Abstract
Background and Objectives:
Socket preservation is the procedure which is carried out at the time of extraction to enhance the esthetic predictability of prosthesis and to reduce the number of surgical interventions by minimizing the crestal bone loss. The aim of the present study was to compare the efficacy of natural bovine hydroxyapatite and platelet-rich fibrin (PRF) matrix along with collagen plug to unassisted natural healing in extraction sites.
Materials and Methods:
A sample of 25 patients of age 17–50 years who require extraction of at least two teeth which were not adjacent to each other were included in the study. One site in each patient was subjected to ridge preservation procedure using Cerabone™ PRF along with collagen plug and the other site was subjected to atraumatic extraction alone. Parameters such as loss of ridge width and loss of ridge height were measured clinically and radiographically at baseline and after 6 months.
Results:
The mean loss of width was found to be 2.75 mm (2.75 ± 1.49) at the control site compared to 1.47 mm (1.47 ± 1.44) at the test site. The test site showed 2.31 mm bone fill, (8.7%) compared to the control site.
Conclusion:
Within the limitations of the study, the results suggest that socket preservation procedure is a reliable method that minimizes the alveolar bone loss.
Keywords: Collagen plug, extraction, platelet-rich fibrin, socket preservation, xenograft
INTRODUCTION
Improved perception of esthetics has increased the patient's expectation and demand toward the rehabilitation of edentulous areas with restorations of high quality in appearance and function. Although the reasons for extraction of teeth such as severe decay, periodontal disease, tooth fracture, or failed endodontic treatment are varied, they eventually result in marked morphological and dimensional changes of the alveolar ridge.[1] These changes can be collectively referred to as alveolar ridge resorption which is a chronic, irreversible phenomenon, the result of which is an inadequate bone volume of the ridge.[2]
Following extraction of a tooth, a series of events occur which cause significant alterations in the height and width of the alveolar ridge. These events start immediately after extraction of the tooth and continue to a period of 5–10 weeks. Although the socket is gradually replaced with bone, it is well known that the alveolar crest reduces in volume after tooth extraction, especially during the first 6 months and mostly on its buccal wall.[3]
The most rapid changes are found in the early postextraction period, from 6 months to 2 years. Two-third of this reduction occurs within the first 3 months.[2] The rate of residual ridge resorption was shown to be four times greater in the mandible than in the maxilla.[3] This resorption can partly be attributed to the traumatic damage to the dentoalveolar housing during extraction, especially with the usage of forceps. The subsequent ridge deformity poses a challenge for prosthetic rehabilitation due to the significant functional and esthetic problems.[4]
These complications can be avoided by conservative atraumatic extraction and socket preservation technique with different materials. An atraumatic extraction is the process of extracting a hopeless tooth in the most delicate and conservative technique; this includes using special instruments that severe the tooth's attachment to its socket. Preserving the residual socket with bone replacement material and using a membrane to cover and protect the material within the socket have been gaining wide attention among the dental professionals. This procedure mainly helps to preserve the residual supporting bone, thus providing a higher success rate for implants and fixed prosthesis.[5,6]
Current methods for socket preservation include the use of particulate autografts, allografts, alloplasts, xenografts, and resorbable or nonresorbable membranes manufactured from various materials.[7,8] However, the gold standard as to the ideal grafting material or the technique has not yet been established. Among the various materials available, xenografts have advantages such a slow resorbing rate, superior handling characteristics, promotion of revascularization and clot stabilization, and also optimal integration with patient's own bone.[9]
An important requirement for the optimum and fast healing of any wound is the availability of abundant growth factors. In the recent times, platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) have been used to provide such growth factors and enhance the healing process. Compared to PRP, the technique of extracting PRF from the patient's own blood is fairly simple, safe, and economical. Hence, the use of PRF in combination with bone grafts in various regenerative procedures such as the treatment of intrabony defects, root-coverage procedures, and sinus-lift procedures has been well documented in the literature.[10,11,12]
However, limited data are available about the use of PRF in combination with xenografts in socket preservation procedures. Hence, the aim of the present study is to evaluate the effectiveness of naturally derived bovine hydroxyapatite, (Cerabone ™) combined with PRF matrix in socket preservation in patients undergoing extractions.
