Abstract
Background:
Acute Care Surgery (ACS) comprises Trauma, Surgical Critical Care, and Emergency General Surgery (EGS), encompassing both operative and non-operative conditions. While the burden of EGS and trauma have been separately considered, the global footprint of ACS has not been fully characterized. We sought to characterize the costs and scope of influence of ACS-related conditions. We hypothesized that ACS patients comprise a substantial portion of the U.S. inpatient population. We further hypothesized that ACS patients differ from other surgical and non-surgical patients across patient characteristics
Methods:
We queried the National Inpatient Sample (NIS) 2014, a nationally representative database for inpatient hospitalizations. In order to capture all adult ACS patients, we included adult admissions with any ICD-9-CM diagnosis of trauma or an ICD-9-CM diagnosis for one of the 16 AAST-defined EGS conditions. Weighted patient data were presented to provide national estimates.
Results:
Of the 29.2 million adult patients admitted to U.S. hospitals, approximately 5.9 million (20%) patients had an ACS diagnosis. ACS patients accounted for $85.8 billion dollars, or 25% of total U.S. inpatient costs ($341 billion). When comparing ACS to non-ACS inpatient populations, ACS patients had higher rates of healthcare utilization with longer lengths of stay (5.9 vs. 4.5 days, p<0.001), and higher mean costs ($14,466 vs. $10,951, p<0.001. Of all inpatients undergoing an operative procedure, 27% were patients with an ACS diagnosis. Overall, 3,186 (70%) of U.S. hospitals cared for both trauma and EGS patients.
Conclusion:
Acute care surgery patients comprise 20% of the inpatient population, but 25% of total inpatient costs in the U.S. In addition to being costly, they overall have higher healthcare utilization and worse outcomes. This suggests there is an opportunity to improve clinical trajectory for ACS patients that in turn, can affect the overall U.S. healthcare costs.
Keywords: Acute care surgery, emergency general surgery, trauma, trauma systems, healthcare utilization
Introduction:
Within the U.S., patients with Emergency General Surgical (EGS) conditions have their care provided through a broad range of practice models.1–4 More recently, “Acute Care Surgery” (ACS) has evolved as a practice model that incorporates Trauma, EGS, and Surgical Critical Care. Whether EGS is provided by surgical hospitalists, surgeons on call, or an ACS service, the combined universe of ACS conditions covers a large number of patients hospitalized in the United States and also likely comprise a large “footprint” of inpatient healthcare utilization and costs.
Previous studies focusing only on Trauma or Emergency General Surgery have found that the costs of each are substantial; however, studies vary in their methodology making the creation of a complete picture of ACS-related costs difficult. Traumatic injuries have been estimated to have annual healthcare costs at over $400 billion when considering index and subsequent hospitalizations, and over $670 billion when considering total cost of care and lost productivity.5 For those with a primary diagnosis of an EGS condition, total inpatient costs for their index admission have been estimated to be approximately $28.2 billion, with an projected increase of nearly 50% between 2010 and 2060.6,7 It stands to reason that a conservative estimate of the combined inpatient costs of these two services alone (e.g.. excluding critical care) may be significant when compared to the whole.
With healthcare expenditures in the United States on the rise, there is increasing pressure to better understand cost distribution and allocation of resources. An important part of this process involves identifying patient populations with the greatest impact on utilization and expenditures so that the relevant stakeholders can appropriately target interventions. This has yet to be done for the combined trauma and EGS population. Furthermore, providers caring for patients with ACS conditions should have a substantial voice in shaping the national dialogue on healthcare reform.
In the current study, we sought to characterize the economic burden of ACS-related conditions. We hypothesized that ACS patients comprise a substantial portion of the U.S. inpatient population as well as healthcare utilization and costs. We also hypothesize that these patients differ substantially from non-ACS surgical patients. Finally, we postulated that there would be regional variation and differences in characteristics among the U.S. hospitals providing ACS services.
