Abstract
Background
The objective of the study was to identify risk factors for poor prognosis of cervical spinal cord injury (SCI) with subaxial cervical fracture-dislocation after surgical treatment.
Material/Methods
A total of 60 cervical SCI patients with subaxial cervical fracture-dislocation were primarily included in the study from April 2013 to April 2018. All the enrolled subjects received surgical treatment. The enrolled patients with complete follow-up record were divided into 2 groups based on the neural function prognosis: a non-functional restoration group and a functional restoration group. Multivariate regression analysis was performed to identify independent risk factors for poor prognosis of SCI after surgical treatment.
Results
Fifty-five subjects were included in this study, and the follow-up time ranged from 8.5 to 44.5 months. A total of 25 subjects were categorized into the non-functional restoration group and 30 subjects into the functional restoration group. According to the results of multivariate regression analysis, time from injury to operation (more than 3.8 days), subaxial cervical injury classification (SLIC, score more than 7.5), and maximum spinal cord compression (MSCC, more than 55.8%) are independent risk factors for poor prognosis of SCI after surgical treatment (p<0.05), with AUCs of 0.95 (time from injury to operation), 0.91 (SLIC score), and 0.96 (MSCC).
Conclusions
Time from injury to operation (more than 3.8 days), SLIC score (more than 7.5), and MSCC (more than 55.8%) are independent risk factors for poor prognosis of SCI with subaxial cervical fracture-dislocation after surgical treatment.
MeSH Keywords: Advance Care Planning; Neurosurgery; Osteoarthritis, Spine
Background
Spinal cord injury (SCI) has placed a formidable emotional, physical, and financial burden on people worldwide. Cervical spinal cord injury is the most common form of SCI. The most frequent cause of cervical SCI is violence-related injury. Moreover, the weight-bearing and flexible nature of vertebrae at the cervical level make it particularly susceptible to injury [1,2]. Clinical studies have shown that the incidence of cervical SCI in most countries ranges from 30 to 70 new cases per year, and lower cervical SCI (C3 to C7) accounts for approximately two-thirds of SCI with cervical fractures and three-quarters of SCI with cervical dislocations [3,4].
There has been no clear consensus on the optimal treatment for cervical SCI with subaxial cervical fracture-dislocation [5]. Multiple factors may influence treatment strategies, such as classification of fracture-dislocation, neurological status of the patient, traumatic disc herniation, and unilateral and bilateral cervical facet dislocation; surgery is the recommended treatment for patients with persistent spinal cord compression [6–8]. Thus, this study was carried out to identify risk factors for poor prognosis of SCI with subaxial cervical fracture-dislocation after surgical treatment.
Material and Methods
Ethical considerations
The study protocol was approved by the Ethics Committee of the First People’s Hospital of Taizhou. Informed consent was obtained from the enrolled subjects before the study. All the research methods were carried out in accordance with relevant ethics guidelines and regulations.
Subjects selected for the study
Sixty cervical SCI patients with subaxial cervical fracture-dislocation were primarily included in the study from April 2013 to April 2018. Inclusion criteria were: cervical SCI with subaxial cervical fracture-dislocation (C3–C7) confirmed by magnetic resonance imaging (MRI) and computed tomography (CT), underwent surgical treatment (anterior cervical approach), age 18–60 years, and patients or family agreed to participate and signed the informed consent. The exclusion criteria were: previous history of cervical spine surgery, compression fracture of the cervical vertebra, cervical tumour, or other diseases associated with cervical spondylosis (disc protrusion or spinal canal stenosis); lost during the follow-up period; incomplete prognosis condition and treatment data; did not sign informed consent; and refused surgical treatment. In addition to the demographic and follow-up data, we also collected information on the following potential risk factors: types of injury (e.g., traffic injury, high falling injury, and heavy impact injury), time between injury and medical treatment; time between injury and operation, injury segment that indicates cervical vertebrae segment is involved in SCI, and information regarding whether the patients underwent steroid therapy within 8 h after SCI (methylprednisolone impact therapy or dexamethasone impact therapy). The classification of patients with SCI was based on the subaxial cervical injury classification (SLIC) system, which is based on the injury morphology determined by the pattern of spinal column disruption using available imaging studies, the disco-ligamentous complex represented by both anterior and posterior ligamentous structures and intervertebral disc, and neurologic status, and these 3 injury characteristics were recognized as the significant predictors of clinical outcome. Surgical treatment was recommended for patients with scores >4 and conservative treatment [9] for patients with scores <4; length of spinal cord edema caused by cervical SCI was measured during MRI before surgery. The American Spinal Injury Association (ASIA) system was used to measure neurological function and for outcome analysis preoperatively and postoperatively, where grade A indicates complete SCI without sensory and motor function retention, grade B indicates incomplete SCI with sensory function retention, grade C indicates incomplete SCI with motor function retention (muscle strength is less than 3), grade D indicates incomplete SCI with motor function retention (muscle strength is more than 3), and grade E indicates incomplete SCI with normal sensory and motor function [10]. Maximum spinal cord compression (MSCC) was the parameter used to describe the degree of spinal compression: {1–di/[1/2(da+db)}×100%, where da and db denote the spinal cord diameter in the upper and lower injury segment [11], respectively.
