Abstract
Low distress tolerance, the perceived or actual inability to tolerate negative emotional states, is a transdiagnostic risk marker associated with greater PTSD symptoms and poorer treatment outcomes. However, the role of distress tolerance in PTSD symptom trajectories has not yet been explored. This study examined the mediating role of distress tolerance in PTSD symptom change among outpatients participating in a trial of computerized interventions for anxiety-related and mood-related risk factors. It was hypothesized that pre- to post-intervention change in distress tolerance would predict PTSD symptoms at three- and six-month follow-up, and mediate the effect of condition on PTSD symptoms above and beyond the effects of a competing mediator, anxiety sensitivity. Although condition differences in distress tolerance change were non-significant, distress tolerance change predicted month-three PTSD symptoms and mediated the direct effect of condition on month-three PTSD symptoms. After accounting for the direct effect of condition on month-six PTSD symptoms, distress tolerance change did not predict month-six PTSD symptoms. Findings suggest distress tolerance does play a longitudinal role in PTSD symptom change, and distress tolerance interventions may benefit certain samples who may otherwise not be able to immediately access, or remain in PTSD treatments.
Keywords: Posttraumatic stress disorder, distress tolerance, maintenance factor, treatment
1. Introduction
Posttraumatic stress disorder (PTSD), a Diagnostic and Statistical Manual of Mental Disorders (DSM-5) trauma- and stressor-related disorder, represents a constellation of four symptom clusters following exposure to a traumatic event: cognitive intrusions or re-experiencing; avoidance of internal and external trauma-associated stimuli; negative alterations in mood and beliefs; and changes in arousal and reactivity (American Psychiatric Association [APA], 2013). The estimated 12-month prevalence of PTSD is near 4% in the general population of United States adults. Despite significant personal and societal costs, only a minority of individuals with PTSD seek treatment (Kessler, 2000).
Several empirically supported treatments have been developed for PTSD, including cognitive processing therapy (CPT; Resick et al., 2007) and prolonged exposure (PE; Foa et al., 2007); however, it has been estimated that 30–50% of treatment-seekers are either non-respondent, remain substantially symptomatic, or drop out prior to treatment termination, which suggests that many individuals do not benefit from empirically supported treatments for PTSD (Bradley et al., 2005; Schottenbauer et al., 2008). One potential explanation for such poor rates outcomes is the high degree of comorbidity observed among individuals with PTSD, particularly mood and substance use disorders (Galatzer-Levy et al., 2013; Kessler et al., 1995). As a result, alternative transdiagnostic approaches to treating PTSD have been suggested (Gutner et al., 2016).
Distress tolerance represents one transdiagnostic risk marker, as low distress tolerance is associated with symptoms of eating pathology (Corstorphine et al., 2007), substance use disorders (Buckner et al., 2007), and PTSD (e.g., Banducci et al., 2016), among others. Distress tolerance has been conceptualized as one’s perceived or actual ability to tolerate negative experiential emotions, sensations, and states (Leyro et al., 2010). Therefore, trauma-exposed individuals with low distress tolerance may be less equipped to tolerate PTSD symptoms. This in turn may increase their efforts to avoid negative memories or emotions associated with their trauma, and create a negative feedback cycle to perpetuate their symptomology. Cross-sectional studies have demonstrated that low distress tolerance is related to greater PTSD symptom severity in non-clinical samples of trauma-exposed adults (Fetzner et al., 2014; Vujanovic et al., 2011a,b; Vujanovic et al., 2013). Evidence for this association has also been found among clinical samples of veterans with PTSD (Banducci et al., 2017) and acute care psychiatric inpatients with a history of trauma exposure (Vujanovic et al., 2016). Several studies have also examined the effect of low distress tolerance on PTSD symptom severity among clinical samples of individuals with comorbid PTSD and substance use disorders (Banducci et al., 2016; Vinci et al., 2016; Vujanovic et al., 2016). As support has grown for the concurrent relationship between distress tolerance and PTSD symptoms, distress tolerance has emerged as a potential maintenance factor (Stice, 2002) for PTSD symptoms, and therefore a plausible therapeutic target. Yet, little is known about the longitudinal role of distress tolerance in PTSD symptom maintenance.
To date, we are aware of only one study to have investigated the longitudinal effect of distress tolerance on PTSD symptoms. Banducci et al. (2017) demonstrated that increases in distress tolerance across treatment predicted lower PTSD symptoms at discharge. These results further corroborate the putative role of distress tolerance in PTSD symptom maintenance, such that increases in perceived ability to cope with negative experiences were associated with lower reported distress related to PTSD symptoms. Though this study marks a promising initial step in delineating the role of distress tolerance in PTSD symptom change, several limitations preclude its generalizability. Namely, the study sample was primarily (97%) male, and all were veterans receiving intensive and combined forms of residential treatment. Most importantly, because distress tolerance and PTSD symptoms were assessed at the same time points, we cannot draw any specific conclusions about distress tolerance as a chronologically sufficient mechanism (i.e., mediator) for PTSD symptom change.
1.1. The present study
The extant literature suggests distress tolerance may be a maintenance factor for PTSD. However, we are unaware of any study that has demonstrated that changes in distress tolerance mediate changes in PTSD symptoms, as would be the case for a maintenance factor (Stice, 2002). The current study sought to address this gap in the literature by evaluating whether changes in distress tolerance mediate subsequent changes in PTSD symptoms following intervention.
These data were taken from a PTSD-diagnosed subsample of outpatient adults enrolled in a randomized clinical trial (RCT) that evaluated two computerized interventions for reducing suicide-relevant risk factors. The first intervention, which targeted stress sensitivity (i.e., Anxiety condition), has previously been shown to reduce anxiety sensitivity and increase distress tolerance (Norr et al., 2014), two interrelated facets of a higher-order “affect tolerance and sensitivity” (Bernstein et al., 2009) that are strongly related to PTSD. This intervention has been demonstrated to reduce PTSD symptoms among trauma-exposed samples, in part through reductions in anxiety sensitivity (Allan et al., 2015; Short et al., 2017). However, no studies have investigated whether increases in distress tolerance further account for this association above and beyond changes in anxiety sensitivity. The second intervention targeted interpersonal constructs relevant to feelings of social isolation (i.e., perceived burdensomeness and thwarted belongingness) closely associated with mood disorders. Although there is no prior evidence to suggest that this intervention would directly affect distress tolerance, low distress tolerance is related to negative affect and mood (Leyro et al., 2010), and may be more strongly tied to negative affect and anhedonic depressive symptoms than anxious arousal (Bernstein et al., 2009). Thus, it may be hypothesized that this intervention, by targeting features of depression, could increase distress tolerance more than the third, wait-list condition (i.e., Repeated Contact Control).
In the present study, we hypothesized (1) a significant time by condition interaction such that pre- to post-intervention increases in distress tolerance would be greater among participants randomized to the Anxiety and Mood interventions than Repeated Contact Control. We also hypothesized that, (2) controlling for baseline PTSD symptoms, depression symptoms, and participant sex, pre- to post-intervention changes in distress tolerance would predict PTSD symptoms at three- and six-month follow-ups. To test distress tolerance as a mechanism of PTSD symptom change, we hypothesized that (3) pre- to post-intervention changes in distress tolerance would mediate the relationship between intervention condition and PTSD symptoms at three- and six-month follow-up. Finally, we hypothesized that (4) mediation would be evident of distress tolerance, above and beyond the influence of anxiety sensitivity as a parallel mediator.
2. Methods
2.1. Participants and procedures
Individuals were recruited from a community in the southeastern United States to participate in a larger treatment study (N=304) designed to examine the effects of computer-based interventions on suicide (clinicaltrials.gov #NCT01941862). Following a brief phone screen, individuals who met initial screening criteria were brought into the clinic, consented, administered a battery of self-report measures, and completed the Structured Clinical Interview for DSM-5–Research Version (SCID-5-RV; First et al., 2015) during a baseline appointment. Eligible participants were required to be at least 18 years of age and demonstrate elevated levels of suicide-relevant risk factors (i.e., anxiety sensitivity, perceived burdensomeness, thwarted belongingness). Exclusion criteria included the presence of current or past psychotic spectrum disorders, unmedicated bipolar spectrum disorders, significant suicidal intent requiring immediate hospitalization, and/or participation in current psychotherapy.
