Abstract
Treating mycotic aortic aneurysm with thoracic endovascular aortic repair (TEVAR) remains controversial because of sustained infection post-treatment. In this study, an 83-year-old man, who had a ruptured mycotic thoracic aortic aneurysm, underwent salvage TEVAR. However, because an abscess appeared in the aneurysm on follow-up computed tomography, video-assisted thoracoscopic debridement (VATD) followed by continuous drainage was performed next and was successful in eliminating the infection from the abscess. Although frozen elephant trunk and proximal aortic arch repair were further required owing to another pseudoaneurysm, there was no sign of recurrent infection thereafter. The combination of TEVAR and VATD can be effective in treatment of mycotic aortic diseases in selected patients.
Keywords: mycotic aortic aneurysm, stent-graft, video-assisted thoracoscopic debridement
Introduction
Mycotic aortic aneurysm is a life-threatening condition in which the early mortality rate associated with traditional surgery can be as high as 43%.1) The standard treatment for mycotic aortic aneurysm includes antibiotic therapy, surgical debridement, and restoration of vascular continuity. However, most patients with mycotic aneurysms have significant comorbidities, which result in there being a lethal risk for major surgery. Alternatively, thoracic endovascular aortic repair (TEVAR) has been applied for aortic infections as emergency therapy and has appeared feasible in selected cases.2) However, controversy remains as to whether local infection can be controlled after TEVAR. We herein report a case of ruptured mycotic thoracic aortic aneurysm treated with emergency TEVAR followed by local debridement using a video-assisted thoracoscopic surgery technique, i.e., video-assisted thoracoscopic debridement (VATD), to control a remaining infection.
Case Report
An 83-year-old man presented with a complaint of chest pain. He had undergone a right pulmonary lower lobectomy for lung cancer 3 years previously, and he was taking several drugs daily to treat hypertension and diabetes. Upon arrival at the emergency room in Ise Red Cross Hospital, the patient had a high fever reaching 39.6°C and hypoxia with saturation of percutaneous oxygen of 89% that necessitated oxygen inhalation. His blood pressure was 140/80 mmHg at the time of presentation but gradually deteriorated thereafter. Computed tomography (CT) showed a ruptured aortic aneurysm located at the proximal descending aorta with extensive mediastinal hematoma (Figs. 1A–1E). Laboratory testing revealed an increased peripheral leukocyte count of 11,500 cells/mm3 and an elevated C-reactive protein level of 7.7 mg/dL. A sustained high-grade fever and elevated inflammatory response in his laboratory testing pointed to underlying aortic infection. Because the patient’s condition was too severe to undergo surgical debridement and reconstruction of the diseased aorta, we performed emergency TEVAR to salvage the patient upon arrival. Under general anesthesia, the left common femoral artery, exposed through an inguinal incision, was used as the remote access vessel. Preoperative CT showed that the aneurysm was present as a pseudoaneurysm with a 12 mm orifice and 62 mm maximal diameter. The proximal landing zone, i.e., the distance between the left subclavian artery and the orifice of the pseudoaneurysm, was estimated to be 27 mm, and the diameter of the proximal neck was 30 mm. Initial aortography confirmed the orifice of the aneurysm to be distal to the left subclavian artery, in agreement with the preoperative CT finding. Of the c-TAG (W. L. Gore & Assoc., Flagstaff, AZ, USA), 34×150 mm was carefully advanced over the stiff wire and deployed with the proximal edge of the stent-graft positioned just distal to the left subclavian artery. Consequently, the distal edge of the stent-graft was located at the level of Th8 and 11 cm of distal sealing distance was obtained. However, because the proximal type 1 endoleak persisted after balloon dilatation at the proximal landing zone, another stent-graft of Zenith TX2 (Cook, Bloomington, IN, USA) for proximal extension (34×77 mm) was deployed by overlapping on the proximal side of the c-TAG to reinforce the proximal sealing. Finally, the completion angiogram showed no evidence of an endoleak, resulting in complete thrombosis of the aneurysm without any leakage of blood. Empirical administration of ceftriaxone sodium and vancomycin hydrochloride was started simultaneous to TEVAR. After a blood culture test detected methicillin-sensitive Staphylococcus aureus (MSSA) as a pathogen of the mycotic aneurysm, only ceftriaxone sodium was continued. Although the blood culture test turned negative soon afterward, follow-up CT examination revealed an abscess developing within the aneurysm 2 weeks after TEVAR (Figs. 1F–1J). We