Abstract
Uterine fibroids are common benign tumors seen in women and can be managed with a variety of treatment options, including hysterectomy, myomectomy, and uterine fibroid embolization (UFE). UFE is an acceptable alternative to surgical treatment in well-selected cases and offers the added benefit of decreased hospital stay and avoidance of general anesthesia risk. Like any other procedure, UFE carries risks and complications. Post-UFE fibroid expulsion is one of them.
We present a case of impending fibroid expulsion pre-emptively identified on magnetic resonance imaging at 6-month follow-up after UFE. While the majority of fibroid expulsions occur spontaneously by 3 months post-UFE, delayed expulsions have been reported as late as 4 years following the procedure. Therefore, a high degree of clinical suspicion is paramount for early diagnosis of this complication in UFE patients.
Keywords: Uterine artery embolization, Fibroid expulsion, Submucosal
Introduction
Uterine fibroids are the most common benign uterine tumors in women [1]. Risk factors for uterine fibroids include African-American background, early menarche, and older age [2]. Uterine fibroids are classified based on their location within the uterine wall—submucosal, intramural, subserosal and are termed transmural when involving any combination of the preceding categories. Women may present with a wide range of symptoms including menorrhagia with resultant anemia, bulk symptoms such as urinary urgency, frequency, or incontinence, pelvic pain, and infertility [2]. While magnetic resonance imaging (MRI) offers detailed anatomic localization of the fibroids and can assist in the identification of optimal candidates for uterine fibroid embolization (UFE) [2], the gold standard for diagnosing uterine leiomyomas is still ultrasound. Several treatment options are available including uterine artery embolization, hormonal therapy, myomectomy, and hysterectomy. The first described uterine artery embolization (UAE) procedure dates back to 1995 [3]. Since then, UAE has been shown to be a safe and effective form of treatment for uterine fibroids [4]. Indications are predominantly symptomatic fibroids with menorrhagia, pelvic pain, or bulk symptoms, while contraindications include ongoing pregnancy, pelvic infection or malignancy [5]. The benefits of UFE include shorter recovery time and hospital stay, effective symptomatic treatment of uterine fibroids regardless of number of lesions, and there is no difference in quality of life scores between surgical therapies and UFE [2], [6].
This case brings to attention a delayed complication of UFE-impeding fibroid expulsion preemptively identified on follow-up MRI. Prolapsing uterine fibroids are known complications of UAE/UFE [4], [7], [8]. However, most of them prolapse by three months after the procedure with only a handful of reported cases of delayed expulsion [4]. In this case, the expulsion occurred at six months and was facilitated by office-based forceps removal.
Case report
A 51-year-old female presented with worsening pelvic pain, menorrhagia, and prolonged menses of three-year duration. The patient also reports generalized fatigue and weakness secondary to anemia. Papanicolaou smear and endometrial biopsy were negative. An initial transvaginal ultrasound (TVUS) evaluation of the uterus showed a single 11 × 13 centimeter (cm) fundal fibroid (Fig. 1A). MRI before embolization demonstrated a 15.5 × 8.8 cm submucosal fibroid arising from the anterior uterine fundal aspect (Fig. 2A and B). The enlarged uterus—measuring 16 cm in longitudinal dimension—was deviated to the right and compressing the mid ureter at the pelvic brim with consequent right hydroureteronephrosis. The patient was given the option to either pursue daily progesterone therapy, uterine fibroid embolization or hysterectomy. The patient has used 10 mg medroxyprogesterone acetate daily (for 3 out of 4 weeks every month) that resulted in decreased menorrhagia, but the medication caused her leg weakness, and as a result it had to be discontinued. The patient decided to purse UFE.
Fig. 1.
Ultrasound images of the submucosal fibroid. (A) Initial transverse gray scale transvaginal ultrasound image demonstrating submucosal fibroid measuring 11 × 13 cm. (B) Two weeks follow-up transverse gray scale transvaginal ultrasound image after fibroid expulsion/removal demonstrating residual fibroid tissue measuring 2.17 × 2.16 cm at the uterine fundus with extensive calcifications.