Eligible participants were randomized to one of four conditions; three active conditions (see Experimental Conditions below), or a Repeated Contact Control (RCC). Following randomization at the baseline appointment, participants returned to complete one intervention session during the next three consecutive weeks. Participants returned to complete a battery of follow-up self-report measures at three and six months following their last intervention session. Participants were compensated a pre-determined sum at the end of each appointment based on estimated time-commitment. All procedures were approved by the university’s Institutional Review Board.
As an extension of the findings reported by Banducci et al. (2017), participants were included in the present analyses only if they met DSM-5 criteria for PTSD. Moreover, participants were selected if they were randomized to either the RCC control (N=14), Anxiety (N=18), or Mood conditions (N=22). Participants randomized to a fourth condition, which combined the active components of both the Anxiety and Mood condition, were excluded from the present analyses because there was no way to account for the additional time they spent participating in the interventions. Thus, 54 participants were included in the present analyses.
The sample was largely female (61.1%), and varied in age (M=38.78; SD=14.95). Ethnic composition was 57.4% White/Caucasian, 29.6% African American, 3.8% Native American, and 9.2% ‘Other’. Additionally, 42.6% of participants were veterans. PTSD was the primary diagnosis for 59.3% of the sample. The most common index trauma reported was sexual assault (36.4%), followed by physical assault (21.8%), sudden death of a family member (20.0%), combat (14.6%), death or serious injury to a family member (3.6%), motor vehicle accident (1.8%), and repeated exposure as a first responder (1.8%). The average time elapsed since the index trauma was 41.8 months (SD=32.4). Most participants (64.8%) had a comorbid depressive disorder diagnosis (i.e., major depressive disorder, persistent depressive disorder, depressive disorder not otherwise specified) at baseline, and 16.7% of the sample was diagnosed with at least one substance use disorder. The number of diagnoses per participant at baseline ranged from 1–8 (M=3.52; SD=1.52).
2.2. Experimental conditions
2.2.1. Anxiety condition.
Individuals randomized to receive the anxiety condition completed the Cognitive Anxiety Sensitivity Treatment (CAST). A complete description of CAST is provided by Schmidt et al., (2014); briefly, CAST is a 45-minute computerized intervention that models the educational and behavioral techniques typically used in anxiety treatments. It comprises a psychoeducational component that explains why feared symptoms of anxiety are not in fact dangerous and a brief set of interoceptive exercises (i.e., hyperventilation) to demonstrate that conditioned fear responses to anxiety symptoms can be corrected.
In addition to completing one session of CAST, individuals randomized to the anxiety condition also completed an anxiety sensitivity focused cognitive bias modification (CBM) program (CBM-I for AS; see Capron and Schmidt, 2016 for complete description). CBM-I for anxiety sensitivity presents participants with multiple trials in which a word appears for 1 second (e.g. “excited”), followed by a sentence (e.g. “You notice your heart is beating faster”). The word and sentence create a benign meaning on half of the trials (as in the previous example), and an anxious meaning in the other half of the trials (e.g. “stressful” followed by the sentence “Your mind is full of thoughts”). Participants were instructed to indicate, yes or no, whether the word was related to the sentence, and were given feedback during training regarding whether responses were “correct” or “incorrect.” Judging anxious combinations to be “unrelated” and benign combinations as being “related” would produce a “correct” response message. Conversely, judging anxious combinations as “related” and benign combinations as “unrelated” would produce an “incorrect” response message, accompanied by an 85-decibel horn blast. One session of CBM-I for anxiety sensitivity consists of a baseline interpretation bias assessment period (40 trials with no reinforcement); a first training block (80 trials with reinforcement); a filler task (5 minutes of simple math problems); a second training block (80 trials with reinforcement); and a follow-up assessment period to measure bias change (40 trials with novel word-sentence pairs).
2.2.2. Mood Condition.
Like the anxiety condition, the mood condition included a top-down psychoeducational portion followed by a bottom-up CBM exercise. However, the content of the psychoeducation and CBM-I components of the mood condition were specific to empirical correlates of suicidality (Joiner, 2005), perceived burdensomeness (PB) and thwarted belongingness (TB), rather than anxiety and stress. Participants completed a 50-minute, fully-computerized intervention that models the educational and behavioral techniques common to depression treatments. The psychoeducation portion of the mood condition used CBT principles to modify problematic thoughts and behaviors related to PB/TB. As such, the mood intervention was developed in consultation with experienced clinicians well-versed in treating suicidal individuals experiencing PB/TB. The program emphasizes that social interaction is a critical human need, and negative beliefs about isolation and being a burden are usually inaccurate. Following psychoeducation, the mood condition introduced behavioral activation techniques (e.g., volunteering, time with friends) as a means of decreasing isolation and burdensomeness.
In addition to the computerized mood intervention, individuals randomized to the mood condition also completed the Cognitive Bias Modification (CBM)–Mood Interpretation Bias (MIB). CBM-MIB was programmed in E-Prime utilizing the positive CBM-I paradigm developed by Holmes et al. (Holmes et al., 2006). In the present CBM-MIB, participants were presented with 100 scenarios across five training blocks of 20 scenarios. Each scenario, which lasted 10–13 seconds, was read aloud to the participant (via headphones) in a female voice, with 2-second gaps in between each scenario. All scenarios began ambiguously, but were designed to be resolved positively (e.g. “At your computer lesson you finish your work early so the lecturer gives you a new task to do. You don’t understand the task so you ask for help. The lecturer tells you that your request is the sign of being a good student”). Participants were directed to imagine the events while listening to each scenario, and after each passage subsequently prompted to rate the vividness of imagery (“How vividly could you imagine the situation that was described?”) using a 5-point Likert scale ranging from 1 (not at all vivid) to 5 (extremely vivid). Given that all scenarios had more than one possible outcome, the overarching aim of the trials was to train participants to generate positive outcomes to ambiguous situations that could have resolved in less desirable ways.
2.2.3. Repeated Contact Control Condition.
Individuals randomized to the RCC condition reported to the clinic once per week for three consecutive weeks just as those the Anxiety and Mood condition did, and completed the same set of self-report measures each week. Each RCC session also consisted of a face-to-face suicide risk assessment with a trained graduate-level clinician.
2.3. Diagnostic interview
2.3.1. Structured Clinical Interview for DSM-5–Research Version (SCID-RV).
The SCID-RV (First et al., 2015) was administered to evaluate participants’ current diagnostic status and trauma history at baseline. SCIDs were administered by clinical psychology graduate students, all of whom completed extensive training in SCID administration and scoring via SCID training tapes, live observation of SCID administrations, and practice interviews with experienced psychologists. All SCID results were reviewed by a licensed clinical psychologist to confirm diagnostic accuracy. This training process has produced high inter-rater reliability within our clinic during prior investigations (k=0.86; Schmidt et al., 2017).
2.4. Self-report measures
2.4.1. Beck Depression Inventory-II (BDI-II).
The BDI-II is a 21-item self-report questionnaire administered to assess depression symptom severity (Beck et al., 1996). The BDI-II is widely used and has been shown to possess strong psychometric properties among both nonclinical and clinical samples (Endler et al., 1999). The BDI-II was completed at baseline, and used to covary for depression symptoms in the present analyses. In the present study, scores on the BDI-II demonstrated excellent reliability (α=0.92).