further performed local debridement and implanted a drainage catheter using a video-assisted thoracic surgery technique (Figs. 2A–2D). The operation was performed under general anesthesia with differential lung ventilation. Two ports were used to operate instruments and one was used for a thoracoscope. Firstly, the aneurysm was visualized after detaching the adhesive surrounding tissue and lung. The abscess was entirely capsulized below the aneurysmal wall, and there was no finding of infection outside of the aneurysm (Fig. 2A). Secondly, the aneurysm was partially opened in the middle. There were old thrombi and necrotic tissue inside, but no endoleak was recognized. The infected tissue was carefully excised so as not to cause blood leakage between the stent-graft and the native aorta. Consequently, the stent-graft was partially exposed after sufficient debridement, but no blood leakage occurred (Figs. 2B and 2C). MSSA, which is the same strain as that detected in the previous blood culture test, was recognized by culture test of the excised tissue. Finally, a 5 mm silicon catheter from the SB VAC™ drainage kit (Sumitomo Bakelite Co., Ltd., Tokyo, Japan) was placed in the cavity of the aneurysm, led out through the chest wall and connected to a portable low-pressure suction bottle from the SB VAC™ (Fig. 2D). Drainage was continued postoperatively with pressure of between −50 and −100 cm H2O. No recurrence of the abscess was seen afterward and culture tests of the discharge from the drainage catheter became negative at 10 days after the VATD. During the following 2 weeks, the patient’s condition remained uneventful and inflammatory response in his laboratory testing was decreased with a peripheral leukocyte count of 7,500 cells/mm3 and a C-reactive protein level of 0.7 mg/dL. However, another pseudoaneurysm developed at the proximal edge of the stent-graft because of its erosion (Figs. 2E–2I). As the proximal sealing distance was too short to treat the pseudoaneurysm with additional TEVAR, we performed a surgical stent-graft insertion, i.e., frozen elephant trunk (FET) technique, combined with a proximal aortic arch repair through the median sternotomy. The patient was placed on cardiopulmonary bypass and was cooled to moderate hypothermia (25°C). During the circulatory arrest combined with selective cerebral perfusion, the ascending aorta and aortic arch were opened and inspected. The pseudoaneurysm was located at the greater curvature of the aortic arch just distal to the left subclavian artery, and it originated from the proximal edge of the previously inserted stent-graft, which had eroded through the aorta. The aortic arch was dissected at the proximal level of the left carotid artery, and the orifice of the left carotid artery was closed. A 33 mm diameter of J Graft open stent-graft (Japan Lifeline Co., Ltd., Tokyo, Japan), which has 9 cm stented part, was inserted 12 cm distally into the previous stent-graft (FET technique), which covered the pseudoaneurysm with a 5 cm distal landing zone, and was then fixed to the aortic wall by a 3-0 polypropylene running suture followed by end-to-end distal anastomosis with an additional four-branched fabricated graft (J graft Shield Neo; Japan Lifeline Co., Ltd., Tokyo, Japan). After distal perfusion was restarted from a branch of the graft, proximal anastomosis was performed at the level of the sinotubular junction. The brachiocephalic artery and left carotid artery were then individually reconstructed with branches of the graft. Finally, the third branch of the graft was anastomosed with the graft that was already sewn to the left axillary artery and which led to the mediastinum through the left thoracic cavity. The proximal left subclavian artery was occluded percutaneously with 12 mm diameter of AMPLATZER™ Vascular Plug II (Abbott Medical Japan Co., Ltd., Tokyo, Japan) before this operation, in event that the left subclavian artery was involved in severe inflammation and adhesion around the pseudoaneurysm. There was therefore no need to manipulate the proximal left subclavian artery at the time of the operation. The patient was easily weaned from the cardiopulmonary bypass. Hemostasis of the operative field was ensured, and the chest was closed. The patient was transferred to the intensive care unit in a stable hemodynamic state. By the following morning, he was awake and was extubated with no neurological deficits, and his postoperative course was uneventful thereafter. Intravenous administration of ceftriaxone was continued for 2 weeks after the final operation, after which the oral cephalexin was prescribed and was continued for a further 6 months. The drainage catheter was removed 2 months after the final operation when the discharge discontinued. No further aneurysm or abscess was detected in a one-year postoperative CT (Fig. 3).