Methods:
The 2014 National Inpatient Sample (NIS) from the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality (AHRQ) was used. While 2015 data are available, the methodology for reporting diagnosis codes changed mid-year from International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) to ICD-10-CM codes, which limited the ability to calculate total costing for acute care surgery conditions for the calendar year. For this reason, the year 2014 was used. The NIS is a nationally representative, all-payer, all-hospital database capturing inpatient hospitalizations and contains data for approximately 35 million weighted discharges from U.S. hospitals annually. Throughout this manuscript, weighted data are presented to provide nationally representative estimates.
We captured all adult patients with any trauma or an EGS diagnosis, regardless of whether or not they underwent operative management. The rationale for using any diagnosis vs. primary diagnosis is that patients admitted for another reason who are found to have an ACS diagnosis were likely to require attention to these conditions. Trauma diagnoses were based upon ICD-9CM codes (ICD-9-CM 800.0 to 959.0, excluding 905 to 924), and EGS conditions were based upon one of 16 AAST-defined and graded EGS conditions.8 We excluded patients under the age of 18, and those with missing cost data. Injury Severity Score (ISS) was calculated for each patient using the ICDPIC version 3.0 within Stata/SE version 14.2 (StataCorp, College Station, Texas). Non-ACS patients were defined as all other adult inpatients within our database, including both elective and emergency admissions to hospital.
The primary outcome of interest was the cost of hospitalization. Cost data were obtained by converting charges to cost using conversion ratios provided by HCUP.9 Patient demographic, outcome and utilization variables were analyzed. The NIS codes for race and ethnicity into a single variable. Sub-analysis was performed based upon whether or not patients underwent operative intervention, as defined by HCUP coding for major procedures.10 We also conducted sensitivity analyses on patients who had a primary diagnosis of trauma versus EGS.
Hospital level analysis was also performed in order to determine which hospitals provide ACS services (inpatient care to both trauma and EGS patients). We analyzed the differentiating characteristics of these ACS hospitals, as compared to others in the NIS database. Hospitals within the NIS were categorized by region, teaching status, and as private for-profit, non-profit, and government-owned. Although the region and division location of the hospital were identifiable through the NIS, data was not available at the state or county level. The NIS provides a quartile classification of the estimated median household income of residents in the patients’ ZIP Code, but this was not granular enough to provide data on socioeconomic status at the local patient or hospital level.
Finally, in order to identify predictors associated with differences in costs of an ACS admission, we used a random intercept mixed effects multivariate linear regression model, with a significance set at p<0.05. This controlled for potential confounders at both the patient (including demographic, injury specific and clinical) and hospital level (including urban/rural status, ownership, and region). We tested and verified that the assumptions of the model were satisfied.
All analyses were conducted using StataSE v14.2. The study was exempt from review by the Stanford IRB as data were provided by HCUP in a de-identified format. Use of the NIS followed regulations within the data use agreement as defined by AHRQ.
Results:
Of the weighted 29.2 million adult patients admitted to U.S. hospitals in 2014, approximately 5.9 million (20.3%) inpatients had an ACS diagnosis (Table 1). The majority of ACS patients had an EGS diagnosis (4.3 million, 72.0%), whereas 1.7 million (28.0%) had a diagnosis of trauma.
Table 1.
