Abstract
Background:
There is growing interest in utilizing community pharmacies to support opioid abuse prevention and addiction treatment efforts. However, it is unknown whether the placement of community pharmacies is conducive to taking on such a role.
Objective:
To examine the distribution of community pharmacies in Wisconsin and its relationship with the location of addiction treatment facilities and opioid-related overdose events in rural and urban areas.
Methods:
The total number of opioid-related overdose deaths and crude death rates per 100,000 population were determined for each county in Wisconsin. Substance abuse treatment facilities were identified in each county to estimate access to formal addiction treatment. A list of pharmacies in the state was screened to identify community pharmacies in each county. Descriptive statistics and Pearson correlation coefficients were used to describe the distribution of and relationships between county-level opioid-related overdose death rates and the number of treatment facilities and community pharmacies in the state.
Results:
Wisconsin has 72 counties, of which 45 (62.5%) are classified as rural. Although the number of opioid-related overdose deaths was highly concentrated in urban areas, crude death rates per 100,000 population were similar in urban and rural areas. Rural counties were significantly less likely to have formal substance abuse treatment facilities (r = −.42, P = .00) or community pharmacies (r = −.44, P = .00) compared to urban counties. However, community pharmacies were more prevalent and more likely to be located in rural counties with higher rates of opioid-related overdose deaths than substance abuse treatment facilities. All but 1 of the 14 counties without a formal substance abuse treatment facility had access to 1 or more community pharmacies.
Conclusions:
Community pharmacies are ideally located in areas that could be used to support medication-assisted addiction treatment efforts, particularly in rural areas lacking formal substance abuse treatment facilities.
Keywords: Access to care, Drug abuse, Pharmacy, Policy, Rural
1. Introduction
There has been a significant increase in the misuse and abuse of both illicit and prescription opioids, leading to rapid increases in drug overdoses and death rates.1,2 Rural areas have been hit particularly hard by the opioid epidemic.3–5 Rural residents face challenges due to the lack of access to addiction treatment, an inadequate mental health workforce, and long travel times to access addiction treatment, leading to higher treatment costs.6–8 While telehealth has shown promise as an alternative, cost-effective care option for individuals living in rural or remote areas,6 there remain unmet personnel needs to supplement telehealth services for addiction treatment, particularly when it comes to medication-assisted treatment of opioid use disorders.
Community pharmacies are an integral part of the rural health care system, as they are often the only formal access point for health care in smaller rural communities.9 Pharmacies are increasingly taking on community and public health roles related to the opioid epidemic, such as creating prescription medication take-back programs to support safe medication disposal, and patient education in areas such as pain management, mental health, and substance abuse.10,11 Although current assessments of pharmacy’s role in reducing opioid-related morbidity and mortality have focused on the use and impact of prescription drug monitoring programs,12–15 there is a growing movement to involve pharmacies in other public health activities such as naloxone dispensing and opioid safety counseling.16–21 All states now have naloxone access laws that confer pharmacists with greater authority to independently dispense naloxone,22,23 and a growing number of states also allow pharmacists to engage in more clinical-oriented services such as the administration of long-acting injectable drugs to treat opioid addiction.24,25 A recent literature review of primary care models for treating opioid use disorders found that pharmacists working as clinical care managers was a key design factors among successful programs.26
Since nearly 93% of US residents live within 5 miles of a pharmacy,27 this may provide an opportunity for community pharmacies to support formal opioid abuse prevention and addiction treatment efforts, particularly in rural areas. However, it is unknown whether the placement of community pharmacies is conducive to taking on such a role. Therefore, the overall goal of this descriptive study was to examine the distribution of community pharmacies in Wisconsin and its relationship with the location of addiction treatment facilities and opioid-related overdose events in rural and urban areas. Data from the state of Wisconsin were used, as opioid-related overdose deaths are the leading cause of injury deaths in the state, and have more than tripled from 194 deaths in 2003 to 622 deaths in 201 4.28 In addition, over one-quarter of the population lives in a rural area. The information from this study will be useful to identify areas of unmet need for substance abuse treatment as well as potential opportunities to utilize community pharmacies as access points to support opioid abuse prevention and treatment efforts.
