ABSTRACT
Afghanistan is one of the countries with the poorest maternal mortality ratio in the world. Inadequate utilization of antenatal care (ANC) services increases the risk of maternal mortality. This study aimed to identify the factors associated with ANC visits in Afghanistan. The dataset of the Afghanistan Demographic and Health Survey (AfDHS) 2015 were used for taking the socio-demographic factors, cultural factors, and the number of ANC visits. The subjects of this study were 18,790 women who had at least one live birth in the last five years, and 10,554 women (56.2%) had availed of at least one ANC visit. Most women were 20-29 years old (53.3%), poor (41.7%), had 2–4 children (43.9%), lived in rural areas (76.1%), and had no education (85.0%) or no job (86.7%). Most women answered that husbands made a decision about their healthcare and that getting permission from their husbands was a major challenge. Multivariate analysis showed that age, ethnicity, area of residence, parity, women’s education, husband’s education, literacy, having a job, wealth, the decision maker for healthcare, and difficulty in getting permission from the husband were significantly correlated with availing of the ANC visits. This study showed that not only the socio-demographic factors but also the cultural factors were associated with ANC visits. The Afghanistan government should improve the education programs at schools and healthcare facilities, for both men and women. To augment women’s propensity to take a decision, the programs for women’s empowerment need to be supported and extended across the country.
Key Words: Afghanistan, Afghanistan Demographic and Health Survey, antenatal care, women
INTRODUCTION
The maternal mortality ratio (MMR) was 216 per 100,000 live births in 2015 globally, which was decreased from 385 per 100,000 live births in 1990.1 However, the target for reduction of the global MMR, as part of the Sustainable Development Goals (SDGs), is 70 per 100,000 live births by 2030.2 The MMR in 2015 was 239 per 100,000 livebirths in the developing countries, while it was only 12 per 100,000 live births in developed countries.3 Approximately 830 women die due to pregnancy and childbirth-related causes every day in the world1 and 99% of maternal deaths occur in the developing countries.3 Direct causes such as postpartum hemorrhage, puerperal sepsis, pre-eclampsia and eclampsia, complications of delivery and unsafe abortions, account for approximately 73% of all maternal deaths. The other causes of maternal deaths are indirect causes such as malaria and tuberculosis.4
A study on the trend of maternal mortality in low and middle-income countries showed that low utilization of ANC services almost doubled the maternal mortality risk.5 Therefore, maternal healthcare, particularly ANC as the initial care can reduce pregnancy-related deaths and prevent complications.3 Globally, at least four ANC check-ups during pregnancy are conducted in the high-income countries, which is not the case in low-income countries. The coverage of at least four ANC was 46% in developing countries in 2000–2007.6 To reduce the maternal mortality, the World Health Organization (WHO) recommends eight ANC visits to detect disorders and complications, through frequent communication with the healthcare providers; the first visit during the first trimester, and two and five visits during the second and third trimesters, respectively.7
The primary survey in 2002 estimated the MMR in Afghanistan to be 1,600 deaths per 100,000 live births.8 Although another primary survey estimated the MMR to be 327 per 100,000 live births in 2010,9 this result was controversial.10 Finally, the Afghanistan Demographic and Health Survey (AfDHS) 2015 reported that the pregnancy related mortality ratio (all maternal deaths during pregnancy, child birth, or within two months after pregnancy) was 1,291 maternal deaths per 100,000 live births.11 Thus, the MMR in Afghanistan was revealed to be the poorest in the world.12 The factors related to high maternal mortality in Afghanistan were reported to be high birth rates, early childbearing and frequent pregnancies at close intervals.8 The total fertility rate was reported to be 5.3 by the AfDHS 2015, and was found to be more than twice the global average.8,11
Maternal deaths and the risk of mortality for mothers and babies during pregnancy and delivery, can be reduced by ANC provided by skilled healthcare workers.7,13 Some studies on maternal healthcare utilization in Afghanistan reported that ANC was a significant factor associated with complete immunization, child survival, delivery by skilled birth attendant, and institutional delivery.14-16 In Afghanistan, the maternal health care services can be availed for free at all public healthcare facilities and are provided by skilled healthcare staff including doctors, midwives, nurses, auxiliary midwives, and community health workers, although similar services at private healthcare facilities or through home visits, are chargeable to the patients.11,17 Previous studies reported that factors associated with utilization of ANC in Afghanistan were education, area of residence, knowledge of risk signs during pregnancy, media exposure, wealth status, transportation and healthcare personnel’s behavior with patients.18-22 Husband’s education, ethnicity, literacy, having or not having a job, husband’s permission for healthcare, and decision maker for women’s healthcare were reported to be significantly associated with ANC visits in the developing countries.23-29 However, there is no report about the association between these factors and ANC visits in Afghanistan.