MATERIALS AND METHODS
This is a randomized controlled clinical study conducted to compare the efficacy of natural bovine bone graft material and PRF matrix along with the collagen plug to unassisted natural healing in patients requiring extraction of two teeth. To evaluate the feasibility, recruitment of participants, and data analysis, a pilot study was done for the proposal. Based on the results of the pilot study, sample size was calculated for the trial.
Patient selection
A total of 25 patients ranging in age from 17 to 50 years who require extraction of at least two teeth, which are not adjacent to each other, were selected from patients attending the department of periodontics and implantology and the department of oral surgery. The study was conducted in accordance with the World Medical Association Declaration of Helsinki and approved by the Institutional Ethical Committee.
Inclusion criteria
Patients requiring extraction of two teeth, which were indicated due to either severe decay, periodontal disease, tooth fractures, or failed endodontic treatment, were included in the study.
Exclusion criteria
Smokers, patients having uncontrolled systemic diseases, pregnant patients, patients receiving therapeutic radiation in the head and neck, who require extraction of most of their teeth, who show unwillingness to return for the follow-up examination, who opt for immediate implant placement were excluded from the study.
Study design
After the sample size calculation, a total of 25 patients fulfilling the above-mentioned criteria were selected for the study. The patients were informed about the intended purpose of the study and informed written consent was obtained from them and if any under 18 years, written consent was obtained from their parent or guardian.
A detailed case history was recorded in the specially prepared pro forma, which includes baseline clinical parameters as mentioned below:
Soft-tissue assessment:
Mesial and distal papilla appearance (Nordland and Tarnow, 1998)
Soft-tissue color, consistency, and contour
Biotype of gingival tissue (Juodzbalys, 2008).[13]
Initial periodontal therapy consisted of patient education and motivation, full-mouth scaling followed by root planning if necessary and oral hygiene instructions.
Preoperative procedure
Alginate impressions of the upper and lower arches were made on the 1st day. Preoperative casts were poured and an occlusal stent was prepared, including one tooth anterior and posterior to the hopeless tooth. Over the cast, the extraction site was trimmed to reproduce the alveolar crest. The vertical and horizontal measurements were done preoperatively on the casts.
The vertical ridge height was measured from the stent to the alveolar crest through the holes created in the mid-buccal, mid-lingual, mesial, and distal sites. The horizontal ridge width was measured between the most prominent sites buccally and lingually using a Digital Vernier Caliper.
Radiographic examination
Standardized intraoral periapical radiographs using long-cone paralleling technique at baseline and 6 months were taken. The following parameters were recorded:
Cementoenamel junction (CEJ) of the teeth adjacent to the extraction site
Crestal bone level – the distance from distal CEJ of the adjacent tooth to the radiographic crest of bone
Depth of the socket – the distance between the CEJ of the adjacent teeth till the base of the socket
Bone fill = Depth of the socket–distance from the CEJ to bone crest.
Bone fill percentage was calculated using 1 mm2 counting grid.
The radiographic measurements were made with the help of standardized AUTOCAD software (Autodesk Inc., San Rafael, CA, USA) at baseline and 6-month reevaluation.
Surgical procedure
The test and control sites were randomized using the coin-flip method [Figure 1]. All the extraction procedures were performed under the standard surgical protocol. The procedure was performed under local anesthesia of 2% lignocaine containing adrenaline at a concentration of 1: 2,00,000. Before the extraction procedure in the test site, according to Choukroun et al.,[14] 10 ml of blood was drawn from the patient's antecubital vein. The blood sample was immediately placed in a dry glass tube and centrifuged at 3000 RPM for 10 min. After centrifugation, the PRF which was collected in the middle of the tube was removed using sterile tweezers and was placed in a sterile Dappen dish.
Figure 1.

