Abstract
Eating disorders and weight problems across the life span have been linked to adverse childhood experiences. Previous research often focused on child abuse and omitted investigating effects of child neglect. The present study evaluates effects of neglect on bodyweight across the life span and how emotional neglect and bodyweight are linked via mental distress. Within a large survey representative of the German population (N = 2,500), individuals completed measures of mental distress, childhood trauma, and height and weight. We conducted logistic regression analyses on bodyweight extremes and a moderated mediation analysis. In men, physical neglect aggravated the risk to be underweight. In women, emotional neglect was linked to severe obesity. In both sexes, emotional neglect was related to mental distress. We found an indirect effect of emotional neglect on bodyweight via mental distress, however, it was only present in women. Our results attest to long-term consequences of adverse early experiences. We showed a possible mechanism for women’s higher vulnerability towards eating disorders. In general, investigations of eating and weight disorders should also include men and employ sex-specific methods of analyses. Lastly, neglect should also receive more attention to prevent suffering and negative sequelae over the life span.
Introduction
Since the first landmark study investigating adverse effects of child maltreatment by Felitti, et al.1, a growing body of research has focused on the consequences of early, potentially traumatic events2,3. Childhood trauma represents a major health issue in the US and around the world e.g.4. A recent representative survey of the German population using the established taxonomy of the Childhood Trauma Questionnaire CTQ5 which differentiates emotional, physical, and sexual abuse, and physical and emotional neglect, found that almost a third of participants had suffered at least one type of child maltreatment6. Maltreatment was associated with lower educational attainment, employment status, and income. This was true for abuse and neglect. Prospective, large scale studies with long follow-up times consistently showed a profound negative impact of maltreatment on development, educational and social attainment, and behavioral problems such as criminal offending7, and substantial physical8 and mental9–11 health risks.
In fact, complex trauma-dependent developmental alterations pertain to the psychological, interpersonal, physiological, and neurological domain. Survivors of maltreatment show aberrations with regard to the stress-response-system, metabolic risk factors such as inflammation12 and dyslipidemia13, and have an elevated risk to suffer from cardiovascular diseases, diabetes, and autoimmune disorders14,15.
Substantial evidence exists for the connection of eating disorders and weight problems with childhood adversities16–19. In particular, effects of sexual and physical abuse have drawn attention: Beutel, et al.20 found a link between sexual abuse and obesity in a large number of female psychosomatic inpatients. This finding corroborates previous research by Wonderlich, et al.21, Williamson, et al.22, and Brewerton, et al.23, the latter citing molestation and physical abuse as risk factors for an early onset of binge eating disorder. A review24 confirmed strong links of childhood physical and sexual abuse and obesity in adulthood. Childhood trauma has also been identified as a contributing factor to eating disorders entailing lower weight, such as bulimia and anorexia25,26. The connection was confirmed for sexual, physical, and emotional abuse27.
The contribution of neglect to eating and weight problems is less clear. A recent review by Molendijk, et al.17 attested to high prevalence rates (21–59%) of any type of childhood trauma in individuals with eating disorders. However, in a sample of 142 young female psychology students, neither emotional nor physical neglect contributed to disordered eating28. Beutel, et al.20 found no connection of emotional neglect and obesity, however, physical neglect aggravated women’s risk for obesity, even after adjusting for depression. Likewise, in a sample of 73 mostly female patients treated for eating disorders, Kong and Bernstein29 confirmed an effect of childhood physical neglect on disordered eating.
An investigation of a community-based sample of mothers and their children including Child Protective services data yielded that physical and emotional neglect elevated the offspring’s risk to suffer from eating and/or weight problems16. Along the same lines, within the National Comorbidity Survey emotional neglect was related to a lifetime diagnosis of any kind of eating disorder30. However, comparisons with other studies are difficult due to the investigation’s qualitative nature and its lack of a psychometrically validated instrument.
Thus, effects of childhood neglect should be addressed in more depth. Although perhaps a more subtle form of child maltreatment than beatings or sexual abuse, it interferes with children’s emotional development in important ways14,24,31,32.
Emotion regulation difficulties are a centrepiece of etiological models of eating disorders. Disturbances, e.g. in the aftermath of childhood trauma, render individuals susceptible to a range of mental disorders and distress33,34. Trauma-dependent alterations at the brain level relate to structural and functional changes in regions implicated in emotion perception as well as regulation – and they were also present in neglected individuals35–37. Correspondingly, eating psychopathology has been shown to be used as a means of regulating negative emotional states, especially by individuals who lack more productive coping strategies38,39.
The mediating role of emotion dysregulation (the absence of adaptive coping strategies in the face of negative emotional states as measured by the Difficulties in Emotion Regulation Scale (DERS) by Gratz and Roemer40) between childhood abuse and disordered eating has previously been confirmed in a sample of young female students28. However, questions remain: it is unclear whether the model can be extended onto large population-based samples and how an individual’s sex shapes the outcomes of childhood trauma. Especially regarding eating and weight problems, previous investigations often focused on women.
The present study aims at expanding previous research on long-term effects of childhood emotional and physical neglect by investigating a representative sample from the community, using sex-specific analyses, considering extreme bodyweight categories on both ends of the spectrum (i.e. underweight and severely obese individuals). First, we investigated weight extremes in men and women using logistic regression analyses. Focusing on emotional neglect, in the second part of the paper, the proposed mediating role of mental distress is tested empirically. Building on previous research, we hypothesized that mental distress links childhood adversity and bodyweight extremes, as the latter can be brought about by distressed individuals using eating or fasting as inadequate coping behaviors. Thus, we aimed to expand previous research by empirically testing whether mental distress symptoms are indeed the proposed link between early interpersonal difficulties and eating and weight problems later in life.
