Abstract
The purpose of this study was to investigate the clinical and radiological features of osteoporotic burst fractures affecting levels below the second lumbar (middle-low lumbar) vertebrae, and to clarify the appropriate surgical procedure to avoid postoperative complications. Thirty-eight consecutive patients (nine male, 29 female; mean age: 74.8 years; range: 60–86 years) with burst fractures affecting the middle-low lumbar vertebrae who underwent posterior-instrumented fusion were included. Using the Magerl classification system, these fractures were classified into three types: 16 patients with superior incomplete burst fracture (superior-type), 11 patients with inferior incomplete burst fracture (inferior-type) and 11 patients with complete burst fracture (complete-type). The clinical features were investigated for each type, and postoperative complications such as postoperative vertebral collapse (PVC) and instrumentation failure were assessed after a mean follow-up period of 3.1 years (range: 1–8.1 years). All patients suffered from severe leg pain by radiculopathy, except one with superior-type fracture who exhibited cauda equina syndrome. Nineteen of 27 patients with superior- or inferior-type fracture were found to have spondylolisthesis due to segmental instability. Although postoperative neurological status improved significantly, lumbar lordosis and segmental lordosis at the fused level deteriorated from the postoperative period to the final follow-up due to postoperative complications caused mainly by PVC (29%) and instrument failure (37%). Posterior-instrumented fusion led to a good clinical outcome; however, a higher incidence of postoperative complications due to bone fragility was inevitable. Therefore, short-segment instrument and fusion with some augumentation techniqus, together with strong osteoporotic medications may be required to avoid such complications.
Keywords: posterior decompression and fusion, osteoporotic vertebral burst fracture, middle-low lumbar spine
Introduction
Although osteoporotic vertebral fractures usually develop in the thoracolumbar transitional zone, fractures affecting levels below the second lumbar (middle-low lumbar) vertebra have often been encountered in recent years among elderly people with active lifestyles. Indications for surgical treatment for middle-low lumbar burst fractures have become more frequent as well because of the severe radiculopathy symptoms caused by foraminal stenosis, with or without central stenosis. However, few studies have focused on the clinical features of burst fractures with neurological deficit, and the appropriate surgical procedure remains controversial.1–3) The purpose of this study was to clarify the clinical and radiological features of patients with middle-low lumbar osteoporotic burst fractures, and to provide appropriate surgical procedure by analyzing the postoperative complications affecting surgical outcomes.
Materials and Methods
Thirty-eight consecutive patients who underwent surgical treatment for middle-low lumbar burst fractures at our institution between 2006 and 2017 were included in this retrospective study. There were nine males and 29 females, with a mean age of 74.8 years (range: 60–86 years), and the mean follow-up period was 3.1 years (range: 1–8.1 years). The affected vertebral levels were L3 in 14 patients, L4 in 17, and L5 in 7, and all patients obtained neither relief from severe radicular pain nor solid bony fusion despite initial conservative treatment such as bed rest and thoracolumbar orthosis. Using the Magerl classification system,4) the burst fractures were classified into three types: superior incomplete burst fracture (superior-type), inferior incomplete burst fracture (inferior-type) and complete burst fracture (complete-type) (Fig. 1). There were 16 superior-type, 11 inferior-type and 11 complete-type patients. All patients underwent decompression at the stenotic levels and were instrumented by in situ fusion with postural reduction. Transpedicular screws were inserted into the affected vertebrae as far as the fracture pattern allowed. Of the 38 patients, 34 underwent posterior lumbar interbody fusion (PLIF) combined with posterolateral fusion (PLF), while two superior-type patients underwent PLF alone, and two complete-type patients demonstrating intravertebral vacuum cleft formation on plain radiographs underwent vertebroplasty using hydroxyapatite blocks and/or calcium phosphate cement combined with PLIF or PLF. Ultrahigh molecular weight polyethylene (UHMWPE) sublaminar cables (NESPLON Cable System; Alfresa Pharma Corporation, Osaka, Japan) were bilaterally tightened to the rod system to prevent screw loosening and back-out. Clinical outcomes were assessed by using the Japanese Orthopaedic Association (JOA) scoring system, and the recovery rate was calculated using the following formula: (postoperative score − preoperative score)/(29 − preoperative score) × 100%. Radiologically, whole lumbar lordosis (LL) and segmental lordosis (SL) at the fused level were evaluated preoperatively, postoperatively and at final follow-up on lateral radiographs in standing neutral, flexion and extension positions. Segmental instabilities associated with lumbar spondylolisthesis were defined radiologically as excessive segmental motion of more than 3 mm of vertebral slippage.5,6) Successful fusion was defined as a loss of mobility in the fused segment on flexion-extension lateral radiographs. Using previously-reported criteria, interbody fusion status was graded as either union in situ (solid fusion without loss of graft height), collapsed union (solid fusion with graft bone collapse or cage subsidence into the adjacent vertebral body), or nonunion.7) Postoperative complications such as vertebral collapse and instrument failure were analyzed.