Extraction indicated site in relation to 44
A flapless atraumatic extraction was carried out using Periotomes. Initially, the periotome was applied between the bone and tooth to severe the subcrestal attachment apparatus. Once the tooth was luxated within the socket, the tooth was removed from the socket using extraction forceps. The socket was thoroughly debrided of the soft-tissue debris using a curette. Furthermore, the bony walls of the socket were scraped to stimulate bleeding.
Then, PRF was minced into small pieces using sterile scissors and mixed with bone graft (Cerabone ™) in a 1:1 ratio [Figure 2]. Except the coronal aspect of 1 mm, the entire socket was filled with the mixture. This 1 mm allowed the space for collagen plug (collaplug ™), which was placed over the bone graft + PRF mixture. The socket was then secured by cross-mattress suture using nonresorbable 3-0 silk suture [Figure 3].
Figure 2.
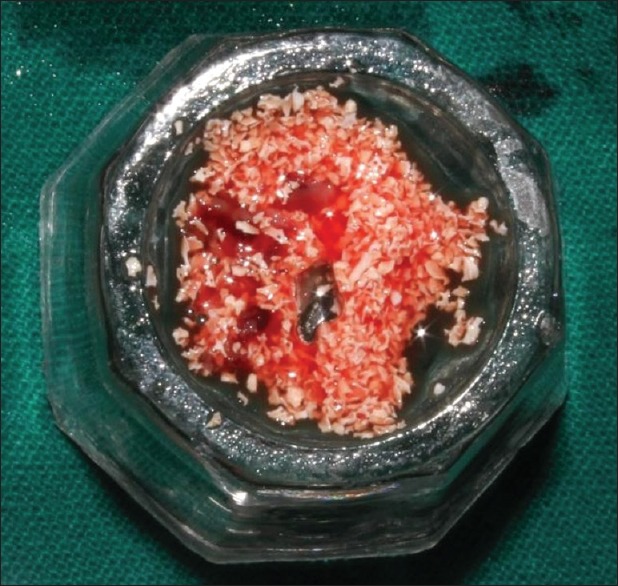
Platelet-rich fibrin mixed with bone graft
Figure 3.
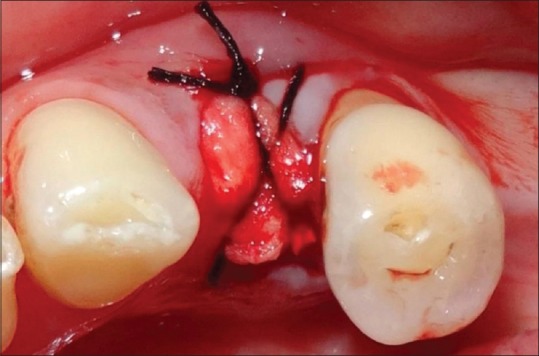
After placement of bone graft and collagen plug suturing done
The control site received the extraction procedure alone, followed by cross-mattress suturing. All the clinical parameters were measured at the time of extraction and after 6 months of extraction [Figure 4].
Figure 4.

Six months evaluation of 44
Postoperative treatment
Patients were instructed not to brush over the surgical area. Antibiotics (amoxicillin 500 mg three times a day for 5 days) and analgesics (ibuprofen 400 mg every 4 h as needed for pain) were prescribed. Patients were advised to use 0.2% chlorhexidine mouth rinse for every 12 h for 2 weeks. Patients were also advised to take soft diet for 2 weeks. Patients were recalled after 2 weeks during which sutures were removed and the operated area was evaluated for healing. No untoward events were reported by any patient [Figures 5 and 6].
Figure 5.

(a) Pre operative radiograph. (b) Post operative radiograph
Figure 6.