Acute Care Surgery (Trauma and EGS) Patient and Healthcare Utilization Characteristics, 2014
| ACS Patients 5,928,865 (20.0%) | Non-ACS Patients 23,262,985 (80.0%) | P value | |
|---|---|---|---|
| Patient Characteristics | |||
| Age in 2014, mean (SD), years | 56.3 (0.1) | 61 (0.1) | <0.001 |
| Age by Category, number (%) | |||
| 18–24 years | 236,454 (4.0) | 1,698,966 (7.3) | <0.001 |
| 25–34 years | 475,827 (8.0) | 3,386,255 (14.6) | |
| 35–44 years | 560,484 (9.5) | 2,189,389 (9.4) | |
| 45–54 years | 872,836 (14.7) | 2,828,690 (12.2) | |
| 55–64 years | 1,047,987 (17.7) | 3,803,698 (16.4) | |
| 65–74 years | 1,045,068 (17.6) | 4,005,122 (17.2) | |
| 75–84 years | 960,412 (16.2) | 3,292,841 (14.2) | |
| 85 and older | 732,715 (12.4) | 2,055,106 (8.8) | |
| Gender, number (%) | |||
| Male | 2,793,660 (47.1) | 9,215,867 (39.6) | <0.001 |
| Female | 3,135,205 (52.9) | 14,047,118 (60.4) | |
| Race and ethnicity, number (%) | |||
| White | 4,355,424 (73.5) | 15,690,619 (67.4) | <0.001 |
| Black | 683,089 (11.5) | 3,611,032 (15.5) | |
| Hispanic | 601,352 (10.1) | 2,475,469 (10.6) | |
| Other | 309,434 (5.2) | 1,468,350 (6.3) | |
| Payer Status, number (%) | |||
| Medicare | 3,006,761 (50.7) | 10,535,339 (45.3) | <0.001 |
| Medicaid | 840,725 (14.2) | 4,416,727 (19.0) | |
| Private insurance | 1,512,138 (25.5) | 6,638,227 (28.5) | |
| Self-Pay/Other | 566,321 (9.5) | 1,675,612 (7.2) | |
| Zip Income Quartile, number (%) | |||
| 0–25th Percentile | 1,687,289 (28.5) | 6,813,378 (29.3) | <0.001 |
| 25–50th Percentile | 1,625,986 (27.4) | 6,302,520 (27.1) | |
| 50–75th Percentile | 1,336,987 (22.6) | 5,190,311 (22.3) | |
| 75–100th Percentile | 1,144,321 (19.3) | 4,425,484 (19.0) | |
| Chronic Conditions, number (%) | |||
| None | 669,962 (11.3%) | 3,396,396 (14.6%) | <0.001 |
| 1 | 1,731,228 (29.2%) | 7,606,996 (32.7%) | |
| 2+ | 3,527,675 (59.5%) | 12,259,593 (52.7%) | |
| Healthcare Utilization | |||
| Major Procedure, number (%) | 2,265,288 (38.2) | 6,267,490 (26.9) | <0.001 |
| Length of Stay (LOS), mean (SD), days | 5.87 (0.03) | 4.47 (0.02) | <0.001 |
| LOS if discharge home | 4.29 (0.02) | 3.57 (0.02) | <0.001 |
| LOS if discharge to rehabilitation | 8.63 (0.06) | 7.31 (0.05) | <0.001 |
| Discharge Destination, number (%) | |||
| Routine home | 3,371,659 (56.9) | 15,614,721 (67.1) | <0.001 |
| Discharged with home health | 820,291 (13.8) | 2,968,811 (12.8) | |
| Transfer to rehabilitation/SNF | 1,386,613 (23.4) | 3,418,366 (14.7) | |
| Transfer to other acute hospital | 131,363 (2.2) | 461,231 (2.0) | |
| Died | 143,040 (2.4) | 496,261 (2.1) | |
| Mean Costs of Hospitalization (SD), $ | |||
| $14,466 ($146) | $10,951 ($104) | <0.001 |
ACS: Acute Care Surgery; EGS: Emergency General Surgery, LOS: length of stay; SNF: skilled nursing facility
ACS patients differed from non-ACS patients across most measures (Table 1). For example, ACS patients were older compared to non-ACS patients (mean age 60.8 vs. 56.3 years, respectively, p<0.001). ACS vs. non-ACS patients were more often male (47.1% vs. 39.6%, respectively, p<0.001), white (73.5% vs. 67.4%, respectively, p<0.001), and had a higher mean number of comorbidities (2+ comorbidities: 59.5% vs. 52.7%, respectively, p<0.001).
Overall outcomes were worse for ACS patients. ACS patients had higher rates of mortality compared to non-ACS patients (2.4% vs. 2.1%, respectively, p<0.001). ACS patients also had longer lengths of stay vs. non-ACS patients (5.9 vs. 4.5 days, respectively, p<0.001) and higher rates of discharge to rehabilitation (23.4% vs. 14.7%, respectively, p<0.001).