Operation and postoperative treatment
Presurgical preparation
Continuous skull traction was performed for each patient using Gardner-Wells tongs with 8–10 lbs of weight to achieve cervical immobilization and to avoid secondary spinal cord injury.
Operation
All the enrolled subjects agreed to anterior cervical surgery including anterior open decompression, reduction, and spinal arthrodesis. The surgical methods included anterior cervical discectomy and fusion (ACDF) and anterior cervical corpectomy decompression and fusion (ACCF). The surgical intervention is planned based on the physical condition of patients after severe trauma. The operation was performed under skull traction.
Postoperative treatment
Antibiotics, dexamethasone, dehydrating agents (mannitol), and neurotrophic agents (ganglioside) were routinely given for 2–5 days after surgery. All patients were recommended to wear a rigid cervical collar for 6–8 weeks after surgery.
Follow-up and grouping
Postoperative follow-up included clinical visits every 3 months. All the enrolled subjects were divided into 2 groups – a functional restoration group and a non-functional restoration group-based on the last ASIA score of spinal function. Patients in the functional restoration group showed improved neural function after the operation, from A to B or C or D or E, from B to C or D or E, and from D to E, based on the ASIA scores; whereas the patients in the non-functional restoration group did not show any improvement based on the ASIA scores. No other complications were recorded in the enrolled subjects. The follow-up period was defined as the time from initial surgery to last follow-up.
Statistical analysis
All statistical analyses were carried out using SPSS 21.0 (SPSS, Chicago, IL, USA). Normal distribution analysis was carried out before the univariate analysis of data. The t test and χ2 test (univariate analysis) were used for comparison of continuous and categorical data (normally distributed) between the functional restoration group and non-functional restoration group, while the rank sum test was used for comparison of normally distributed data between the 2 groups. Logistic multivariate regression analysis was used to identify factors associated with poor prognosis after surgical treatment. Receiver operating characteristic (ROC) curves were constructed to identify the most significant predictors of poor prognosis after surgical treatment. Tests were 2-tailed and a p<0.05 was considered significant. Data are presented as mean ± standard deviations.
Results
Patient characteristics
A total of 55 subjects with complete follow-up were included, and the follow-up time ranged from 12.0 to 74.5 months. Five subjects died immediately after the operation, 2 died within 1 year, 2 died at 1–2 years, and 1 died 2–3 years after the operation. Three subjects died due to respiratory failure, 1 died due to pulmonary infection, and died from asphyxia due to phlegm clogging, respectively. The dead subjects were excluded from the study. On the basis of the ASIA grading of preoperative and final follow-up, a total of 30 subjects with recovery of spinal function were assigned into the functional restoration group, and 25 subjects without recovery of spinal function were assigned into the non-functional restoration group (Table 1).
Table 1.