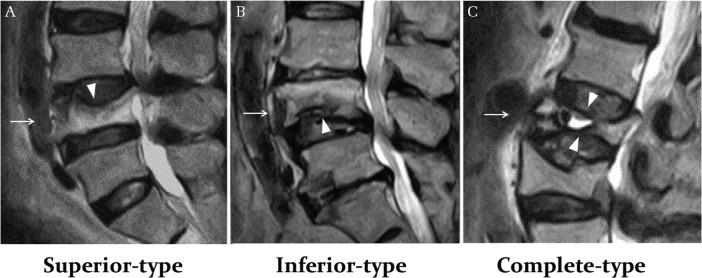
Fig. 1.
Preoperative MRI images showing the three types of burst fracture according to the Magerl classification system. (A) Superior-type patient with superior incomplete burst fracture (arrow). (B) Inferior-type patient with inferior incomplete burst fracture (arrow). (C) Complete-type patient with complete burst fracture (arrow). Arrowheads indicate regions of collapse. MRI: magnetic resonance imaging.
Statistical analysis between groups was performed by the way of a Mann–Whitney U test, a Wilcoxon signed-rank test, or one-way analysis of variance for continuous variables, and Fisher’s exact test for categorical variables. A P-value of less than 0.05 was considered to be statistically significant. All statistical analysis was performed using EZR Software (Saitama Medical Center, Jichi Medical University, Saitama, Japan).
Results
All patents suffered from sciatic nerve pain in the leg, except one superior-type patient who exhibited cauda equina syndrome. Overall, the mean JOA score improved significantly from 8.8 points (range: 2–19 points) preoperatively to 22.8 points (range: 13–29 points, P < 0.001) at the final follow-up, and the mean recovery rate was 70% (range: 7.1–100%). Although the mean preoperative JOA score in complete-type patients tended to be lower than that in the other types, this difference did not reach statistical significance (10.4 vs. 8.8 vs. 6.5 for superior-, inferior- and complete-type, respectively; P = 0.08). The neurological recovery rate was similar in all the three types (superior-: 71%, inferior-: 69% and complete-type: 70%, P = 0.98) (Table 1).
Table 1.
Comparison of surgical results between the three fracture types
| Superior-type (n = 16) | Inferior-type (n = 11) | Complete-type (n = 11) | P-value | ||
|---|---|---|---|---|---|
| JOA score (points) | Pre-op | 10.4 ± 5.1 | 8.8 ± 3.9 | 6.5 ± 3.6 | 0.08 |
| Follow-up | 23.5 ± 3.8 | 22.4 ± 5.8 | 22.2 ± 5.6 | 0.75 | |
| RR (%) | 70.6 ± 21.3 | 68.6 ± 25.2 | 70.1 ± 21.9 | 0.98 |
Values are expressed as mean ± SD. RR: recovery rate at follow-up.
Table 2 shows the comparison of radiological data and postoperative complications between the three fracture types. Twenty-two patients (58%) demonstrated spondylolisthesis in the damaged motion segments, which was due to a higher rate of superior- or inferior-type (19/27; 70%) burst fractures localized in the upper or lower half of the vertebra than in the complete-type (3/11; 27%, P = 0.028). Significantly higher rates of canal stenosis and foraminal stenosis were observed in patients with respectively superior- (15/16; 94%; P = 0.045) and inferior-type (8/11; 73%; P = 0.016) fractures.