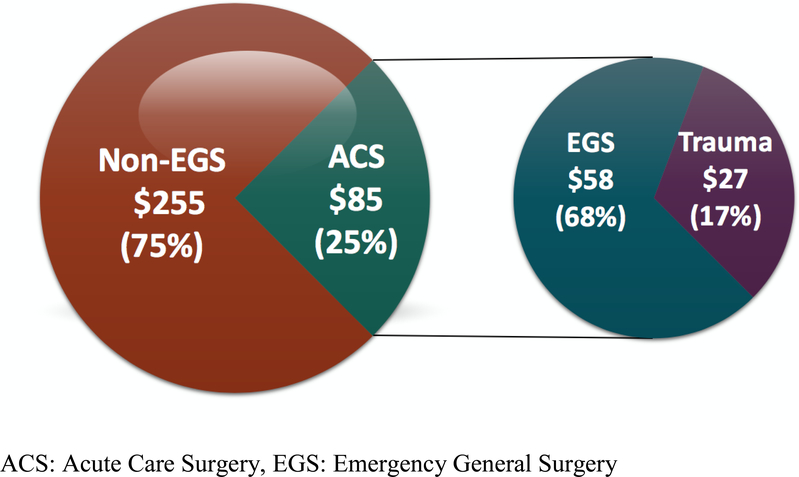
Together, ACS patients accounted for $85.8 billion dollars, or 25.2% of total adult U.S. inpatient costs for 2014 ($341 billion) (Figure 1). Of ACS patients, EGS diagnoses accounted for $56.8 billion (66.2%), whereas $29.0 billion (33.8%) were associated with trauma. Mean costs for ACS patients were overall higher ($14,466) than for non-ACS inpatients ($10,951, p<0.001). Patient factors associated with higher costs in regression for ACS patients included increasing age and increasing income (Table 2). When controlling for known confounders, EGS patients were less expensive than trauma patients by approximately $2,000. Average costs and frequency of EGS conditions are described in Table 3.
Figure 1.
ACS Burden and Total Costs, in Billions of Dollars, 2014
Table 2.
Linear Random Mixed Effects Regression to Predict Cost, Based on Any ACS Diagnosis
| Coefficient ($) | p value | 95% CI | |||
|---|---|---|---|---|---|
| Low ($) | High ($) | ||||
| Base Cost ($) | 3,374 | ||||
| Age Category | |||||
| 18–24 years | -reference- | ||||
| 25–34 years | 261 | =0.03 | 20 | 502 | |
| 35–44 years | 875 | <0.001 | 640 | 1,110 | |
| 45–54 years | 2,623 | <0.001 | 2,399 | 2,846 | |
| 55–64 years | 4,170 | <0.001 | 3,948 | 4,391 | |
| 65–74 years | 3,995 | <0.001 | 3,755 | 4,235 | |
| 75–84 years | 3,247 | <0.001 | 3,001 | 3,491 | |
| 85 and older | 1,876 | <0.001 | 1,622 | 2,129 | |
| Payer Status | |||||
| Medicare | -reference- | ||||
| Medicaid | 1,146 | <0.001 | 994 | 1,298 | |
| Private insurance | −1,710 | <0.001 | −1,835 | −1,585 | |
| Self-pay | −2,460 | <0.001 | −2,658 | −2,261 | |
| Race and ethnicity | |||||
| White | -reference- | ||||
| Black | 1,981 | <0.001 | 1,852 | 2,109 | |
| Hispanic | 967 | <0.001 | 832 | 1,383 | |
| Zip Income Quartile | |||||
| 0–25th percentile | -reference- | ||||
| 25–50th percentile | 251 | <0.001 | 145 | 357 | |
| 50–75th percentile | 1,039 | <0.001 | 927 | 1,152 | |
| 75–100th percentile | 1,869 | <0.001 | 1,750 | 1,988 | |
| Had Major OR procedure | 12,284 | <0.001 | 12,201 | 12,368 | |
| Type of ACS Diagnosis | |||||
| Any Diagnosis of Trauma | -reference- | ||||
| Any Diagnosis of EGS | −1,976 | <0.001 | −2,085 | −1,867 | |
| Hospital Location | |||||
| Rural | reference- | ||||
| Urban | 1,856 | <0.001 | 1,658 | 1,923 | |
| Hospital Region | |||||
| Northeast | reference- | ||||
| Midwest | 1,045 | =0.07 | 986 | 1,265 | |
| South | 865 | =0.19 | 756 | 988 | |
| West | 1,118 | =0.06 | 1,045 | 1,256 | |
ACS: Acute Care Surgery; EGS: Emergency General Surgery, LOS: length of stay; SNF: skilled nursing facility
Table 3.