2.4.2. Distress Tolerance Scale (DTS).
The DTS is a self-report measure used to assess an individual’s perceived ability to tolerate negative emotional states or experiences (Simons and Gaher, 2005). Participants are presented with 15 statements pertaining to distress (e.g. “I can’t handle feeling distressed or upset”), and asked to rate them on a 5-point Likert scale ranging from 1 (strongly agree) to 5 (strongly disagree). Consistent with scoring procedures reported in the initial validation study (Simons and Gaher, 2005), all DTS items were sum-scored and averaged to produce a DTS total score ranging from 1–5. Higher scores represent greater perceived ability to tolerate experiential distress. The DTS was administered during the baseline assessment session (i.e., pre-intervention) and again after the third and final intervention session (i.e., post-intervention). Scores on the DTS in the present study demonstrated excellent internal consistency at pre- and post-intervention (α’s=0.90 and 0.91, respectively).
2.4.3. Anxiety Sensitivity Index-3 (ASI-3).
The ASI-3 (Taylor et al., 2007) is an 18-item self-report measure that assesses the degree to which individuals fear the potentially negative consequences of anxiety-related symptoms and/or sensations (Reiss and McNally, 1985). Items are rated on a scale from 0 (very little) to 4 (very much). The ASI-3 has good internal consistency and good convergent, discriminant, structural, and criterion-related validity (Taylor et al., 2007). In the present study, the ASI-3 was administered with the DTS at pre-intervention and post-intervention and demonstrated excellent internal consistency at each time point (α’s=0.94)
2.4.4. PTSD Checklist- Civilian Version (PCL-C).
The PCL-C (Weathers et al., 1991) is a 17-item self-report measure designed to assess past-month severity of DSM-IV (APA, 2000) PTSD symptoms. Individuals are asked to rate the extent to which they have been bothered by various problems resulting from a stressful experience on a 5-point Likert-style scale from 1 (not at all) to 5 (extremely), with possible scores ranging from 17 to 85, with greater scores indicating greater PTSD symptom severity. The PCL-C has been shown to have good psychometric properties (Blanchard et al., 1996). In the present sample, scores on the PCL-C demonstrated excellent internal consistency at baseline, month-three and six-month follow-up (α’s= 0.94, 0.95, and 0.95, respectively).
2.5. Statistical analysis
All study variables were screened for skew, kurtosis, and outliers, and found to be within acceptable ranges (Gravetter et al., 2016). Missing values analysis of all study variables revealed that 14.7% of all values were missing. This amount was accounted for by 51.9% of month-six PCL-C scores (range of missingness per condition = 45.5–64.3%), 29.6% of month-three PCL-C scores (range = 21.4–36.4%), 18.5% of post-intervention DTS scores (range = 11.1–22.7%), and 18.5% of ASI-3 scores missing (range = 11.1–22.7%). Data were determined to be missing at random given a non-significant value for Little’s test (χ2[3]=4.27, p=0.234), and non-significant chi squared values (p’s >0.5) for tests of case missingness across intervention conditions for the abovementioned variables. Missing values were replaced using multiple imputation by fully conditional specification (Liu and De, 2015) in SPSS version 22.0. Variables in the imputation models included: pre-intervention PCL-C, DTS, and ASI-3; post-intervention DTS and ASI-3; and month-three PCL-C scores. Using a conservative approach to assume 20% missing values and 95% confidence intervals, 23 imputations were used to derive value estimates for the study variables (Bodner, 2008). The process outlined above was used to impute values separately for each condition (Sullivan et al., 2016). Full descriptive statistics, including bivariate correlations, are presented in Table 1.
Table 1.
Bivariate correlations and descriptive statistics for study variables across all study time points.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Condition | -- | |||||||||||
| 2. Sex | 0.02 | -- | ||||||||||
| 3. BL BDI-II | −0.07 | −0.04 | -- | |||||||||
| 4. Pre ASI-3 | 0.26 | 0.25 | 0.44** | -- | ||||||||
| 5. Post ASI-3 | 0.45** | 0.12 | 0.17 | 0.68** | -- | |||||||
| 6. Pre DTS | 0.24 | 0.01 | −0.25 | −0.19 | 0.07 | -- | ||||||
| 7. Post DTS | −0.10 | −0.30* | 0.08 | −0.25 | −0.26 | 0.24 | -- | |||||
| 8. BL PCL-C | −0.01 | −0.07 | 0.65** | 0.39** | 0.25 | −0.33* | −0.04 | -- | ||||
| 9. M3 PCL-C | 0.21 | −0.01 | 0.57** | 0.40** | 0.39** | −0.14 | −0.27* | 0.72** | -- | |||
| 10. M6 PCL-C | 0.51** | 0.09 | 0.41** | 0.41** | 0.49** | 0.08 | −0.27* | 0.47** | 0.73** | -- | ||
| 11. Δ ASI-3 | 0.38** | −0.07 | −0.18 | 0.00 | 0.73** | 0.28* | −0.12 | −0.02 | 0.16 | 0.28* | -- | |
| 12. Δ DTS | −0.16 | −0.31* | −0.03 | −0.21 | −0.28* | 0.00 | 0.97** | 0.04 | −0.24 | −0.30* | −0.19 | -- |
| M | 0.93 | 1.61 | 28.54 | 36.70 | 27.85 | 2.60 | 2.59 | 58.35 | 47.83 | 41.70 | −8.85† | −0.01† |
| SD | 0.77 | 0.49 | 12.77 | 17.17 | 16.86 | 0.90 | 1.10 | 15.85 | 15.95 | 13.26 | 13.59† | 1.24† |
| Range | 0 – 2 | 1 – 2 | 3 – 60 | 5 – 72 | 1 – 72 | 1 – 5 | 0 – 5 | 27 – 85 | 17 – 85 | 18 – 85 | −48 – 23† | −3.67 – 2.88† |
Note. Condition coded as 0 (Anxiety), 1 (Mood), and 2 (RCC); BL = Baseline time point; Pre = Pre-intervention; Post = Post-intervention; M3 = Month-three follow-up; M6 = Month-six follow-up; BDI-II = Beck Depression Inventory-II; ASI-3 = Anxiety Sensitivity Index-3; DTS = Distress Tolerance Scale; PCL-C = PTSD Checklist- Civilian Version; Δ ASI-3 = ASI-3 residualized change score; Δ DTS = DTS residualized change score.
p < 0.05
p < 0.01
Raw change scores (Post-intervention minus pre-intervention) displayed for mean, standard deviation, and range
A two by three time (pre-, post-intervention) by group (Anxiety, Mood, RCC) repeated measures ANOVA was conducted to test the first hypothesis, that DTS distress tolerance scores would increase more among the Anxiety and Mood conditions than the RCC control condition. Significant effects were probed with follow-up comparisons, with Tukey’s HSD corrections applied. Because the raw change scores examined in repeated measures ANOVA do not account for individual differences in baseline DTS distress tolerance, a separate ANOVA was conducted to test for group differences in residualized DTS distress tolerance change scores as well. DTS residualized change scores were calculated by regressing post-intervention DTS scores on pre-intervention DTS scores; standardized residuals were then saved for use as our treatment distress tolerance treatment outcome variable. Residualized DTS change scores were used in the mediation analyses as a more stringent test than raw change scores.
An analysis of covariance (ANCOVA) was conducted to test the hypothesis that pre- to post-intervention changes in distress tolerance (i.e., DTS residualized change scores) would predict PCL-C PTSD symptoms at month-three follow-up, over and above the effect of intervention condition, and controlling for baseline PCL-C PTSD symptoms. Given previously reported gender differences in distress tolerance (Simons and Gaher, 2005), sex was covaried in each model. Because depression and PTSD symptoms are highly comorbid (e.g., Campbell et al., 2007), baseline BDI-II scores were controlled for in each analysis. Finally, pre- to post-intervention change in our alternate mediator, anxiety sensitivity (i.e., ASI-3 residualized change scores) were included in the model. A separate ANCOVA was conducted with the same independent variables predicting PCL-C symptom severity at month-six follow-up. Significant main effects of distress tolerance change on PTSD symptoms at either three- or six-month follow-up were then to be tested for significant indirect effects.