This study aimed to identify factors that influenced the ANC visits in Afghanistan by secondary analysis of the data from the AfDHS 2015. The AfDHS 2015 was conducted through a joint collaboration between the United States Agency for International Development (USAID), Central Statistics Organization (CSO), Ministry of Public Health (MoPH), and ICF International Inc. to study and evaluate the demographic and health indicators.11
MATERIALS AND METHODS
The Afghanistan Demographic and Health Survey in 2015
The AfDHS 2015 implemented by MoPH and CSO in 2015, was the first standard demographic and health survey in Afghanistan. A stratified sampling two-step design was used. The first step was the selection of 950 out of 25,974 enumeration areas (EAs). The selected 950 EA consisted of 260 EA from the urban areas and 690 EA from the rural areas. EAs are dwelling units that serve as counting units for the census, which is conducted by the CSO. The second step was the selection of 27 households in each EA by an equal probability systematic selection process. A total of 25,650 households were selected. The target samples were all ever-married women and men aged 15 to 49 years, who were at their homes on the night before the survey, even if they were not permanent residents of the selected house or were visitors. The AfDHS 2015 was a national survey conducted throughout the country and collected recent information about marriage, fertility, awareness and use of family planning aids, nutrition, adult feeding practices, child feeding practices, childhood mortality, views about HIV/AIDS and other sexually transmitted infections (STIs), women’s empowerment, domestic violence, and other health problems such as tuberculosis, hepatitis B and C, cancer, and smoking. The data was collected from June 15 2015 to February 23 2016. The final report of the AfDHS 2015 was released on February 15 2017. The method of data collection was explained in detail in the report.11 The dataset of the AfDHS 2015 is available on the DHS program website as open access to the registered authors.
Study subjects
This is a cross-sectional study based on a secondary data analysis of the AfDHS 2015 focusing on ANC visits of expectant mothers. The subjects were women who had at least one live birth in the five years preceding the AfDHS 2015. Women who were not aware of ANC or those whose data was missing were excluded from the sample.
Study measure
To identify the factors associated with the utilization of ANC visits by women, the data of socio-economic factors, demographic factors, cultural factors, and the number of ANC visits were extracted from the dataset of the AfDHS 2015. Socio-economic factors included women’s education, husband’s education, literacy, job, and wealth status. Demographic factors included age, ethnicity, residence locality, and parity. Cultural factors included information about the decision maker for women’s healthcare and the difficulty or ease of getting permission from the husband to avail of healthcare services.
Statistical analysis
A descriptive statistical method was used to calculate the distribution and proportion of socio-economic and demographic variables. A logistic regression model was used to estimate the odds ratios (OR) of ANC and 95% confidence interval (CI). A p-value of less than 0.05 was considered as statistically significant. The analysis was performed using Statistical Package for Social Sciences (SPSS) version 24.0 (IBM SPSS Inc.).
Ethical considerations
The ethical approval for the AfDHS 2015 was secured from the Institutional Review Board (IBR) of MoPH, ICF international Inc. (DHS program), and CSO. The data obtained for this study were based on anonymous public use data with no identifiable information about the survey respondents. Therefore, no further ethical approval was obtained.