Common Inpatient EGS conditions and Mean Costs, 2014
| EGS Condition | Frequency (number, %) | Mean Costs ($) (SD) |
|---|---|---|
| Skin and Soft Tissue Infection | 539,149 (24%) | 7,299 (28) |
| Intestinal Obstruction | 272,886 (12%) | 11,335 (67) |
| Pancreatitis | 268,029 (12%) | 9,434 (68) |
| Diverticulitis | 214,600 (10%) | 10,264 (118) |
| Cholecystitis | 210,626 (10%) | 12,272 (45) |
| Hernia | 165,365 (7%) | 14,400 (86) |
| Appendicitis | 137,768 (6%) | 10,451 (45) |
| Surgical Site Infection | 136,001 (6%) | 13,354 (121) |
| Infectious Colitis | 102,884 (5%) | 9,293 (73) |
| Intestinal Ischemia | 47,247 (2%) | 13,830 (209) |
| Esophageal Perforation | 26,715 (1%) | 11,449 (239) |
| Pelvic Inflammatory Disease | 26,710 (1%) | 8,276 (196) |
| Perirectal Abscess | 21,637 (1%) | 8,064 (145) |
| Perforated Ulcer | 13,688 (1%) | 22,997 (439) |
| Breast Infection | 13,468 (1%) | 6,014 (111) |
| Pleural Space Infection | 11,039 (1%) | 26,700 (500) |
Of all adult inpatients, approximately 8.5 million (29.2%) underwent an operative procedure. Approximately 27% of these were patients who had an ACS diagnosis. When considering the rate of operative procedures for ACS vs. non-ACS conditions, there was a significant difference. Approximately 38.2% (2.3 million) ACS patients underwent an operative procedure, compared to 26.9% of non-ACS patients (6.3 million, p<0.001). There were notable differences between ACS and non-ACS patients who underwent surgery. Findings paralleled those that were observed for the overall ACS and non-ACS populations. ACS surgical patients vs. non-ACS surgical patients were older (59.0 vs. 54.8 years, respectively p<0.001), more often male (46.6% vs. 38.3%, respectively, p<0.001), and had a greater number of pre-existing comorbidities (2+ comorbidities: 63.4% vs. 56.9%, respectively, p<0.001). Operative patients with an ACS diagnosis also had worse outcomes than non-ACS surgical patients. They had higher mortality (2.1% vs. 1.1%, respectively, p<0.001), longer mean LOS (7.1 vs. 4.5 days, respectively, p<0.001), fewer routine discharges home (53.7% vs. 68.4%, respectively, p<0.001). Mean costs for ACS patients undergoing surgery were also higher than for non-ACS surgical patients ($22,094 vs. $18,673, p<0.001). Multivariate linear regression controlling for patient factors revealed that ACS patients undergoing an operative procedure cost approximately $12,285 more compared to their non-surgical ACS counterparts (95% CI: $12,201-$12,368, p<0.001).
We compared the EGS population to the trauma population. EGS patients were on average younger than trauma patients (59.5 vs. 64.3 years, respectively, p<0.001), but had a greater number of comorbidities (2+ comorbidities: 65.3% vs. 57.6%, respectively, p<0.001). Healthcare utilization was lower for EGS patients, with shorter lengths of stay compared to trauma patients (5.4 days vs. 6.1, p<0.001) and EGS patients were more routinely discharged home (63.5% vs. 39.9%, respectively p<0.001). EGS patients also underwent operative intervention less frequently than their trauma counterparts (34.7% vs. 47.1%, p<0.001).