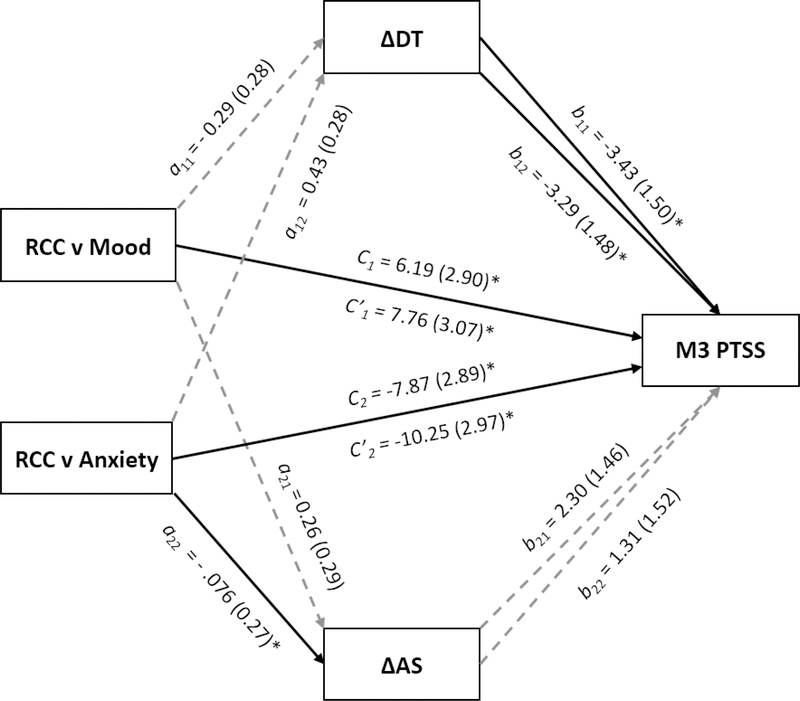
To test the hypothesis that pre- to post-intervention changes in distress tolerance mediate the relationship between intervention condition and PTSD symptoms at follow-up, multiple mediation models (Figure 1) were conducted. Based on a prior expectations that changes in distress tolerance would be greater among the Anxiety and Mood conditions compared to controls, the multicategorical (k=3) condition variable was dummy coded to conduct two (k-1) mediation models (Hayes and Preacher, 2014) in which the RCC control condition served as a reference variable. The PROCESS macros for SPSS (Hayes, 2012) was used to estimate 5,000 bias-corrected bootstrap samples, from which a 97.5% confidence interval (CI) to was created to test the indirect effects through our mediator variables. To correct for the comparison of indirect effects across two independent mediation models (i.e., Mood v. RCC, Anxiety v. RCC) on the same outcome variable, 97.5% CIs were employed (Hayes and Preacher, 2014). Participant sex, and baseline PCL-C and BDI-II symptoms were added as covariates. The indirect effect of condition on PTSD symptoms were tested via two competing mediators: pre- to post-intervention DTS residualized change scores, and pre- to post-intervention ASI-3 change scores. Indirect effects were considered significant if the 97.5% CI of a variable’s respective effect did not contain a value of zero.
Figure 1.
Multiple mediation model of total and direct effects of intervention condition on PCL-C scores at the month-three follow-up through distress tolerance and anxiety sensitivity.
Note. RCC v Mood model coded as 0 (RCC), 1 (Mood), 0 (Anxiety); RCC v Anxiety model coded as 0 (RCC), 0 (Mood), 1 (Anxiety); Unstandardized path coefficients displayed with standard error in parentheses; ΔDT = pre- to post-intervention DTS residualized change score month; ΔAS = pre- to post-intervention ASI-3 residualized change score; Partial effects of sex, baseline PCL-C score, and baseline BDI-II score model covariates are not depicted in figure.
*p < 0.05
3. Results
3.1. Repeated Measures and Univariate ANOVA Models
A 2×3 time (pre-, post-intervention DTS distress tolerance scores) by group (Anxiety, Mood, RCC) repeated measures ANOVA was conducted to test whether DTS distress tolerance scores changed at distinct levels among the three treatment conditions. There were no main effects of time (F[1,51]=0.01, p=0.97, ηp2 < 0.001) or condition (F[1,51]=0.17, p=0.84, ηp2 =0.007). However, there was a significant time by condition interaction (F[2,51]=3.98, p=0.03, ηp2=0.135) in which DTS distress tolerance scores increased from pre (EMM=2.20, SE=0.21) to post (EMM=2.81, SE=0.26) among the Anxiety condition, but decreased from pre (EMM=2.85, SE=0.19) to post (EMM=2.43, SE=0.24) among the Mood condition and to a lesser degree from pre (EMM=2.72, SE=0.23) to post (EMM=2.55, SE=0.30) among the RCC condition. This significant time by condition interaction was probed by three planned comparisons with Tukey’s WSD correction applied. Differences in raw change scores were in the expected direction but non-significant among the Anxiety condition compared to the RCC control condition (p=0.16), and significant compared to the Mood condition (p=0.02). Raw DTS change scores were not significantly difference between the Mood and RCC condition (p=0.81).
To determine whether residualized changes in DTS distress tolerance scores were larger (i.e., greater improvement in distress tolerance) among the Anxiety and Mood conditions than the RCC condition, the condition variable was entered into a univariate ANOVA model predicting a pre- to post-intervention residualized DTS change scores. Contrary to hypothesis, condition did not significantly predict DTS residualized change scores (F[2,51]=1.49, p=0.24, ηp2=0.055), and thus no post-hoc comparisons were conducted.
3.2. ANCOVA Models
The hypothesized effect of change in distress tolerance on PTSD symptoms at month-three follow-up was tested in an ANCOVA model (Table 2). The overall model was significant (F[7,46]=13.69, p< 0.001, ηp2=0.676). As hypothesized, residualized DTS distress tolerance change scores significantly predicted PCL-C PTSD symptoms at month-three follow-up (F[1,46]=4.73, p=0.04, ηp2=0.093), such that increases in distress tolerance predicted lower PTSD symptoms after three months. Intervention condition (F[2,46]=3.63, p=0.04, ηp2=0.136) significantly predicted month-three PCL-C PTSD symptoms. Tukey HSD-corrected pairwise comparisons indicated that month-three PCL-C scores were lower (p=0.03) among the Anxiety condition (EMM=42.60, SE=2.45) compared to the Mood condition (EMM=51.62, SE=2.15) and statistically equivalent between the Anxiety and RCC condition (EMM=48.59, SE=2.71; p=0.35), albeit in the expected direction. No differences were observed in month-three PCL-C scores between the Mood and RCC conditions (p=1.00). Among covariates, only baseline PCL-C PTSD symptoms (F[1,46]=31.39, p< 0.001, ηp2=0.406) were related to month-three PCL-C PTSD symptoms.
Table 2.
ANCOVA models predicting PCL-C total scores at follow-up.
| Month 3 PCL-C | Month 6 PCL-C | |||||
|---|---|---|---|---|---|---|
| Predictors | F | p | ηp2 | F | p | ηp2 |
| Sex | 0.20 | 0.66 | 0.004 | 0.30 | 0.59 | 0.006 |
| Δ AS | 0.92 | 0.34 | 0.02 | 1.16 | 0.29 | 0.025 |
| BL BDI-II | 2.40 | 0.13 | 0.050 | 2.85 | 0.10 | 0.058 |
| BL PCL-C | 31.39 | < 0.001 | 0.406 | 9.30 | < 0.01 | 0.168 |
| Condition | 3.63 | 0.04 | 0.136 | 11.84 | < 0.001 | 0.340 |
| Δ DTS | 4.73 | 0.04 | 0.09 | 2.80 | 0.10 | 0.057 |
Note. BL = Baseline time point; Month 3 = Month-three follow-up time point; Month 6 = Month-six follow-up time point; BDI-II = Beck Depression Inventory-II; PCL-C Total = PTSD Checklist- Civilian Version Total score; Δ DTS = pre- to post-intervention DTS residualized change score; Δ AS = pre- to post-intervention ASI-3 residualized change score; ηp2 = partial eta squared.