Table 2.
Comparison of the radiological data and postoperative complications between the three fracture types
| Superior-type (n = 16) | Inferior-type (n = 11) | Complete-type (n = 11) | P-value | ||
|---|---|---|---|---|---|
| Segmental instability | 12 | 7 | 3 | ||
| Stenosis types | CS | 13 | 3 | 8 | |
| FS | 1 | 5 | 2 | ||
| CS + FS | 2 | 3 | 1 | ||
| VCFs | Fresh | 2 | 1 | 5 | 0.11 |
| Old | 3 | 4 | 2 | 0.62 | |
| LL (°) | Pre-op | 26.7 ± 14.7 | 28.0 ± 9.8 | 16.4 ± 16.9 | 0.12 |
| Post-op | 35.9 ± 9.7 | 35.6 ± 10.1 | 25.0 ± 14.3 | 0.04 | |
| Follow-up | 31.0 ± 11.2 | 30.2 ± 13.0 | 16.1 ± 18.5 | 0.02 | |
| Loss of correction | 4.9 ± 7.4 | 5.4 ± 11.7 | 9.0 ± 13.8 | 0.61 | |
| SL (°) | Pre-op | 7.3 ± 13.2 | 4.8 ± 9.3 | 6.2 ± 15.2 | 0.89 |
| Post-op | 15.8 ± 9.3 | 13.8 ± 6.6 | 15.9 ± 13.5 | 0.85 | |
| Follow-up | 12.5 ± 11.3 | 12.0 ± 8.9 | 8.4 ± 17.1 | 0.68 | |
| Loss of correction | 3.2 ± 4.6 | 1.7 ± 4.6 | 7.5 ± 7.2 | 0.045 | |
| Fusion status | Union in situ | 14 | 8 | 5 | |
| Collapsed union | 2 | 2 | 6 | 0.058 | |
| Nonunion | 0 | 1 | 0 | ||
| Complications | PVC | 6 | 3 | 2 | 0.66 |
| PS loosening | 5 | 1 | 8 | 0.009 | |
| PS back-out | 0 | 1 | 3 | 0.06 | |
Values are expressed as mean ± SD. CS: canal stenosis, FS: foraminal stenosis, LL: lumbar lordosis, PS: pedicle screw, PVC: postoperative vertebral collapse, SL: segmental lordosis at the fused level, VCF: vertebral compression fracture.
Vertebral compression fractures (VCFs) in the thoracolumbar spine accompanied by these burst fractures were found in 17 patients (45%); fresh VCF confirmed by preoperative magnetic resonance (MR) images was observed in eight patients.
Postoperatively, the mean LL and SL angles had improved significantly (24.1 ± 14.7° to 32.7 ± 12.0° and 6.3 ± 12.5° to 15.2 ± 9.9°, respectively; both P < 0.001); however, the correction angle had decreased significantly at the final follow-up (26.4 ± 15.3° and 11.2 ± 12.5°, respectively; both P < 0.001). The mean preoperative, postoperative and follow-up LL angles in complete-type patients tended to be smaller than in the other types (P = 0.12, 0.04 and 0.02, respectively). The mean loss of correction angle, 7.5 ± 7.2°, was significantly greater in complete-type patients than in the other types (P = 0.045). Moreover, a higher rate of collapsed union was observed in patients with complete-type (6/11; 55%) than the other types (P = 0.058). Solid bony fusion as a result of PLIF and PLF procedures was obtained in all patients, except one inferior-type patient who exhibited nonunion and severe kyphotic deformity due to postoperative vertebral collapse (PVC) in the affected vertebra.
Postoperative vertebral collapse was observed in 16 vertebrae of 11 patients (29%). One inferior-type patient required revision surgery. The upper-instrumented vertebra (UIV) was affected in most of the patients suffering from PVC in the early postoperative period. Pedicle screw loosening was observed in 14 patients (37%). A significantly higher rate of screw loosening was observed in patients with complete-type fracture (P = 0.009). All of the screw loosening was observed in the UIV. Alignment with loss of lumbar lordosis or severe local kyphosis was observed in one patient of each of the three types due to multiple PVCs, either in the supra-adjacent vertebra or in the UIV following back-out of the pedicle screws. Only four of 20 patients without sublaminar cables suffered complete screw back-out. Additionally, the rate of screw loosening was also found to be higher in patients without sublaminar cables than in those with cables although the difference was not statistically significant (9/20; 45% vs. 5/18; 28%; P = 0.33).