RESULTS
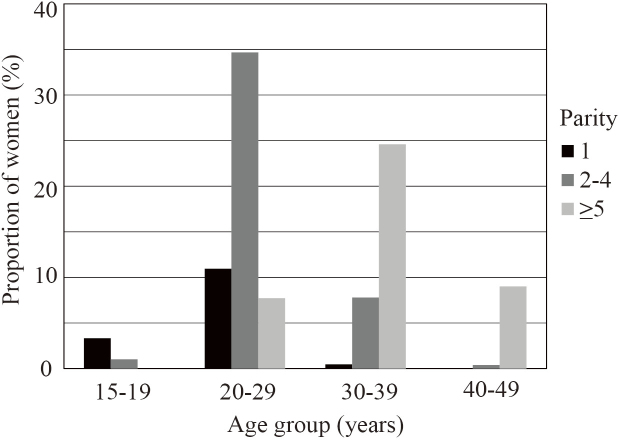
The total number of women who had at least one live birth in the last five years were 19,801. Among them, 409 (2.1%) women who were not aware whether they had availed of ANC and 602 (3%) women who did not answer all questions of the survey were excluded; thus, there were 18,790 women in the final analysis. The number of ANC visits availed of by the women during their last pregnancy is shown in Fig. 1. The results showed that 8,236 women (43.8%) did not avail of any ANC service. Among 10,554 women (56.2%) who undertook ANC visits, two ANC visits were most frequent (17.0%). Women who undertook four visits or more and eight visits or more were 16.5% and 1.8%, respectively (Fig. 1).
Fig. 1. Number of antenatal care visits during last pregnancy (N=18,790).
8,236 women (43.8%) did not use any antenatal care (ANC) service. Among 10,554 women (56.2%) who undertook ANC visits, two ANC visits were most frequent (17.0%). Women who undertook four visits or more and eight visits or more were 16.5% and 1.8%, respectively.
Table 1 shows the socio-economic and demographic background of the 18,790 women. The age group of 20–29 years (53.3%) was the highest, followed by 30–39 years (32.9%). Pashtun ethnicity (42.7%) was the majority, followed by Tajik ethnicity (30.0%). Those residing in the rural areas were 76.1%. Of the 18,790 women, 43.9% had 2–4 children and 41.3% had five children or more. In terms of education, 85.0% of the women had received no education, 13.4 % had received primary or secondary education, and 1.6% had received higher education. The percentage of illiterate women was similar to that with no education. Most women (86.7%) had no job. Utilizing ANC among the rich, middle, and poor women were 66.3%, 53.4%, and 48.9%, respectively.
Table 1. Socio-economic and demographic factors by antenatal care visits in women (n=18,790).
| Characteristics | ANC
(n=10,554) |
No ANC
(n=8,236) |
Total
(n=18,790) |
|||||
| n | % | n | % | n | % | |||
| Age (years) | ||||||||
| 15–19 | 448 | 4.2 | 373 | 4.5 | 821 | 4.4 | ||
| 20–29 | 5,732 | 54.3 | 4,291 | 52.1 | 10,023 | 53.3 | ||
| 30–39 | 3,449 | 32.7 | 2,724 | 33.1 | 6,173 | 32.9 | ||
| 40–49 | 925 | 8.8 | 848 | 10.3 | 1,773 | 9.4 | ||
| Ethnicity | ||||||||
| Pashton | 4,111 | 39.0 | 3,909 | 47.5 | 8,020 | 42.7 | ||
| Tajik | 3,800 | 36.0 | 1,832 | 22.2 | 5,632 | 30.0 | ||
| Hazara | 959 | 9.1 | 672 | 8.2 | 1,631 | 8.7 | ||
| Uzbek/Turkman | 1,155 | 10.9 | 539 | 6.5 | 1,694 | 9.0 | ||
| Baloach/Nuristani/Pashaie/others | 529 | 5.0 | 1,284 | 15.6 | 1,813 | 9.6 | ||
| Residence | ||||||||
| Urban | 3,067 | 29.1 | 1,426 | 17.3 | 4,493 | 23.9 | ||
| Rural | 7,487 | 70.9 | 6,810 | 82.7 | 14,297 | 76.1 | ||
| Parity | ||||||||
| 1 | 1,769 | 16.8 | 1,012 | 12.3 | 2,781 | 14.8 | ||
| 2–4 | 4,653 | 44.1 | 3,591 | 43.6 | 8,244 | 43.9 | ||
| ≥5 | 4,132 | 39.2 | 3,633 | 44.1 | 7,765 | 41.3 | ||
| Education | ||||||||
| No education | 8,384 | 79.4 | 7,586 | 92.1 | 15,970 | 85.0 | ||
| Primary/Secondary | 1,907 | 18.1 | 620 | 7.5 | 2,527 | 13.4 | ||
| Higher | 263 | 2.5 | 30 | 0.4 | 293 | 1.6 | ||
| Husband education | ||||||||
| No education | 5,201 | 49.3 | 5,396 | 65.5 | 10,597 | 56.4 | ||
| Primary/Secondary | 4,392 | 41.6 | 2,481 | 30.1 | 6,873 | 36.6 | ||
| Higher | 961 | 9.1 | 359 | 4.4 | 1,320 | 7.0 | ||
| Iiteracy | ||||||||
| Illiteracy | 8,575 | 81.2 | 7,646 | 92.8 | 16,221 | 86.3 | ||
| Literacy | 1,979 | 18.8 | 590 | 7.2 | 2,569 | 13.7 | ||
| Job | ||||||||
| No | 9,442 | 89.5 | 6,854 | 83.2 | 16,296 | 86.7 | ||
| Yes | 1,112 | 10.5 | 1,382 | 16.8 | 2,494 | 13.3 | ||
| Wealth | ||||||||
| Poor | 3,829 | 36.3 | 4,009 | 48.7 | 7,838 | 41.7 | ||
| Middle | 2,220 | 21.0 | 1,935 | 23.5 | 4,155 | 22.1 | ||
| Rich | 4,505 | 42.7 | 2,292 | 27.8 | 6,797 | 36.2 | ||
ANC, antenatal care.