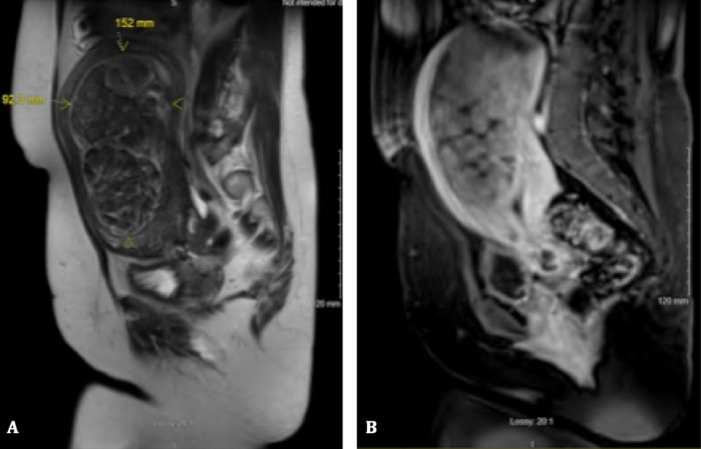
Fig. 2.
Magnetic resonance images (MRI) before uterine artery embolization. (A) T2-weighted sagittal magnetic resonance imaging (MRI) demonstrating large mixed intensity submucosal fibroid. (B) T1-weighted sagittal MRI with contrast demonstrating heterogeneous enhancement of submucosal fibroid.
A Standard UAE was performed where both uterine arteries were embolized using embosphere particles (500-700 microns) followed by embosphere particles (700-900 microns). The procedure was technically successful with occlusion of blood supply to the uterine fibroid (Fig. 3A and B). The patient was admitted overnight for pain management, and was discharged the following day with antibiotics, antiemetics, and pain control medications. At 6-week follow-up, the patient reported significant improvement of her menorrhagia.
Fig. 3.
Digital subtraction angiography (DSA) images during uterine artery embolization procedure. (A) Pre-embolization DSA of the pelvic aorta demonstrating hypertrophic uterine arteries (black arrows). (B) DSA postembolization demonstrating effective embolization of the uterine arteries.
At 6-month follow-up, the patient's MRI demonstrated a 10 × 8 cm submucosal fibroid protruding into a significantly thinned and dilated endocervical canal suggesting impending expulsion (Fig.4A and B). The patient presented to the clinic and reported having on/off vaginal discharge of dark blood and pelvic pain for the last few weeks. On the speculum exam, a large, flesh colored mass was noted to be prolapsing from the cervical os. A ring forceps was utilized to apply gentle twisting traction to remove the mass. The mass was 10 cm in length (Fig. 5). Following the removal, there was a small amount of bleeding and purulent discharge. The patient was discharged with a 7-day course of amoxicillin-clavulanic acid. The pathology report of the mass confirmed it to be a uterine leiomyoma with necrotic and inflammatory changes. On a follow-up TVUS 2 weeks after removal, residual fibroid tissue can seen with internal calcifications at the uterine fundus (Fig. 1B).
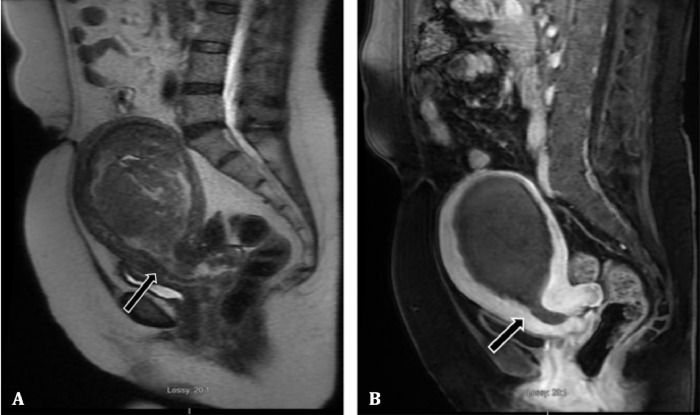
Fig. 4.