A similar model was used to test the effect of change in distress tolerance on PTSD symptoms at month-six follow-up. The overall model was significant (F[7,46]=10.35, p< 0.001, ηp2=0.612). Unlike the previous model, residualized DTS distress tolerance change scores did not significantly predict PCL-C PTSD symptoms at month-six follow-up (F[1,46]=2.80, p=0.10, ηp2=0.057); however, intervention condition did (F[2,46]=11.84, p< 0.001, ηp2=0.340). Tukey HSD-corrected pairwise comparisons suggested that month-six PCL-C PTSD symptoms were significantly lower (p’s < 0.01) among the Anxiety condition (EMM=32.76, SE=2.23) compared to the Mood (EMM=44.97, SE=1.95) and RCC condition (EMM=48.07, SE=2.47), and that symptoms did not differ between the Mood and RCC condition (p = 0.99). Baseline PCL-C PTSD symptoms (F[1,46]=9.30, p< 0.01, ηp2=0.168) remained the only significant covariate. Because distress tolerance change did not predict PTSD symptoms at month-six follow-up, a mediation model testing the indirect effect of condition on month-six PTSD symptoms through change in distress tolerance was not conducted.
3.3. Multiple mediation model
To test the hypothesis that pre- to post-intervention changes in distress tolerance mediate the relationship between intervention condition and month-three PTSD symptoms, two multiple mediation models (Figure 1) were conducted to compare this effect between the RCC control and Mood condition, and RCC control and Anxiety condition. Participant sex, baseline PCL-C PTSD symptoms and baseline BDI-II depression symptoms were controlled for in each model. Indirect effects of intervention condition on month-three PTSD symptoms were tested via two alternate mediators: residualized change scores calculated for pre-to post intervention changes in DTS distress tolerance and ASI-3 anxiety sensitivity.
The full mediation model comparing the RCC control and Mood condition accounted for a significant portion of variance (F[6,47]=15.06, p< 0.001, r2=0.658) in PCL-C PTSD symptoms at month-three follow-up. There were no effects of condition on pre- to post-intervention change in DTS distress tolerance (a11) or ASI-3 anxiety sensitivity (a21). There was a significant negative effect of pre- to post-intervention change in DTS distress tolerance (b11) on month-three PCL-C PTSD symptoms, such that increased distress tolerance predicted lower month-three PTSD symptoms. There was no effect of pre- to post-intervention change in ASI-3 anxiety sensitivity (b21) on month-three PTSD symptoms. Partial effects on month-three PCL-C PTSD symptoms were non-significant for the participant sex (B=−1.23, SE=2.95, 97.5%CI [−7.158, 4.706]) and pre-intervention BDI-II depression symptom (B=0.22, SE=0.15, 97.5%CI [−0.074, 0.513]) covariates, and significant for pre-intervention PCL-C PTSD symptoms (B=0.65, SE=0.12, 97.5%CI [0.416, 0.891]). There was a significant direct effect of condition on month-PTSD symptoms (c1), such that PCL-C scores were, on average, 6.19 points lower among the RCC control condition than the Mood condition. There were no significant indirect effects of condition on month-three PCL-C PTSD symptoms observed through either pre- to post-intervention DTS distress tolerance (B=0.98, SE=1.17, 97.5%CI [−0.773, 4.139]) or ASI-3 anxiety sensitivity change (B=0.60, SE=0.86, 97.5%CI [−0.534, 3.108]).
The full mediation model comparing the RCC control and Anxiety condition accounted for a significant portion of variance (F[6,47]=15.92, p < 0.001, r2=0.670) in PCL-C PTSD symptoms at month-three follow-up. The effect of condition on pre- to post-intervention change in DTS distress tolerance (a12) displayed a non-significant trend (p=0.13) in the expected direction, such that the Anxiety condition displayed increases in distress tolerance whereas the RCC control condition displayed a slight decrease from pre- to post-intervention. There was a significant effect of intervention condition on pre-to post-intervention ASI-3 anxiety sensitivity change (a22), with greater decreases in anxiety sensitivity among the Anxiety condition. There was a significant negative effect of pre- to post-intervention change in DTS distress tolerance (b12) on month-three PCL-C PTSD symptoms, such that increased distress tolerance predicted lower month-three PTSD symptoms. There was no effect of pre- to post-intervention change in ASI-3 anxiety sensitivity (b22) on month-three PTSD symptoms. Partial effects on month-three PCL-C PTSD symptoms were non-significant for the participant sex (B=−1.17, SE=2.89, 97.5%CI [−6.99, 4.644]) and pre-intervention BDI-II depression symptom (B=0.24, SE=0.14, 97.5%CI [−0.047, 0.525]) covariates, and significant for pre-intervention PCL-C PTSD symptoms (B=0.63, SE=0.11, 97.5%CI [0.402, 0.857]). There was a significant direct effect of condition on month- PTSD symptoms (c2), such that PCL-C scores were, on average, 7.87 points lower among the Anxiety condition than the RCC control condition. Consistent with hypothesis, there was a significant indirect effect of condition on month-three PCL-C PTSD symptoms observed through pre- to post-intervention DTS distress tolerance change (B=−1.40, SE=0.92, 97.5%CI [−4.712, −0.005]). The ratio of the DTS distress tolerance indirect effect to the direct effect of condition on month-three PCL-C PTSD symptoms was 0.32. There was no indirect effect observed through ASI-3 anxiety sensitivity change (B=0.98, SE=1.55, 97.5%CI [−0.663, 4.399]).
4. Discussion
The purpose of the current study was to extend recent findings that longitudinal increases in distress tolerance are related to reductions in PTSD symptoms. Results revealed that, although condition differences in distress tolerance change failed to reach significance, pre- to post-intervention changes in distress tolerance were a significant predictor of PTSD symptoms at three-month follow-up. Contrary to hypothesis, distress tolerance changes did not predict PTSD symptoms at six-months; however, this may have been in part due to a large and significant direct effect of intervention condition on six-month PTSD symptoms. Consistent with hypothesis, pre- to post-intervention changes in distress tolerance significantly mediated the effect of intervention condition on month-three PTSD symptoms.
Although most of our hypotheses were supported, we did observe null results that were contrary to hypotheses or did not replicate results reported in prior studies. Anxiety sensitivity change did not mediate three-month PTSD symptoms, which countered expectations based on prior reports (Allan et al., 2015; Short et al., 2017). However, several important differences between those studies and the current one may account for this pattern of results, including nonclinical (i.e., trauma exposed) versus clinical samples and one-month versus three-month follow-up time frames. Related to this, although we observed differences in month-three PTSD symptoms between the Anxiety and RCC condition that were in the expected direction, they failed to reach significance; however, as time elapsed and this gap widened, month-six PTSD symptoms were indeed lower for the Anxiety condition. Unexpectedly, the Mood condition demonstrated reductions in DTS distress tolerance scores rather than increases, and perhaps as a result, more modest decreases in PTSD symptoms that never differed significantly from the RCC control condition. Although the Mood condition had never been tested as an intervention for distress tolerance or PTSD symptoms, we hypothesized that it would impact both given that mood symptoms are empirically associated with distress tolerance (Bernstein et al., 2009; Leyro et al., 2010) and social withdrawal and mood symptoms are a clinical feature of PTSD (APA, 2013). We did not observe a direct effect of the Mood intervention on distress tolerance at post-intervention, leaving open the possibility that distress tolerance may be indirectly affected over a longer time frame through improvements in mood or decreases in social withdrawal – hypotheses which may be tested in future studies. Similarly, although the Mood intervention’s focus is to improve social functioning, PTSD is traditionally marked by behavioral avoidance, which would introduce social impairment; therefore, although the Mood intervention encourages renewing social contact, behavioral avoidance may act as a barrier to global symptom improvement at the level seen in the Anxiety condition, which directly aims to correct behavioral avoidance.