2. Methods
2.1. Data sources
County-level data for all opioid-related overdose deaths were obtained from the Wisconsin Department of Health Services for the year 2015, which was the most current and complete dataset available. The data included opioid-related overdose deaths identified by an ICD-10 code indicating drug poisoning as an underlying cause of death (X40-X44, X60-X64, X85, or Y10-Y14) and any of the following contributing cause of death codes: T400 (opium), T401 (heroin), T402 (natural and semisynthetic opioid), T403 (methadone), T404 (synthetic opioid other than methadone), or T406 (other and unspecified narcotic).29 These data included the total number of deaths and crude death rates, which were calculated by dividing the total number of deaths in a county by the total population in the county and were defined as the death rate per 100,000 population. Each county was classified as rural or urban based on the 2013 Rural-Urban Continuum Codes obtained from the United States Department of Agriculture website.30
A list of all addiction treatment facilities in the state was obtained from the Substance Abuse and Mental Health Services Administration (SAMHSA) website’s behavioral health treatment services locator.31 Available information included facility name, location, websites, and services provided. Only facilities classified as substance abuse treatment facilities (n = 199) by SAMHSA were included in the analysis.
A list of all pharmacies in the state was obtained from the Wisconsin Department of Safety and Professional Services. These data provide detailed information on the name and location of pharmacies licensed in the state of Wisconsin. Only pharmacies with active, in-state licenses were included in the evaluation. Information on CVS pharmacies was obtained using their website as they were not included in the original data file. A total of 1179 pharmacies in the state were identified and labeled by county using the registered 5-digit zip-code. Each pharmacy location was then manually screened by the study team to identify community pharmacy locations by name recognition, looking up pharmacies on the internet, and/or confirming the type of pharmacy by phone.32,33 Community pharmacies included independent, chain, clinic, hospital outpatient, and health maintenance organization pharmacies. Excluded pharmacy practice settings included hospital in-patient pharmacies, long term care pharmacies, and veterinary pharmacies.
2.2. Analysis
ArcGIS version 10.5 software was used to map and identify trends across counties regarding opioid-related overdose deaths, the locations of substance abuse treatment facilities, and community pharmacies in the state of Wisconsin using an approach similar to Burrell et al. (2017).16 Maps were constructed with the use of graduated quintile breaks of opioid-related overdose death rates per 100,000 population by county as the base layer, and were overlaid with the geocoded locations of substance abuse treatment facilities and community pharmacies.34
Descriptive statistics and Pearson correlation coefficients were used to describe the distribution of and relationships between county-level opioid-related overdose death rates and the number of treatment facilities and community pharmacies in the state. Areas of interest included counties with high death rates and counties with limited access to formal addiction treatment. These analyses were conducted using Stata version 15.1. This study was considered exempt by the University of Wisconsin-Madison Institutional Review Board.
3. Results
Wisconsin has 72 counties, of which 27 (37.5%) are classified as urban and 45 (62.5%) as rural. A total of 611 opioid-related overdose deaths were reported in Wisconsin in 2015; however, the distribution of these deaths at the county level was highly skewed towards urban counties (Table 1). The number of opioid-related overdose deaths per county ranged from 0 to 218, with a median of 1 death per county; approximately 25% of counties had 0 deaths, 25% had 1 death, and 50% had 2 or more deaths. The crude death rates were more consistent across counties, ranging from 0 to 23 deaths per 100,000 population, with a median of 5 deaths per 100,000. A strong relationship was seen between population size and the number of opioid-related overdose deaths, such that the highest population counties had the largest number of deaths (r = .94, P = .00) (Table 2). However, when deaths were evaluated as crude death rates per 100,000 population, this relationship was attenuated (r = .38, P = .00). Although a weak negative relationship was seen between rural status and the number of opioid-related overdose deaths (r = –.32, P = .01), urban and rural counties had similar rates of opioid-related overdose deaths (r = – .20, P = .10).
Table 1.
