Abstract
Globally measles remains one of the leading causes of death among young children even though a safe and cost-effective vaccine is available. The World Health Organization (WHO) European Region has seen a decline in measles and rubella cases in recent years. The recent outbreaks have primarily affected adolescents and young adults with no vaccination or an incomplete vaccination history. Eliminating measles and rubella is one of the top immunization priorities of the European Region as outlined in the European Vaccine Action Plan 2015–2020. Following the 2010 decision by the Member States in the Region to initiate the process of verifying elimination, the European Regional Verification Commission for Measles and Rubella Elimination (RVC) was established in 2011. The RVC meets every year to evaluate the status of measles and rubella elimination in the Region based on documentation submitted by each country’s National Verification Committees. The verification process was however modified in late 2014 to assess the elimination status at the individual country level instead of at regional level. The WHO European Region has made substantial progress towards measles and rubella elimination over the past 5 years. The RVC’s conclusion in 2016 that 70% and 66% of the 53 Member States in the Region had interrupted the endemic transmission of measles and rubella, respectively, by 2015 is a testament to this progress. Nevertheless, where measles and rubella remain endemic, challenges in vaccination service delivery and disease surveillance will need to be addressed through focused technical assistance from WHO and development partners.
Keywords: Disease elimination, European Region, Measles, Progress, Rubella, Vaccination, Verification
Introduction
The widespread use of safe and cost-effective measles vaccines in national immunization programmes globally since 1974 has resulted in a marked decrease in measles cases and deaths. Nevertheless, measles remains one of the leading causes of death among children under 5 years of age globally. Measles-related deaths have declined globally from about 548 300 in 2000 [1] to an estimated 114 900 in 2014 [2]. The incidence of rubella has also substantially declined in many countries through the use of rubella-containing vaccines.
The Global Vaccine Action Plan endorsed by the World Health Assembly in 2012 and the Global Measles and Rubella Strategic Plan 2012–2020 both include elimination of measles, rubella and congenital rubella syndrome (CRS) as a main objective [3,4]. In line with these documents, all WHO regions have established goals to eliminate measles (and in some regions also rubella) by 2020 [2]. In September 2016, the International Expert Committee for Documenting and Verifying Measles, Rubella, and Congenital Rubella Syndrome Elimination in the Americas declared that the Region of the Americas had eliminated measles [5], making it the first region in the world to achieve this milestone. In April 2015, the independent Committee determined, based on the available epidemiological evidence, that the WHO Region of the Americas had also eliminated rubella and CRS [6].
Elimination of both measles and rubella is one of the top immunization priorities of the 53 Member States of the WHO Regional Office for Europe. This joint ambition is one of the six primary goals of the European Vaccine Action Plan 2015–2020 [7], which was endorsed by the WHO European Regional Committee in September 2014.
This report summarizes the progress made towards measles and rubella elimination in the WHO European Region and outlines the verification processes implemented in the Region since 2012.
Notifications of measles and rubella in the Region
Over 185 000 measles cases were reported in the WHO European Region in 1990 [8]. The annual vaccine-preventable disease reports received from the Member States indicate that the number of measles cases in the Region declined from 37 421 in 2012 to 24 957 in 2015 [8]. There has also been a substantial reduction in the number of reported rubella cases from 29 617 in 2012 to 2437 in 2015 [8]. However, fewer countries have reported rubella cases (including zero reporting) than measles cases, and this disparity continued in 2015 [8]. The failure of some national surveillance systems to investigate and report every suspected case of measles or rubella and to perform laboratory testing to confirm the diagnosis of the fever and rash cases remains a concern throughout the Region.