Table 2 shows the associations of the cultural factors with ANC visits. Husbands were the decision makers for women’s healthcare in 47.1% of the cases, while only 3.9% of the women took a decision for their own healthcare. Most women (58.1%) revealed that getting permission from their husband for availing healthcare was a major challenge.
Table 2. Cultural-barrier factors and antenatal care visits in women (n=18,790).
| Characteristics | ANC
(n=10,554) |
No ANC
(n=8,236) |
Total
(n=18,790) |
|||||
| n | % | n | % | n | % | |||
| Decision maker for healthcare | ||||||||
| Respondent | 471 | 4.5 | 254 | 3.1 | 725 | 3.9 | ||
| Respondent and husband | 4,604 | 43.6 | 2,949 | 35.8 | 7,553 | 40.2 | ||
| Husband | 4,413 | 41.8 | 4,434 | 53.8 | 8,847 | 47.1 | ||
| Others | 1,066 | 10.1 | 599 | 7.3 | 1,665 | 8.9 | ||
| Permission for healthcare | ||||||||
| Big problem | 5,656 | 53.6 | 5,265 | 63.9 | 10,921 | 58.1 | ||
| Not big problem | 4,898 | 46.4 | 2,971 | 36.1 | 7,869 | 41.9 | ||
ANC, antenatal care.
To examine the characteristics of women who undertook ANC visits, a binary logistic regression analysis was performed. The unadjusted analysis showed that all factors had a significant correlation with availing of the ANC visits (Table 3, left column).
Table 3. Odds ratio and 95% confidence interval of antenatal care visits (n=18,790).
| Variables | Unadjusted | Age-adjusteda) | Adjustedb) | ||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| Age (years) | |||||
| 15–19 | 1.10 (0.93–1.30) | - | 0.65 (0.53–0.80)*** | ||
| 20–29 | 1.23 (1.11–1.35)*** | - | 0.95 (0.84–1.08) | ||
| 30–39 | 1.16 (1.04–1.29)** | - | 1.06 (0.95–1.18) | ||
| 40–49 | 1 (Reference) | - | 1 (Reference) | ||
| Ethnicity | |||||
| Pashtun | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Tajik/ Hazara/Uzbek/Turkman | 1.85 (1.74–1.97)*** | 1.86 (1.75–1.98)*** | 1.70 (1.58–1.81)*** | ||
| Baloach/Nuristani/Pashaie/others | 0.40 (0.35–0.44)*** | 0.39 (0.35–0.44)*** | 0.45 (0.40–0.51)*** | ||
| Residence | |||||
| Urban | 1.96 (1.82–2.10)*** | 1.96 (1.82–2.10)*** | 1.15 (1.06–1.26)** | ||
| Rural | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Parity | |||||
| 1 | 1.54 (1.41–1.68)*** | 1.83 (1.63–2.05)*** | 1.50 (1.32–1.69)*** | ||
| 2–4 | 1.14 (1.07–1.21)*** | 1.23 (1.13–1.33)*** | 1.09 (1.00–1.19) | ||
| ≥5 | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Education | |||||
| No education | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Education | 3.02 (2.75–3.31)*** | 3.06 (2.80–3.36)*** | 1.45 (1.21–1.74)*** | ||
| Husband education | |||||
| No education | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Education | 1.96 (1.84–2.08)*** | 1.95 (1.84–2.07)*** | 1.42 (1.33–1.51)*** | ||
| Iiteracy | |||||
| Illiteracy | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Literacy | 3.00 (2.71–3.30)*** | 3.01 (2.73–3.33)*** | 1.27 (1.06–1.53)* | ||
| Job | |||||
| No | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Yes | 0.60 (0.54–0.64)*** | 0.58 (0.53–0.63)*** | 0.82 (0.74–0.91)*** | ||