County-level distribution of opioid-related overdose deaths, substance abuse treatment facilities, and community pharmacies in Wisconsin.
| All Wisconsin Counties (n = 72) | |||
|---|---|---|---|
| County Median | County Range | Statewide Total | |
| Population | 41,384 | 4232–947,735 | 5,686,986 |
| Opioid-Related Overdose Deaths | 1 | 0–218 | 611 |
| Opioid-Related Overdose Death Ratea | 5 | 0–23 | 11 |
| Substance Abuse Treatment Facilities | 2 | 0–29 | 199 |
| Community Pharmacies | 6 | 0–152 | 941 |
| Urban Counties (n = 27) | |||
| County Median | County Range | Urban Total | |
| Population | 101,633 | 20,574–947,735 | 4,267,683 |
| Opioid-Related Overdose Deaths | 7 | 0–218 | 526 |
| Opioid-Related Overdose Death Ratea | 7 | 0–23 | 12 |
| Substance Abuse Treatment Facilities | 3 | 0–29 | 135 |
| Community Pharmacies | 16 | 3–152 | 692 |
| Rural Counties (n = 45) | |||
| County Median | County Range | Rural Total | |
| Population | 21,430 | 4232–102,228 | 1,419,303 |
| Opioid-Related Overdose Deaths | 1 | 0–15 | 85 |
| Opioid-Related Overdose Death Ratea | 4 | 0–23 | 6 |
| Substance Abuse Treatment Facilities | 1 | 0–6 | 64 |
| Community Pharmacies | 4 | 0–16 | 249 |
Crude death rates were calculated by dividing the total number of deaths in a county by the total population in the county and were defined as the death rate per 100,000 population.
Table 2.
Correlations between study variables.
| All Wisconsin Counties (n = 72) | ||||||
|---|---|---|---|---|---|---|
| Population | Rural | Opioid-Related Overdose Deaths | Opioid-Related Overdose Death Rate | Substance Abuse Treatment Facilities | Community Pharmacies | |
| Population | 1.00 | |||||
| Rural | −.47* | 1.00 | ||||
| Opioid-Related Overdose Deaths | .94* | −.32* | 1.00 | |||
| Opioid-Related Overdose Death Rate | .38- | −.20 | .44* | 1.00 | ||
| Substance Abuse Treatment Facilities | .94* | −.42* | .89* | .38* | 1.00 | |
| Community Pharmacies | .99* | −.44* | .91* | .36* | .94* | 1.00 |
| Urban Counties (n = 27) | ||||||
| Population | Opioid-Related Overdose Deaths | Opioid-Related Overdose Death Rate | Substance Abuse Treatment Facilities | Community Pharmacies | ||
| Population | 1.00 | |||||
| Opioid-Related Overdose Deaths | .95* | 1.00 | ||||
| Opioid-Related Overdose Death Rate | .61* | .67* | 1.00 | |||
| Substance Abuse Treatment Facilities | .97* | .92* | .58* | 1.00 | ||
| Community Pharmacies | .99* | .91* | .58* | .97* | 1.00 | |
| Rural Counties (n = 45) | ||||||
| Population | Opioid-Related Overdose Deaths | Opioid-Related Overdose Death Rate | Substance Abuse Treatment Facilities | Community Pharmacies | ||
| Population | 1.00 | |||||
| Opioid-Related Overdose Deaths | .71* | 1.00 | ||||
| Opioid-Related Overdose Death Rate | .08 | .58* | 1.00 | |||
| Substance Abuse Treatment Facilities | .36* | .37* | .13 | 1.00 | ||
| Community Pharmacies | .91* | .61* | .05 | .39* | 1.00 | |
significant at p < .05.
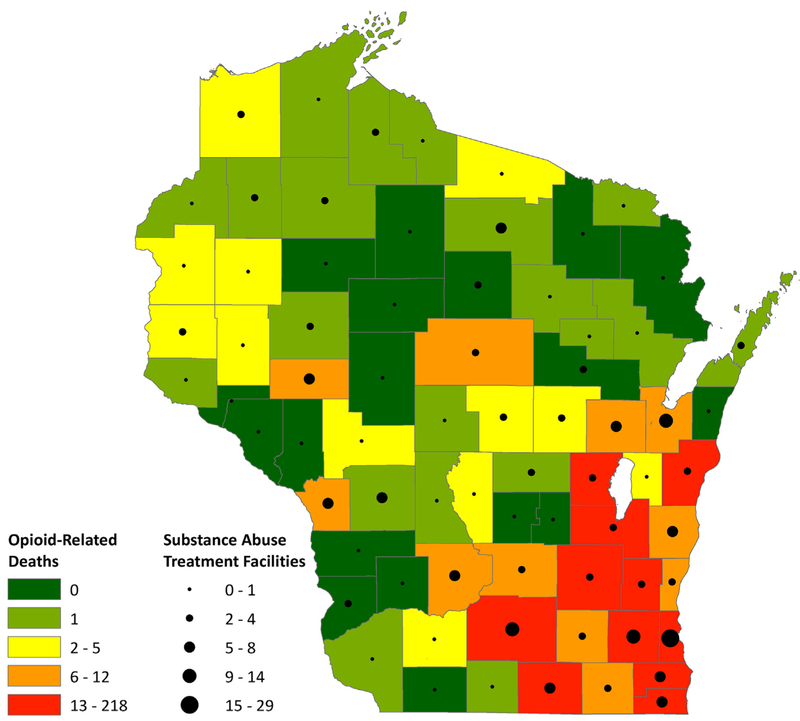
A total of 199 substance abuse treatment facilities were identified in Wisconsin, ranging from 0 to 29 per county, with a median of 2 per county (Table 1, Fig. 1). Approximately 20% of counties (n = 14) had 0 facilities, 50% had 1–2 facilities, and 30% had 3 or more facilities. A strong relationship was also seen between population size and the number of substance abuse treatment facilities (r = .95, P = .00). In addition, rural counties were significantly less likely than urban counties to have formal substance abuse treatment facilities (r = – .42, P = .00), as approximately two-thirds of rural counties had either 0 or 1 facility.