Power was indeed an issue in this study, as we did not observe the hypothesized effect of condition on distress tolerance change for either raw change scores or residualized change scores in the ANOVA or mediation models. Although the condition means of distress tolerance change were in the expected direction, a post hoc analysis revealed that power to detect a significant condition effect in the present sample was .69 for raw change scores, but only 0.30 for residualized change scores. While this is likely due in part to the fact that residualized change scores account for individual differences among baseline scores, power to detect effects using residualized change scores suffers compared to raw change scores when the reliability of a measure is any less than perfect (Kisbu-Sakarya et al., 2013). Ultimately, observed direct effects of distress tolerance change on three-month PTSD symptoms, and a significant indirect effect of condition on three-month PTSD symptoms through changes in distress tolerance are promising, and suggest further study among larger samples is warranted to delineate the longitudinal role of distress tolerance in PTSD symptom maintenance.
Cross-sectional relationships between distress tolerance and PTSD symptoms have been replicated across a variety of samples, which has prompted discussion of the theoretical role of distress tolerance in the experience of PTSD symptoms. Though PTSD symptoms are distressing in and of themselves, low distress tolerance individuals may perceive the subjective experience of PTSD symptoms as more distressing than high distress tolerance individuals, leading to greater impairment. Alternatively, low distress tolerance individuals may perceive themselves as less capable of coping with PTSD symptoms, increasing efforts to avoid situations, emotions, or reminders of an index trauma in a manner that serves to maintain symptom severity (Dunmore et al., 1999). Thus, increasing distress tolerance would theoretically decrease efforts to avoid PTSD-relevant symptoms and stimuli, thereby reducing distress and impairment. Moreover, increased efficacy in tolerating distress associated with PTSD symptoms may also facilitate engagement in PTSD-specific treatments such as PE or PCT. This putative role of distress tolerance in PTSD symptoms remediation therefore has several clinical implications.
4.1. Clinical implications
Contemporary models of inhibitory learning suggest that the ability to tolerate distress allows an individual to complete goal-directed exposures, which disconfirm fear-expectancies and allow fear extinction (Craske et al., 2008). Indeed, evidence suggests that most individuals do not demonstrate reliable between-session reductions in subjective distress over 10 sessions of prolonged exposure, yet achieve significant reductions in PTSD symptoms (Bluett et al., 2014). Coupled with our findings that increased distress tolerance mediates PTSD symptom change, this suggests that reductions in exposure-related distress may be less important to symptom improvement than one’s perceived ability to tolerate and approach the temporarily distressing aspects of PTSD treatment. Brief adjunct treatment components designed explicitly to increase distress tolerance, such as the one described in this study, may therefore help to facilitate PTSD treatment compliance or retention. Although such phased treatment approaches have been deemed generally unnecessary for effective PTSD treatment (Jongh et al., 2016), it is important to consider that there may be specific samples for whom brief and portable distress tolerance interventions may be of benefit.
Although we possess empirically supported treatments for PTSD, they are not immediately accessible to a significant portion of individuals. Military veterans have noted several practical barriers to mental health services, including insufficient time with health care providers (Hoge et al., 2014). Although service utilization has increased through the Veterans Healthcare Administration in recent years, the underlying data indicate that wait times for initiating treatment may be longer than a month (Mott et al., 2014). Among civilians, ethnic minorities report difficulty accessing quality mental health services (Davis et al., 2008) and are more likely to have delayed access to mental health services (Wells et al., 2001). For samples such as these, efforts to initiate mental health services with delayed or no success are frustrating, and may therefore lead to less persistence or follow-through with PTSD treatment. For individuals who initiate contact with mental health professionals but face delays in beginning PTSD treatment, brief and portable interventions for maintenance factors like distress tolerance present a potential stop-gap solution prior to the availability of PTSD treatment. For those whom PTSD treatment is immediately available, Jongh et al. (2016) have called into question the necessity of phase-based treatment approaches, arguing that stabilization phases provide no incremental value and may instead delay the full benefits of trauma-focused treatments. However, these authors acknowledge that the literature base for phased-based treatment of PTSD has excluded several subgroups, including individuals with comorbid substance use disorders. Importantly, supplementing PTSD treatment with distress tolerance interventions may be most useful in samples with comorbid PTSD and substance use. Distress tolerance has been shown to mediate the relationship between PTSD and substance use (Duranceau et al., 2014; Potter et al., 2011; Vujanovic et al., 2011), potentially because low distress tolerance individuals may use substances to avoid distressing PTSD symptoms (Bremner et al., 1996; Chilcoat and Breslau, 1998; Jacobsen, et al., 2001). Increasing distress tolerance may therefore decrease substance use, increase approach tolerance of PTSD symptoms, and promote recovery. Moreover, slower PTSD symptom reductions are associated with greater treatment dropout among individuals with greater PTSD severity and alcohol use (Zandberg et al., 2016). If increasing distress tolerance promotes PTSD symptom reduction as the current study suggests, this may provide a catalyst to trauma-focused treatment for these individuals, and promote greater treatment retention. Although comorbid substance use disorders were present in a minority of the present sample, other distress tolerance interventions have been shown to increase distress tolerance among larger SUD samples (Bornovalova, et al., 2012). Future studies may therefore seek to test the efficacy of combined distress tolerance and trauma-focused protocols among this unique sample.
4.2. Limitations and future directions
Though the present data are an encouraging step toward disentangling the role of distress tolerance in PTSD symptom trajectories, several limitations must be acknowledged. Our clinical sample presented as demographically diverse and relatively severe in terms of diagnostic comorbidity, however, it was limited in size and the reported results should be replicated among larger samples. Sample size presented a barrier to observing significant differences between intervention conditions with regard to pre- to post-intervention change in distress tolerance; post hoc analyses revealed that power to detect such an effect was low (power =0.30), and we believe that, given an adequate sample size, condition differences in distress tolerance change would be significant. There was a non-trivial amount of missing data at the three- and six-month follow-up periods; however, full information multiple imputation is a powerful tool for handling missing data that provides confidence in these results among a full sample, rather than a complete case analysis (Liu and De, 2015).
PTSD symptoms were measured with the PCL-C (Weathers et al., 1991), which does not reflect current PTSD criteria; however, PCL-C and PCL-5 (Weathers et al., 2013a) items are strongly correlated (median r = 0.80; Blevins et al., 2015), and thus comparable results would be expected. Although the SCID-5 is a gold standard diagnostic tool, it is not as detailed or flexible as other PTSD diagnostic interviews, such as the Clinical Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013b). These results should be replicated with the CAPS-5. Finally, the intervention utilized in the present study consisted of only three, hour-long computerized modules. While their scalability is a positive, the results achieved in the present study may be different, perhaps stronger, with other distress tolerance intervention protocols (e.g., Bornovalova et al., 2012). Future studies should continue to investigate the effect of validated distress tolerance interventions on PTSD symptom change. Investigators may wish to test distress tolerance interventions in conjunction with PTSD treatments among specific samples, such as individuals with comorbid PTSD and substance use disorders, given that they exhibit increased treatment attrition and greater disability than individuals without comorbid substance disorders (Bowe and Rosenheck, 2015; Brady et al., 2001; Norman et al., 2007; Schäfer and Najavits, 2007).
4.3. Conclusions
Despite these limitations, this study advances our understanding of the longitudinal relationship between distress tolerance and PTSD symptoms. It is the first study, to our knowledge, to demonstrate that changes in distress tolerance mediate changes in PTSD symptoms. These findings suggest that distress tolerance interventions may in part contribute to reduced PTSD symptom severity, and encourage further study of the potential benefits of supplementing PTSD treatments with brief distress tolerance interventions among targeted samples.