Discussion
This study investigated not only the clinical and radiological features, but also the surgical outcomes of patients with middle-low lumbar osteoporotic burst fractures who underwent posterior-instrumented fusion and decompression. Each type of burst fracture exhibited substantial differences in radiological features; segmental instability with lumbar spondylolisthesis was evident mainly in superior- and inferior-type patients, while a higher rate of canal stenosis and foraminal stenosis was observed in respectively superior- and inferior-type patients. Deterioration of lumbar lordosis due to VCFs accompanied by these burst fractures was most often seen on radiographs in complete-type patients. Furthermore, high rates of postoperative complications, such as vertebral collapse and instrument failure, were noted in this series; also, all cases of pedicle screw loosening found in the UIV and with PVC were observed in the UIV in the early postoperative period.
Etiologies of these fractures
Failure of motion segments with lumbar spondylolisthesis due to accelerated progression of disc degeneration after single end-plate fracture was the main etiology observed in superior- and inferior-type patients. In contrast, disruption of spinal components such as the vertebral body or the ligaments holding the spine together could give rise to a highly unstable lumbar spine in complete-type patients who were noted to have higher rates of screw loosening.
Severe foraminal stenosis was most often observed in inferior-type patients due to descent of the pedicle and lower vertebral body collapse and either damaged end-plates or posterior-wall bone fragments pressing directly onto the intervertebral foramen, while canal stenosis was most often seen in superior-type patients due to a higher incidence of segmental instability; various types of stenosis were seen in complete-type patients due to retropulsion of bony fragments into the spinal canal. Almost all the patients in this study exhibited symptoms of radiculopathy, such as severe lower-back and leg pain due to multiple etiologies, as a result of which they needed to undergo further surgical treatment.
Recommendation for surgical procedures
For inferior-type patients, single-level instrumented PLIF can lead to complete circumferential decompression including the foraminal zone and stability in the intervertebral discs with damaged end-plates, thus providing a method of treating the morbidity. However, surgical intervention to obtain adequate solid bony fusion and maintain correct alignment are unsolved problems because of the severe kyphosis due to the vertebral collapse following screw loosening that was observed in one inferior-type patient. Pedicle screw fixation of the affected vertebrae is recommended as far as the fracture pattern allows because the loading force on each screw can be lowered.8,9) However, for both superior- and complete-type patients, accurate pedicle screw insertion into the affected vertebrae is often difficult due to pedicle fractures; therefore, two-level instrumented PLIF is highly recommended as a means of insuring spinal stability (Fig. 2). Interbody fusion procedures are required to fill the damaged segments with a sufficient volume of block and chipped bone, especially in complete-type patients in order to avoid progressive and severe subsidence graft. Vertebroplasty combined with PLF should be limited to properly selected complete-type patients exhibiting intravertebral vacuum cleft formation in the affected vertebrae without segmental instability on radiographs. PLF alone is recommended for superior-type patients with neither lumbar kyphosis nor segmental instability because the load impact on the affected vertebrae may increase, resulting in gradual collapse (Fig. 3). Although it may be reasonable to choose decompression alone when a superior-type patients primary symptom is neurogenic claudication due to spinal canal stenosis without segmental instability on radiographs, bed rest and then external immobilization with a hard corset may be essential for effective management with careful attention to progressive vertebral collapse. Although no patients in this study exhibited severe kyphosis as well as osteoporosis preoperatively, for these patients, corrective osteotomy and posterior long instrumentation fusion may be required to achieve optimal sagittal alignment in order to get relief from pain and prevent postoperative complications. However, these interventions can lead to serious complications in older patients because of the high risk of blood loss and longer operative times and should be selected only for appropriate patients.10,11)
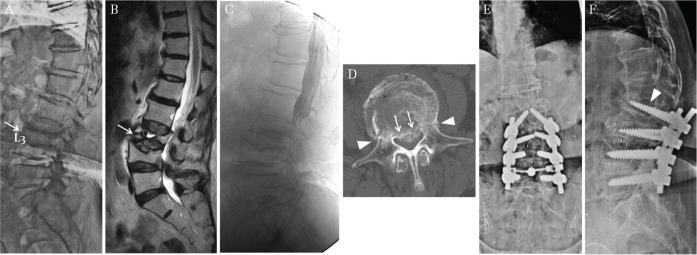
Fig. 2.