Fig. 1.
GIS map of Wisconsin depicting drug-related overdose deaths and locations of substance abuse treatment facilities.
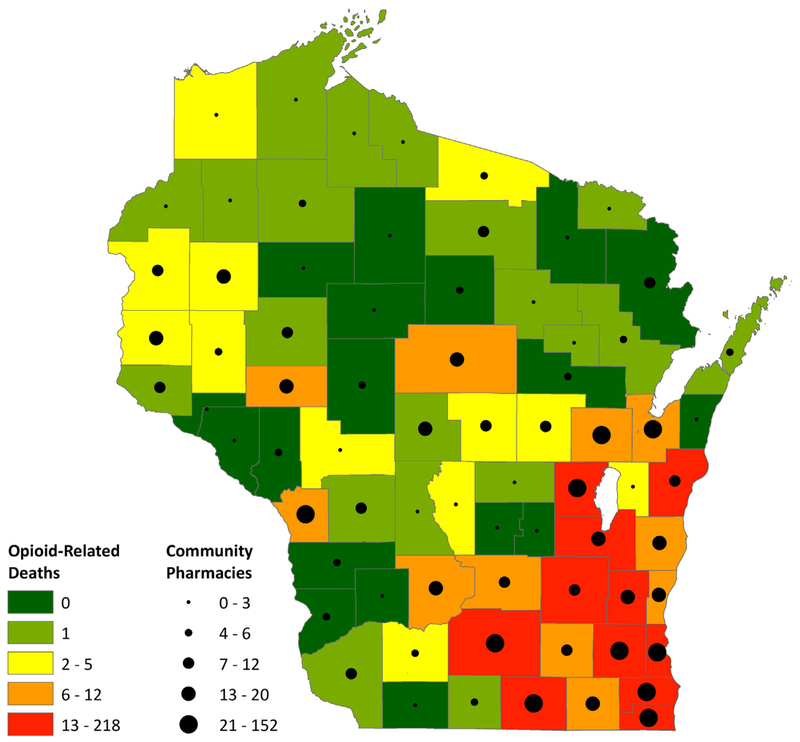
Of the 1179 pharmacies that in the state, 941 pharmacies (79.8%) were identified as community pharmacies. The number of community pharmacies per county ranged from 0 to 152 pharmacies, with a median of 6 pharmacies per county (Table 1, Fig. 2). About one-third of Wisconsin counties had 3 or fewer community pharmacies, one-third had 4–10 pharmacies, and one-third had greater than 10 pharmacies. However, the distribution of community pharmacies in the state was highly skewed towards counties with higher populations (r = .99, P = .00), with a median of 16 pharmacies per county in urban areas and 4 pharmacies per county in rural areas. Similar to the relationship seen for substance abuse treatment facilities, rural counties were significantly less likely to have community pharmacies (r = –.44, P = .00); however, all but 1 rural county (Florence county) had at least 1 community pharmacy.
Fig. 2.
GIS map of Wisconsin depicting drug-related overdose deaths and locations of community pharmacies.