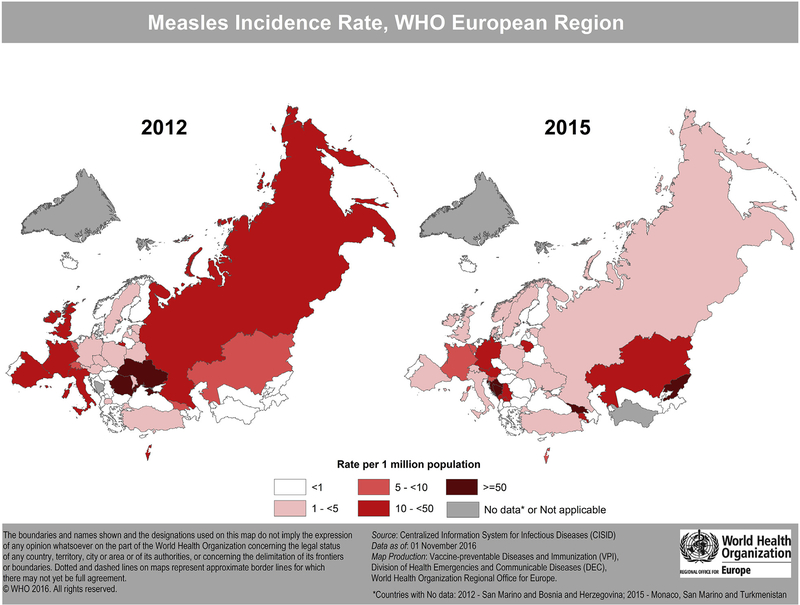
Fig. 1 compares measles incidence rates in 2012 and 2015 in the WHO European Region.
Fig. 1.
Map compares measles incidence rates in 2012 and 2015 in the WHO European Region.
Immunization activities in the Region
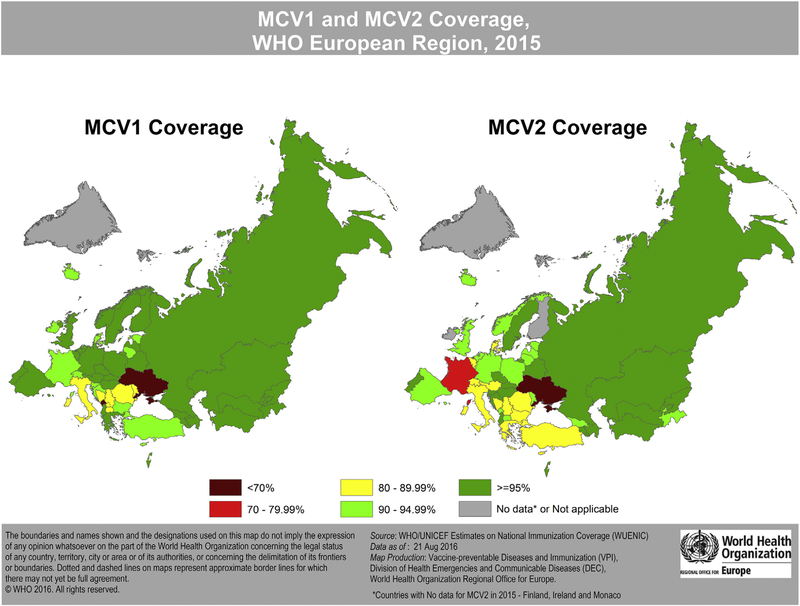
The reported routine vaccination coverage at the national level for 2015 showed that out of 51 countries in the Region (three countries did not report the coverage data). Twenty-five countries achieved the WHO-recommended coverage of >95% for the first dose of measles-containing vaccine (MCV1) and 15 countries achieved this target for the second dose of measles containing vaccine (MCV2) [9]. In 2015, five countries (Azerbaijan, Cyprus, Georgia, Kazakhstan, Kyrgyzstan) in the Region also conducted national supplementary immunization activities covering various age groups using measles or measles-rubella or measles-mumps-rubella vaccine. Barring Georgia and Kazakhstan, all other countries have attained coverage of >85% in these supplementary immunization activities. Kyrgyzstan reported >90% in both supplementary immunization activities conducted [9].