The following questions shall be answered:
How does childhood (emotional and physical) neglect affect bodyweight in both sexes across the life span?
a) Does current mental distress mediate the effects of childhood emotional neglect on bodyweight in adulthood?
b) Is this indirect effect moderated by sex?
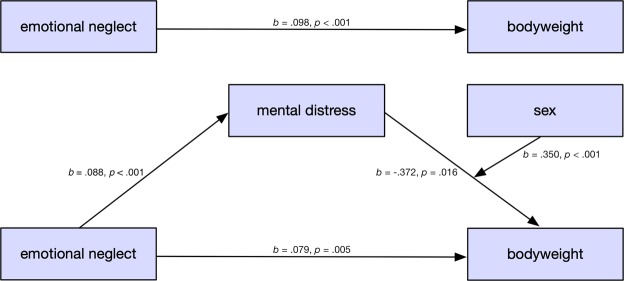
The statistical model at the basis of questions 2 (a, b) is displayed in Fig. 1.
Figure 1.
Depiction of the theoretical model. The effect of emotional neglect on bodyweight is mediated by mental distress and moderated by sex.
Results
Sample description
In the following, we report survey results of 2,510 individuals. 53.35% of participants were women. Means, standard deviations, and correlations of measures of interest are presented in Table 1. Mean age was 48.4 (SD 18.2) (ranging from 14 to 94) years and mean BMI was 25.76 (SD 4.67) (ranging from 11.47 to 67.76). A higher level of emotional neglect was positively related to increased mental distress, higher age, and higher BMI. BMI was higher for older participants, men, and those with a lower income.
Table 1.
Means, standard deviations, and correlations among measures.
| Variable | Mean (SD)/percentage | Physical neglect | Mental distress | Age | Sex | Income | BMI |
|---|---|---|---|---|---|---|---|
| Emotional neglect | 9.48 (4.43) | 0.636** | 0.263** | 0.082** | 0.002 | 0.013 | 0.071** |
| Physical neglect | 9.48 (4.44) | 0.244** | 0.241** | −0.027 | 0.036 | 0.061** | |
| Mental distress | 1.38 (2.16) | 0.028 | 0.114** | −0.002 | 0.020 | ||
| Age | 48.4 (18.2) | 0.031 | 0.243** | 0.191** | |||
| Sex | 1Men = 46.65 2Women = 53.35 | −0.084** | −0.132** | ||||
| Income | 1.55 (0.55) | −0.016 | |||||
| BMI | 25.76 (4.68) |
Note. Bivariate analyses are Pearson product-moment correlations, Spearman’s Rho for categorical variables. *p ≤ 0.05, ** p ≤ 0.01. Statistics of categorical variables indicate percentages. Emotional neglect and physical neglect: CTQ subscales, range for each: 5–25. Mental distress: PHQ-4 total score, range 0–12. Cut-off according to Löwe, et al.65: low mental distress: 0–5, high mental distress: 6–12. Income: Equivalised income calculated according to the OECD guideline67: household income/√(people in household); household income per month: 1 =< 1,250€, 2 = 1,250–2,500€, 3 => 2,500€. N = 2,404.
Logistic regression analyses on severe obesity and underweight
In order to answer research question 1 concerning the relationship of different types of neglect and weight extremes across the life span, we conducted sex-specific logistic regression analyses (controlling for age and equivalised income). They yielded different predictors for severe obesity and underweight in men and women (see Table 2). In men, neither emotional nor physical neglect was related to severe obesity. Physical neglect was associated with underweight in men.
Table 2.
Associations of different types of childhood maltreatment and weight extremes in men and women (adjusted for age, equivalised income, and the respective other four types of childhood adversity assessed by the CTQ).
| Severe Obesity | Underweight | |||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Nagelkerke R² | p | OR (95% CI) | Nagelkerke R² | p | |
| Men | ||||||
| Emotional neglect | 0.00 (0.00–0.00) | 0.027 | 0.99 | 1.51 (0.07–33.59) | 0.233 | 0.794 |
| Physical neglect | 0.88 (0.20–3.79) | 0.027 | 0.86 | 5.30 (1.10–25.47) | 0.233 | 0.037 |
| Women | ||||||
| Emotional neglect | 3.30 (1.07–10.22) | 0.055 | 0.038 | 3.22 (0.19–53.87) | 0.057 | 0.416 |
| Physical neglect | 1.16 (0.46–2.95) | 0.055 | 0.758 | 0.45 (0.06–3.63) | 0.057 | 0.457 |
In women, emotional neglect statistically predicted severe obesity. The association was positive, i.e. severe obesity was related to having experienced relevant levels of neglect. Physical and emotional neglect failed to predict underweight in women.
Moderated mediation analysis: Testing the effect of emotional neglect on bodyweight via mental distress
To test our hypotheses that emotional neglect has an indirect effect on bodyweight via mental distress and that this effect further differs dependent on sex, we conducted a moderated mediation model.
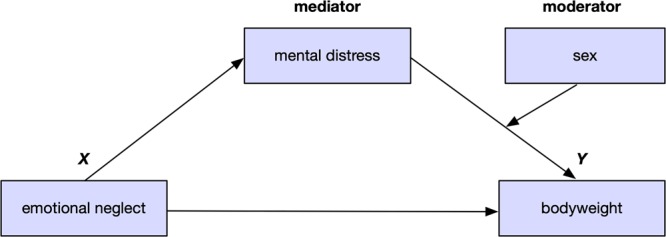
Results are displayed in Table 3 and Fig. 2.
Table 3.