Case of an 85-year-old woman with L3 complete burst fracture (complete-type) and old compression fractures at L4 with degenerative spondylolisthesis, who was presented with severe low back pain and bilateral radicular thigh pain. (A) Preoperative lateral plain radiograph, showing L3 vertebral collapse with spondylolisthesis at L4–5. (B) Preoperative sagittal T2-weighted MR image showing multiple canal stenosis at L2–3, L3–4 and L4–5 levels with vertebral cleft sign (arrows) at L3. (C) Preoperative myelogram showing L3 collapse and complete block at L2–3. (D) Preoperative axial CT scan showing L3 collapse with bilateral pedicle fracture (arrowhead) and canal stenosis due to bony fragments (arrows). (E and F) Coronal (E) and sagittal (F) radiographs at final follow-up, showing successful fusion after PLIF at L2–3, L3–4 and L4–5 levels despite pedicle screw loosening with a change of placement status (arrowhead). PLIF: posterior lumbar interbody fusion.
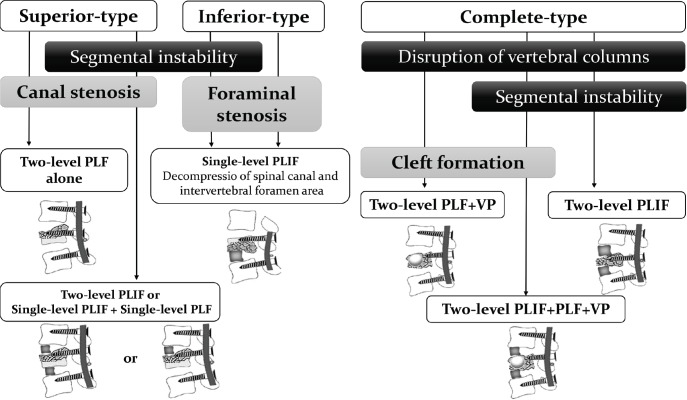
Fig. 3.
Surgical intervention algorithm for osteoporotic vertebral burst fractures in middle-low lumbar spine. PLF: posterolateral fusion, PLIF, posterior lumbar interbody fusion; VP: vertebroplasty.
Effect of augmentation techniques
Upper-instrumented vertebra collapse after screw loosening in the early postoperative period was observed in a relatively large number of patients; therefore, it may be that excess loading in the fused segments following spinal instrumentation increases stress and motion in the vertebrae.12–15) Although screw loosening alone often presents with no noticeable symptoms and has little adverse impact on clinical outcomes,15,16) vertebral collapse following screw back-out, which can lead to a marked decrease in lumbar lordosis as well as residual lumbar pain, should be avoided as much as possible. Common clinical methods to improve the fixation of pedicle screws in the osteoporotic spine include the addition of laminar hooks or sublaminar cables to the fixation construct, or the supplementation of the pedicle channel with polymethyl methacrylate (PMMA) or calcium phosphate cement (CPC). Several previous studies have shown the highly beneficial effects of an instrumented construct with sublaminar cables using UHMWPE in preventing screw loosening in the treatment of thoracolumbar collapse.17,18) The material of the cable system a softer and more flexible with a flat cross-sectional configuration that has the advantage of being able to be easily placed at the same level of lamina as the UIV, avoiding neural damage and reducing focal distribution of the fragile bone. A biomechanical study of the thoracic spine reported that the lamina hook claw system dislocated with significantly less force than other spinal implants: sublaminar wires, pedicle screws and pedicle screws with wire.19) Several studies have reported that fenestrated screws with PMMA augmentation offer the possibility of treating patients with reduced bone quality due to severe osteoporosis.20,21) Also, CPC augmentation enabled an average 77% increase in maximum pull-out strength compared to a pedicle screw-only group.22) Although the disadvantages of PMMA included body toxicity, circulation response by the cement monomer, and lack of bone compatibility, CPC was easily infused into the vertebral bone trabeculae and had the advantage of superior osteoconductivity with the peripheral bones, biocompatibility and bone repair. Thus, using pedicle screws with CPC augumentation may provide clinical benefits, especially for complete-type patients with substantial screw loosening.