| Wealth | |||||
| Poor | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Middle | 1.20 (1.11–1.30)*** | 1.20 (1.11–1.30)*** | 1.32 (1.22–1.43)*** | ||
| Rich | 2.06 (2.00–2.20)*** | 2.05 (1.92–2.20)*** | 1.64 (1.51–1.80)*** | ||
| Decision maker for healthcare | |||||
| Respondent | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Respondent and husband | 0.84 (0.72–0.99)* | 0.84 (0.72–0.98)* | 0.87 (0.73–1.03) | ||
| Husband | 0.54 (0.46–0.63)*** | 0.53 (0.46–0.62)*** | 0.68 (0.57–0.80)*** | ||
| Others | 0.96 (0.80–1.15) | 0.94 (0.78–1.13) | 1.12 (1.26–1.40) | ||
| Permission for healthcare | |||||
| Big problem | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||
| Not big problem | 1.54 (1.45–1.63)*** | 1.54 (1.45–1.63)*** | 1.35 (1.26–1.44)*** | ||
* P<0.05; ** P<0.01; *** P<0.001; OR, odds ratio; CI, confidence interval.
a) Adjusted by age as the categorical variable.
b) Adjusted by age, ethnicity, residence, parity, education, husband education, literacy, job, wealth, decision for healthcare, and permission for healthcare.
The multivariate analysis showed that young age (15–19 years of age) (OR=0.65, P<0.001), having a job (OR=0.82, P<0.001), and decision for healthcare being taken by the husband (OR=0.68, P<0.001) were significantly associated with no ANC visits (Table 3, right column). Compared to the Pashtun, the ethnic group of Uzbek/Turkman/Tajik/Hazara (OR=1.70, P<0.001) and the group of Baloach/Noristani/Pashaie/others (OR=0.45, P<0.001) showed significantly higher and lower OR, respectively. Residing in the urban area (OR=1.15, P<0.002), parity of one (OR=1.50, P<0.001), having an education (OR=1.45, P<0.001), husband having an education (OR=1.42, P<0.001), literate (OR=1.27, P<0.011), rich and middle wealth status (OR=1.64, P<0.001 and OR=1.32, P<0.001, respectively), and no big challenge in getting permission for availing healthcare (OR=1.33, P<0.001) were factors significantly associated with undertaking ANC visits (Table 3, right column). Further analysis by three levels of education (no education, primary and secondary education, higher education) showed that higher education of women as well as their husbands, had a higher proportion of women undertaking ANC visits, than those with primary and secondary education (data not shown).
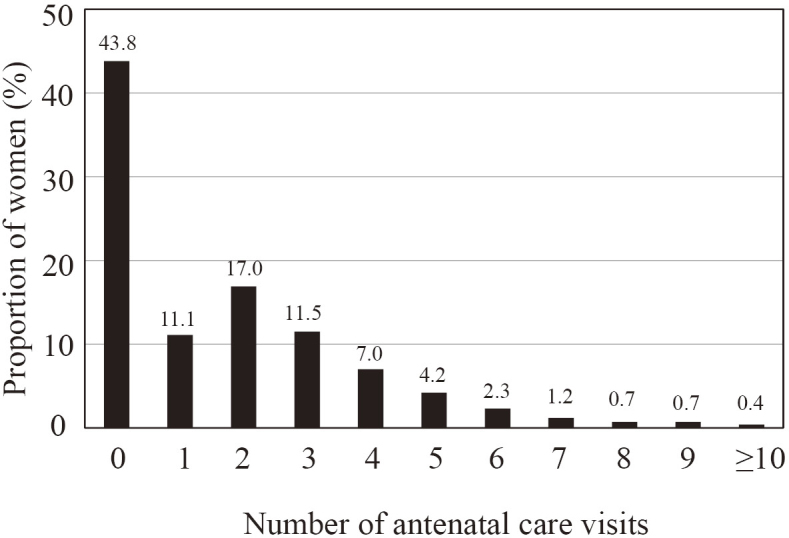
The OR of age and parity seemed contradicting in the multivariate analysis. Those in the youngest age group had less number of ANC visits than those aged 40–49 years, although women with one parity had more ANC visits than those with parities of five or more. The distribution of parity in age groups showed that 2,781 women with one parity were distributed across all age groups and most of them were 20–29 years old (Fig. 2). The logistic regression analysis adjusted by age as the categorical variable showed the same results in parity as the results of multivariate analysis (Table 3, middle column).