Highlights.
Low distress tolerance (DT) predicts posttraumatic stress disorder (PTSD) symptoms
Two interventions hypothesized to change DT were compared to a control
Post-intervention changes in DT predicted PTSD symptoms at three months
Changes in DT mediated condition effects on PTSD symptoms at three months
DT appears to be a maintenance factor for PTSD symptoms
Acknowledgments
Funding information
This work was supported by the National Institute of Mental Health (Grant no. T32 MH93311) and by the Military Suicide Research Consortium, an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs (Grant nos. W81XWH-10-2-0181, W81XWH-16-2-0003). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Government, Department of Defense, or Military Suicide Research Consortium. The authors have no other conflicts of interest to declare. Funding sources had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. All authors report no financial relationships with commercial interests.
Footnotes
Disclosure
The authors declare no conflict of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allan NP, Short NA, Albanese BJ, Keough ME, Schmidt NB, 2015. Direct and mediating effects of an anxiety sensitivity intervention on posttraumatic stress disorder symptoms in trauma-exposed individuals. Cogn. Behav. Ther 44(6), 512–524. doi: 10.1080/16506073.2015.1075227 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2000. Diagnostic and statistical manual of mental disorders (4 ed.). Author, Washington, DC. [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders (5 ed.). Author, Washington, DC. [Google Scholar]
- Banducci AN, Bujarski SJ, Bonn-Miller MO, Patel A, Connolly KM, 2016. The impact of intolerance of emotional distress and uncertainty on veterans with co-occurring PTSD and substance use disorders. J. Anxiety Disord 41, 73–81. doi: 10.1016/j.janxdis.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Banducci AN, Connolly KM, Vujanovic AA, Alvarez J, Bonn-Miller MO, 2017. The impact of changes in distress tolerance on PTSD symptom severity post-treatment among veterans in residential trauma treatment. J. Anxiety Disord 47, 99–105. doi: 10.1016/j.janxdis.2017.01.004 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK (1996). Beck depression inventory-II. San Antonio, TX, 78204–72498. [Google Scholar]
- Bernstein A, Zvolensky MJ, Vujanovic AA, Moos R, 2009. Integrating anxiety sensitivity, distress tolerance, and discomfort intolerance: A hierarchical model of affect sensitivity and tolerance. Behav. Ther 40(3), 291–301. doi: 10.1016/j.beth.2008.08.001 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA,1996. Psychometric properties of the PTSD Checklist (PCL). Behav. Res. Ther 34(8), 669–673. [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL, 2015. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 28(6), 489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bluett EJ, Zoellner LA, Feeny NC, 2014. Does change in distress matter? Mechanisms of change in prolonged exposure for PTSD. J. Behav. Ther. Exp. Psy 45(1), 97–104. doi: 10.1016/j.jbtep.2013.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodner TE, 2008. What improves with increased missing data imputations? Struct. Equ. Modeling 15(4), 651–675. [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, Lejuez CW, 2012. Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug Alcohol Depen. 122(1–2), 70–76. doi: 10.1016/j.drugalcdep.2011.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowe A, Rosenheck R, 2015. PTSD and Substance Use Disorder among veterans: characteristics, service utilization and pharmacotherapy. J Dual Diagn. 11(1), 22–32. doi: 10.1080/15504263.2014.989653 [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D, 2005. A multidimensional meta-analysis of psychotherapy for PTSD. Am. J. Psychiat 162(2), 214–227. doi: 10.1176/appi.ajp.162.2.214 [DOI] [PubMed] [Google Scholar]
- Brady KT, Dansky BS, Back SE, Foa EB, Carroll KM, 2001. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: Preliminary findings. J. Subst. Abuse Treat 21(1), 47–54. doi: 10.1016/S0740-5472(01)00182-9 [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Darnell A, Charney DS, 1996. Chronic PTSD in Vietnam combat veterans: Course of illness and substance abuse. Am. J. Psychiat 153(3), 369–375. doi: 10.1176/ajp.153.3.369 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Keough ME, Schmidt NB, 2007. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addict. Behav 32(9), 1957–1963. doi: 10.1016/j.addbeh.2006.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell DG, Felker BL, Liu C-F, Yano EM, Kirchner JE, Chan D, et al. , 2007. Prevalence of Depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. J. Gen. Intern. Med 22(6), 711–718. doi: 10.1007/s11606-006-0101-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capron DW, Schmidt NB, 2016. Development and randomized trial evaluation of a novel computer-delivered anxiety sensitivity intervention. Behav. Res. Ther 81, 47–55. doi: 10.1016/j.brat.2016.04.001 [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N, 1998. Posttraumatic stress disorder and drug disorders: Testing causal pathways. Arch. Gen. Psychiat 55(10), 913–917. doi: 10.1001/archpsyc.55.10.913 [DOI] [PubMed] [Google Scholar]
- Corstorphine E, Mountford V, Tomlinson S, Waller G, Meyer C, 2007. Distress tolerance in the eating disorders. Eat. Behav 8(1), 91–97. doi: 10.1016/j.eatbeh.2006.02.003 [DOI] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A, 2008. Optimizing inhibitory learning during exposure therapy. Behav. Res. Ther 46(1), 5–27. doi: 10.1016/j.brat.2007.10.003 [DOI] [PubMed] [Google Scholar]
- Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, Bradley RG, 2008. Treatment barriers for low income, urban African Americans with undiagnosed posttraumatic stress disorder. J. Trauma. Stress 21(2), 218–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunmore E, Clark DM, Ehlers A, 1999. Cognitive factors involved in the onset and maintenance of posttraumatic stress disorder (PTSD) after physical or sexual assault. Behav. Res. Ther 37(9), 809–829. doi: 10.1016/S0005-7967(98)00181-8 [DOI] [PubMed] [Google Scholar]
- Duranceau S, Fetzner MG, Carleton RN, 2014. Low distress tolerance and hyperarousal Posttraumatic Stress Disorder symptoms: A pathway to alcohol use? Cognitive Ther. Res 38(3), 280–290. doi: 10.1007/s10608-013-9591-7 [DOI] [Google Scholar]
- Endler NS, Rutherford A, Denisoff E, 1999. Beck Depression Inventory: Exploring its dimensionality in a nonclinical population. J. Clin. Psychol 55(10), 1307–1312. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO, 2007. Prolonged exposure therapy for PTSD. New York: Oxford University Press. [Google Scholar]
- Fetzner MG, Peluso DL, Asmundson GJ, 2014. Tolerating distress after trauma: differential associations between distress tolerance and posttraumatic stress symptoms. J. Psychopathol. Behav 36(3), 475–484. doi: 10.1007/s10862-014-9413-6 [DOI] [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL, 2015. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV). American Psychiatric Association, Arlington, VA. [Google Scholar]
- Galatzer-Levy IR, Nickerson A, Litz BT, Marmar CR, 2013. Patterns of lifetime PTSD comorbidity: A latent class analysis. Depress. Anxiety 30(5), 489–496. doi: 10.1002/da.22048 [DOI] [PubMed] [Google Scholar]
- Gravetter FJ, Wallnau LB, Forzano L-AB, 2016. Essentials of statistics for the behavioral sciences: Nelson Education. [Google Scholar]
- Gutner CA, Galovski T, Bovin MJ, Schnurr PP, 2016. Emergence of transdiagnostic treatments for PTSD and posttraumatic distress. Curr. Psychiat. Rep 18(10), 95. doi: 10.1007/s11920-016-0734-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper]. Retrieved from http://www.afhayes.com/public/process2012.pdf
- Hayes AF, Preacher KJ, 2014. Statistical mediation analysis with a multicategorical independent variable. Brit. J. Math. Stat. Psy 67(3), 451–470. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, Wilk JE, 2014. PTSD treatment for soldiers after combat deployment: Low utilization of mental health care and reasons for dropout. Psychiatr. Serv 65(8), 997–1004. [DOI] [PubMed] [Google Scholar]