Finally, we determined the mix of hospitals caring for ACS patients throughout the U.S. Overall, 3,186 (69.6%) of U.S. hospitals treated patients with both EGS and trauma diagnoses. To determine the ACS burden for hospitals, we compared the proportion of ACS patients in each hospital to its total population. The median percent of ACS to all inpatients within these centers was 21% with an interquartile range of 18%−24%. ACS-treating hospitals were compared to hospitals that did not treat any ACS patients. Their healthcare utilization differed significantly, with longer mean LOS in ACS-treating hospitals (vs. non-ACS hospitals: 5.3 days vs. 4.4 days, p<0.001) and higher rates of non-routine discharge (42.1% vs. 39.3%, p<0.001). ACS-treating hospitals were more frequently located in the East North Central states of Wisconsin, Michigan, Illinois, Indiana and Ohio (16.2% vs. 8.2%, p<0.001) as well as the South Atlantic states including Maryland, District of Columbia, Virginia and the Carolinas (37.8% vs. 32.0%, p<0.001) compared to hospitals that did not treat ACS patients. They were also more often situated within urban environments at teaching facilities (37.4% vs. 11.8%, p<0.001), and were of large bed size (vs. other hospitals: 32.2% vs. 6.6%).
Discussion:
Of the 29.2 million adult hospitalized patients in 2014, patients with an ACS diagnosis comprised 20%. Costs associated with ACS diagnoses are even larger, at $85.8 billion, or 25% of annual U.S. inpatient costs. Furthermore, these estimates are likely an under-estimate as we could not ascertain surgical critical care costs in this database. These numbers are comparable to those for conditions that receive substantial attention. In 2015, approximately 7.5 million patients were estimated to have a diagnosis of stroke, with costs of care estimated to be approximately $34 billion.11 Similarly, roughly $87.8 billion was spent in 2014 on cancer-related health care. The cost and burden of ACS diseases confirm our initial hypothesis that ACS conditions comprise a significant proportion of U.S. healthcare utilization and costs. These findings highlight both the critical importance of the specialty as well as an opportunity for ACS providers to have substantial impact on US healthcare costs. An extension of this concept is the ability of surgeons to influence the national discussion on healthcare policy and funding.
Not surprisingly to those who care for these patients, ACS patients are sicker when compared to non-ACS hospitalized patients. ACS patients, on average, present with a greater number of comorbidities, are older, and experience higher rates of inpatient mortality. These findings are consistent with Gale et. al. who found that EGS patients are medically complex, with a mean age around 60 years and with multiple comorbidities.7 The result of the higher acuity and more frequent comorbid conditions result in higher average costs for ACS patients. Therefore, in addition to the large “footprint” for admissions and costs, ACS patients may provide opportunities for cost reduction. Cost reduction efforts might occur through efficiencies in care, but also potentially through the prevention of emergent surgical presentations.
Since the operating room is a large driver for costs, we compared ACS surgical patients to non-ACS surgical patients. ACS surgical patients comprise nearly 30% of all adult surgical inpatients within the United States. Similar to costs for the general ACS population, ACS patients undergoing surgery have high costs of care when compared with ACS non-surgical patients ($22,094 vs. $18,673, p<0.001). This is consistent with the findings of Ogola et. al. that major operative procedures are an important predictor of many high-cost hospitalizations.12 ACS patients who underwent surgery stay in the hospital for 2.6 days longer. In addition to patient factors and severity of illness, other drivers for increased length of stay may include lack of dedicated operating theater time for ACS cases, as compared to elective cases. A recent study by Wang et. al. demonstrated that prolonged time to operation was a significant driver of cost and LOS in their acute surgical unit, whereby patients on average spent almost half of their hospitalization waiting for surgery.13 These delays add significantly to costs, utilization and ultimately place our sickest surgical patients at risk for further deterioration due to prolonged surgical wait-times. It is possible that one opportunity to impact these costs may therefore be to address delays that are unevenly experienced by the ACS population. For example, twenty-four hour access to dedicated emergency operating rooms, as well as readily available acute care surgeons has been associated with cost reductions and improved outcomes in multiple studies reviewing ACS practices.2,14,15–17. In order to ensure the success of these efforts, appropriate funding, resources and hospital cultural acceptance need to be channeled into streamlining the efficiency of ACS services.