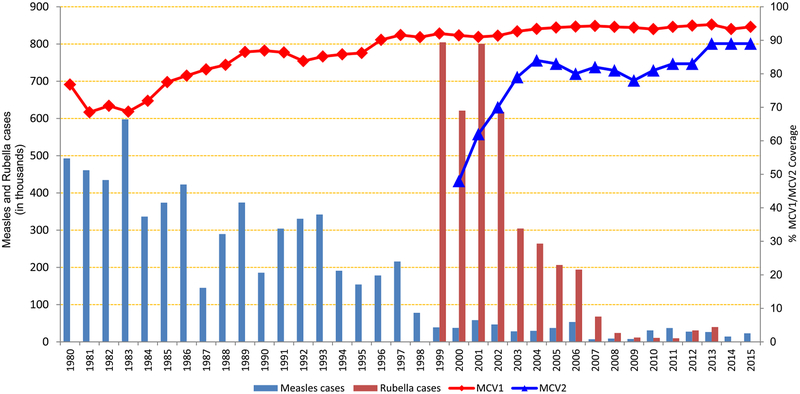
Fig. 2 shows measles and rubella cases, and MCV1 and MCV2 coverage by year (1980–2015) in the WHO European Region; Fig. 3 shows MCV1 and MCV2 coverage in 2015 in the WHO European Region.
Fig. 2.
Graph shows measles and rubella cases, and first and second doses of measles-containing vaccine (MCV1 and MCV2) coverage by year (1980–2015) in the WHO European Region. Data source: WHO/UNICEF Joint Reporting Form data; 1980–2015 (data as of 1 November 2016).
Fig. 3.
Map shows first and second doses of measles-containing vaccine (MCV1 and MCV2) coverage in 2015 in the WHO European Region.
Outbreaks in the Region and their characteristics
Sporadic cases of measles and rubella are reported by several countries in the WHO European Region each year; whereas large outbreaks tend to occur in just a few different countries each year. Large-scale measles outbreaks in 2015 were reported by Bosnia and Herzegovina, Germany, Kyrgyzstan and the Russian Federation [8]. The data indicate that confirmed measles cases in 2015 spanned several age groups. Only 15% of the cases have received two doses of measles vaccine whereas a large proportion (85%) of the cases were either unvaccinated or inadequately vaccinated; 29% were not immunized, 11% were incompletely immunized and 45% had an unknown immunization status. Rubella outbreaks in 2015 were reported by Georgia, Kyrgyzstan, Poland and Ukraine [8,10], with the majority of cases reported among children <15 years of age.
The immunization response activities following the outbreaks in 2015 varied considerably in the Region. The activities involved raising awareness of the health physicians and parents of unvaccinated children, post-exposure vaccination in outbreak-affected institutions and conducting catch-up vaccinations [10].
Vulnerable population groups identified in the recent measles outbreaks
The persistence of measles cases despite high reported national vaccination coverage indicates that there are pockets of suboptimal coverage throughout the region. Some outbreaks disproportionately affected ethnic, religious and/or philosophical minorities. Historically, poor vaccine uptake has been identified among the Anthroposophists in Germany, Netherlands and Switzerland, the Orthodox Protestant denominations in the Netherlands and the Roma communities in almost all European countries but especially in central and southeastern Europe who are either opposed to or had been critical towards vaccination [11]. The measles outbreaks in Poland and the Russian Federation in 2014 and in Croatia in 2015 affected mostly members of Roma families who have traditionally had lower vaccination coverage [10,12]. No additional information is available on ethnic characteristics of the outbreaks in Poland, the Russian Federation and Croatia.