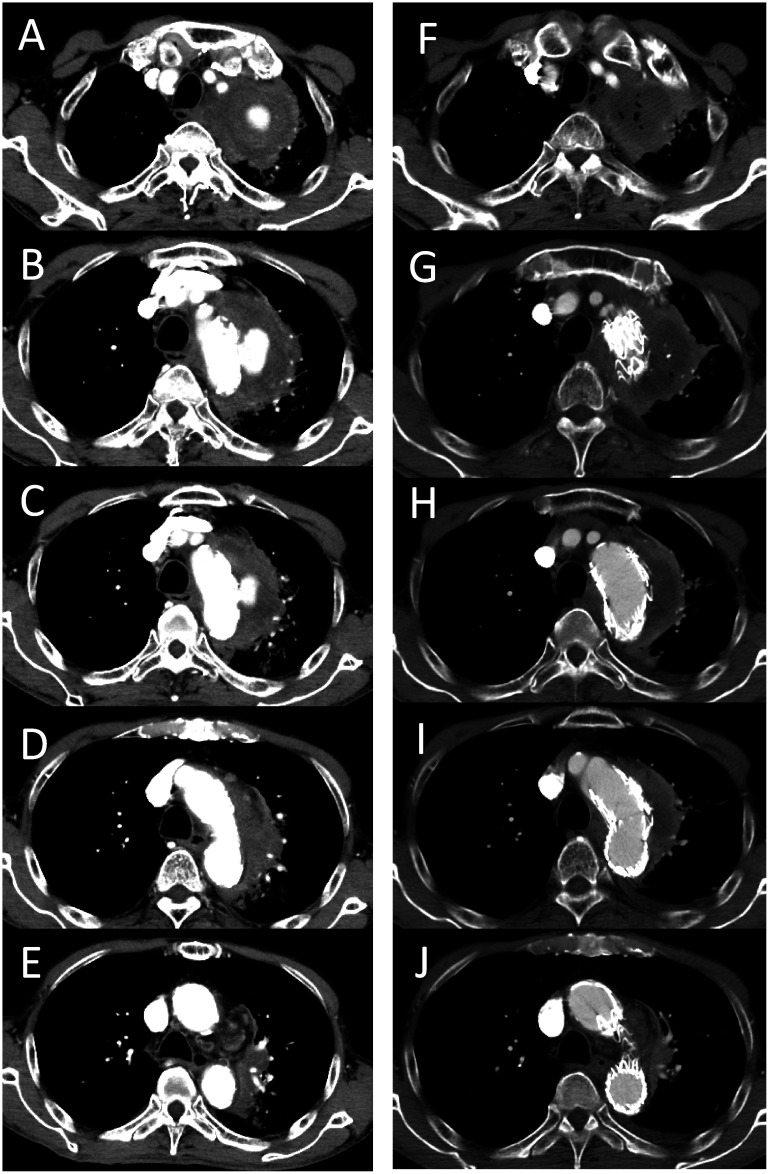
Fig. 1 Computed tomography series before and after thoracic endovascular aortic repair (TEVAR) for the ruptured mycotic aortic aneurysm.
(A–E) Before TEVAR, a pseudoaneurysm is located at the distal aortic arch and is surrounded by a hematoma. (F–J) No leakage was seen after TEVAR, while the aneurysm was replaced with an abscess containing air.
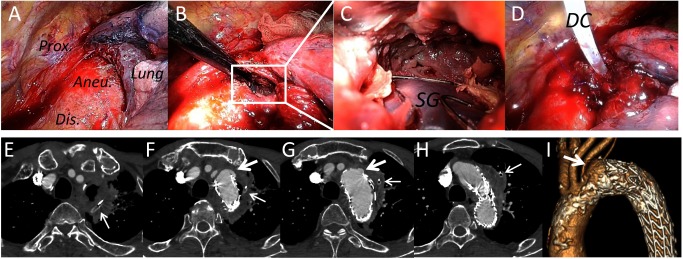
Fig. 2 Video-assisted thoracoscopic debridement for delayed abscess after thoracic endovascular aortic repair.