Results of the moderated mediation analysis on BMI.
| Coeff. | SE | 95% CI (L, U) | T | p | |
|---|---|---|---|---|---|
| Model 0: BMI as criterion | |||||
| Constant | 23.291 | 0.399 | 22.908/24.473 | 59.363 | <0.001 |
| Emotional neglect | 0.098 | 0.028 | 0.043/0.152 | 3.527 | <0.001 |
| Covariates | |||||
| Age | 0.053 | 0.006 | 0.042/0.064 | 9.543 | <0.001 |
| Income | −0.478 | 0.176 | −0.823/−0.133 | −2.720 | 0.007 |
| Other adversities (sum) | −0.100 | 0.043 | −0.185/0.015 | −2.308 | 0.021 |
| Model 1: Mental Distress as criterion | |||||
| Constant | 0.354 | 0.182 | −0.003/0.712 | 1.945 | 0.052 |
| Emotional Neglect | 0.088 | 0.013 | 0.063/0.113 | 6.945 | <0.001 |
| Covariates | |||||
| Age | 0.001 | 0.003 | −0.004/0.006 | 0.339 | 0.902 |
| Income | −0.501 | 0.175 | −0.845/−0.157 | −2.858 | 0.004 |
| Other adversities (sum) | −0.115 | 0.043 | −0.199/0.031 | −2.677 | 0.008 |
| Model 2: BMI as criterion | |||||
| Constant | 25.749 | 0.530 | 24.710/26.788 | 48.611 | <0.001 |
| Emotional Neglect | 0.079 | 0.028 | 0.024/0.134 | 2.837 | 0.005 |
| Mental Distress | −0.372 | 0.154 | −0.673/−0.070 | −2.418 | 0.016 |
| Sex | −1.358 | 0.221 | −1.792/−0.924 | −6.133 | <0.001 |
| Covariates | |||||
| Age | 0.054 | 0.005 | 0.044/0.065 | 9.902 | <0.001 |
| Income | −0.501 | 0.175 | −0.861/−0.177 | −2.978 | 0.003 |
| Other adversities (sum) | 0.028 | 0.030 | −0.845/−0.157 | −2.858 | 0.004 |
| Interaction terms | |||||
| Distress × sex | 0.350 | 0.091 | 0.172/0.528 | 3.854 | <0.001 |
Note. EN: Emotional neglect according to the CTQ (range 5–25). Income: Equivalised income calculated according to the OECD guideline67: household income/√(people in household); household income per month: 1 = < 1,250€, 2 = 1,250–2500€, 3 = > 2,500€. N = 2,404.
Figure 2.
Depiction of the unmediated effect of emotional neglect on bodyweight (model 0, top), and the full moderated mediation model (model 2, bottom). The effect was partially mediated by distress, so that the direct effect (b = 0.098, p < 0.001) observed in model 0 was smaller in model 2 (b = 0.079, p = 0.005).
First, we tested a regression model (model 0) predicting BMI which included only emotional neglect (p < 0.001), and the covariates age (p < 0.001), equivalised income (p = 0.007), and sum of other childhood adversities (p = 0.021) (R2 = 0.042, F (4, 2289) = 25.991, p < 0.001). Note that mediator (mental distress) and moderator (sex) were not included. The model yielded a significant positive effect of emotional neglect on BMI. It is visualized in the upper half of Fig. 3. Thus, it established a statistically relevant connection.
Figure 3.
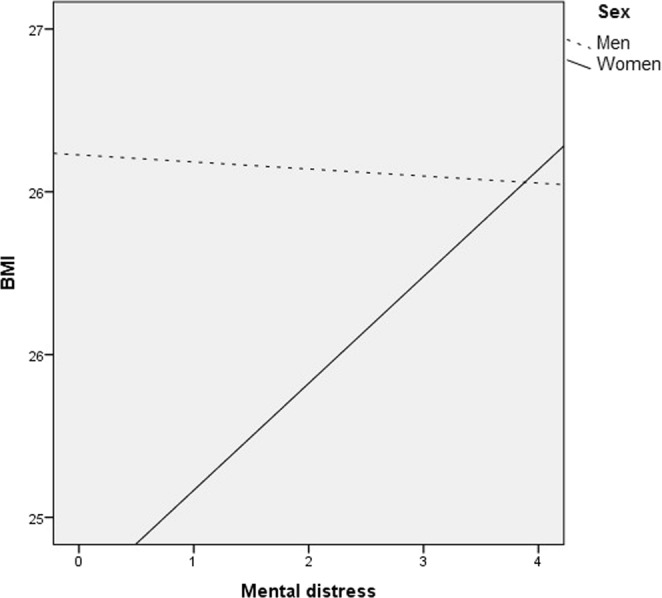
Association of mental distress and BMI as a function of sex: The drawn through line represents a significant positive association between distress and BMI among women (b = 0.328 [95% CI 0.215–0.441], p < 0.001). The dotted line indicates a nonsignificant association of BMI and distress among men (b = −0.022 [95% CI −0.163–0.120], p = 0.764).
We then tested whether the mediator (mental distress) was, in accordance with our hypotheses, significantly predicted by emotional neglect (and covariates age, equivalised income, and sum of other childhood adversities). This was the case (model 1: R2 = 0.0724, F(4, 2278) = 44.477, p < 0.001).
The full model (model 2) included the covariates age, equivalised income, and sum of other childhood adversities, the proposed mediator mental distress, and the proposed moderator sex (i.e. the interaction term mental distress x sex). It predicted BMI (R2 = 0.0652, F(7, 2275) = 22.655, p < 0.001) with the significant predictors age, equivalised income, distress, sex, and the interaction distress x sex (b = 0.350, p < 0.001). The direct, unconditional effect of emotional neglect on BMI was smaller, yet remained significant (p = 0.005).
We further probed the interaction of sex and distress using the Johnson-Neyman-technique41 (see Fig. 3).
Only in women more distress was related to higher BMI scores (b = 0.328, p < 0.001). In men, this was not the case (b = −0.022, p = 0.764). The interaction is visualized in Fig. 4 (Table 4 yields mean values and SD). In summary, this interaction effect in the absence of a significant direct effect of emotional neglect supports the idea of a moderated mediation.