Susceptible healthcare workers (HCWs) [10,12] played an important role in nosocomial infection in several measles outbreaks. Approximately 13 HCWs in Latvia and 30 in Spain were affected in 2014 and nine were affected in Croatia in 2015. Vaccination of HCWs not only protects them from occupational exposure but also prevents the spread of vaccine-preventable diseases to the susceptible patients. Most of the HCWs affected in Latvia, Spain and Croatia were either unvaccinated or their vaccination status was unknown [12]. Evaluation of the national policies for vaccination of HCWs in Europe indicates that only one country (Finland) has mandatory measles vaccination while, in 15 countries of the Region, it is neither recommended nor a mandatory requirement [13].
Surveillance activities in the Region
Measles surveillance in the WHO European Region includes case-based reporting with both clinical and laboratory case confirmation of the cases but the quality varies across the Region. The WHO Regional Office for Europe receives monthly reports of measles and rubella cases from Member States. Rubella and CRS surveillance remain a challenge with few countries having an established system for monitoring and reporting.
In 2015, all measles and rubella reference laboratories in the region were WHO accredited. Most countries submitted genomic sequence information on measles cases to the measles nucleotide surveillance database; however, only a few countries submitted genomic sequence information on rubella cases to the rubella nucleotide surveillance database [14]. The predominant measles genotypes identified in 2015 were D8, B3, H1 and D4 [15]. The major rubella genotypes identified in 2015 were 2B, 1E and 1a [16].
Prioritizing interventions in the countries where measles is endemic
In August 2016, with WHO, the United States Centers for Disease Control and Prevention and European Centre of Disease Prevention and Control conducted a joint technical consultation to review the situation of measles and rubella in the European Region and identify priority elimination activities. During the consultation, all the identified priority countries were assessed for the presence of the diseases, quality and performance of surveillance including laboratory activities, immunization coverage, population immunity and commitment to the elimination targets. A draft global measles-rubella categorization method [17] was used to identify specific determinants (immunization status and surveillance performance) in countries endemic for measles and rubella in the Region. This consultation resulted in developing country profiles outlining the challenges, interventions and priority activities to be carried out in 2017 to accelerate the elimination efforts in each of these endemic countries.
Measles and rubella elimination resolutions of the Region
In September 2005, the WHO Regional Committee for Europe, as part of a resolution on strengthening national immunization systems through measles and rubella elimination and prevention of congenital rubella infection, approved the plan and key strategies needed to attain the elimination objectives in the WHO European Region [18]. In September 2010, the WHO Regional Committee for Europe renewed its commitment to elimination of measles and rubella and prevention of CRS by 2015 and sustained support for polio-free status of the WHO European Region in a resolution that further requested the establishment of a regional measles and rubella elimination verification commission to review documentation and verify elimination of measles and rubella in the Region. The resolution also urged each Member State to establish a national measles and rubella elimination verification committee to document progress towards measles and rubella elimination [19].
Verification activities in the Region
The European Regional Verification Commission for Measles and Rubella Elimination (RVC) was established in 2011 (WHO internal communication) to evaluate the status of measles and rubella elimination in the Region. The Commission is an independent panel of experts that evaluates progress made by Member States through documentation submitted by national verification committees (NVCs). The verification process involves examining the evidence presented by the NVCs based on the WHO-recommended performance indicators for both surveillance and immunization coverage [20]. The Commission also provides guidance to Member States to support their efforts to achieve measles and rubella elimination. The vaccine-preventable diseases and immunization programme of the WHO Regional Office for Europe serves as the secretariat of the RVC.
To facilitate documentation of elimination at the national level, every country in the Region was requested to establish an NVC [19]. As of November 2016, 51 out of 53 Member States in the WHO European Region have functioning NVCs (unpublished report), including the Scandinavian Verification Committee established by Denmark, Norway and Sweden. The NVCs are responsible for reviewing and endorsing the information provided by the national immunization programme, including monitoring and advocating strengthening of the elimination activities in the countries.