ASIA grading of preoperative and final follow-up.
| Preoperative ASIA | Number of cases | ASIA of the final follow-up | |||||
|---|---|---|---|---|---|---|---|
| Recovery rate | A | B | C | D | E | ||
| A | 25 | 5/25 (20.0%) | 20 | 3 | 1 | 1 | 0 |
| B | 17 | 13/17 (76.5%) | 0 | 4 | 9 | 3 | 1 |
| C | 8 | 7/8 (87.5%) | 0 | 0 | 1 | 5 | 2 |
| D | 5 | 5/5 (100.0%) | 0 | 0 | 0 | 0 | 5 |
Univariate and multivariate analysis
Univariate analysis was carried out for all follow-up data. The results showed that time from injury to operation, steroid therapy within 8 h after injury, SLIC score, and MSCC were associated with poor prognosis of cervical spinal cord injury with subaxial cervical fracture-dislocation after surgical treatment (p<0.05) (Table 2). No significant differences were detected in age of patients, cause of injury, time from injury to medical treatment, length of the cord edema, injury segment, and mean follow-up duration (p>0.05). For the significant parameters of univariate analysis (time from injury to operation, steroid therapy in 8 h after injury, SLIC score, and MSCC), stepwise regression was carried out in the process of multivariate analysis, showing that time from injury to operation (more than 3.8 days), SLIC score (more than 7.5), and MSCC (more than 55.8%) are independent risk factors for poor prognosis after surgical treatment, based on the results of the logistic multivariate analysis (p<0.05) (Table 2).
Table 2.
Univariate and multivariate analysis of poor prognosis (n=55).
| Factor | Non-functional restoration group (n=25) | Functional restoration group (n=30) | Univariate analysis | Multivariate analysis | |
|---|---|---|---|---|---|
| P | (HR 95% CI) | P | |||
| Age (years) | 31.9±5.7 | 29.4±6.7 | 0.14 | ||
| Cause of injury | |||||
| Traffic injury | 12 (48.0%) | 14 (46.7%) | |||
| High falling injury | 7 (28.0%) | 10 (33.3%) | |||
| Heavy impact injury | 6 (24.0%) | 6 (20.0%) | 0.89 | ||
| Time from injury to medical treatment (h) | 12.2±6.7 | 10.6±6.5 | 0.38 | ||
| Time from injury to operation (days) | 4.4±2.0 | 1.2±0.5 | 0.00 | 0.26, 0.13–0.40 | 0.00 |
| Length of the cord edema (mm) | 15.4±1.8 | 14.1±2.5 | 0.27 | ||
| Injury segment | |||||
| C3–C4 | 4 (16.0%) | 3 (10.0%) | |||
| C4–C5 | 5 (20.0%) | 6 (20.0%) | |||
| C5–C6 | 7 (28.0%) | 10 (33.3%) | |||
| C6–C7 | 7 (28.0%) | 9 (30.0%) | |||
| C7–T1 | 2 (8.0%) | 2 (6.7%) | 0.96 | ||
| Hormone therapy within 8 h after injury | |||||
| Yes | 16 (64.0%) | 27 (90.0%) | |||
| No | 9 (36.0%) | 3 (10.0%) | 0.02 | 1.23, 0.21–2.20 | 0.07 |
| SLIC score | 7.6±0.6 | 6.3±0.7 | 0.00 | 0.07, 0.02–0.26 | 0.00 |
| MSCC (%) | 69.9±13.5 | 36.6±12.9 | 0.00 | 0.85, 0.78–0.92 | 0.00 |
| Mean follow-up duration (months) | 48.0±6.8 | 50.2±9.2 | 0.81 | ||
SLIC – subaxial cervical injury classification; MSCC – maximum spinal cord compression.
ROC curve analysis
ROC curves were constructed to identify effective predictors for poor prognosis. The results confirmed that all the 3 parameters – time from injury to operation, SLIC score, and MSCC – are significant predictors for poor prognosis of cervical spinal cord injury with subaxial cervical fracture-dislocation after surgical treatment, with AUC of 0.95 (time from injury to operation more than 3.8 days) (Figure 1), 0.91 (SLIC score, more than 7.5) (Figure 2), and 0.96 (MSCC, more than 55.8%) (Figure 3), respectively.
Figure 1.