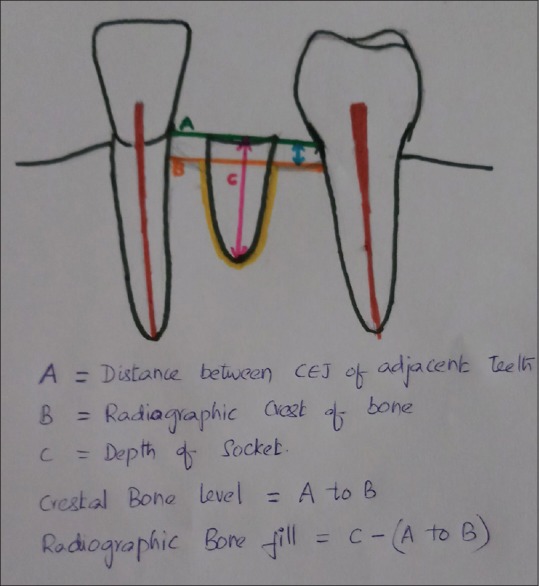
Line diagram for Radiographic measurements
Patients were recalled every month for reevaluation and oral hygiene reinforcement and final evaluation was done at 6 months.
Statistical analysis
Paired samples t-test, independent samples t-test, and Mann–Whitney U test were used. The statistical software, namely, Statistical Package for the Social Sciences SPSS 20.0 (IBM, NY, USA) was used for analysis of the data.
RESULTS
All surgical procedures were successfully carried out without any complications. Twenty-three patients returned for the recall visits and were included for the final analysis. Two patients were excluded from the study as they did not return after extraction.
Demographic variables
Age
The age of the participants ranged from 17 to 50 years with a mean age range of 35.08 ± 13.34 years [Table 1].
Table 1.
Mean age of the participants
| Sex | Number of patients (%) | Mean age |
|---|---|---|
| Male | 9 (39.13) | 38.44 |
| Female | 14 (60.87) | 32.93 |
| Total | 23 (100.00) | 35.09 |
Gender
Nine female participants and 14 male participants participated in the study.
Soft-tissue parameters
The following soft-tissue dimensions were recorded at the baseline to evaluate the type of extraction socket.
Mesial and distal papilla appearance
About 60.8% of the test sites showed Type II papilla, while 30.4% showed Type I papilla and 8.6% showed Type III papilla. In the control sites, 69.5% showed Type II papilla, while 21.7% showed Type I papilla and 17.3% showed Type III papilla.
Soft-tissue color, contour, and consistency
All the sites in the test and control groups exhibited pale pink, scalloped, and firm tissues.
Biotype of gingival tissues
In the test group, 43.4% sites were of thin biotype (<1.0), 47.8% with thick biotype (1–2), and 8.6% were with moderate biotype (>2). In the control group, 26.7% sites were of thin biotype, 56.5% with thick biotype, and 21.7% were with moderate biotype. Thus, the extraction sockets in the present study exhibited similar gingival findings but different gingival biotypes.
Clinical parameters
Width of the alveolar ridge
The results showed that from baseline to 6 months, the mean loss of width at the control site was 2.75 mm, while the mean loss of width at the test site was 1.47 mm. Thus, the mean loss of width at control site was 1.28 mm greater than at the test site [Table 2]. The difference between the test and control sites was statistically significant (P < 0.05).
Table 2.
Comparison of the width of the alveolar ridge at baseline and after 6 months
| Sites | Time | Mean | Mean difference | P |
|---|---|---|---|---|
| Test site | Baseline | 8.27±1.96 | 1.47 | 0.0006* |
| 6 months | 6.80±1.61 | |||
| Control site | Baseline | 8.86±1.82 | 2.75 | 0.0001* |
| 6 months | 6.11±1.27 |
P≤0.05 – Statistically significant. P – Significant
Height of the alveolar ridge
Buccal height
The results showed that from baseline to 6 months, the mean reduction in buccal height was 0.96 mm at the test site. While at the control site, the reduction in height was 2.26 mm. Thus, the loss in buccal height at the control site was 1.3 mm greater than at the test site [Table 3]. This difference between the test and control sites was statistically significant.
Table 3.
Comparison of buccal height of the alveolar ridge at baseline and after 6 months
| Sites | Time | Mean | Mean difference | P |
|---|---|---|---|---|
| Test site | Baseline | 9.26±1.25 | −0.96 | 0.0023* |
| 6 months | 10.22±1.47 | |||
| Control site | Baseline | 8.17±1.94 | −2.26 | 0.0001* |
| 6 months | 10.43±1.92 |
P≤0.05 – Statistically significant. P – Significant
Lingual height
From baseline to 6 months, it was found that the mean loss of lingual height was 2.17 mm at the control site, while it was 1.04 mm at the test site. Thus, the mean lingual bone loss was 1.13 mm greater at control site compared to the test site [Table 4]. These results were found to be statistically significant.
