Dear Editor:
We report the following TMS-related seizure or spell. The subject was a 51 year old man with the following diagnoses: superior sagittal vein thrombosis caused right-sided hemorrhagic lesion (~25 cc) 8 months prior to event. The patient had the following risk factors: protein C and S deficiency, hypercoagulable disorder of unknown type, hypertension, and hyperlipidemia. He was taking the following medications: Vitron-C (125/200 mg), Folic Acid, Lyrica (25 mg PRN), Thiamine (100 mg), Tramadol (50 mg every 6 h), Lisinopril (20 mg), Warfarin (4 mg twice per day), Amlodipine (10 mg), and Lipitor (80 mg). On the day of the event, the subject had no known additional risk factors.
We were delivering TMS in the following manner: The day prior to the seizure, the patient was seen from 10 AMe1 PM and received 70 trials of single pulse TMS (using a MagPro × 100 with an C-B60 coil) over the unaffected hemisphere primary motor cortex. Stimulation intensity was 90% of maximum stimulator output (MSO) for the first 20 trials and 75–85% of MSO for the subsequent 50 trials to determine resting motor threshold. We then applied double-pulse stimulation (ISI = 25 ms, intensity = 90% MSO, 5–8 s interval between successive trials) in the context of a psychomotor reaction time task. These double-pulse trials were applied first over dorsal premotor cortex of the affected hemisphere (80 trials) and then over primary motor cortex of the affected hemisphere (70 trials). He had participated in multiple TMS testing sessions three and five weeks prior, including intermittent theta burst over the unaffected hemisphere and single- and double-pulse disruption over the unaffected hemisphere.
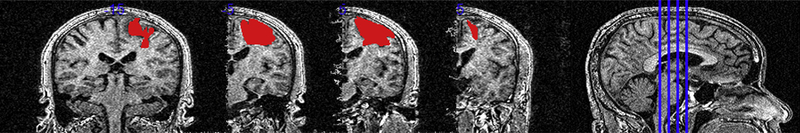
The subject tolerated testing well. However, the next morning, the patient had uncontrollable “twitching” in his affected arm, leg, and face without any change in mental status beginning at approximately4:30AM.Thetwitchingpersistednearlycontinuouslyfortwo days despite administration of lorazepam and low doses of levetiracetam. The twitching resolved after titration of levetiracetam. An MRI showed no acute change. An EEG showed intermittent right central slowing and occasional right parietal sharp waves indicating a right cerebral abnormality and potential right parietal epileptogenic focus. Seizure symptoms resolved but the patient reported new weakness in his leg, and was admitted to an acute rehabilitation hospital. He was ultimately discharged home 16 days after the incident. The patient has had no further seizure activity while on levetiracetam. Blood pressure recorded the day after the event was 118/73. Abnormal labs included high PT (29.3), INR (2.9), chloride (109), and MPV (11.3) as well as low platelet (87) and patient was oriented 4. The patient was not retreated with TMS (Fig. 1).
Figure 1.
Patient multislice.
It is unclear if the prolonged seizure in this case was directly related to TMS, having occurred approximately 20 h after stimulation. Nevertheless, the timing of event is suggestive. The duration of the seizure and persistence of motor effects afterward are noteworthy.
Acknowledgments
NIH K01 HD060886 (PI: ML Harris-Love); NIH T32 NS041231 (PI: K Gale); AHA 14GRNT20460001 (PI: ML Harris-Love): Clint Wutzke, Ph.D.This event was presented at the NYC Neuromodulation Conference 2015. This event was also reported to the Medstar Health IRB.
Contributor Information
Rachael M. Harrington, Graduate Research Assistant, Georgetown University, Interdisciplinary Program in Neuroscience, Medstar National Rehabilitation Hospital, USA.
Evan Chan, Research Engineer, Medstar Health, Research Institute, USA.
Peter E. Turkeltaub, Assistant Professor of Neurology, Georgetown University, Medical Center, USA Director, Aphasia Clinic, Medstar National Rehabilitation Hospital, USA.
Alexander W. Dromerick, Professor of Neurology and Rehabilitation Medicine, Vice Chair and Chief of Service, Department of Rehabilitation, Medicine, Georgetown University Medical Center, USA Vice President for Research, Medstar National, Rehabilitation Hospital, USA.
Michelle L. Harris-Love, Assistant Professor of Neurology, Georgetown University, Medical Center, USA Director of MOTR Lab, National Rehabilitation Hospital, USA.