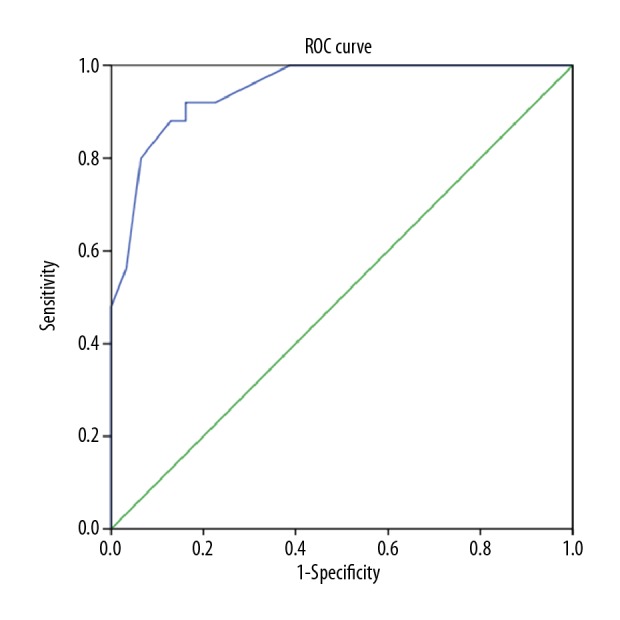
The ROC curve of the time from injury to operation is shown, and the AUC value is 0.95 with good prediction of poor prognosis after the anterior cervical fusion. ROC – receiver operating characteristic; AUC – area under curve.
Figure 2.
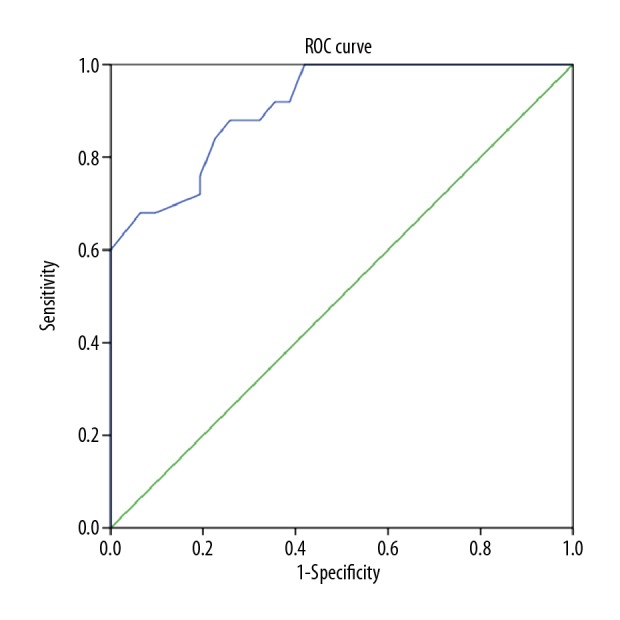
The ROC curve of SLIC score is shown, and the AUC value is 0.91 with good prediction of poor prognosis after the anterior cervical fusion. ROC – receiver operating characteristic; AUC – area under curve; SLIC – subaxial cervical injury classification.
Figure 3.
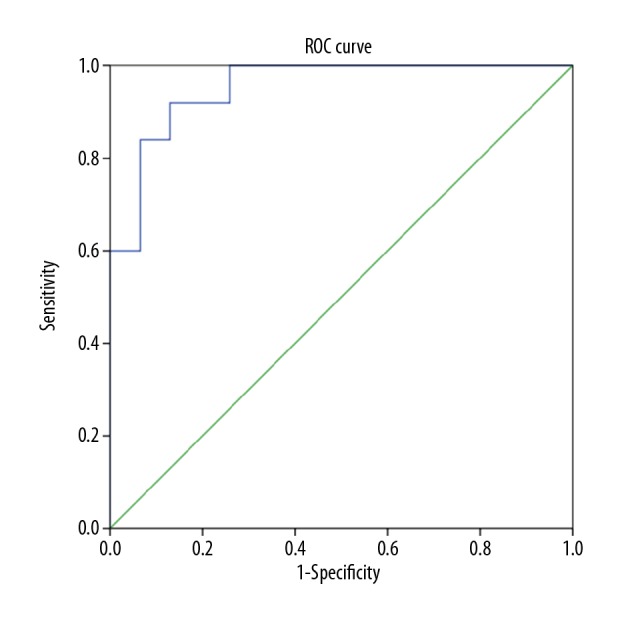
The ROC curve of MSCC is shown, and the AUC value is 0.96 with good predictions of poor prognosis after the anterior cervical fusion. ROC – receiver operating characteristic; AUC – area under curve; MSCC – maximum spinal cord compression.