Fig. 2. Distribution of parity in age groups.
In the youngest age group (15–19 years), the majority was one parity. However, 2,781 women with one parity were distributed across all age groups and most of them were 20–29 years old. There were 6 women of 40–49 years (0.03%) who had one parity.
DISCUSSION
This is the first study conducted in Afghanistan, which showed that the husband’s education, literacy, ethnicity, the decision maker for availing healthcare services, and difficulty in getting permission for healthcare were significantly correlated with the utilization of ANC services. Not just socio-demographic factors but cultural factors were also associated with undertaking ANC visits. It was consistent with the results of previous studies that more women with education, urban residence, and rich wealth status undertook ANC visits compared to women with no education, rural residence, and poor status.18-22
Not just education of women but also that of their husbands was significantly associated with utilization of ANC usage in Afghanistan. In addition, more women with a higher level of education for both self and their husband availed of ANC compared to those with primary and secondary education. This result was consistent with other studies in many developing countries.23-30 Women with higher education availed of ANC services more than the lesser educated group in Ethiopia,25 and higher education of husbands was associated with higher ANC utilization in Sudan.23 The significant association of education with ANC visits could be because educated women have access to written information, and women with higher education are more knowledgeable about healthcare. Moreover, educated husbands might be more aware and have a good communication with their spouses about availing maternal healthcare. These assumptions are supported by previous studies in Nepal and other developing countries.31,32 To guide the society towards a healthy community, the Afghanistan government should improve education by focusing on parallel programs in the educational system as well as vertical projects for the literacy of old population with support from donors. Furthermore, free school education should be made mandatory for increasing the level of education in the country.
Ethnicity was significantly associated with ANC visits. In the primary analysis, Uzbek, Turkman, Tajik, and Hazara ethnic groups were associated with more ANC visits and Baloach, Nuristani, Pashaie and other minority ethnic groups were associated with lesser ANC visits compared to Pashtun. Therefore, two groups were created for the logistic regression analyses. This result was similar to results of other studies conducted in developing countries, such as Nepal and Ethiopia.24,25 It could be because each ethnic group has a different culture, beliefs and norms.25 It can be assumed that those belonging to minor ethnic groups are less educated, reside away from cities and the media, and are unaware of healthcare benefits. The MoPH conveys health messages to people through the media. A pervious study in Afghanistan showed that more women who were exposed to TV undertook ANC visits, than women with no access to TV.19 To improve the cultural practices about health, ANC messages should be spread through the media and community based Family Health Active Groups (FHAGs).
This study found that the decision maker for healthcare, and difficulty in getting permission from their husbands was significantly correlated with ANC visits. These results were similar to the results of other studies in Nigeria, Zambia and Uganda.28,29,33 The decision for healthcare is very important, but might be affected by the fact that Afghanistan is a male dominant country. In Afghanistan, when a woman wants to step of the home for any reason, she needs to obtain permission from her husband before leaving home. It was reported that cultural and religious norms affected the use of maternal health care.34,35 To enhance the women’s ability to take a decision, the government needs to support programs and projects for women’s empowerment, expanding them to all 34 provinces. Some of these are women empowerment projects supported by USAID, the Afghan women empowerment program (AWEP) supported by Sweden, and the women’s empowerment program provided by the Asia Foundation. To increase the awareness about maternal healthcare among men, the importance of ANC should be included in the health education sessions at clinics all over the country.