The RVC holds annual meetings to review reports submitted by the NVCs and assess the status of measles and rubella elimination in the Region. The reports include information on measles and rubella epidemiology, molecular data, population immunity, surveillance and status of the immunization programme since the last report [21]. The RVC reviews these five lines of evidence and classifies the Member States according to WHO’s definition of elimination, i.e. the absence of endemic measles or rubella cases in a geographic area for a period of at least 12 months or more in the presence of a well-performing surveillance system [20]. Elimination can be verified once the country has sustained interruption of endemic transmission for 36 consecutive months. To facilitate assessment, the RVC approved a standard format for the Annual Status Update reports (ASU) submitted by the Member States. In 2014, the ASU template was revised to encourage countries to provide more information on the effective linkages between laboratory and epidemiological surveillance as well as documentation on chains of transmission [21]. Monaco and San Marino are the only two Member States that have not established NVCs. As they are small countries with limited human resources, the secretariat is exploring alternative mechanisms for them to report to the RVC without establishing NVCs.
The European RVC has met every year since 2012 to assess the elimination status of each Member State. In late 2014, the RVC modified the verification procedures to verify the measles and rubella elimination status at the national level as opposed to the regional level [21]. A total of 50 country reports were reviewed by the RVC during its fourth meeting, in 2015. After reviewing the individual country update reports for the period 2012–2014, the RVC concluded that as of the end of 2014, 32 Member States had interrupted the endemic transmission of measles and 32 Member States had interrupted endemic transmission of rubella [21]. Member States that demonstrate sustained interruption of endemic transmission for at least 36 consecutive months can be verified as having eliminated the disease. Twenty-one of the above countries were therefore verified as having eliminated measles and 20 were verified as having eliminated rubella. Following its review of the 2015 reports at its fifth annual meeting in October 2016, the RVC concluded that 24 Member States had eliminated measles and 13 additional Member States had interrupted endemic measles transmission; 24 had eliminated rubella and 11 additional Member States had interrupted endemic rubella transmission (unpublished report).
Discussion
The Member States of the WHO European Region have made tremendous progress towards eliminating measles and rubella. However, variable commitment to the elimination goal, competing health priorities, and the lack of capacity and resources in some countries jeopardize the ability of the Region as a whole to achieve measles and rubella elimination by 2020. To maintain momentum toward the goal, Member States, along with partners, need to explore opportunities to accelerate action and overcome the challenges.
Reflecting upon the changes in the verification mechanism
The RVC decision to shift the verification process from the regional level to the country level has provided an opportunity to recognize the achievements of individual Member States. The standardized approach to the verification process has helped to identify challenges and prioritize technical support for elimination activities. Shifting the verification process to the national level highlights the need to customize the approach depending on Member States size, health system structure or surveillance system. The WHO Secretariat is exploring other health initiatives in the Region, and best practices from other WHO Regions that can support the verification process in the countries.
Taking a closer look at surveillance
From discussions with national counterparts and surveillance reviews, there are challenges to fully implementing standardized case-based measles and rubella surveillance across the Region. While case-based measles surveillance is conducted in most of the countries in the Region, rubella is not a notifiable disease condition in Belgium, Denmark and France. As a result, no comprehensive rubella surveillance system exists in these countries [22]. But, in 2017, rubella is expected to become a notifiable condition in Denmark (WHO internal communication). A critical part of improving case-base surveillance is strengthening the link between epidemiology and laboratory data, including in-depth investigations and documentation of all outbreaks. As more Member States are verified as having eliminated measles and rubella, documenting every case and outbreak with supporting genetic data becomes more important, particularly to distinguish remaining endemic chains of transmission from importations. Characterizing the origin of individual cases and chains of transmission is critical information needed in the ASU to document measles and rubella elimination status. In recent years, measles surveillance and information sharing across the Region have improved; however, much more needs to be done, including expansion of rubella and CRS surveillance supported by genetic sequencing data.