Another finding from our study is that there is variability in the “footprint” of ACS in different hospitals across the country. Hospitals treating ACS patients likely experience greater healthcare utilization given that they treat overall sicker surgical populations, in large hospitals and in urban locations (including both teaching or non-teaching). Although there were certain areas where the percent of ACS hospitals was higher than that of non-ACS hospitals, it is unlikely that the burden of ACS diseases is truly confined by geographic regions. Our findings suggest that access to ACS services were present throughout the U.S., albeit somewhat more limited in certain areas of the country. Given the significant and growing burden of ACS-related diseases, efforts to continue to expand the presence of hospital and providers delivering ACS specialized services will further streamline care for these sick patients.
There are several limitations to this study. The analysis is constrained by the fact it is a retrospective nationally representative administrative database. While NIS provides a valuable overview of the demographic characteristics, and healthcare utilization patterns of ACS patients, NIS does not provide granular clinical data nor trauma-specific information such as trauma center status or mechanism of injury. NIS also lacks provider-level information, and therefore we were unable to ascertain the specialty of surgeons providing care and whether they were acute care surgery trained. All trauma-related information (injuries and injury severity) was derived from ICD-9-CM codes, converted using the ICDPIC tool. Furthermore, while more than 16 EGS diagnoses exist, we chose to limit our sample to those for which a standardized classification and grading system by the AAST exists, in order to more accurately clarify the EGS burden. There are likely other populations for which ACS-practicing surgeons provide care. Again, this would result in an under-estimate. Similarly, we did not include costs associated with the provision of surgical critical care services by ACS surgeons. This is due to the fact that critical care services are a subset of the study population already, and that critical care services provided for other patient populations but cared for by critical-care boarded surgeons would be hard to identify (e.g. an ACS surgeon caring for a liver transplant patient in the ICU). Finally, the NIS uniquely captures data associated with inpatient hospitalizations. Consequently, we were not able to extrapolate upon outpatient costs of ACS care, the burden of long-term disability, nor the out-of-hospital mortality rate (i.e. for patients who never survived to be admitted to hospital, or those who later died after discharge). We also suspect that many patients presenting with certain EGS conditions such as appendicitis and cholecystitis, were likely operated upon and discharged within the same day, thereby not being counted within our inpatient sample. Given the variety of practice models covering EGS and trauma patients, our findings simply provide a national snapshot of the scope of ACS care. We hope that the findings from this study spur follow-up analyses with more robust clinical data are required from trauma registries and possibly nascent EGS registries to help delineate the ACS burden in more detail.
Conclusion:
Acute care surgery patients comprise 20% of the inpatient population, but 25% of total inpatient costs in the U.S. In addition to being costly, they overall have higher healthcare utilization and worse outcomes. This suggests there is an opportunity to improve clinical trajectory for ACS patients that in turn, can affect the overall U.S. healthcare costs. As EGS comprises 70%−80% of ACS activities and 70% of ACS costs, the greatest impact may lie in improvements in care for the EGS population.
Acknowledgments
Disclosure of Funding: Dr. Staudenmayer is currently receiving a grant (1K08AG04442801A1) from the National Institute of Health.
Footnotes
There are no conflicts of interest to report for any of the authors.
This manuscript will be presented as a podium oral presentation at the 77th Annual Meeting of the American Association for the Surgery of Trauma; September 26–29, 2018 in San Diego, CA.