Discussion
Cervical spinal cord trauma with subaxial cervical fracture-dislocation (whether complete or incomplete) is a devastating injury and is considered incurable. Patients with such injuries are confronted with 2 interrelated problems: one is an ongoing neurologic injury by continued compression, and the other is instability that prevents mobilization and rehabilitation and may interfere with management of coexisting problems [12,13]. Numerous methods are used to address these problems. Spinal immobilization, early surgical decompression, and steroids for SCI and blood pressure augmentation are recommended for early management. Trials in neuroprotection should be the next step, including pharmacological therapies and nonpharmacologic therapies [14]. Spinal surgery is recommended for patients with an unstable cervical spine, as it can impart immediate stability and alignment to promote fusion [15,16]. Several studies have reported the clinical advantages of the posterior stabilization method for resisting flexion-extension injuries [17–20]. The anterior stabilization method has received considerable interest among spinal surgeons because it can decompress the spinal canal by removing the disc or bony fragments from the anterior side [21–23].
Results of multivariate analysis showed that time from injury to operation, SLIC score, and MSCC are independent risk factors for poor prognosis after surgical treatment. A previous study [24] in dogs sought to determine whether there is a relationship between the duration of sustained spinal cord compression and the extent of spinal cord injury and the capacity for functional recovery after decompression. The results confirmed that the spinal cord underwent viscoelastic relaxation during sustained compression; nonetheless, a longer duration of compression injury was associated with reduced electrophysiological recovery, increased pathological changes, and significant functional impairment. Hence, sustained displacement is an important factor in the secondary injury process, and early spinal cord compression can prevent or reduce secondary injury. Schlege et al. [25] revealed that the mortality rate and hospitalization time could be reduced if the patient underwent an initial operation within 72 h after the cervical SCI; however, no clinical or experimental studies ever explored the exact decompression time until now. We found that the average time from injury to operation was 1.4±0.5 days in the functional restoration group, and 4.4±2.0 days in the non-functional restoration group. ROC curve analysis confirmed that delaying time from injury to operation (more than 3.8 days) can lead to poor prognosis after surgical treatment, which may provide evidence for the spinal surgeon in deciding on the optimal operation time. Some studies found that patients with rotation of cervical vertebra, incomplete SCI, continuous multisegmental spinal compression, and DLC disrupture were suitable for surgical treatment [26]. Some other studies confirmed that surgical treatment could be used for patients with SLIC scores >4, and nonsurgical treatment is best for subjects with SLIC scores <4 [9]. The SLIC scores of all the enrolled subjects in the 2 groups were over 4; therefore, surgical treatments were used. The results of multivariate analysis showed that SLIC score (more than 7.5) could be a risk factor for poor prognosis of cervical SCI with subaxial cervical fracture-dislocation after surgical treatment, because the degree of the cervical SCI aggravates as the SLIC score increases, which indicates poor fracture morphology, severe cervical nerve injury, or SLC complex injury. Full functional recovery of the cervical spinal cord is hard to achieve for patients with a degree of spinal cord compression more than 50% in the acute injury mode [27–29]. Our study showed that MSCC of more than 55.8% can result in poor prognosis of cervical SCI with inferior cervical fracture-dislocation after surgical treatment, and our results are consistent with previous studies and could also be helpful for the spinal surgeon in deciding on the optimal operation time. Our study has certain limitations that should be considered: the limited number of enrolled subjects, short follow-up time, retrospective design, and few evaluation indicators. Further studies are urgently needed to investigate possible risk factors for poor prognosis of cervical spinal cord injury with subaxial cervical spine fracture-dislocation after surgical treatment.