Efforts to ensure equitable vaccination services
The verification framework for measles and rubella elimination in the WHO European Region recommends achieving and sustaining greater than 95% coverage for the first and second doses of measles- and rubella-containing vaccines at subnational administrative levels [23]. The European Vaccine Action Plan envisages a Region in which every person has equitable access to high-quality, safe and affordable vaccines and immunization services throughout the life-course [7]. This vision statement calls for improving coverage of all antigens offered in the national immunization schedules of all the countries in the Region. Also in view of the measles and rubella elimination goal, this includes attaining and sustaining high vaccination coverage with the first and second doses of measles- and rubella-containing vaccines.
The region-specific information provided by the Member States in the 2015 WHO/UNICEF Joint Reporting Form indicate that most of the countries in the region either do not require a proof or no information is available on mandatory check for vaccination at school entry. In line with the WHO position paper on measles, this could be considered as a lost opportunity to ensure completion of vaccination for those children who have otherwise missed their routine doses [24].
Officially reported national coverage with the first and second doses shows tremendous variation across the Region from 53% to 99% [9]. The subnational coverage data provided by Member States in their 2015 ASUs indicate equally wide variations at the subnational levels. Detailed subnational coverage data from all Member States will be critical for supporting the verification process and assessing risk.
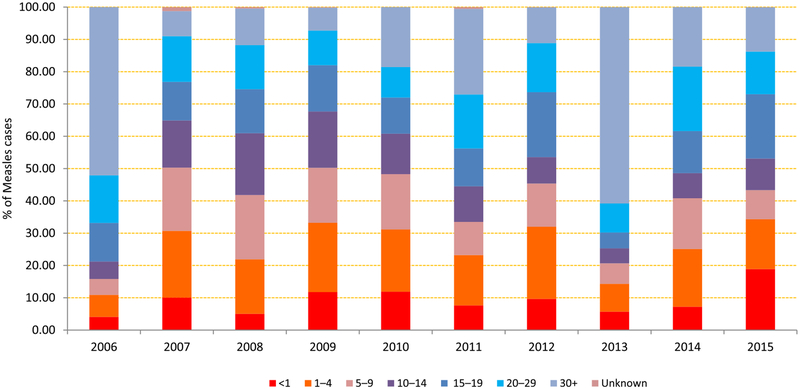
As 45% of the measles cases in the Region in 2015 were among adults aged ≥20 years, Member States need to explore innovative ways to effectively reach out to adults who are still susceptible to measles and rubella and close immunity gaps. Serosurveys can be useful in determining the population immunity for measles and rubella in adolescents and adults to determine the at-risk population in selected areas, especially, when substantive evidence is lacking or cannot be provided from other sources [25]. Opportunities were availed to assess the serological protection of measles and rubella during the nationwide poliovirus serosurvey conducted among 1- to 24-year-olds in Tajikistan in 2011. As part of the vaccine-preventable disease seroprevalence, a serological assessment for measles and rubella is planned in Ukraine in 2017. A multisectoral, comprehensive approach to identifying and addressing under- and unimmunized communities or subgroups throughout the Region is needed.
Fig. 4 shows the characteristics of age groups affected by measles by year (2006–2015) in the WHO European Region
Fig. 4.
Graph shows the characteristics of age groups affected by measles by year (2006–2015) in the WHO European Region. Data source: WHO/UNICEF Joint Reporting Form data; 2006–2015 (data as of 1 November 2016).
Conclusions
The WHO European Region has steadily progressed towards the elimination of measles and rubella since 2010. By the end of 2015, over half of Member States had interrupted endemic transmission of both diseases.
Despite this progress, however, the Region faces ongoing challenges in surveillance performance and vaccination service delivery. To achieve regional elimination, it will be crucial to close immunity gaps in specific populations and subgroups through routine immunization strengthening and supplementary immunization activities. Highly sensitive surveillance supported by an accredited laboratory network is critical to identifying cases, responding to outbreaks and verifying progress towards elimination. Improvements in measles surveillance in the Region should be capitalized upon to improve rubella surveillance, including reporting of genomic sequence data.