Figure 4.
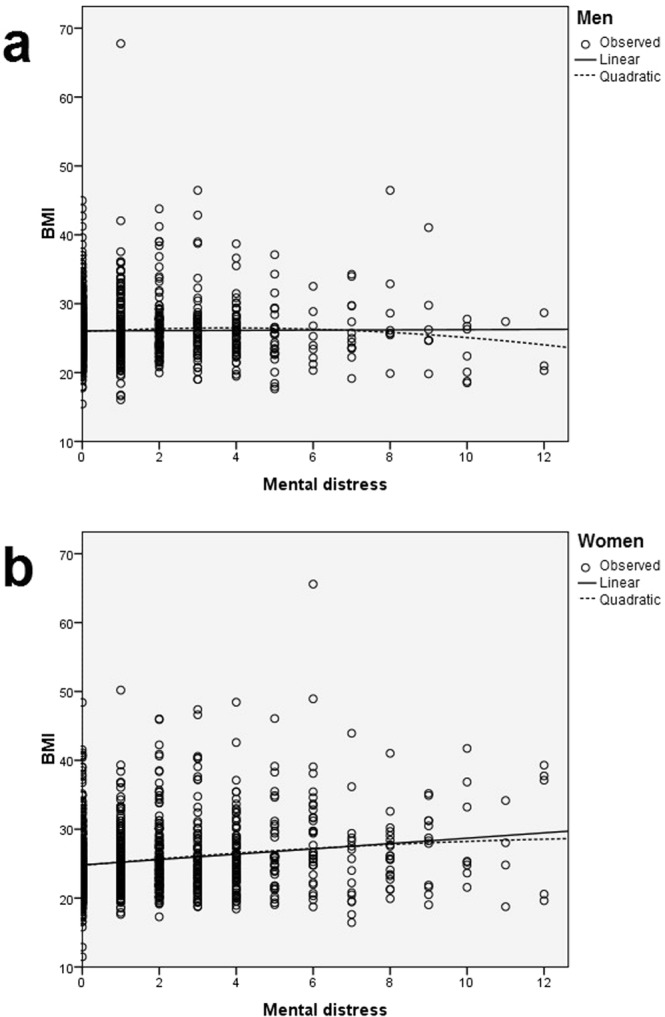
Scatter plots with fitted curves (linear and quadratic) depicting the relationship of mental distress and BMI in men and women. A two-way ANOVA of sex and mental distress on BMI yielded a significant interaction of the fixed effects sex and mental distress (model: F(3) = 14.382, p < 0.001. mental distress: F(1) = 9.768, p < 0.001; sex: F(1) = 1.918, p < 0.001, mental distress by sex: F(1) = 11.544, p < 0.001). For mean values and SD, see Table 4.
Table 4.
The effects of mental distress and sex on bodyweight.
| Mental distress | |||||||
|---|---|---|---|---|---|---|---|
| Low | High | Total | |||||
| BMI | M (SD) | N | M (SD) | N | M (SD) | N | |
| Sex | Men | 26.08 (4.09) | 1,097 | 25.96 (5.46) | 48 | 26.10 (4.16) | 1,145 |
| Women | 25.23 (4.77) | 1,207 | 27.97 (7.39) | 99 | 25.46 (5.08) | 1,306 | |
| Total | 25.64 (4.48) | 2,304 | 27.31 (6.86) | 147 | 25.76 (4.68) | 2,451 | |
Note. Mental distress: PHQ-4 total score, range 0–12. Cut-off according to Löwe, et al.65: low mental distress: 0–5, high mental distress: 6–12.
Discussion
In a large, representative community sample, we found associations between maltreatment suffered during childhood and consequences observed in adulthood related to mental distress and bodyweight.
Thus, the present research endeavor replicated previous findings on the association of childhood trauma, in particular of emotional neglect, and mental distress in adulthood35,42,43. In the whole sample, we found a relationship between emotional neglect suffered as a child and current mental distress levels across the lifespan. The link of emotional neglect and severe obesity we confirmed in women also corroborates previous research13,20,22,44.
Previous research indicated an indirect relationship of childhood trauma and eating disorders in adulthood via emotion dysregulation as previously shown by Racine and Wildes27, Moulton, et al.28 (who had both used the Difficulties in Emotion Regulation Scale). Our model is compatible with these results, placing mental distress (i.e. a manifestation of failed emotional regulation) at the center. We showed that the proposed mediation effect was present in a large, community-based sample with a broad age range, and that it pertained to emotional neglect. Our results also specify that in this sample, the described effect can only be found in women.
Our study differed from previous research which failed to establish a link between childhood emotional neglect and adult weight or eating problems in a number of ways. On the one hand, our participants were older (M = 48.4, SD = 18.2) than those of the Korean study which investigated adolescents29, or the students questioned by Moulton, et al.28. Also, our sample was drawn from a representative survey, thus it certainly differs from clinical investigations e.g. by20 as the overwhelming majority reported no considerable mental distress.
Due to the abovementioned psychometric and socio-historical reasons elaborated by Häuser, et al.45, we focused on emotional neglect instead of physical neglect. Emotional neglect might be more difficult to verify than physical neglect (as studies investigating physical neglect could also draw from third parties’ records such as Child Protective Services), yet there is broad consensus that emotional neglect measures are relevant as they speak to an atmosphere of emotional invalidation which lay the foundation of psychopathological development e.g.46,47. Substantial and long-lasting detrimental effects of emotional neglect have been underscored by the present results.