Strong positive relationships were seen between county population size and the numbers of opioid-related overdose deaths, substance abuse treatment facilities, and community pharmacies (Table 2). In addition, there were strong positive relationships between the number of opioid-related overdose deaths with substance abuse treatment facilities (r = .89, P = .00) as well as with community pharmacies (r = .91, P = .00). These relationships were much smaller when death rates were used instead of the number of deaths (Table 2). In addition, there was a strong correlation between the location of treatment facilities and community pharmacies (r = .94, P = .00).
When the results were stratified by urban and rural location, slightly different patterns emerged. The relationships between these variables in urban areas were similar to those seen overall (Table 2). However, more variability was seen in rural areas. Although population size was strongly related to the number of opioid-related overdose deaths (r = .71, P = .00) and community pharmacies (r = .91, P = .00), it was only weakly associated with the number of substance abuse treatment facilities (r = .36, P = .02). In contrast to urban areas, the relationships seen between the number of opioid-related deaths, treatment facilities, and community pharmacies were much lower in rural areas (Table 2) Of particular note was that the strength of the relationship between opioid-related overdose deaths with community pharmacies was nearly twice as high as the relationship with treatment facilities (r = .61, P = .00 vs r = .37, P = .01), which indicates community pharmacies were more likely to be located in rural counties with higher rates of opioid-related overdose deaths than substance abuse treatment facilities. In addition, a low to moderate correlation between community pharmacies and treatment facilities (r = .39, P = .01) suggests differential access to these types of organizations in rural counties. These findings contrast with urban areas, where there were strong correlations of similar size between opioid-related overdose deaths, treatment facilities, and community pharmacies, which indicates similar placement of these organizations in urban counties. All but 1 of the 14 counties in Wisconsin without any substance abuse treatment facilities had at least 1 community pharmacy, which ranged from 0 to 12 pharmacies. Thus, 1 or more community pharmacies were commonly located in counties with limited access to formal addiction treatment facilities.
4. Discussion
Several rural Wisconsin counties have been disproportionately affected by deaths due to opioids,29 and there is limited access to addiction treatment facilities in many of these areas, which is not a problem unique to Wisconsin.7,8 While there is a growing interest in the utilization of telehealth services to address these gaps,6 this approach has a limited ability to address key aspects of medication-assisted treatment including the dispensing, administration, and monitoring of medications. This is particularly relevant as the US Food and Drug Administration has recently expressed interested in broadening access to medication-assisted treatment for opioid addiction.35
Although opioid-reported deaths were fairly rare at the county level, addiction treatment facilities may not always be located in the counties that have the most need of them, particularly in rural areas. Our findings suggest that community pharmacies may be ideally located in areas that could be used to support opioid treatment efforts in counties with limited or no access to formal addiction treatment facilities. All but 1 of the 14 Wisconsin counties lacking a formal substance abuse treatment facility had at least 1 community pharmacy, and often included multiple pharmacies. Utilizing community pharmacies in this way may enable rapid expansion and greater reach of addiction treatment efforts. In addition, this could help alleviate the significant challenges currently seen in rural areas with access and travel time to receive addiction treatment.5–8
Pharmacies are increasingly dispensing medications to treat opioid addiction and overdose, and such approaches have been proposed as promising ways to promote access to effective opioid use disorder treatment and further the integration of addiction treatment across the healthcare system.21 Although pharmacy organizations around the country have expressed interest in developing new pharmacy services centered on opioid misuse and addiction such as the administration of naltrexone injections, this practice remains relatively rare.24,36 Important barriers to pharmacist engagement in these activities may include state pharmacy practice laws, lack of provider recognition at the state or federal level, a lack of integrated support services and administrative support, and low reimbursement.7,25,37
4.1. Limitations
Only treatment facilities classified by SAMHSA as substance abuse treatment facilities were included in the analysis; other facilities (ie, mental health treatment facilities) are not included, even though some of these facilities may provide some substance abuse or opioid treatment services. However, this is likely not a major limitation as many facilities are classified as both substance abuse and mental health treatment facilities. Data on opioid-related overdose deaths is based on information provided on Wisconsin resident death certificates. Underreporting of deaths may have occurred due to the lack of specify of drug involvement on death certificates, as well as variations in diagnosis or reporting.2 In addition, caution should be used when comparing crude county-level death rates, as they do not take into account underlying differences in the age distribution of the population.
5. Conclusions
Community pharmacies are ideally located in areas that could be used to support medication-assisted addiction treatment efforts, particularly in rural areas lacking formal substance abuse treatment facilities. Utilizing community pharmacies to provide access to quality opioid addiction and overdose treatments may be a promising approach to rapidly expand addiction treatment in underserved areas.