There are some limitations in this study. First, this study did not include all villages in the selected areas of the country. For security reasons during the AfDHS 2015, it was difficult to include some villages in some provinces like Zabul. Second, there could be a recall bias, since the questions to women were about what happened or what they did during the last five years. Third, the demographic and health surveys did not cover health facility factors and service availability; hence, this study could not explore the quality of ANC services, though, the quality of healthcare services plays an important role in the satisfaction and use by patients. However, this study used the national survey as a source of data, which included 25,650 households all over the country. The response rate of women was 97%, and the method of collecting and analyzing the data followed the international methods accurately.
In conclusion, this study showed that availing of at least one ANC visit was 56.2% in Afghanistan, which is very low. Husband’s education, literacy, ethnicity, decision maker for healthcare, and difficulty in obtaining permission for healthcare were the important factors which were significantly associated with the use of ANC visits. Not only socio-demographic factors, but also cultural factors were associated with ANC visits. Further studies are needed to focus on the quality of maternal healthcare and ANC services to address the poor MMR in Afghanistan.
ACKNOWLEDGMENTS
We would like to thank Dr. Zaw Zaw Aung (Ministry of Health and Sports, Myanmar) and Dr. Sayed Hashmat Masoud for their supporting the data analysis and writing the manuscript, respectively. We would also like to thank the Ministry of Education, Culture, Sports, Science and Technology of Japan for a one-year scholarship providing the opportunity to make this report at Nagoya University.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest associated with this study.
Abbreviations
- AfDHS
the Afghanistan Demographic and Health Survey
- ANC
antenatal care
- EA
enumeration area
- MMR
maternal mortality ratio
- MoPH
Ministry of Public Health.
REFERENCES
- 1.Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387(10017):462–474. [DOI] [PMC free article] [PubMed]
- 2.UN General Assembly. Transforming our world: the 2030 Agenda for Sustainable Development, resolution adopted by the General Assembly. http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E. Published October 21, 2015. Accessed July 19, 2018.
- 3.WHO. Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization; 2015. http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/. Accessed July 19, 2018.
- 4.Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–333. [DOI] [PubMed]
- 5.Bauserman M, Lokangaka A, Thorsten V, et al. Risk factors for maternal death and trends in maternal mortality in low- and middle-income countries: a prospective longitudinal cohort analysis. Reprod Health. 2015;12(Suppl 2):S5. [DOI] [PMC free article] [PubMed]
- 6.UNICEF. Maternal and newborn health. New York: United Nations Children’s Fund; 2009. https://www.unicef.org/publications/files/SOWC_2009_Main__Report__03112009.pdf. Accessed July 19, 2018.
- 7.WHO. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016. http://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1. Accessed July 19, 2018. [PubMed]
- 8.Ministry of Public Health. National Risk and Vulnerability Assessment (NRVA). Kabul, Afghanistan: Ministry of Public Health; 2007.
- 9.Ministry of Public Health. Afghanistan Mortality Survey (AMS). Kabul, Afghanistan: Ministry of Public Health; 2010.
- 10.Britten S. Maternal mortality in Afghanistan: setting achievable targets. Lancet. 2017;389(10083):1960–1962. [DOI] [PubMed]
- 11.Ministry of Public Health. Afghanistan Demographic and Health Survey (AfDHS). Kabul, Afghanistan: Ministry of Public Health; 2015.
- 12.World Health Organization. Global Health Observatory data repository. Maternal mortality Data by country. http://apps.who.int/gho/data/node.main.15?lang=en. Accessed January 27, 2018.
- 13.Sinha S, Upadhyay RP, Tripathy JP, Patro BK. Does utilization of antenatal care result in an institutional delivery? Findings of a record-based study in urban Chandigarh. J Trop Pediatr. 2013;59(3):220–222. [DOI] [PubMed]
- 14.Farzad F, A Reyer J, Yamamoto E, Hamajima N. Socio-economic and demographic determinants of full immunization among children of 12–23 months in Afghanistan. Nagoya J Med Sci. 2017;79(2):179–188. [DOI] [PMC free article] [PubMed]
- 15.Akseer N, Bhatti Z3, Rizvi A, Salehi AS, Mashal T, Bhutta ZA. Coverage and inequalities in maternal and child health interventions in Afghanistan. BMC Public Health. 2016;16:797. [DOI] [PMC free article] [PubMed]
- 16.Azimi MD, Najafizada SA, Khaing IK, Hamajima N. Factors influencing non institutional deliveries in Afghanistan: secondary analysis of the Afghanistan mortality survey 2010. Nagoya J Med Sci. 2015;77(1–2):133–143. [PMC free article] [PubMed]
- 17.Ministry of Public Health. Afghanistan National Health Policy 2015–2020. Kabul, Afghanistan: Ministry of Public Health; 2015.