(A–D) Thoracoscopic findings at the time of the debridement. (A) Overview of the aneurysm located on the aortic arch. (B) The aneurysm was partially opened at the middle (white square). (C) Enlarged view inside the aneurysm. Infected tissue around the stent-graft (SG) was sufficiently excised, and thus the stent-graft was partially exposed. (D) A drainage catheter (DC) was placed in the cavity of the aneurysm after the debridement. (E–I) Computed tomography following the debridement. A delayed pseudoaneurysm appeared at the proximal edge of the stent-graft (large arrows). Small arrows: drainage catheter.
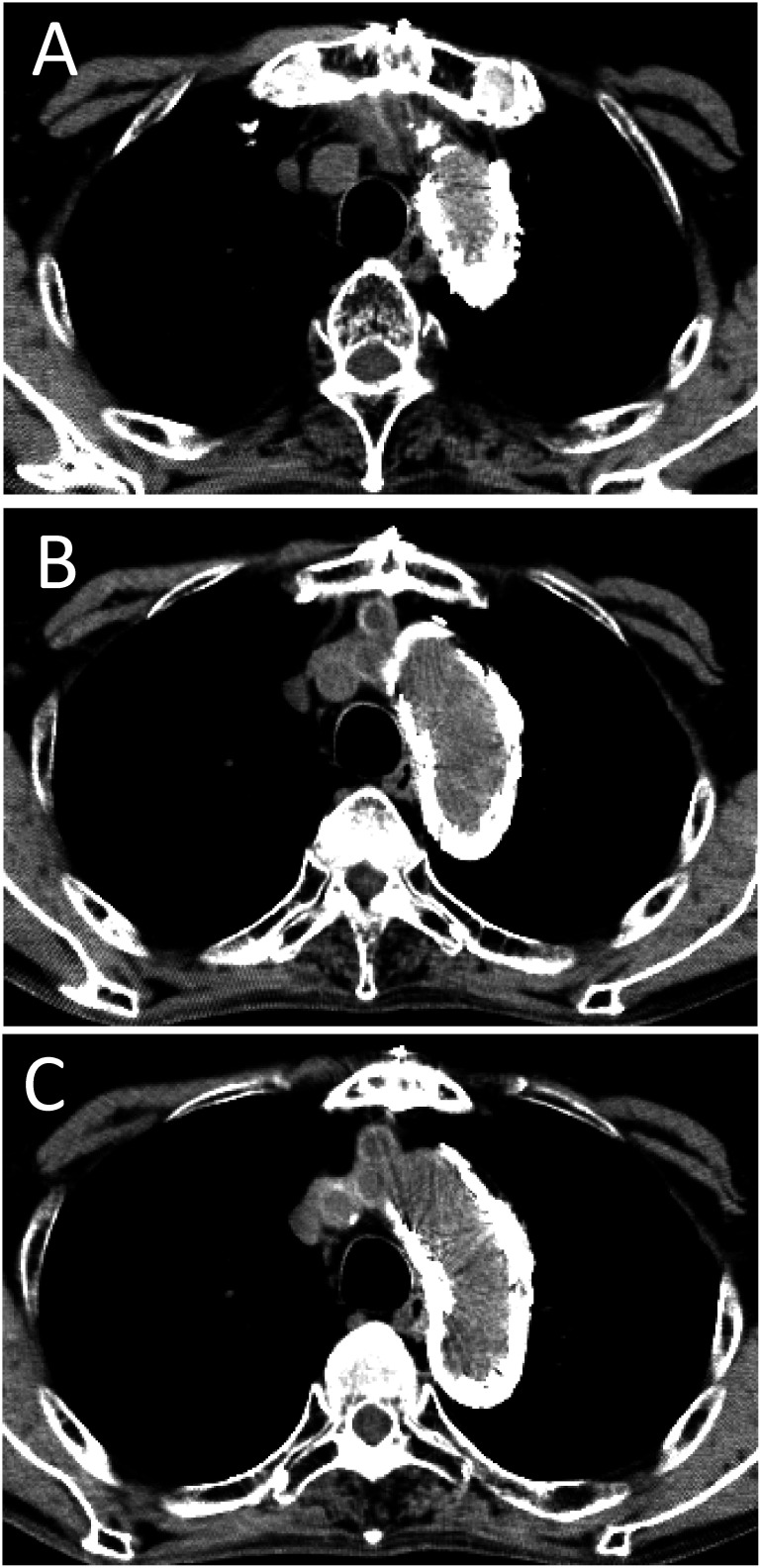
Fig. 3 Computed tomography after all treatments (1-year follow-up).