Conclusions
Time from injury to operation, SLIC score, and MSCC are independent risk factors for poor prognosis of cervical SCI patients with inferior cervical fracture-dislocation after surgical treatment.
Abbreviations
- SCI
spinal cord injury
- MRI
magnetic resonance imaging
- CT
computed tomography
- SLIC
subaxial cervical injury classification
- ASIA
American Spinal Injury Association
- MSCC
maximum spinal cord compression
- ACDF
anterior cervical discectomy and fusion
- ROC
receiver operating characteristic
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Wilcox JT, Satkunendrarajah K, Zuccato JA, et al. Neural precursor cell transplantation enhances functional recovery and reduces astrogliosis in bilateral compressive/contusive cervical spinal cord injury. Stem Cells Transl Med. 2014;3(10):1148–59. doi: 10.5966/sctm.2014-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y, Li J, Li Y, Shen Y, et al. Incidence and risk factors of poor clinical outcomes in patients with cervical kyphosis after cervical surgery for spinal cord injury. Ther Clin Risk Manag. 2017;13:1563–68. doi: 10.2147/TCRM.S150096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodrigues LF, Moura-Neto V. Biomarkers in spinal cord injury: From prognosis to treatment. Mol Neurobiol. 2018;55(8):6436–48. doi: 10.1007/s12035-017-0858-y. [DOI] [PubMed] [Google Scholar]
- 4.Wang B, Zhu Y, Jiao Y, et al. A new anterior-posterior surgical approach for the treatment of cervical facet dislocations. J Spinal Disord Tech. 2014;27(3):E104–9. doi: 10.1097/BSD.0b013e318291c9f9. [DOI] [PubMed] [Google Scholar]
- 5.Shen Y, Shen HL, Feng ML, et al. Immediate reduction under general anesthesia and single-staged anteroposterior spinal reconstruction for fracture-dislocation of lower cervical spine. J Spinal Disord Tech. 2015;28(1):E1–8. doi: 10.1097/BSD.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 6.Khorasanizadeh M, Yousefifard M, Eskian M, et al. Neurological recovery following traumatic spinal cord injury: A systematic review and meta-analysis. J Neurosurg Spine. :2019. doi: 10.3171/2018.10.SPINE18802. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Sun K, Sun J, Wang S, et al. Placement of titanium mesh in hybrid decompression surgery to avoid graft subsidence in treatment of three-level cervical spondylotic myelopathy: Cephalad or caudal. Med Sci Monit. 2018;24:9479–87. doi: 10.12659/MSM.912650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen S, Levi AD. Restorative treatments for spinal cord injury. Neurosurg Clin N Am. 2017;28(1):63–71. doi: 10.1016/j.nec.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Vaccaro AR, Hulbert RJ, Patel AA, et al. The subaxial cervical spine injury classification system: A novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007;32(21):2365–74. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 10.Waters RL, Adkins R, Yakura J, et al. Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch Phys Med Rehabil. 1994;75(7):756–60. [PubMed] [Google Scholar]
- 11.Fehlings MG, Furlan JC, Massicotte EM, et al. Interobserver and intraobserver reliability of maximum canal compromise and spinal cord compression for evaluation of acute traumatic cervical spinal cord injury. Spine (Phila Pa 1976) 2006;31(15):1719–25. doi: 10.1097/01.brs.0000224164.43912.e6. [DOI] [PubMed] [Google Scholar]
- 12.Brodke DS, Anderson PA, Newell DW, et al. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech. 2003;16(3):229–35. doi: 10.1097/00024720-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Koivikko MP, Myllynen P, Santavirta S. Fracture dislocations of the cervical spine: A review of 106 conservatively and operatively treated patients. Eur Spine J. 2004;13(7):610–16. doi: 10.1007/s00586-004-0688-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahuja CS, Nori S, Tetreault L, et al. Traumatic spinal cord injury-repair and regeneration. Neurosurgery. 2017;80(3S):S9–22. doi: 10.1093/neuros/nyw080. [DOI] [PubMed] [Google Scholar]
