outcomes of intraocular lens exchange in patients with opacified lenses. Graefes Arch Clin Exp Ophthalmol. 2013;251:2141–6. doi: 10.1007/s00417-013-2411-7. [DOI] [PubMed] [Google Scholar]
- 18.Moussa K, Leng T, Oatts JT, Bhisitkul RB, Hwang DG, Stewart JM, et al. Manual removal of intraocular lens silicone oil droplets and dystrophic calcifications using a nitinol loop: A case series. Ophthalmic Surg Lasers Imaging Retina. 2017;48:422–6. doi: 10.3928/23258160-20170428-09. [DOI] [PubMed] [Google Scholar]