Medications for osteoporosis
Moreover, there remain the problems of poor bone fragility caused by aging and various comorbidities that make it difficult for the instrumentation to maintain the alignment of the fixed spine.2,14,17) Therefore, osteoporotic medications are considered essential to stop further bone loss, to stimulate bone formation and to prevent further fractures. Among these, teriparatide has been administered initially to recent cases for the purpose of accelerating early bone union after lumbar arthrodesis and reducing pedicle screw loosening.16,23,24)
Consequently, for adequate stability of the short-segment instrumentation and fusion, augmented by way of sublaminar cables and pedicle channel with CPC, especially in the UIV, currently-available strong osteoporotic medications such as teriparatide may be administered to avoid complications.
Study limitations
Several limitations of this study should be acknowledged. First, this study is based on a small number of patients who underwent surgical treatment alone and is a retrospective case series. Second, because either diverse osteoporosis treatments were administered or intervention with augmentation such as sublaminar cables was performed as appropriate, the present study may not provide an accurate evaluation of postoperative complications. However, as few previously-reported studies have examined patients with osteoporotic burst fractures affecting the middle-low lumbar vertebrae, the present study of augmented fusion surgery with UHMWPE cables provides important information regarding surgical strategies and suggests a benefit in preventing screw back-out for increased mobility of patients with burst fractures in the middle-lower lumbar spine. Further study with a larger patient population should elucidate the optimal treatment modality.
Conclusion
The results of this study suggest that each type of osteoporotic burst fracture in the middle-low lumbar spine has different clinical features according to the type of lumbar stenosis, with or without segmental instability, and that posterior decompression and fusion with instrumentation may provide better surgical outcomes. However, deterioration of lumbar lordosis due to postoperative complications such as instrument failure or vertebral collapse were observed with a high incidence among the patients in this study. Therefore, surgical strategy, careful postoperative management and strong osteoporotic medications may be essential for these patients.
Footnotes
Conflicts of Interest Disclosure
All authors have no conflict of interest.
References
- 1).Sasaki M, Aoki M, Nishioka K, Yoshimine T: Radiculopathy caused by osteoporotic vertebral fractures in the lumbar spine. Neurol Med Chir (Tokyo) 51: 484–489, 2011 [DOI] [PubMed] [Google Scholar]
- 2).Nakajima H, Uchida K, Honjoh K, Sakamoto T, Kitade M, Baba H: Surgical treatment of low lumbar osteoporotic vertebral collapse: a single-institution experience. J Neurosurg Spine 24: 39–47, 2016 [DOI] [PubMed] [Google Scholar]
- 3).Yamashita, Sakaura H, Miwa T, Ohwada T: Modified posterior lumbar interbody fusion for radiculopathy following healed vertebral collapse of the middle-lower lumbar spine. Global Spine J 4: 255–262, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S: A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3: 184–201, 1994 [DOI] [PubMed] [Google Scholar]
- 5).Iguchi T, Ozaki T, Chin T, et al. : Intimate relationship between instability and degenerative signs at L4/5 segment examined by flexion-extension radiography. Eur Spine J 20: 1349–1354, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Kanemura A, Doita M, Kasahara K, Sumi M, Kurosaka M, Iguchi T: The influence of sagittal instability factors on clinical lumbar spinal symptoms. J Spinal Disord Tech 22: 479–485, 2009 [DOI] [PubMed] [Google Scholar]