Level of evidence: Epidemiologic, level III
References:
- 1.Mok JM, Martinez M, Smith HE, Sciubba DM, Passias PG, Schoenfeld A, Isaacs RE, Vaccaro AR, Radcliff KE, Assoication for Collaborative Spine Research Investigators. Impact of a Bundled Payment System on Resource Utilization During Spine Surgery. Int J Spine Surg. 2016;10:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chana P, Burns EM, Arora S, Darzi AW, Faiz OD. A Systematic Review of the Impact of Dedicated Emergency Surgical Services on Patient Outcomes. Ann Surg. 2016;263(1):20–27. [DOI] [PubMed] [Google Scholar]
- 3.Sorelli PG, El-Masry NS, Dawson PM, Theodorou NA. The dedicated emergency surgeon: towards consultant-based acute surgical admissions. Ann R Coll Surg Engl. 2008;90(2):104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tisherman SA, Kaplan L, Gracias VH, Beilman GJ, Toevs C, Byrnes MC, Coopersmith CM, Surgery Section Society of Critical Care Medicine. Providing care for critically ill surgical patients: challenges and recommendations. JAMA Surg. 2013;148(7):669–674. [DOI] [PubMed] [Google Scholar]
- 5.Olufajo OA, Cooper Z, Yorkgitis BK, Najjar PA, Metcalfe D, Havens JM, Askari R, Brat GA, Haider AH, Salim A. The truth about trauma readmissions. Am J Surg. 2016;211(4):649–655. [DOI] [PubMed] [Google Scholar]
- 6.Ogola GO, Gale SC, Haider A, Shafi S. The financial burden of emergency general surgery: National estimates 2010 to 2060. J Trauma Acute Care Surg. 2015;79(3):444–448. [DOI] [PubMed] [Google Scholar]
- 7.Gale SC, Shafi S, Dombrovskiy VY, Arumugam D, Crystal JS. The public health burden of emergency general surgery in the United States: A 10-year analysis of the Nationwide Inpatient Sample−−2001 to 2010. J Trauma Acute Care Surg. 2014;77(2):202–208. [DOI] [PubMed] [Google Scholar]
- 8.Utter GH, Miller PR, Mowery NT, Tominaga GT, Gunter O, Osler TM, Ciesla DJ, Agarwal SK Jr, Inaba K, Aboutanos MB, Brown CV, Ross SE, Crandall ML, Shafi S. ICD-9-CM and ICD-10-CM mapping of the AAST Emergency General Surgery disease severity grading systems: Conceptual approach, limitations, and recommendations for the future. J Trauma Acute Care Surg. 2015;78(5):1059–1065. [DOI] [PubMed] [Google Scholar]
- 9.Healthcare Cost and Utilization Project. Cost-to-Charge Ratio Files. https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed August 12, 2018.
- 10.Healthcare Cost and Utilization Project. Major operating room ICD-9-CM procedure indicator. 2014; https://www.hcup-us.ahrq.gov/db/vars/sedddistnote.jsp?var=orproc. Accessed August 10, 2018.
- 11.Center for Disease Control. Stroke Facts. 2017; https://www.cdc.gov/stroke/facts.htm. Accessed August 22, 2018.
- 12.Ogola GO, Shafi S. Cost of specific emergency general surgery diseases and factors associated with high-cost patients. J Trauma Acute Care Surg. 2016;80(2):265–271. [DOI] [PubMed] [Google Scholar]
- 13.Wang E, Jootun R, Foster A. Management of acute appendicitis in an acute surgical unit: a cost analysis. ANZ J Surg. 2018. [DOI] [PubMed] [Google Scholar]
- 14.Dultz LA, Pachter HL, Simon R. In-house trauma attendings: a new financial benefit for hospitals. J Trauma. 2010;68(5):1032–1037. [DOI] [PubMed] [Google Scholar]
- 15.Williams TE Jr., Satiani B, Thomas A, Ellison EC. The impending shortage and the estimated cost of training the future surgical workforce. Ann Surg. 2009;250(4):590–597. [DOI] [PubMed] [Google Scholar]
- 16.Hutter MM. Specialization: the answer or the problem? Ann Surg. 2009;249(5):717–718. [DOI] [PubMed] [Google Scholar]
- 17.Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. J Am Coll Surg. 2008;206(5):782–788; discussion 788–789. [DOI] [PubMed] [Google Scholar]