Importantly, our results highlighted sex differences: The link between mental distress and higher BMI was only found in women. Thus, in women, severe obesity likely is a consequence of disordered eating behavior utilized to cope with adverse subjective emotional states as self-regulation and emotional regulation capacities prove insufficient. This is in line with theories put forth by Cloitre, et al.48 and Kent and Waller46, postulating that an emotionally invalidating environment impedes a child’s capacity to effectively regulate their own emotions, predisposing them to suffer from mental health disturbances later in life. Learned strategies employed to calm or distract oneself when facing distress then include maladaptive ones with negative long-term consequences, such as overeating. Previous research indicated that men and women differ with respect to their preferred coping strategies, e.g. with women favoring emotion-focused strategies previously linked to binge eating49,50, and with higher rates of alcohol use disorders in men51. Eating has been shown to dampen negative affect and alleviate inner tensions38,52. Generally, eating disturbances are part of an internalizing phenotype of psychopathology which is much more common in women e.g.53. Perhaps this is why emotional neglect and bodyweight in men were not linked in a statistically significant way. By way of example, a large US study failed to find an association of most types of childhood adversity (including emotional neglect and abuse) with the lifetime prevalence of eating disorders in men30.
Additionally, it has been shown that distress is aggravated by a loss of interoceptive awareness and emotion recognition, changes reported in traumatized individuals as well as in eating disorder patients. They entail subdued joy derived from activities which normally contribute to a person’s well-being and positive mood, such as social interactions or hobbies33,54–56. The inadequate perception of bodily signals also implicates disturbed appraisal of hunger or satiety, thus influencing food intake57.
Furthermore, neuropsychological studies of traumatized individuals have demonstrated diminished capacities to inhibit behavioral actions58,59, hence making it difficult to stop eating after having consumed a reasonable amount. Elton, et al.60 showed that trauma-dependent aberrations of brain circuitry implicated in inhibition differed between men and women. In summary, the results speak to substantial long-term effects of neglect, or “acts of omission”, following the definition offered by Leeb, et al.61. Therefore, the investigation of childhood adversities should not be limited to “acts of commission” like abuse or violence, but instead include indicators of negative/inadequate caregiver interactions as they also put children at risk for negative sequelae.
A strength of our study is its large, representative population-based sample and its broad age range. Sex-specific analyses are another strong point. Limitations pertain to self-report data with regard to height and weight (used to calculate the BMI), current mental distress, and childhood trauma. Especially the latter could be influenced by memory biases. Previous research attested to the validity62 of retrospective, self-reported childhood adversity while an earlier review suggests that there is a bigger risk of self-reports under- than overestimating past childhood maltreatment63. Another limitation is that as we investigated mental distress symptoms, the model tests the contribution of risk factors rather than identifying possible resilience factors buffering the impact of childhood adversity e.g. as proposed by current models of risk and resilience64. The model explained roughly 7% of the criterion’s variance which means that apart from the factors we included, there should be other major influences on bodyweight across the lifespan. However, the present findings highlight a modifiable risk factor for eating and weight problems which has previously received little attention.
Childhood emotional neglect elevates the risk to suffer from mental distress later in life. However, only in women, this also entailed higher bodyweight. Sex-dependent pathways of emotional neglect on bodyweight via mental distress might be ascribed to different coping strategies and neurocognitive inhibitory capacities. The association between childhood adversity and lower weight in men is less clear. As research on eating psychopathology has often focused on women, less is known about disturbed eating and other factors impacting weight gain and weight loss in men. Our results suggest that for men, these might be different than for women.
With the present study, we confirmed links between different types of childhood abuse/neglect and the lowest and highest BMI categories. Moreover, we found notable sex differences to the effect that for women, childhood emotional neglect was linked to severe obesity, eliciting a possible mechanism behind women’s higher vulnerability towards eating disorders. For men, this connection could not be confirmed. Instead, in men physical neglect was linked to being underweight. Consequently, future research should aim to clarify the pathways of emotional neglect and eating disorders and weight extremes in men and women alike. Both prevention and treatment approaches could benefit from this knowledge.
Methods
Participants
From September to November 2016, a representative sample of the German population was surveyed by the demographic consulting company USUMA (based in Berlin, Germany). Participants were chosen via a random route procedure. To be included, individuals had to be 14 years of age or older and to have sufficient understanding of the German language. The final sample used in the present investigation was representative of the German population regarding age, sex, and geographic region. Out of 4,902 designated addresses, 2,510 households participated. Persons in multi-person households were randomly selected using a Kish-Selection-Grid. All participants provided informed consent. In the case of minors, participants gave informed assent with informed consent being provided by their parents/legal guardians. Responses were anonymous. Socio-demographic information was obtained in an interview-format by the research staff and all other information was provided via a questionnaire (handed out with by a sealable envelope). Completed questionnaires were linked to respondent’s demographic data without containing any identifying information. The study was conducted in accordance with the Declaration of Helsinki, and fulfilled the ethical guidelines of the International Code of Marketing and Social Research Practice of the International Chamber of Commerce and of the European Society of Opinion and Marketing Research. The study was approved by the Ethics Committee of the Medical Department of the University of Leipzig. In total, 2,510 individuals took part (1,171 men and 1,339 women).
Measurements
Childhood trauma was measured using the Childhood Trauma Questionnaire (CTQ). The CTQ comprises five subscales: emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse. Each of the 28 items (e.g. “I had to wear dirty clothes”, assessing physical neglect) is scored on a five-point Likert scale (ranging from 1 = never to 5 = very often). The CTQ has been widely used in community samples as well as in clinical practice and research. Klinitzke, et al.5 confirmed its 5-factor-structure and attested to its good internal consistencies ranging from Cronbach’s α = 0.62–0.96. Cut-off scores used in this investigation follow norms provided by Häuser, et al.45 (rating each type of maltreatment “none-minimal”, “minimal-moderate”, “moderate-severe”, or “severe-extreme”). For the present investigation, these categories were transformed into dichotomous variables indicating the presence (i.e. at least moderate-severe scores) of physical and emotional neglect. The 4-item-version of the Patient Health Questionnaire (PHQ-4) was used to measure mental distress65. As a widely used 4-item screening tool of anxiety and depression, it combines GAD-2 and PHQ-2. It begins with the question: “Over the last 2 weeks, how often have you been bothered by the following problems?”. Response options range from 0 = not at all to 3 = nearly every day, yielding a sum score from 0 to 12. Bodyweight categories were calculated according to the WHO’s criteria defining underweight as a BMI (kg/m2) < 18.5, and severe obesity as a BMI >= 3566.
