Abstract
Hydatidosis is a frequent infestation in large endemic areas, caused by helminths. Primary localization within the muscle or bone tissues is rare. We report the case of a 52-year-old woman with a cystic lesion located in the right pectoralis minor muscle, who was initially diagnosed with cystic lymphangioma by imaging examination. She was submitted for surgical treatment; in block resection of the tumor along with the involved muscle was performed. The histopathological diagnosis was of hydatid cyst. The contribution of the ancillary lab tests is analyzed for a precise preoperative diagnostic approach. This case well illustrates that the most likely is not always what it appears to be. Facing of a cystic lesion in the lungs, liver or muscle, clinicians should always think on hydatid disease, particularly in endemic areas.
Keywords: Echinococcosis; Lymphangioma, Cyst; Muscular Disease; Thoracic Wall
INTRODUCTION
Hydatidosis is a frequent infestation in large endemic areas, caused by helminths. The involvement of the muscular or bone tissues is rare. Hydatidosis is a zoonosis caused by the larval form of the genus Echinococcus. The infestation occurs in humans after the ingestion of the eggs excreted with the feces by the definitive hosts such as dogs and foxes. Hydatidosis involves the liver and the lungs primarily, since they are capillary filters.1 Musculoskeletal hydatidosis occurs in only 1-4% of the cases.1 As far as we know, this is the first case report showing the involvement of the pectoralis minor muscle.
We present a clinical case of hydatid disease of the pectoralis muscle, accompanied by a discussion on the contribution of the ancillary tests to the diagnostic approach.
CASE REPORT
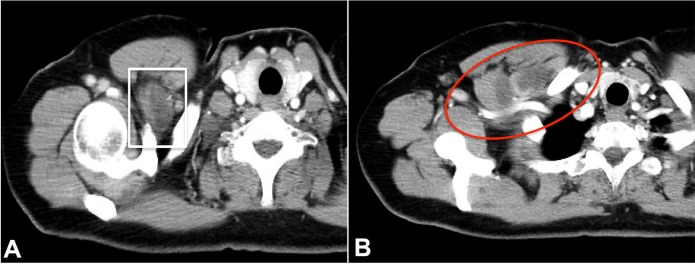
A 52-year-old woman sought the medical facility complaining of a painful tumor in the right pectoral region over the last 8 months. The patient lived in the rural area but had no contact with livestock or domestic animals. During the last 5 months, she reported two episodes of bulging mass over the right frontal chest region accompanied by inflammatory signs that subsided within 1-2 weeks. Her past medical history was unremarkable. Her blood tests were normal. However, the thoracic computed tomography (CT) depicted a 60 mm bilobed and cystic lesion in the right pectoralis minor muscle, which compressed the right subclavian vein at the exit of the costoclavicular space. These findings were consistent with cystic lymphangioma or intramuscular myxoma (Figure 1).
Figure 1. Thoracic CT – Axial plane showing a bilobed cystic lesion within the pectoralis minor muscle, which bulges the muscle contour from its insertion into the coracoid process (A) and compresses the right subclavian vein to the outlet of the costoclavicular space (B).
The magnetic resonance imaging (MRI) of the shoulder confirmed a soft-tissue tumor affecting the pectoralis minor, which measured 6.3x4.4x1.6 cm. The mass was delimited by the muscular aponeurosis, preserved the brachial plexus; and cranially reached the coracoid process. The lesion showed a thin and well-defined margin except for its posterior and cranial margin, showed hyperintense signal in T2 weighted images, and no contrast enhancement was observed. These findings were consistent with a vascular malformation of lymphatic origin (cystic lymphangioma) (Figure 2).
Figure 2. MRI T2 weighted images of the pectoral region showing a cystic tumor of 6.3 cm within the pectoralis minor muscle (A and B: axial plane; C and D: coronal plane). The lobed cyst (D) presented a density with a very high signal in T2 weighted images (A and B).