Magnetic resonance images (MRI) after uterine artery embolization (UAE). (A) T2-weighted sagittal MRI demonstrating interval decrease in size of the submucosal fibroid. Prolapse of submucosal fibroid into the cervical canal (arrow) with internal os dilation. (B) T1-weighted sagittal MRI demonstrating cervical canal dilation (arrow). No evidence of fibroid enhancement/viability is seen.
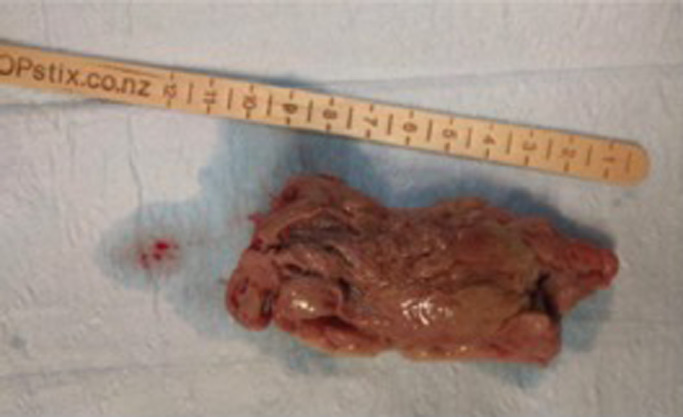
Fig. 5.
Gross specimen of the submucosal fibroid after retrieval measuring 10 cm in length.
Discussion
UFE is a minimally invasive therapeutic option that offers similar clinical and technical success rates as compared to surgical alternatives with the additional benefits of faster recovery time and shorter hospital stay [9]. However, as with any procedure, there are complications that may arise from UFE. Intraoperative complication rates were similar between surgery and UFE, with a greater incidence of minor complications for the latter that could potentially be attributed to the experience level of physicians performing it [9]. However, requirement of blood transfusion was significantly lower in UFE compared to surgery [9].
Complications seen in the immediate postprocedural period are related to the vascular access site, including access site hematoma, infection, arterial dissection, and postembolization syndrome [7]. Major complications include pulmonary embolism, uterine ischemia and subsequent necrosis, sepsis related to endometritis, and death [7]. Expulsion of fibroid tissue post-UFE has been reported to be a common complication occurring in 1%-10% of the cases, and up to 50% of submucosal fibroids in 1 reported study [8]. Major complication rate in a large meta-analysis was reported to be 2.9% with an average rate of fibroid expulsion of 4.7% [10].
Predominantly submucosal or transmural fibroids with volumes less than 66 mL are at a greater risk for undergoing expulsion [4], [8]. The average time reported for fibroid expulsion after UFE is approximately 15 weeks, with majority of them taking place before 3 months [4]. Some expulsions have been noted within days after the procedure while others have been as late as 50 months afterwards [4], [11]. The average size of expelled fibroids is approximately 8 cm [4].
Prior to fibroid expulsion, patients may present with new onset vaginal discharge, bleeding, fever, and pelvic pain [4]. Fibroid expulsion post-UFE can be managed either by observation, forceps or hysteroscopic removal, transvaginal myomectomy, and hysterectomy [4]. The need for hysterectomy is primarily determined by the presence of endometritis and sepsis unresponsive to conservative management. This is more common in nulliparous females, as cervical dilation occurs more efficiently to facilitate expulsion of fibroid tissue in parous females [4]. Following fibroid expulsion, majority of the patients do well, with only a few reported complications of uterine sepsis and uteroenteric fistulae [11], [12].
Necrosed fibroid tissue is either absorbed by the myometrium or expelled via the cervical os. It has been proposed that expulsion of the fibroid tissue occurs as a result of uterine contractions in response to inflammatory reaction from fibroid tissue necrosis [12]. This is likely more common in fibroids with a submucosal component [12].