- Holmes EA, Mathews A, Dalgleish T, Mackintosh B, 2006. Positive interpretation training: effects of mental imagery versus verbal training on positive mood. Behav. Ther 37(3), 237–247. doi: 10.1016/j.beth.2006.02.002 [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR, 2001. Substance use disorders in patients with Posttraumatic stress disorder: A review of the literature. Am. J. Psychiat 158(8), 1184–1190. doi: 10.1176/appi.ajp.158.8.1184 [DOI] [PubMed] [Google Scholar]
- Joiner T (2005). Why people die by suicide. Cambridge, MA, US: Harvard University Press. [Google Scholar]
- Jongh A, Resick PA, Zoellner LA, Minnen A, Lee CW, Monson CM, et al. , 2016. Critical analysis of the current treatment guidelines for complex PTSD in adults. Depress. Anxiety 33(5), 359–369. [DOI] [PubMed] [Google Scholar]
- Kessler RC (2000). Posttraumatic stress disorder: the burden to the individual and to society. J. Clin. Psychiat 61, 4–12. [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, 1995. Posttraumatic stress disorder in the national comorbidity survey. Arch. Gen. Psychiat 52(12), 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kisbu-Sakarya Y, MacKinnon DP, Aiken LS, 2013. A Monte Carlo comparison study of the power of the analysis of covariance, simple difference, and residual change scores in testing two-wave data. Educ. Psychol. Meas 73(1), 47–62. doi: 10.1177/0013164412450574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A, 2010. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychol. Bull 136(4), 576–600. doi: 10.1037/a0019712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, De A, 2015. Multiple imputation by fully conditional specification for dealing with missing data in a large epidemiologic study. Stat. Methods Med. Res 4(3), 287–295. doi: 10.6000/1929-6029.2015.04.03.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Zvolensky MJ, 2011. Main and interactive effects of a nonclinical panic attack history and distress tolerance in relation to PTSD symptom severity. J. Anxiety Disord 25(2), 185–191. doi: 10.1016/j.janxdis.2010.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mott JM, Hundt NE, Sansgiry S, Mignogna J, Cully JA, 2014. Changes in psychotherapy utilization among veterans with depression, anxiety, and PTSD. Psychiatr. Serv 65(1), 106–112. [DOI] [PubMed] [Google Scholar]
- Norman SB, Tate SR, Anderson KG, Brown SA, 2007. Do trauma history and PTSD symptoms influence addiction relapse context? Drug Alcohol Depen. 90(1), 89–96. doi: 10.1016/j.drugalcdep.2007.03.002 [DOI] [PubMed] [Google Scholar]
- Norr AM, Allan NP, Macatee RJ, Keough ME, Schmidt NB, 2014. The effects of an anxiety sensitivity intervention on anxiety, depression, and worry: Mediation through affect tolerances. Behav. Res. Ther 59, 12–19. doi: 10.1016/j.brat.2014.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter CM, Vujanovic AA, Marshall-Berenz EC, Bernstein A, Bonn-Miller MO, 2011. Posttraumatic stress and marijuana use coping motives: The mediating role of distress tolerance. J. Anxiety Disord. 25(3), 437–443. doi: 10.1016/j.janxdis.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S, McNally RJ, 1985. Expectancy model of fear In Reiss S, Bootzin R (Eds.), Theoretical issues in behavior therapy (pp. 107–121). San Diego, CA: Academic Press. [Google Scholar]
- Resick PA, Monson CM, Chard KM, 2007. Cognitive processing therapy: Veteran/military version. Washington, DC: Department of Veterans’ Affairs. [Google Scholar]
- Schäfer I, Najavits LM, 2007. Clinical challenges in the treatment of patients with posttraumatic stress disorder and substance abuse. Curr. Opin. Psychiatr 20(6), 614–618. doi: 10.1097/YCO.0b013e3282f0ffd9 [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, Allan NP, 2014. Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. J. Consult. Clin. Psych 82(6), 1023–1033. doi: 10.1037/a0036651 [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Norr AM, Allan NP, Raines AM, Capron DW, 2017. A randomized clinical trial targeting anxiety sensitivity for patients with suicidal ideation. J. Consult. Clin. Psych doi: 10.1037/ccp0000195 [DOI] [PubMed] [Google Scholar]
- Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH, 2008. Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry. 71(2), 134–168. doi: 10.1521/psyc.2008.71.2.134 [DOI] [PubMed] [Google Scholar]
- Short NA, Boffa JW, Norr AM, Albanese BJ, Allan NP, Schmidt NB, 2017. Randomized clinical trial investigating the effects of an anxiety sensitivity intervention on posttraumatic stress symptoms: A replication and extension. J. Trauma. Stress 30(3), 296–303. doi: 10.1002/jts.22194 [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, 2005. The distress tolerance scale: Development and validation of a self-report measure. Motiv. Emotion 29(2), 83–102. doi: 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Stice E, 2002. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol. Bull 128(5), 825. doi: 10.1037/0033-2909.128.5.825 [DOI] [PubMed] [Google Scholar]
- Sullivan TR, White IR, Salter AB, Ryan P, Lee KJ, 2016. Should multiple imputation be the method of choice for handling missing data in randomized trials? Stat. Methods Med. Res doi: 10.1177/0962280216683570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR et al. , 2010. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 105(6), 1117–1128. doi: 10.1111/j.1360-0443.2010.02902.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. , 2007. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol. Assessment 19(2), 176. [DOI] [PubMed] [Google Scholar]
- Vinci C, Mota N, Berenz E, Connolly K, 2016. Examination of the relationship between PTSD and distress tolerance in a sample of male veterans with comorbid substance use disorders. Mil. Psychol 28(2), 104–114. doi: 10.1037/mil0000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Potter CM, Marshall EC, Zvolensky MJ, 2011a. An evaluation of the relation between distress tolerance and posttraumatic stress within a trauma-exposed sample. J. Psychopathol. Behav 33(1), 129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Dutcher CD, Berenz EC, 2017. Multimodal examination of distress tolerance and posttraumatic stress disorder symptoms in acute-care psychiatric inpatients. J. Anxiety Disord 48 45–53. doi: 10.1016/j.janxdis.2016.08.005 [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Hart AS, Potter CM, Berenz EC, Niles B, Bernstein A, 2013. Main and Interactive Effects of Distress Tolerance and Negative Affect Intensity in Relation to PTSD Symptoms among Trauma-Exposed Adults. J. Psychopathol. Behav 35(2), 235–243. doi: 10.1007/s10862-012-9325-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Marshall-Berenz EC, Zvolensky MJ, 2011b. Posttraumatic stress and alcohol use motives: A test of the incremental and mediating role of distress tolerance. J. Cog. Psychother 25(2), 130–141. doi: 10.1891/0889-8391.25.2.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Rathnayaka N, Amador CD, Schmitz JM, 2016. Distress tolerance: associations with posttraumatic stress disorder symptoms among trauma-exposed, cocaine-dependent adults. Behav. Modif 40(1–2), 120–143. doi: 10.1177/0145445515621490 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM 2013a. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). Interview available from the National Center for PTSD at www.ptsd.va.gov.
- Weathers FJ, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP, 2013b. The PTSD Checklist for DSM-5 (PCL-5). Boston, MA: National Center for PTSD. [Google Scholar]
- Weathers FW, Huska JA, Keane TM, 1991. PCL-C for DSM-IV. Boston: National Center for PTSD-Behavioral Science Division. [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C, 2001. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am. J. Psychiat 158(12), 2027–2032. [DOI] [PubMed] [Google Scholar]
- Zandberg LJ, Rosenfield D, Alpert E, McLean CP, Foa EB, 2016. Predictors of dropout in concurrent treatment of posttraumatic stress disorder and alcohol dependence: Rate of improvement matters. Behav. Res. Ther 80, 1–9. doi: 10.1016/j.brat.2016.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]