Table 4.
Comparison of lingual height of the alveolar ridge at baseline and after 6 months
| Sites | Time | Mean | Mean difference | P |
|---|---|---|---|---|
| Test site | Baseline | 8.44±1.27 | −1.04 | 0.0057* |
| 6 months | 9.48±1.41 | |||
| Control site | Baseline | 8.58±1.53 | −2.17 | 0.0001* |
| 6 months | 10.74±1.48 |
P≤0.05 – Statistically significant. P – Significant
Mesial height
From baseline to 6 months, it was found that the mean loss of height was 1.3 mm at the control site, while at the test site, the height decreased by 0.69 mm [Table 5]. Thus, there was 0.62 mm greater bone loss in control group compared to test group. These results were not found to be statistically significant.
Table 5.
Comparison of mesial height of the alveolar ridge at baseline and after 6 months
| Sites | Time | Mean | Mean difference | P |
|---|---|---|---|---|
| Test site | Baseline | 7.48±1.34 | −0.69 | 0.7172 |
| 6 months | 8.17±1.61 | |||
| Control site | Baseline | 7.39±1.50 | −1.30 | 0.1474 |
| 6 months | 8.70±1.39 |
P≤0.05 – Statistically significant. P – Not significant
Distal height
The results showed that from baseline to 6 months, there was loss of 0.86 mm at test site. While at the control site, the bone loss was 1.24 mm [Table 6]. Thus, the mean bone loss in the height at control site was 0.38 mm greater than at the test site. These results were not statistically significant.
Table 6.
Comparison of distal height of the alveolar ridge at baseline and after 6 months
| Sites | Time | Mean | Mean difference | P |
|---|---|---|---|---|
| Test site | Baseline | 7.72±1.81 | −0.86 | 0.8446 |
| 6 months | 8.57±1.5 | |||
| Control site | Baseline | 7.89±1.94 | −1.24 | 0.2971 |
| 6 months | 9.13±2.00 |
P≤0.05 –Statistically significant. P – Not significant
Radiographic measurements
AUTOCAD software (Autodesk Inc., San Rafael, CA, USA) was used for the radiographic measurements [Table 7].
Table 7.
Comparison of radiographic measurements between test and control groups
| Measurements | Test | Control | Mean difference | P |
|---|---|---|---|---|
| Crestal bone level | 0.09±0.51 | 0.60±0.68 | 0.51 | 0.027 |
| Socket depth | 10.61±2.89 | 8.95±2.55 | 1.65 | 0.046 |
| Bone fill | 8.67±2.96 | 6.36±2.52 | 2.30 | 0.007* |
| Bone fill percentage | 97.29±2.67 | 88.5±10.69 | 8.76 | 0.000* |
P≤0.05 – Statistically significant. P – Significant
Crestal bone level
From baseline to 6 months, the test site showed a mean loss of 0.1 mm, while the control site showed mean loss of 0.6 mm. Thus, there is an increase of 0.5 mm crestal bone loss at the control site than at the test site. These results were not statistically significant.
Bone fill
The results showed a 2.31 mm more bone fill at the test site than at the control site. The results were statistically significant.
Bone fill percentage
The bone fill percentage was found to be 8.7% more at the test site than at the control site. These results were found to be statistically significant.
DISCUSSION
As the patient's perception toward esthetics had enhanced from the past few years, the value as well as the number of implants and fixed prostheses had also increased. Certainly, patient treatment acceptance toward these restorations can be affected by some esthetic shortcomings. These can be ascribed to the ridge deformities that occur as a sequel of tooth extraction. The resorption of the alveolar ridge is a chronic and irreversible phenomenon that may result in an inadequate bone volume.[15] Sometimes, ridge augmentation procedures may be required to achieve a precise prosthetic rehabilitation. Thus, to reduce the number of surgical interventions and to enhance the chances of achieving the esthetics with greater predictability, it would be better to preserve the socket at the time of extraction.