This case brings to light one of the delayed complications of UAE/UFE—impending fibroid expulsion, with succinct depiction of cervical dilation and necrotic tissue prolapse on MRI prompting office-based removal at 6-month follow-up.
In conclusion, fibroid expulsion is a rather common complication after UAE/UFE and high clinical suspicion is necessary during the follow-up period even at the 6-month follow-up interval. Our case clearly depicts the findings of impeding fibroid expulsion on MRI, adding rather unique images to the literature, and may help other providers pursue more immediate intervention when faced with similar situations.
References
- 1.Martins J.G., Gaudenti D., Crespo F., Ganesh D., Verma U. Uncommon complication of uterine artery embolization: expulsion of infarcted myoma and uterine sepsis. Case Rep Obstet Gynecol. 2016;2016:8695318. doi: 10.1155/2016/8695318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Donnez J., Dolmans M.M. Uterine fibroid management: from the present to the future. Human Reproductive Update. 2016;22:665–686. doi: 10.1093/humupd/dmw023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ravina J.H., Herbreteau D., Ciraru-Vigneron N., Bouret J.M., Houdart E., Aymard A., Merland J.J. Arterial embolisation to treat uterine myomata. Lancet. 1995;346:671–672. doi: 10.1016/s0140-6736(95)92282-2. [DOI] [PubMed] [Google Scholar]
- 4.Shlansky-Goldberg R.D., Coryell L., Stavropoulos S.W., Trerotola S.O., Mondschein J., Beshara M., Butts S.F., Sondheimer S., Turek R.W., Rosen M. Outcomes following fibroid expulsion after uterine fibroid embolization. J Vasc Int Radiol. 2011;22:1586–1593. doi: 10.1016/j.jvir.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Cura M., Cura A., Bugnone A. Role of magnetic resonance imaging in patient selection for uterine artery embolization. Acta Radiologica. 2006;47:1105–1114. doi: 10.1080/02841850600965047. [DOI] [PubMed] [Google Scholar]
- 6.Moss J.G., Cooper K.G., Khaund A., Murray L.S., Murray G.D., Wu O., Craig L.E., Lumsden M.A. Randomised comparison of uterine artery embolisation (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5 year results. BJOG. 2011;118:936–944. doi: 10.1111/j.1471-0528.2011.02952.x. [DOI] [PubMed] [Google Scholar]
- 7.Schirf B.E., Vogelzang R.L., Chrisman H.B. Complications of uterine fibroid embolization. Semin Intervent Radiol. 2006;23:143–149. doi: 10.1055/s-2006-941444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Radeleff B., Eiers M., Bellemann N., Ramsauer S., Rimbach S., Kauczor H.U., Richter G.M. Expulsion of dominant submucosal fibroids after uterine artery embolization. Eur J Radiol. 2010;75:57–63. doi: 10.1016/j.ejrad.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 9.Spies J. Current role of uterine artery embolization in the management of uterine fibroids. Clin Obstet Gynecol. 2016;59:93–102. doi: 10.1097/GRF.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 10.Toor S.S., Jaberi A., Macdonald D.B., McInnes M.D., Schweitzer M.E., Rasuli P. Complication rates and effectiveness of uterine artery embolization in the treatment of symptomatic leiomyomas: a systematic review and meta-analysis. AJR. 2012;199:1153–1163. doi: 10.2214/AJR.11.8362. [DOI] [PubMed] [Google Scholar]
- 11.Marret H., Keris Y.L.B., Acker O., Cottier J.P., Herbreteau D. Late leiomyoma expulsion after uterine artery embolization. JVIR. 2004;15:1483–1485. doi: 10.1097/01.RVI.0000141445.13873.7D. [DOI] [PubMed] [Google Scholar]
- 12.Gutierrez L.B., Bansal A.K., Hovsepian D.M. Uteroenteric fistula resulting from fibroid expulsion after uterine fibroid embolization: case report and review of the literature. Cardiovasc Intervent Radiol. 2012;35:1231–1236. doi: 10.1007/s00270-011-0318-4. [DOI] [PubMed] [Google Scholar]