- 18.Rahmani Z, Brekke M. Antenatal and obstetric care in Afghanistan-a qualitative study among health care receivers and health care providers. BMC Health Serv Res. 2013;13:166. [DOI] [PMC free article] [PubMed]
- 19.Shahram MS, Hamajima N, Reyer JA. Factors affecting maternal healthcare utilization in Afghanistan: secondary analysis of Afghanistan Health Survey 2012. Nagoya J Med Sci. 2015;77(4):595–607. [PMC free article] [PubMed]
- 20.Kim C, Saeed KM, Salehi AS, Zeng W. An equity analysis of utilization of health services in Afghanistan using a national household survey. BMC Public Health. 2016;16:1226. [DOI] [PMC free article] [PubMed]
- 21.Rahman MM, Karan A, Rahman MS, et al. Progress toward universal health coverage: a comparative analysis in 5 South Asian countries. JAMA Intern Med. 2017;17(9):1297–1305. [DOI] [PMC free article] [PubMed]
- 22.Akseer N, Salehi AS, Hossain SM, et al. Achieving maternal and child health gains in Afghanistan: a Countdown to 2015 country case study. Lancet Glob Health. 2016;4(6):395–413. [DOI] [PubMed]
- 23.Ali AA, Osman MM, Abbaker AO, Adam I. Use of antenatal care services in Kassala, eastern Sudan. BMC Pregnancy Childbirth. 2010;10:67. [DOI] [PMC free article] [PubMed]
- 24.Paudel YR, Jha T, Mehata S. Timing of First Antenatal Care (ANC) and inequalities in early initiation of ANC in Nepal. Front Public Health. 2017;5:242. [DOI] [PMC free article] [PubMed]
- 25.Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14:161. [DOI] [PMC free article] [PubMed]
- 26.Mugo NS, Dibley MJ, Agho KE. Prevalence and risk factors for non-use of antenatal care visits: analysis of the 2010 South Sudan household survey. BMC Pregnancy Childbirth. 2015;15:68. [DOI] [PMC free article] [PubMed]
- 27.Yaya S, Bishwajit G, Ekholuenetale M, Shah V, Kadio B, Udenigwe O. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS One. 2017;12(9):e0184934. [DOI] [PMC free article] [PubMed]
- 28.Abimbola JM, Makanjuola AT, Ganiyu SA, Babatunde UMM, Adekunle DK, Olatayo AA. Pattern of utilization of ante-natal and delivery services in a semi-urban community of North-Central Nigeria. Afr Health Sci. 2016;16(4):962–971. [DOI] [PMC free article] [PubMed]
- 29.Kawungezi PC, AkiiBua D, Aleni C, et al. Attendance and utilization of antenatal care (ANC) services: multi-center study in upcountry areas of Uganda. Open J Prev Med. 2015;5(3):132–142. [DOI] [PMC free article] [PubMed]
- 30.Chankham T, Yamamoto E, Reyer JA. Knowledge of free delivery policy among women who delivered at health facilities in Oudomxay Province, Lao PDR. Nagoya J Med Sci. 2017;79(2):135–145. [DOI] [PMC free article] [PubMed]
- 31.Ahmed S, Andreea A, Creanga mail, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One. 2010;5(6):e11190. [DOI] [PMC free article] [PubMed]
- 32.Sharma S, Sawangdee Y, Sirirassamee B. Access to health: women’s status and utilization of maternal health services in Nepal. J Biosoc Sci. 2007;39(5):671–692. [DOI] [PubMed]
- 33.Chama-Chiliba CM, Koch SF. Utilization of focused antenatal care in Zambia: examining individual-and community-level factors using a multilevel analysis. Health Policy Plan. 2015;30(1):78–87. [DOI] [PubMed]
- 34.Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85(10):812–819. [DOI] [PMC free article] [PubMed]
- 35.Singh P, Rai R, Alagarajan M, Singh L. Determinants of maternity care services utilization among married adolescents in rural India. PLoS One. 2012;7(2):e31666. [DOI] [PMC free article] [PubMed]