Although none of the materials have been proved as the gold standard, xenografts due to their superior characteristics were extensively studied in this arena. In addition, growth factors when used along with the bone substitutes have been found to enhance the healing process. While the use of autologous blood concentrates in the treatment of intrabony defects has been extensively studied, very limited data are available about its use in socket preservation.[16]
In the present study, a healing period of 6 months was selected because after extraction alveolar ridge undergoes rapid resorption in the first 3–6 months, followed by gradual reduction in the dimensions. This time point was used in two previously reported systematic reviews.[17,18] The systematic review by Lang et al.[19] demonstrated mean horizontal reduction in ridge width 3.8 mm and mean vertical reduction in ridge height 1.24 mm in the first 6 months.
It is generally admitted that flap elevation interrupts the periosteal vascular supply and has an impact on bone remodeling.20. Previous studies reported that flapless techniques could preserve hard tissue dimensions and increased keratinized tissue than flapped techniques. Hence, a flapless extraction procedure for both test and control sites was selected in this study. However, the effect of flap elevation on alveolar bone loss is still a controversy. Even though a marginal bone resorption of 1 mm was attributed to flap elevation, recent evidence from preclinical studies indicates that flap elevation does not promote alveolar bone loss.[18]
Among all the bone grafts, naturally derived bovine hydroxyapatite (Cerabone ™) was chosen because it was extensively studied and also known to exhibit certain superior characteristics. These include superior handling characteristics, promotion of revascularization and clot stabilization, scaffold action for the formation of new bone, better osseointegration with the patient's own bone, and slow resorbing rate.[9,21] Since an ideal bone graft material has not been found yet, the incorporation of various growth factors (platelet-derived growth factor and transforming growth factor-beta) and proteins (BMP) has been advocated to speed up the osteogenic process.[10,22] This had led to the application of PRF in various regenerative procedures. Their use along with bone grafts was supposed to enhance bone density and maturation. A radiographic maturation rate of bone grafts with platelet growth factors was observed to be 1.62–2.16 times more rapid than grafts without platelet growth factors.[23] In the present study, PRF from the patient's own blood was prepared and used along with the Cerabone ™ for preserving the extraction sockets. This study was done in accordance with the Sklar's “Bio-col technique,” wherein after filling two-third of the socket with bovine hydroxyapatite, the remaining socket was filled with a bioabsorbable collagen plug.
In the present study, the soft-tissue parameters such as mesial and distal papilla appearance, color, contour, consistency, and tissue biotypes were recorded at baseline. The results showed that the extraction sockets in the present study exhibited similar gingival findings, but different soft-tissue quantities, qualities, and gingival biotypes. Obviously, some of these characteristics may influence the final outcome of any socket preservation procedure.[13]
In this study, a reduction in the buccolingual width from baseline to 6 months was observed in both test and control sites. This showed that some loss of buccolingual width was inevitable after extraction. In other terms, complete preservation of preextraction alveolar ridge dimensions cannot be anticipated even with alveolar ridge preservation techniques. However, the control site showed greater mean loss of width 2.75 mm compared to test site 1.47 mm. The control site at baseline demonstrated greater buccolingual width. While at 6 months, the buccolingual width of the test site was greater. This indicates that PRF in combination with xenograft and collagen plug reduced the resorption activity at the test site.
In the present study, the vertical height was measured at four sites, that is, mid-buccal, mid-lingual, mesial, and distal as the distance between the stent and alveolar crest. Statistically significant differences were observed between the test and control groups in the mid-buccal and mid-lingual measurements. Whereas, mesial and distal measurement differences were not statistically significant. These results were in accordance with the previous studies.[24,25]
As a whole, in the present study, when all the measurements were compared, the bone loss was more pronounced at the buccal sites compared to the mesial and distal sites. This can be explained by the bundle bone concept, that is, the buccal plate comprised bundle bone alone.[2] Hence, the extraction of tooth compromised the blood supply to the bundle bone causing more resorption of the buccal plate. The relatively less resorption at the mesial and distal sites can be explained by the trend that the mesial and distal heights can be dependent on the presence of adjacent teeth, that is, the presence of adjacent teeth maintained stable bone levels at the mesial and distal sites.