- 7).Yamamoto T, Ohkohchi T, Ohwada T, Kotoku H, Harada N: Clinical and radiological results of PLIF for degenerative spondylolisthesis. J Musculoskelet Res 2: 181–195, 1998 [Google Scholar]
- 8).Gelb D, Ludwig S, Karp JE, et al. : Successful treatment of thoracolumbar fractures with short segment pedicle instrumentation. J Spinal Disord Tech 23: 293–301, 2010 [DOI] [PubMed] [Google Scholar]
- 9).Guven O, Kocaoglu B, Bezer M, Aydin N, Nalbantoglu U: The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech 22: 417–421, 2009 [DOI] [PubMed] [Google Scholar]
- 10).Lau D, Osorio JA, Deviren V, Ames CP: The relationship of older age and perioperative outcomes following thoracolumbar three-column osteotomy for adult spinal deformity: an analysis of 300 consecutive cases. J Neurosurg Spine 28: 593–606, 2018 [DOI] [PubMed] [Google Scholar]
- 11).Hassanzadeh H, Jain A, El Dafrawy MH, et al. : Three-column osteotomies in the treatment of spinal deformity in adult patients 60 years old and older: outcome and complications. Spine (Phila Pa 1976) 38: 726–731, 2013 [DOI] [PubMed] [Google Scholar]
- 12).Lewis SJ, Abbas H, Chua S, et al. : Upper instrumented vertebral fractures in long lumbar fusions: what are the associated risk factors? Spine 37: 1407–1414, 2012 [DOI] [PubMed] [Google Scholar]
- 13).Toyone T, Ozawa T, Kamikawa K, et al. : Subsequent vertebral fractures following spinal fusion surgery for degenerative lumbar disease: a mean ten-year follow-up. Spine 35: 1915–1918, 2010 [DOI] [PubMed] [Google Scholar]
- 14).Watanabe K, Lenke LG, Bridwell KH, Kim YJ, Koester L, Hensley M: Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine 35: 138–145, 2010 [DOI] [PubMed] [Google Scholar]
- 15).Wu JC, Huang WC, Tsai HW, et al. : Pedicle screw loosening in dynamic stabilization: incidence, risk, and outcome in 126 patients. Neurosurg Focus 31: E9, 2011 [DOI] [PubMed] [Google Scholar]
- 16).Ohtori S, Inoue G, Orita S, et al. : Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine 38: E487–E492, 2013 [DOI] [PubMed] [Google Scholar]
- 17).Sudo H, Ito M, Abumi K, et al. : One-stage posterior instrumentation surgery for the treatment of osteoporotic vertebral collapse with neurological deficits. Eur Spine J 19: 907–915, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Hamasaki T, Tanaka N, Kim J, Okada M, Ochi M, Hutton WC: Pedicle screw augmentation with polyethylene tape: a biomechanical study in the osteoporotic thoracolumbar spine. J Spinal Disord Tech 23: 127–132, 2010 [DOI] [PubMed] [Google Scholar]
- 19).Paxinos O, Tsitsopoulos PP, Zindrick MR, et al. : Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J Neurosurg Spine 13: 469–476, 2010 [DOI] [PubMed] [Google Scholar]
- 20).Amendola L, Gasbarrini A, Fosco M, et al. : Fenestrated pedicle screws for cement-augmented purchase in patients with bone softening: a review of 21 cases. J Orthop Traumatol 12: 193–199, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Girardo M, Cinnella P, Gargiulo G, Viglierchio P, Rava A, Aleotti S: Surgical treatment of osteoporotic thoraco-lumbar compressive fractures: the use of pedicle screw with augmentation PMMA. Eur Spine J 26: 546–551, 2017 [DOI] [PubMed] [Google Scholar]
- 22).Masaki T, Sasao Y, Miura T, et al. : An experimental study on initial fixation strength in transpedicular screwing augmented with calcium phosphate cement. Spine (Phila Pa 1976) 34: E724–E728, 2009 [DOI] [PubMed] [Google Scholar]
- 23).Ohtori S, Inoue G, Orita S, et al. : Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine 37: E1464–E1468, 2012 [DOI] [PubMed] [Google Scholar]
- 24).Cho PG, Ji GY, Shin DA, Ha Y, Yoon DH, Kim KN: An effect comparison of teriparatide and bisphosphonate on posterior lumbar interbody fusion in patients with osteoporosis: a prospective cohort study and preliminary data. Eur Spine J 26: 691–697, 2017 [DOI] [PubMed] [Google Scholar]