Funding
This study was not funded by any agency or organization.
Footnotes
Disclosure
The authors report no conflicts of interest.
References
- 1.Centers for Disease Control and Prevention. Understanding the epidemic; drug overdose; CDC injury center. https://www.cdc.gov/drugoverdose/epidemic/index.html. Published January 19, 2018. Accessed September 21, 2017.
- 2.Ruhm CJ. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am J Prev Med. 2017;53(6):745–753. 10.1016/j.amepre.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Keyes KM, Cerdá M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Pυbl Health. 2014;104(2):e52–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villapiano NLG, Winkelman TNA, Kozhimannil KB, Davis MM, Patrick SW. Rural and urban differences in Neonatal Abstinence syndrome and maternal opioid use, 2004 to 2013. JAMA Pediatr. 2017;171(2):194–196. 10.1001/jamapediatrics.2016.3750. [DOI] [PubMed] [Google Scholar]
- 5.Chan Y-F, Lu S-E, Howe B, Tieben H, Hoeft T, Unützer J. Screening and follow-up monitoring for substance use in primary care: an exploration of rural-urban variations. J Gen Intern Med. 2016;31(2):215–222. 10.1007/s11606-015-3488-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services (HHS). Office of the Surgeon General. Facing Addiction in America: the Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: HHS; 2016. [PubMed] [Google Scholar]
- 7.Quest TL, Merrill JO, Roll J, Saxon AJ, Rosenblatt RA. Buprenorphine therapy for opioid addiction in rural Washington: the experience of the early adopters. J Opioid Manag. 2012;8(1):29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stein BD, Pacula RL, Gordon AJ, et al. Where is buprenorphine dispensed to treat opioid use Disorders? The role of private offices, opioid treatment programs, and substance abuse treatment facilities in urban and rural counties. Milbank Q. 2015;93(3):561–583. 10.1111/1468-0009.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ullrich F, Salako A, Mueller K. Issues confronting rural pharmacies after a decade of medicare Part D. Rural Policy Brief. 2017;3:1–5. [PubMed] [Google Scholar]
- 10.Strand MA, Tellers J, Patterson A, Ross A, Palombi L. The achievement of public health services in pharmacy practice: a literature review. Res Soc Adm Pharm. 2016;12(2):247–256. 10.1016/j.sapharm.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Scott DM, Strand M, Undem T, Anderson G, Clarens A, Liu X. Assessment of pharmacists’ delivery of public health services in rural and urban areas in Iowa and North Dakota. PharmPract 2016;14(4) 10.18549/PharmPract.2016.04.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fleming ML, Barner JC, Brown CM, Shepherd MD, Strassels S, Novak S. Using the theory of planned behavior to examine pharmacists’ intention to utilize a prescription drug monitoring program database. Res Soc Adm Pharm 2014;10(2):285–296. http://dx.doi.org/10.10167j.sapharm.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 13.Bao Y, Pan Y, Taylor A, et al. Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Aff. 2016;35(6):1045–1051. 10.1377/hlthaff.2015.1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yarbrough CR. Prescription drug monitoring programs produce a limited impact on painkiller prescribing in medicare Part D. Health Serv Res. 2017. 10.1111/1475-6773.12652 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Piper BJ, Desrosiers CE, Lipovsky JW, et al. Use and misuse of opioids in Maine: results from pharmacists, the prescription monitoring, and the diversion alert programs. J Stud Alcohol Drugs. 2016;77(4):556–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burrell A, Ethun L, Fawcett JA, et al. The pharmacist’s role in overdose: using mapping technologies to analyze naloxone and pharmacy distribution. J Am Pharm Assoc JAPhA. 2017;57(2):S73–S77. 10.1016/j.japh.2016.11.006e1. [DOI] [PubMed] [Google Scholar]
- 17.Carpenter J, Wong K, Ndje P, Ezeonyebuchi U. Opioid overdose and naloxone delivery devices in the community setting. Am J Pharm Benefits. 2016;8(6):e96–e100. [Google Scholar]
- 18.Bratberg J. Opioids, naloxone, and beyond: the intersection of medication safety, public health, and pharmacy. J Am Pharm Assoc JAPhA. 2003;57(2S):S5–S7. 10.1016/j.japh.2017.02.0062017. [DOI] [PubMed] [Google Scholar]