In the present study, the results showed a 2.31 mm more bone fill at the test site than at the control site. In a similar study, 0.98 mm more bone fill was observed at the test site compared to the control site.[24] This difference between the studies can be partly related to the use of PRF in the present study which has shown to enhance the healing process and osteoblastic activity of bone graft.
Overall, the strengths of the study are the use of PRF in combination with a xenograft, the design of the study which was split-mouth design. This design removed the interindividual variability from the estimates of the treatment effect. Atraumatic extraction using Periotomes also added an advantage of preserving the buccal plate.
The limitations of the study are the thickness of the buccal bony plate that was not estimated; the number of walls of the socket was not measured during the extraction procedure, dimensional disparity in the residual socket size of the study teeth and advanced radiographic techniques are not considered. Histologic examination could have provided the type of bone formed in preserved sockets which was not planned in the study. Further studies with advanced radiographic techniques are recommended to evaluate the effectiveness of PRF in socket preservation procedure
CONCLUSION
Since the major changes in the dimensions of the ridge occur within the first 2 months, it is better to preserve the ridge at the time of extraction itself. Besides the routine usage of bone graft in socket preservation, the addition of PRF provided additional growth factors which enhanced the wound healing process and maintained the dimensions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pagni G, Pellegrini G, Giannobile WV, Rasperini G. Postextraction alveolar ridge preservation: Biological basis and treatments. Int J Dent. 2012;2012:151030. doi: 10.1155/2012/151030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang HL, Kiyonobu K, Neiva RF. Socket augmentation: Rationale and technique. Implant Dent. 2004;13:286–96. doi: 10.1097/01.id.0000148559.57890.86. [DOI] [PubMed] [Google Scholar]
- 3.Caplanis N, Lozada JL, Kan YK. Extraction defect: Assessment, classification and management. Int J Clin Implant Dent. 2009;1:1–11. [PubMed] [Google Scholar]
- 4.Chappuis V, Engel O, Reyes M, Shahim K, Nolte LP, Buser D, et al. Ridge alterations post-extraction in the esthetic zone: A 3D analysis with CBCT. J Dent Res. 2013;92:195S–201S. doi: 10.1177/0022034513506713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atwood DA, Coy WA. Clinical, cephalometric, and densitometric study of reduction of residual ridges. J Prosthet Dent. 1971;26:280–95. doi: 10.1016/0022-3913(71)90070-9. [DOI] [PubMed] [Google Scholar]
- 6.Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J Clin Periodontol. 2009;36:1048–58. doi: 10.1111/j.1600-051X.2009.01482.x. [DOI] [PubMed] [Google Scholar]
- 7.Wood RA, Mealey BL. Histologic comparison of healing after tooth extraction with ridge preservation using mineralized versus demineralized freeze-dried bone allograft. J Periodontol. 2012;83:329–36. doi: 10.1902/jop.2011.110270. [DOI] [PubMed] [Google Scholar]
- 8.Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313–23. [PubMed] [Google Scholar]
- 9.Calasans-Maia M, Resende R, Fernandes G, Calasans-Maia J, Alves AT, Granjeiro JM, et al. Arandomized controlled clinical trial to evaluate a new xenograft for alveolar socket preservation. Clin Oral Implants Res. 2014;25:1125–30. doi: 10.1111/clr.12237. [DOI] [PubMed] [Google Scholar]