(A–C) The mycotic aneurysm was completely obliterated and there is no evidence of the infection.
Discussion
Mycotic aortic aneurysms are associated with a high risk of rupture if not treated promptly. The use of stent-grafts for mycotic aortic aneurysms simplifies the procedure and may provide a good alternative to conventional surgical repair for this critical condition. However, a problem with this treatment is that infected tissue that remains after TEVAR might cause sustained infection and might even result in a disastrous aortic rupture. Razavi MK and Razavi MD in their review article reported 91 cases of mycotic aneurysm treated with stent-grafts, with the early mortality rate shown to be low at 5.6%, while incidences of late aneurysm-related mortality and complications were relatively high at 12.2% and 7.8%, respectively.1) Accordingly, the essential factor in obtaining a better outcome seems to be controlling local infection after TEVAR. From this point of view, it seems reasonable to establish local drainage to reduce the amount of bacteria and to attenuate the infection, especially in cases that are complicated with abscess after TEVAR. Chino et al. in their study described two cases of infected abdominal aortic aneurysms successfully treated with the combination of endovascular aneurysm repair and percutaneous CT-guided drainage.3) However, percutaneous CT-guided drainage has some limitations: it is only available for abscesses located where the percutaneous puncture can be safely performed; and the size of a drainage catheter may be insufficient to excrete the viscous discharge. By contrast, VATD allows for more extensive debridement and placement of various sizes of drainage catheter, which can be used for continuous drainage thereafter. In addition, VATD was reported to achieve comparable or even better outcome than open thoracic drainage in cases of empyema or mediastinitis in terms of operative time, postoperative hospital stay, relapse rate, morbidity, and mortality.4,5) In the present case, the location of the abscess was difficult for CT-guided percutaneous drainage. In addition, the patient’s respiratory function was impaired because of the previous lung cancer, which was motivation for us to perform VATD. Previously, Yoneyama et al. in their study reported an experience of thoracoscopic drainage that was performed in an endograft infection after TEVAR and was successful in controlling the infection by thoracoscopic drainage following continuous irrigation.6) The difference between their case and ours is over whether irrigation was used following the debridement. Irrigation may be more effective to attenuate the infection, while it requires multiple catheters both for irrigation and drainage, which may inhibit the patient’s activity. We think that the infection cavity is the determinant of whether irrigation should be included or not. In our case, the abscess mostly consisted of necrotic tissue without the pus seen in the study of Yoneyama et al., and therefore it did not require irrigation to heal.
When performing VATD, the most important consideration is avoidance of blood leakage from the interstice between the aortic wall and the stent-graft during debridement, which may directly cause massive bleeding and a critical hemodynamic state. We carefully evaluated presence of endoleak with preoperative CT and confirmed that there was no endoleak and there was sufficient distance of the landing zone both proximally and distally. With VATD, the debridement was carefully advanced and limited within the aneurysm without manipulating the sealing zones so as not to develop endoleak. In addition, the patient was placed in an upper body right lateral and a lower body 45 degree semi-lateral position during VATD, which would have allowed us to establish a cardiopulmonary bypass with inguinal canulation in event of accidental bleeding.
Appropriate antibiotic therapy is also crucial in obtaining a better outcome of infective aortic disease. Our strategy of antibiotic therapy was basically in agreement with the treatment of infective endocarditis. The patient received intravenous antibiotic treatment with ceftriaxone for a total of 8 weeks in accordance with antibiotic susceptibility and published guidelines.7) Whether to continue oral antibiotics after completion of intravenous administration and its length is still controversial and varies according to published literature.8) We continued oral antibiotics until the drainage catheter was removed and inflammatory response in laboratory testing was completely abolished. The timing of removal of the drainage catheter is another concern. In the present case, the drainage catheter was removed after discontinuation of discharge, which suggests that the abscess cavity was completely closed.