In its current iteration, the main role of the European RVC is to assess the measles and rubella elimination status of each of the 53 Member States of the WHO European Region. Member States’ elimination status provides a platform for defining priorities and focusing technical assistance from WHO and development partners. As more Member States move from endemic to interrupted and then eliminated status, the RVC will need to develop mechanisms to identify risk and monitor risk-mitigation activities, thereby ensuring that the verification process remains relevant and supports the regional and eventually global elimination goals.
Acknowledgements
The authors thank all the countries in the WHO European Region for providing the epidemiological and laboratory surveillance data on measles and rubella. Measles and rubella surveillance data for EU countries is sent through European Centre of Disease Prevention and Control (ECDC), Sweden. The authors also extend their gratitude to Catharina de Kat for her suggestions in the preparation of this article.
Footnotes
Transparency declaration
The authors declare no conflicts of interest and also that no external funding was received in preparation of this manuscript.
References
- [1].World Health Organization. Progress in global control and regional elimination of measles, 2000–2011. Wkly Epidemiol Rec 2013;88:29–36. Available at: http://www.who.int/wer/2013/wer8803.pdf. [PubMed] [Google Scholar]
- [2].World Health Organization Measles fact sheet, reviewed March 2016 Available at: http://www.who.int/mediacentre/factsheets/fs286/en/.
- [3].World Health Organization. Global vaccine action plan. Geneva, Switzerland: World Health Organization; 2012. Available at: http://apps.who.int/iris/bitstream/10665/78141/1/9789241504980_eng.pdf?ua=1. [Google Scholar]
- [4].World Health Organization. Global measles and rubella strategic plan: 2012–2020. Geneva, Switzerland: World Health Organization; 2012. Available at: http://apps.who.int/iris/bitstream/10665/44855/1/9789241503396_eng.pdf. [Google Scholar]
- [5].PAHO & WHO Americas, Region of Americas is declared free of measles. Available at: http://www.paho.org/hq/index.php?option=com_content&view=article&id=12528%3Aregion-americas-declared-free-measles&Itemid=1926&lang=en.
- [6].PAHO & WHO Fact sheet 2015, Elimination of rubella and congenital rubella syndrome in the Americas. Available at: http://www.paho.org/hq/index.php?Option=com_docman&task=doc_download&gid=29946&Itemid270&lang=en.
- [7].World Health Organization Regional Office for Europe. European Vaccine Action Plan 2015–2020. Copenhagen: World Health Organization; 2015. Available at: http://www.euro.who.int/__data/assets/pdf_file/0007/255679/WHO_EVAP_UK_v30_WEBx.pdf?ua=1. [Google Scholar]
- [8].World Health Organization [Internet site]. Disease incidence, WHO/UNICEF joint reporting process. Geneva: WHO; 2016. Available at: http://www.who.int/entity/immunization/monitoring_surveillance/data/incidence_series.xls?ua=1, accessed10 October 2016. [Google Scholar]
- [9].World Health Organization [Internet site]. Immunization coverage, WHO/UNICEF joint reporting process. Geneva: WHO; 2016. Available at: http://www.who.int/immunization/monitoring_surveillance/data/administrative_coverage.xls?ua=1, accessed on 10 October 2016. [Google Scholar]
- [10].World Health Organization Regional Office for Europe. WHO EpiBrief, 2016,1: 1–8. Available at: http://www.euro.who.int/__data/assets/pdf_file/0009/313020/EpiBrief_EpiData_1_2016-rev1.pdf?ua=1. [Google Scholar]
- [11].Under-vaccinated groups in Europe: Who are they and how to communicate with them in outbreak situations? Work Package 6 [Internet site]. Effective Communication in Outbreak Management for Europe. Available at: http://ecomeu.info/wp-content/uploads/2015/11/ECOM-Under-vaccinated-groups-in-Europe-WP6.pdf, accessed on 14 December 2016.