We calculated equivalised income according to the OECD guideline67 by dividing the household income through the square root of people in household. The result was then recoded into the following categories: 1 =< 1250€, 2 = 1250–2500€, 3 => 2500€.
Statistical analyses
P-values correspond to two-tailed tests. Confidence intervals (CIs) are reported for Odds Ratios (OR) and regression coefficients. Analyses were carried out using SPSS for Windows 24 and the Process Macro by Andrew F. Hayes68. We conducted sex-specific binary logistic regressions to test the associations of emotional and physical neglect as assessed by the CTQ and severe obesity/underweight, controlling for age, equivalised income, and the presence of other types of childhood trauma as measured by the CTQ and classified by the proposed cut-offs45. We subsequently used a second-stage moderated mediation model (Fig. 1) to ascertain links between emotional neglect, mental distress, and BMI while testing whether this relation was different in men and women. In this model (e.g. described by Edwards and Lambert69, the moderator (sex) affects the magnitude of the mediator’s (mental distress) partial association with the outcome (BMI). We entered age, equivalised income, and the sum of the other four CTQ-subscales into the model as covariates. We focused on emotional neglect as a predictor as we aimed to statistically test effects of parental disregard or contempt. For these purposes, researchers have previously cautioned against the interpretation of the physical neglect scale on its own in samples comprising older individuals who lived through/shortly after WWII: At that time, not being provided clean clothing or sufficient amounts of food might have been commonplace and not related to parental neglect45.
Acknowledgements
We thank all participants and staff involved in data retrieval and management. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit-sectors. JMF has received research funding from the EU, DFG (German Research Foundation), BMG (Federal Ministry of Health), BMBF (Federal Ministry of Education and Research), BMFSFJ (Federal Ministry of Family, Senior Citizens, Women and Youth), German armed forces, several state ministries of social affairs, State Foundation Baden-Württemberg, Volkswagen Foundation, European Academy, Pontifical Gregorian University, RAZ, CJD, Caritas, Diocese of Rottenburg-Stuttgart. Moreover, he received travel grants, honoraria and sponsoring for conferences and medical educational purposes from DFG, AACAP, NIMH/NIH, EU, Pro Helvetia, Janssen-Cilag (J&J), Shire, several universities, professional associations, political foundations, and German federal and state ministries during the last five years. Every grant and every honorarium has to be declared to the law office of the University Hospital Ulm. PLP has received research funding from the German Federal Institute for Drugs and Medical Devices (BfARM), the German Federal Ministry of Education and Research (BMBF), VW-Foundation, Baden-Württemberg Stiftung, Lundbeck and Servier. No author holds stocks of pharmaceutical companies.
Author Contributions
All authors have made substantial contributions to this work and have read and approved the final manuscript as submitted. They agree to be accountable for all aspects of the work. All authors were involved in conceiving and designing the study and interpreting the data. M.E. analysed the data. M.E., A.N.T., A.W., M.E.B. and E.B. drafted the article. J.M.F. and P.L.P. revised the article for important intellectual content.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Felitti VJ, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert R, et al. Burden and consequences of child maltreatment in high-income countries. The Lancet. 2009;373:68–81. doi: 10.1016/s0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 3.van der Kolk, B. The body keeps the score. Mind, brain and body in the transformation of trauma. (Penguin Books, 2014).
- 4.Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, van Ijzendoorn MH. The Prevalence of Child Maltreatment across the Globe: Review of a Series of Meta-Analyses. Child Abuse Review. 2015;24:37–50. doi: 10.1002/car.2353. [DOI] [Google Scholar]
- 5.Klinitzke G, Romppel M, Häuser W, Brähler E, Glaesmer H. The German Version of the Childhood Trauma Questionnaire (CTQ): psychometric characteristics in a representative sample of the general population. Psychotherapie, Psychosomatik, medizinische Psychologie. 2012;62:47–51. doi: 10.1055/s-0031-1295495. [DOI] [PubMed] [Google Scholar]