The FET technique, which is usually combined with aortic arch repair, can be used to treat thoracic aortic disease that is unsuitable for TEVAR treatment because of a short proximal landing zone, as well as being used for the treatment of extensive thoracic aneurysms as a single stage operation. The FET technique is also useful for failed cases after TEVAR, such as retrograde aortic dissection,9) or persistent type 1 endoleak.10) In the present case, the etiology of the pseudoaneurysm that developed at the proximal edge of the stent-graft was erosion of the stent-graft because there was no sign of reactivation of infection, i.e., repeated culture tests of both blood samples and the discharge from the drainage catheter were all negative during the previous 2 weeks. Therefore, we considered that additional TEVAR would be a feasible treatment for the pseudoaneurysm. However, it was located close to the origin of the left subclavian artery, indicating insufficient sealing distance for additional TEVAR. The combination of debranching to the supra-arch vessels and zone 0 TEVAR might be another treatment option. However, there was severe calcification in the ascending aorta, which was not thought to be optimal for the debranching. Taking all these factors into account, we employed the FET technique.
Conclusion
In this research study, we successfully treated a ruptured mycotic thoracic aortic aneurysm with a hybrid therapy including stent-grafts implantation and VATD. This strategy can be an effective alternative to conventional surgical treatment in selected patients.
Disclosure Statement
All authors have no conflict of interest.
Author Contributions
Study conception: KH
Patient treatment: all authors
Data collection: KH
Analysis: KH
Writing: KH
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).Razavi MK, Razavi MD. Stent-graft treatment of mycotic aneurysms: a review of the current literature. J Vasc Interv Radiol 2008; 19 Suppl: S51-6. [DOI] [PubMed] [Google Scholar]
- 2).Stellmes A, Von Allmen R, Derungs U, et al. Thoracic endovascular aortic repair as emergency therapy despite suspected aortic infection. Interact Cardiovasc Thorac Surg 2013; 16: 459-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Chino S, Kato N, Noda Y, et al. Treatment of infected aneurysms of the abdominal aorta and iliac artery with endovascular aneurysm repair and percutaneous drainage. Ann Vasc Surg 2016; 36: 289.e11-5. [DOI] [PubMed] [Google Scholar]
- 4).Pan H, He J, Shen J, et al. A meta-analysis of video-assisted thoracoscopic decortication versus open thoracotomy decortication for patients with empyema. J Thorac Dis 2017; 9: 2006-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Cho JS, Kim YD, I H, et al. Treatment of mediastinitis using video-assisted thoracoscopic surgery. Eur J Cardiothorac Surg 2008; 34: 520-4. [DOI] [PubMed] [Google Scholar]
- 6).Yoneyama F, Sato F, Sakamoto H, et al. Preservation of the infected thoracic aortic endograft with thoracoscopic drainage and continuous irrigation. Gen Thorac Cardiovasc Surg 2018; Jan 30. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Miyatake K, Akaishi M, Ishizuka N, et al. Guidelines for the prevention and treatment of infective endocarditis (JCS 2008). http://www.j-circ.or.jp/guideline/pdf/JCS2008_miyatake_h.pdf. (in Japanese)
- 8).Kan CD, Lee HL, Yang YJ. Outcome after endovascular stent graft treatment for mycotic aortic aneurysm: a systematic review. J Vasc Surg 2007; 46: 906-12. [DOI] [PubMed] [Google Scholar]
- 9).Hirano K, Tokui T, Nakamura B, et al. Retrograde ascending dissection after thoracic endovascular aortic repair combined with the chimney technique and successful open repair using the frozen elephant trunk technique. Vasc Endovascular Surg 2018; 52: 80-5. [DOI] [PubMed] [Google Scholar]
- 10).Landau JH, Dubois LA, Chu MWA. Hybrid arch frozen elephant trunk for persistent endoleak after thoracic endovascular aortic repair. Ann Thorac Surg 2017; 104: e227-9. [DOI] [PubMed] [Google Scholar]