Given the nature of these findings and their potential vascular injury, the surgical resection was performed through a right infraclavicular incision. The exeresis of the tumor also involved the right pectoralis minor muscle. Intraoperatively, an intramuscular tumor of 6 cm was found, lined by a fibrous capsule. The cranial tumor part was in close contact with the coracoid process, and with the subclavian-axillary axis, which required careful dissection to avoid a vascular injury. During the resection, the tumor capsule was violated with drainage of a caseous content but was immediately sutured.
The gross examination revealed an irregular lobed cystic and encapsulated tumor of 6.5x4x2.5 cm, which at the cut surface showed a light-yellowish center. The histopathology revealed a fibrous capsule admixed with inflammatory infiltrate. The center of the lesion showed abundant proteinaceous debris, and a thick, acellular layer fragmented and collapsed towards the lumen (Figure 3). No germ layer was identified with nucleated cells, daughter vesicles or a scolex. The final pathologic diagnosis was a hydatid cyst with pericystic layer and cuticle, with free surgical margins.
Figure 3. Photomicrograph of the lesion. A – Panoramic view of the encapsulated cystic lesion containing a hydatid cyst cuticle (H&E, low power), B – Cystic wall composed of fibrous tissue and inflammatory infiltrate. Inside, hydatid membranes (H&E, 4X). C and D – Wall of the hydatid membranes. (H&E, 10X and 20X respectively).
The postoperative period was uneventful. After the diagnostic confirmation, a serological study was performed and was positive for Echinococcus granulosus. No involvement was found in other sites in a postoperative body CT scan. The patient was treated with oral albendazole, 800 mg/day, two cycles of 28 days, separated by a rest period of 14 days. Currently, the patient is asymptomatic, without any functional sequelae.
DISCUSSION
Hydatid disease is a parasitic infestation caused by a tapeworm of the genus Echinococcus.1 The main endemic areas are the Mediterranean countries, the Middle East, southern Africa, the southern part of South America, New Zealand, Australia, and Iceland.2 The most frequent clinical forms of hydatidosis are pulmonary (15%) and hepatic (65%). The musculoskeletal condition is uncommon (1%–4%),1 what renders few data on this involvement.3 Daali et al.3 published a series comprising 15 cases with muscular involvement, mostly affecting the diaphragm or the psoas muscles, without synchronous hepatic or pulmonary involvement. However, the involvement of these visceral organs should be discarded during the diagnostic process, because of its frequency.
Imaging exams are fundamental to the diagnosis and include some typical patterns as the unilocular cyst, the multivesicular lesion (highly characteristic), and the atypical complex or solid lesion.4,5 The multivesicular lesion is formed by the grouping of multiple daughter vesicles within the original cyst is characteristic but not pathognomonic, though.4,6 When the cysts are not viable, they do not produce fluid;5 the case presented corresponded to a non-viable hydatid cyst. In some cases, an inflammatory reaction may produce changes that resemble an atypical complex or solid lesion, challenging the differential diagnosis. The MRI is considered the imaging exam of choice, because of the higher sensitivity and specificity.5,6
Immunological tests have been shown to be useful for the diagnosis of visceral hydatid disease.7 Cystic echinococcosis is one of the few parasitic infections in which the basis for laboratory diagnosis is primarily serology.8 Indirect hemagglutination test and enzyme-linked immunosorbent assay are the most widely used methods for detection of anti-Echinococcus antibodies (IgG). Nonetheless, no standard, highly sensitive, and specific serologic test exists for cystic echinococcosis antibody detection.9 Furthermore, in the cases of osteomuscular involvement, the sensitivity of these tests is decreased.10 According to Rigano et al.11 the decrease in the sensitivity may be due to inadequate activation of T-helper-2 lymphocytes, with the consequent reduction in the peripheral expression of immunoglobulins. In our case, the lack of the diagnosis suspicion was responsible for not testing the serologic exam. However, once the diagnosis was established, the serological study was performed, which was positive.