- 10.Del Fabbro M, Bortolin M, Taschieri S. Is autologous platelet concentrate beneficial for post-extraction socket healing? A systematic review. Int J Oral Maxillofac Surg. 2011;40:891–900. doi: 10.1016/j.ijom.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Thakkar DJ, Deshpande NC, Dave DH, Narayankar SD. A comparative evaluation of extraction socket preservation with demineralized freeze-dried bone allograft alone and along with platelet-rich fibrin: A clinical and radiographic study. Contemp Clin Dent. 2016;7:371–6. doi: 10.4103/0976-237X.188567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suttapreyasri S, Leepong N. Influence of platelet-rich fibrin on alveolar ridge preservation. J Craniofac Surg. 2013;24:1088–94. doi: 10.1097/SCS.0b013e31828b6dc3. [DOI] [PubMed] [Google Scholar]
- 13.Juodzbalys G, Sakavicius D, Wang HL. Classification of extraction sockets based upon soft and hard tissue components. J Periodontol. 2008;79:413–24. doi: 10.1902/jop.2008.070397. [DOI] [PubMed] [Google Scholar]
- 14.Choukroun J, Adda F, Schoeffler C, Vervelle A. An opportunity in perio-implantology: The PRF (in French) Implantodontie. 2001;42:55–62. [Google Scholar]
- 15.Moghaddas H, Stahl SS. Alveolar bone remodeling following osseous surgery. A clinical study. J Periodontol. 1980;51:376–81. doi: 10.1902/jop.1980.51.7.376. [DOI] [PubMed] [Google Scholar]
- 16.Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: A systematic review and meta-analysis. J Dent Res. 2014;93:950–8. doi: 10.1177/0022034514541127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hämmerle CH, Araújo MG, Simion M Osteology Consensus Group 2011. Evidence-based knowledge on the biology and treatment of extraction sockets. Clin Oral Implants Res. 2012;23(Suppl 5):80–2. doi: 10.1111/j.1600-0501.2011.02370.x. [DOI] [PubMed] [Google Scholar]
- 18.Tan WL, Wong TL, Wong MC, Lang NP. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23(Suppl 5):1–21. doi: 10.1111/j.1600-0501.2011.02375.x. [DOI] [PubMed] [Google Scholar]
- 19.Lang NP, Pun L, Lau KY, Li KY, Wong MC. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res. 2012;23(Suppl 5):39–66. doi: 10.1111/j.1600-0501.2011.02372.x. [DOI] [PubMed] [Google Scholar]
- 20.Barone A, Borgia V, Covani U, Ricci M, Piattelli A, Iezzi G, et al. Flap versus flapless procedure for ridge preservation in alveolar extraction sockets: A histological evaluation in a randomized clinical trial. Clin Oral Implants Res. 2015;26:806–13. doi: 10.1111/clr.12358. [DOI] [PubMed] [Google Scholar]
- 21.Festa VM, Addabbo F, Laino L, Femiano F, Rullo R. Porcine-derived xenograft combined with a soft cortical membrane versus extraction alone for implant site development: A clinical study in humans. Clin Implant Dent Relat Res. 2013;15:707–13. doi: 10.1111/j.1708-8208.2011.00398.x. [DOI] [PubMed] [Google Scholar]
- 22.Triveni MG, Tarun Kumar AB, Jain V, Mehta DS. Alveolar ridge preservation with β-TCP graft and platelet-rich fibrin. Int J Oral Implant Clin Res. 2012;3:96–100. [Google Scholar]
- 23.Kassim B, Ivanovski S, Mattheos N. Current perspectives on the role of ridge (socket) preservation procedures in dental implant treatment in the aesthetic zone. Aust Dent J. 2014;59:48–56. doi: 10.1111/adj.12098. [DOI] [PubMed] [Google Scholar]
- 24.Gupta D, Gundannavar G, Chinni DD, Alampalli RV. Ridge preservation done immediately following extraction using bovine bone graft, collagen plug and collagen membrane. Int J Oral Implantol Clin Res. 2012;3:8–16. [Google Scholar]
- 25.Barone A, Aldini NN, Fini M, Giardino R, Calvo Guirado JL, Covani U, et al. Xenograft versus extraction alone for ridge preservation after tooth removal: A clinical and histomorphometric study. J Periodontol. 2008;79:1370–7. doi: 10.1902/jop.2008.070628. [DOI] [PubMed] [Google Scholar]