- [12].World Health Organization Regional Office for Europe. WHO EpiBrief, 2014, 2: 1–8. Available at: http://www.euro.who.int/__data/assets/pdf_file/0020/254234/EpiBrief_2_2014-rev3-with-data.pdf?ua=1. [Google Scholar]
- [13].Maltezou HC, Poland GA. Vaccination policies for healthcare workers in Europe. Vaccine 2014;32:4876–80. Available at: 10.1016/j.vaccine.2013.10.046. [DOI] [PubMed] [Google Scholar]
- [14].World Health Organization Regional Office for Europe. Copenhagen: 2016. Immunization highlights 2015, report of the WHO Regional Office for Europe. Available at: www.euro.who.int/__data/assets/pdf_file/0018/307620/Immunization-highlights-2015.pdf?ua=1. [Google Scholar]
- [15].Measles Nucleotide Surveillance database (MeaNS). www.who-measles.org.
- [16].Rubella Nucleotide Surveillance database (RubeNS). www.who-rubella.org.
- [17].World Health Organization. Meeting of the Strategic Advisory Group of Experts on immunization, October 2016 – conclusions and recommendations. Wkly Epidemiol Rec 2016;91:570–1. Available at: http://apps.who.int/iris/bitstream/10665/251810/1/WER9148.pdf?ua=1. [Google Scholar]
- [18].World Health Organization Regional Office for Europe. Regional Committee for Europe resolution EUR/RC55/R7 on strengthening national immunization systems through measles and rubella elimination and prevention of congenital rubella infection in WHO’s European Region. Copenhagen: WHO Regional Office for Europe; 2005. Available at: http://www.euro.who.int/__data/assets/pdf_file/0003/88086/RC55_eres07.pdf?ua=1. [Google Scholar]
- [19].World Health Organization Regional Office for Europe. Regional Committee for Europe. Sixtieth session; 2010. Renewed commitment to elimination of measles and rubella and prevention of congenital rubella syndrome by 2015 and sustained support for polio-free status in the WHO European Region. Available at: www.euro.who.int/__data/assets/pdf_file/0016/122236/RC60_eRes12.pdf?ua=1.
- [20].Biellik R, Davidkin I, Esposito S, Lobanov A, Kojouharova M, Pfaff G, et al. Slow progress in finalizing measles and rubella elimination in the European Region. Health Affairs 2016;35:322–6. [DOI] [PubMed] [Google Scholar]
- [21].Meeting report of 4th Meeting of the European Regional Verification Commission for Measles and Rubella Elimination, 26–29 October 2015, Copenhagen, Denmark. Available at: http://www.euro.who.int/__data/assets/pdf_file/0011/304958/4th-RVC-meeting-report.pdf?ua=1.
- [22].World Health Organization Regional Office for Europe. WHO EpiData, Oct. 2015 – Sept. 2016, 1–2. Available at: http://www.euro.who.int/__data/assets/pdf_file/0017/324206/EpiData-No03-2016.pdf?ua=1.
- [23].World Health Organization Regional Office for Europe. Framework for the verification process in the WHO European Region, Copenhagen, Denmark. Available at: http://www.euro.who.int/__data/assets/pdf_file/0009/247356/Eliminating-measles-and-rubella-Framework-for-the-verification-process-inthe-WHO-European-Region.pdf.
- [24].World Health Organization. Measles vaccines: WHO position paper. Wkly Epidemiol Rec 2009;84:359–60. [Google Scholar]
- [25].Meeting report of 15th meeting of the European Technical Advisory Group of Experts on Immunization (ETAGE), 30 September – 1 October 2015 Copenhagen, Denmark. Available at: http://www.euro.who.int/__data/assets/pdf_file/0008/295559/ETAGE-2015-Report.pdf?ua=1.