- 6.Witt A, Brown RC, Plener PL, Brähler E, Fegert JM. Child maltreatment in Germany: prevalence rates in the general population. Child Adolesc Psychiatry Ment Health. 2017;11:47. doi: 10.1186/s13034-017-0185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mersky JP, Topitzes J. Comparing early adult outcomes of maltreated and non-maltreated children: A prospective longitudinal investigation. Child Youth Serv Rev. 2010;32:1086–1096. doi: 10.1016/j.childyouth.2009.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Widom CS, Czaja SJ, Bentley T, Johnson MS. A prospective investigation of physical health outcomes in abused and neglected children: new findings from a 30-year follow-up. Am J Public Health. 2012;102:1135–1144. doi: 10.2105/AJPH.2011.300636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herrenkohl TI, Herrenkohl RC. Examining the Overlap and Prediction of Multiple Forms of Child Maltreatment, Stressors, and Socioeconomic Status: A Longitudinal Analysis of Youth Outcomes. Journal of Family Violence. 2007;22:553–562. doi: 10.1007/s10896-007-9107-x. [DOI] [Google Scholar]
- 10.Weich S, Patterson J, Shaw R, Stewart-Brown S. Family relationships in childhood and common psychiatric disorders in later life: systematic review of prospective studies. Br J Psychiatry. 2009;194:392–398. doi: 10.1192/bjp.bp.107.042515. [DOI] [PubMed] [Google Scholar]
- 11.Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child abuse & neglect. 2008;32:607–619. doi: 10.1016/j.chiabu.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Danese A, Pariante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. Proc Natl Acad Sci USA. 2007;104:1319–1324. doi: 10.1073/pnas.0610362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Reedt Dortland AK, Giltay EJ, van Veen T, Zitman FG, Penninx BW. Personality traits and childhood trauma as correlates of metabolic risk factors: the Netherlands Study of Depression and Anxiety (NESDA) Prog Neuropsychopharmacol Biol Psychiatry. 2012;36:85–91. doi: 10.1016/j.pnpbp.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Widom CS, Horan J, Brzustowicz L. Childhood maltreatment predicts allostatic load in adulthood. Child abuse & neglect. 2015;47:59–69. doi: 10.1016/j.chiabu.2015.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 16.Johnson JG, Cohen P, Kasen S, Brook JS. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. The American journal of psychiatry. 2002;159:394–400. doi: 10.1176/appi.ajp.159.3.394. [DOI] [PubMed] [Google Scholar]
- 17.Molendijk, M. L., Hoek, H. W., Brewerton, T. D. & Elzinga, B. M. Childhood maltreatment and eating disorder pathology: a systematic review and dose-response meta-analysis. Psychol Med, 1–15, 10.1017/S0033291716003561 (2017). [DOI] [PubMed]
- 18.Guillaume S, et al. Associations between adverse childhood experiences and clinical characteristics of eating disorders. Sci Rep. 2016;6:35761. doi: 10.1038/srep35761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014;19:544–554. doi: 10.1038/mp.2013.54. [DOI] [PubMed] [Google Scholar]
- 20.Beutel TF, Zwerenz R, Michal M. Retrospektiv berichtete Kindheitstraumatisierung und Gesundheitsverhalten im Erwachsenenalter von psychosomatischen Patienten. Z PsychosomMed Psychother. 2016;62:306–321. doi: 10.13109/zptm.2016.62.4.306. [DOI] [PubMed] [Google Scholar]
- 21.Wonderlich SA, et al. Eating disturbance and sexual trauma in childhood and adulthood. Int J Eat Disord. 2001;30:401–412. doi: 10.1002/eat.1101. [DOI] [PubMed] [Google Scholar]
- 22.Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord. 2002;26:1075–1082. doi: 10.1038/sj.ijo.0802038. [DOI] [PubMed] [Google Scholar]
- 23.Brewerton TD, Rance SJ, Dansky BS, O’Neil PM, Kilpatrick DG. A comparison of women with child-adolescent versus adult onset binge eating: results from the National Women’s Study. Int J Eat Disord. 2014;47:836–843. doi: 10.1002/eat.22309. [DOI] [PubMed] [Google Scholar]
- 24.Norman RE, et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9:e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jaite C, et al. Etiological role of childhood emotional trauma and neglect in adolescent anorexia nervosa: a cross-sectional questionnaire analysis. Psychopathology. 2012;45:61–66. doi: 10.1159/000328580. [DOI] [PubMed] [Google Scholar]
- 26.Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- 27.Racine SE, Wildes JE. Emotion dysregulation and anorexia nervosa: an exploration of the role of childhood abuse. Int J Eat Disord. 2015;48:55–58. doi: 10.1002/eat.22364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moulton SJ, Newman E, Power K, Swanson V, Day K. Childhood trauma and eating psychopathology: a mediating role for dissociation and emotion dysregulation? Child abuse & neglect. 2015;39:167–174. doi: 10.1016/j.chiabu.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Kong S, Bernstein K. Childhood trauma as a predictor of eating psychopathology and its mediating variables in patients with eating disorders. J Clin Nurs. 2009;18:1897–1907. doi: 10.1111/j.1365-2702.2008.02740.x. [DOI] [PubMed] [Google Scholar]
- 30.Afifi TO, et al. Child maltreatment and eating disorders among men and women in adulthood: Results from a nationally representative United States sample. Int J Eat Disord. 2017;50:1281–1296. doi: 10.1002/eat.22783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schore, A. N. Affect Regulation and the Origin of the Self. The Neurobiology of EmotionalDevelopment. (Routledge, 2015).