- 15.Wang J, Eltorai A, Depasse JM, et al. Variability in treatment for patients with cervical spine fracture and dislocation: An analysis of 107,152 patients. World Neurosurg. 2018;114:e151–57. doi: 10.1016/j.wneu.2018.02.119. [DOI] [PubMed] [Google Scholar]
- 16.Guo H, Wang B, Hao D. Surgical treatment of lower cervical fracture-dislocations with spinal cord injuries by anterior approach (5 to 15 years follow-up) Spine J. 2015;15(10 Suppl):S92. doi: 10.1016/j.wneu.2018.03.213. [DOI] [PubMed] [Google Scholar]
- 17.Kim SM, Lim TJ, Paterno J, et al. A biomechanical comparison of 3 surgical approaches in bilateral subaxial cervical facet dislocation. J Neurosurg Spine. 2004;1(1):108–15. doi: 10.3171/spi.2004.1.1.0108. [DOI] [PubMed] [Google Scholar]
- 18.Xue D, Chen Q, Chen G, et al. Posterior arthrodesis of C1–C3 for the stabilization of multiple unstable upper cervical fractures with spinal cord compromise: A case report and literature review. Medicine (Baltimore) 2017;96(1):e5841. doi: 10.1097/MD.0000000000005841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kandziora F, Pflugmacher R, Scholz M, et al. Posterior stabilization of subaxial cervical spine trauma: Indications and techniques. Injury. 2005;36(Suppl 2):B36–43. doi: 10.1016/j.injury.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Wu JP, Wang QB, Feng XJ, et al. Relationship between modic changes and sagittal balance parameters in the cervical spine. Med Sci Monit. 2018;24:6102–6. doi: 10.12659/MSM.909773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garvey TA, Eismont FJ, Roberti LJ. Anterior decompression, structural bone grafting, and Caspar plate stabilization for unstable cervical spine fractures and/or dislocations. Spine (Phila Pa 1976) 1992;17(10 Suppl):S431–35. doi: 10.1097/00007632-199210001-00015. [DOI] [PubMed] [Google Scholar]
- 22.Donnarumma P, Bozzini V, Rizzi G, et al. Surgical management of C-type subaxial cervical fractures using cervical traction followed by anterior cervical discectomy and fusion within 12 h after the trauma. J Craniovertebr Junction Spine. 2017;8(4):338–41. doi: 10.4103/jcvjs.JCVJS_99_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dvorak MF, Fisher CG, Fehlings MG, et al. The surgical approach to subaxial cervical spine injuries: An evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976) 2007;32(23):2620–29. doi: 10.1097/BRS.0b013e318158ce16. [DOI] [PubMed] [Google Scholar]
- 24.Carlson GD, Gorden CD, Oliff HS, et al. Sustained spinal cord compression: Part I: Time-dependent effect on long-term pathophysiology. J Bone Joint Surg Am. 2003;85-A(1):86–94. [PubMed] [Google Scholar]
- 25.Schlegel J, Bayley J, Yuan H, et al. Timing of surgical decompression and fixation of acute spinal fractures. J Orthop Trauma. 1996;10(5):323–30. doi: 10.1097/00005131-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of 3 hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61(8):1119–42. [PubMed] [Google Scholar]
- 27.Shen B, Zhang Z, Zhou NF, et al. Preparing platelet-rich plasma with whole blood harvested intraoperatively during spinal fusion. Med Sci Monit. 2017;23:3578–84. doi: 10.12659/MSM.902025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim M, Hong SK, Jeon SR, et al. Early (≤48 hours) versus late (>48 hours) surgery in spinal cord injury: Treatment outcomes and risk factors for spinal cord injury. World Neurosurg. 2018;118:e513–25. doi: 10.1016/j.wneu.2018.06.225. [DOI] [PubMed] [Google Scholar]
- 29.Vicenty-Padilla JC, De Jesus O. Interval recovery of syringomyelia in Chiari I malformation patient with acute cervical trauma after anterior decompression: Case report and review of literature. World Neurosurg. 2018;118:240–42. doi: 10.1016/j.wneu.2018.06.229. [DOI] [PubMed] [Google Scholar]