- 19.Hagemeier NE, Alamian A, Murawski MM, Pack RP. Factors associated with provision of addiction treatment information by community pharmacists. J Subst Abuse Treat. 2015;52:67–72. 10.1016/j.jsat.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Jones CM, Lurie PG, Compton WM. Increase in naloxone prescriptions dispensed in US retail pharmacies since 2013. AmJ Publ Health. 2016;106(4):689–690. 10.2105/AJPH.2016.303062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Compton WM, Jones CM, Stein JB, Wargo EM. Promising roles for pharmacists in addressing the U.S. opioid crisis. Res Soc Adm Pharm. December 2017. 10.1016/j.sapharm.2017.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis C, Carr D. State legal innovations to encourage naloxone dispensing. J Am PharmAssocJAPhA. 2017;57(2):S180–S184. 10.1016/j.japh.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 23.Roberts AW, Carpenter DM, Smith A, Look KA. Reviewing state-mandated training requirements for naloxone-dispensing pharmaacists. Res Soc Adm Pharm. 2018. 10.1016/j.sapharm.2018.04.002 [ePub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sonka J Our Lady of Peace opens pharmacist-operated injection clinic, dispensing long-acting drugs to treat opioid addiction. https://insiderlouisville.com/business/our-lady-of-peace-opens-pharmacist-operated-injection-clinic-dispensing-long-acting-drugs-to-treat-opioid-addiction/; March 2017, Accessed date: 27 November 2017.
- 25.Duvivier H, Gustafson S, Greutman M, et al. Indian Health Service pharmacists engaged in opioid safety initiatives and expanding access to naloxone. J Am Pharm Assoc JAPhA. 2017;57(2):S135–S140. 10.1016/j.japh.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 26.Lagisetty P, Klasa K, Bush C, Heisler M, Chopra V, Bohnert A. Primary care models for treating opioid use disorders: what actually works? A systematic review. PLoS One. 2017;12(10):e0186315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Association of Chain Drug Stores. Chain Pharmacy Industry Profile 2011–2012. Arlington, VA: NACDS; 2012. [Google Scholar]
- 28.State of Wisconsin Department of Health Services. Public Health Advisory. https://www.dhs.wisconsin.gov/opioids/opioid-public-health-advisory.pdf. Published September 21, 2017. Accessed February 28, 2018.
- 29.Wisconsin Department of Health Services Division of Public Health. Select Opioid-Related Morbidity and Mortality Data for Wisconsin. Wisconsin department of Health Services; 2017. https://www.dhs.wisconsin.gov/publications/p01690.pdf, Accessed date: 3 January 2018. [Google Scholar]
- 30.United States Department of Agriculture. Rural-Urban Continuum Codes. 2013; 2013 https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/, Accessed date: 8 June 2017.
- 31.Substance Abuse and Mental Health Services Administration. Behavioral Health Treatment Services Locator. https://findtreatment.samhsa.gov/. Accessed November 16, 2016.
- 32.Gadkari AS, Mott DA, Kreling DH, Bonnarens JK. Characteristics of unmet demand for pharmacists: a survey of rural community pharmacies in Wisconsin. J Am Pharm Assoc JAPhA. 2008;48(5):598–609. 10.1331/JAPhA.2008.07039. [DOI] [PubMed] [Google Scholar]
- 33.Arora P, Mott DA, Chui MA, Kreling DH. Assessing unmet and latent demand for pharmacists at the state level. Innov pharm. 2015;6(3)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909238/., Accessed date: 30 November 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Melnick A Introduction to geographic Information Systems in Public Health. Jones & Bartlett Learning; 2002. [Google Scholar]
- 35.Kounang N FDA Aims to Expand Access to Medication-assisted Treatment for Opioid Addiction. CNN. https://www.cnn.com/2018/02/26/health/medication-assisted-treatment-opioid-azar/index.html. Published February 26, 2018. Accessed February 26, 2018. [Google Scholar]
- 36.Yap D Rx drug abuse: pharmacists part of potential community solutions. Pharm Today. 2015;21(12):50–52. [Google Scholar]
- 37.Tommasello AC. Substance abuse and pharmacy practice: what the community pharmacist needs to know about drug abuse and dependence. Harm Reduct J. 2004;1:3 10.1186/1477-7517-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]