- 32.Brown RC, et al. The impact of child maltreatment on non-suicidal self-injury: data from a representative sample of the general population. BMC psychiatry. 2018;18:181. doi: 10.1186/s12888-018-1754-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harrison A, Sullivan S, Tchanturia K, Treasure J. Emotional functioning in eating disorders: attentional bias, emotion recognition and emotion regulation. Psychological Medicine. 2010;40:1887–1897. doi: 10.1017/s0033291710000036. [DOI] [PubMed] [Google Scholar]
- 34.Fox JR, Power MJ. Eating disorders and multi-level models of emotion: an integrated model. Clin Psychol Psychother. 2009;16:240–267. doi: 10.1002/cpp.626. [DOI] [PubMed] [Google Scholar]
- 35.Nemeroff CB. Paradise Lost: The Neurobiological and Clinical Consequences of Child Abuse and Neglect. Neuron. 2016;89:892–909. doi: 10.1016/j.neuron.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 36.Teicher MH, Samson JA. Annual Research Review: Enduring neurobiological effects of childhood abuse and neglect. Journal of child psychology and psychiatry, and allied disciplines. 2016;57:241–266. doi: 10.1111/jcpp.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim S, Kim JS, Shim M, Im CH, Lee SH. Altered cortical functional network during behavioral inhibition in individuals with childhood trauma. Sci Rep. 2018;8:10123. doi: 10.1038/s41598-018-28329-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leehr EJ, et al. Emotion regulation model in binge eating disorder and obesity–a systematic review. Neurosci Biobehav Rev. 2015;49:125–134. doi: 10.1016/j.neubiorev.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 39.Briere J, Scott C. Assessment of trauma symptoms in eating-disordered populations. Eat Disord. 2007;15:347–358. doi: 10.1080/10640260701454360. [DOI] [PubMed] [Google Scholar]
- 40.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:Joba.0000007455.08539.94. [DOI] [Google Scholar]
- 41.Johnson PO, Fay LC. The Johnson-Neyman technique, its theory and application. Psychometrika. 1950;15:349–367. doi: 10.1007/BF02288864. [DOI] [PubMed] [Google Scholar]
- 42.Nilsson D, Dahlstom O, Priebe G, Svedin CG. Polytraumatization in an adult national sample and its association with psychological distress and self-esteem. Brain and behavior. 2015;5:62–74. doi: 10.1002/brb3.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hanson JL, Hariri AR, Williamson DE. Blunted Ventral Striatum Development in Adolescence Reflects Emotional Neglect and Predicts Depressive Symptoms. Biological psychiatry. 2015;78:598–605. doi: 10.1016/j.biopsych.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bentley T, Widom CS. A 30-year follow-up of the effects of child abuse and neglect on obesity in adulthood. Obesity (Silver Spring, Md.) 2009;17:1900–1905. doi: 10.1038/oby.2009.160. [DOI] [PubMed] [Google Scholar]
- 45.Häuser W, Schmutzer G, Brähler E, Glaesmer H. Maltreatment in childhood and adolescence: results from a survey of a representative sample of the German population. Dtsch Arztebl Int. 2011;108:287–294. doi: 10.3238/arztebl.2011.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kent A, Waller G. Childhood emotional abuse and eating psychopathology. Clinical Psychology Review. 2000;20:887–903. doi: 10.1016/s0272-7358(99)00018-5. [DOI] [PubMed] [Google Scholar]
- 47.Young JC, Widom CS. Long-term effects of child abuse and neglect on emotion processing in adulthood. Child abuse & neglect. 2014;38:1369–1381. doi: 10.1016/j.chiabu.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cloitre, M., Cohen, L. R. & Koenen, K. C. Treating Survivors of Childhood Abuse: Psychotherapy for the InterruptedLife. (The Guilford Press, 2006).
- 49.Matud MP. Gender differences in stress and coping styles. Personality and Individual Differences. 2004;37:1401–1415. doi: 10.1016/j.paid.2004.01.010. [DOI] [Google Scholar]
- 50.Nolen-Hoeksema S, Aldao A. Gender and age differences in emotion regulation strategies and their relationship to depressive symptoms. Personality and Individual Differences. 2011;51:704–708. doi: 10.1016/j.paid.2011.06.012. [DOI] [Google Scholar]
- 51.Gowin JL, Sloan ME, Stangl BL, Vatsalya V, Ramchandani VA. Vulnerability for Alcohol Use Disorder and Rate of Alcohol Consumption. The American journal of psychiatry. 2017;174:1094–1101. doi: 10.1176/appi.ajp.2017.16101180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sulkowski ML, Dempsey J, Dempsey AG. Effects of stress and coping on binge eating in female college students. Eat Behav. 2011;12:188–191. doi: 10.1016/j.eatbeh.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 53.Kuehner C. Why is depression more common among women than among men? The Lancet Psychiatry. 2017;4:146–158. doi: 10.1016/s2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 54.Pollatos O, et al. Reduced perception of bodily signals in anorexia nervosa. Eat Behav. 2008;9:381–388. doi: 10.1016/j.eatbeh.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 55.De Zwaan M, et al. Eating related and general psychopathology in obese females with binge eating disorder. International Journal of Eating Disorders. 1994;15:43–52. doi: 10.1002/1098-108x(199401)15:1<43::aid-eat2260150106>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 56.Aust S, Härtwig EA, Heuser I, Bajbouj M. The role of early emotional neglect in alexithymia. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:225–232. doi: 10.1037/a0027314. [DOI] [Google Scholar]
- 57.Kerr KL, et al. Altered Insula Activity during Visceral Interoception in Weight-Restored Patients with Anorexia Nervosa. Neuropsychopharmacology. 2016;41:521–528. doi: 10.1038/npp.2015.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stevens JS, et al. Childhood Maltreatment Predicts Reduced Inhibition-Related Activity in the Rostral Anterior Cingulate in Ptsd, but Not Trauma-Exposed Controls. Depression and anxiety. 2016;33:614–622. doi: 10.1002/da.22506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Silbersweig D, et al. Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. The American journal of psychiatry. 2007;164:1832–1841. doi: 10.1176/appi.ajp.2007.06010126. [DOI] [PubMed] [Google Scholar]
- 60.Elton A, et al. Childhood maltreatment is associated with a sex-dependent functional reorganization of a brain inhibitory control network. Hum Brain Mapp. 2014;35:1654–1667. doi: 10.1002/hbm.22280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Leeb, R. T., Paulozzi, L., Melanson, C., Simon, T. & Arias, I. (ed. National Center for Injury Prevention and Control Centers for Disease Control and Prevention) (Atlanta (GA), 2008).
- 62.Fergusson DM, Horwood LJ, Boden JM. Structural equation modeling of repeated retrospective reports of childhood maltreatment. Int J Methods Psychiatr Res. 2011;20:93–104. doi: 10.1002/mpr.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 64.McLaughlin KA, Lambert HK. Child trauma exposure and psychopathology: mechanisms of risk and resilience. Current Opinion in Psychology. 2017;14:29–34. doi: 10.1016/j.copsyc.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Löwe B, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of affective disorders. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 66.World Health Organization. (2018).
- 67.OECD. Divided We Stand: Why Inequality Keeps Rising. (OECD Publishing, 2011).
- 68.Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav Res Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- 69.Edwards JR, Lambert LS. Methods for integrating moderation and mediation: a general analytical framework using moderated path analysis. Psychol Methods. 2007;12:1–22. doi: 10.1037/1082-989X.12.1.1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.