Treatment-wise, surgery is the best option, always performed with a large margin of safety due to the high risk of relapse, regardless of the site of the lesion. Depending on the location and the relationship with vital structures, this will determine the prognosis.10 Nevertheless, minimally invasive approaches are currently being considered, as the laparoscopy and the PAIR (puncture, aspiration, injection, and reaspiration).12
Some authors consider the preoperative treatment with benzimidazole derivatives to be fundamental, and likewise for 3 more months postoperatively.3 In our case, the preoperative pharmacological treatment was not considered due to the lack of diagnostic suspicion. The accidental cyst injury during the surgical procedure did not cause any harm due to the absence of viability of the parasite. The convenience of preoperative treatment, together with the risk of rupture of the cyst during surgery with the implications that it entails, highlights the importance of considering the diagnosis of hydatid cyst in the differential diagnosis of this type of lesion for an optimal preoperative study and appropriate therapeutic management (especially in endemic regions).
Footnotes
How to cite: García-Tirado J, Allué-Cabañuz M, Muñoz-González N, Viso-Soriano MJ, Marquina-Ibáñez I. Cystic lesion of pectoralis minor muscle: learning from mistakes. Autops Case Rep [Internet]. 2019;9(2):e20180780. https://doi.org/10.4322/acr.2018.078
The authors retain an informed consent document signed by the patient, and the manuscript is in accordance with the requirements of the institutional ethics committee.
Financial support: None
REFERENCES
- 1.Merkle EM, Schulte M, Vogel J, et al. Musculosketal involvement in cystic echinococcosis: report of eight cases and review of the literature. AJR Am J Roentgenol. 1997;168(6):1531-4. 10.2214/ajr.168.6.9168719. [DOI] [PubMed] [Google Scholar]
- 2.Ito A, Budke CM. The echinococcoses in Asia: the present situation. Acta Trop. 2017;176:11-21. 10.1016/j.actatropica.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 3.Daali M, Hssaida R. L’hydatidose musculaire: 15 cases. Presse Med. 2000;21(29):1166-9. [PubMed] [Google Scholar]
- 4.Martin J, Marco V, Zidan A, Marco C. Hydatid disease of the soft tissues of the lower limb: findings in three cases. Skeletal Radiol. 1993;22(7):511-4. 10.1007/BF00209098. [DOI] [PubMed] [Google Scholar]
- 5.Marzouki A, Naam A, Abdulrazak S, Soumaré B, Lahrach K, Boutayeb F. Musculoskeletal Echinococcus infection as a rare first presentation of hydatid disease: case report. Patient Saf Surg. 2017;11(21):1-5. 10.1186/s13037-017-0136-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vasilevska V, Zafirovski G, Kirjas N, et al. Imaging diagnosis of musculoskeletal hydatid disease. Prilozi. 2007;28(2):199-209. [PubMed] [Google Scholar]
- 7.Torcal J, Navarro-Zorraquino M, Lozano R, et al. Immune response and in vivo production of cytokines in patients with liver hydatidosis. Clin Exp Immunol. 1996;106(2):317-22. 10.1046/j.1365-2249.1996.d01-843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brunetti E, Kern P, Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114(1):1-16. 10.1016/j.actatropica.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Brunetti E. Echinococcosis Hydatid Cyst Workup. Laboratory Studies. New York: Medscape, LLC; 2018. [cited 2019 Dec 27]. Available from: https://emedicine.medscape.com/article/216432-workup [Google Scholar]
- 10.Torcal J, García-Álvarez F, Salinas JC, et al. Hidatidosis muscular primaria. Cir Esp. 2002;72(3):147-51. 10.1016/S0009-739X(02)72029-0. [DOI] [Google Scholar]
- 11.Rigano R, Profumo E, Ioppolo S, Notargiacomo S, Teggi A, Siracusano A. Cytokine patterns in seropositive and seronegative patients with Echinococcus granulosus infection. Immunol Lett. 1998;64(1):5-8. 10.1016/S0165-2478(98)00072-8. [DOI] [PubMed] [Google Scholar]
- 12.Chen X, Cen C, Xie H, Zhou L, Wen H, Zheng S. The comparison of 2 new promising weapons for the treatment of hydatid cyst disease: PAIR and laparoscopic therapy. Surg Laparosc Endosc Percutan Tech. 2015;25(4):358-62. 10.1097/SLE.0000000000000177. [DOI] [PubMed] [Google Scholar]