Abstract
Attached gingiva plays a promising role in maintaining periodontal health. An adequate width of attached gingiva prevents plaque formation and soft-tissue recession. Among various techniques for augmenting width of attached gingiva, modified apically repositioned flap (MARF) is a simple and easy procedure that does not require a second surgical site. It is less time-consuming. It provides better operative and postoperative comfort for the patient. In this case series, MARF technique was used for augmenting the width of attached gingiva.
Keywords: Attached gingiva, gingival augmentation, modified apically repositioned flap
INTRODUCTION
Attached gingiva is the portion of gingiva that extends between the mucogingival junction (MGJ) and free gingival groove.[1] This provides protection for periodontium and helps in maintaining the gingival margin at a stable position. Attached gingiva also minimizes the effect of functional forces which are applied by muscle fibers onto gingival tissues. Therefore, it plays a significant role in preserving the health of gingiva.[2]
The minimum required dimensions of attached gingiva needed for gingival health are a controversy.[3] Nabers in 1966,[4] Lang and Loe in 1972,[5] Ochsenbein and Maynard in 1974,[6] and Matter in 1982 stated that the presence of adequate attached gingiva is necessary to maintain gingival health.[7] However, Lindhe and Nyman in 1980[8] and Freedman in 1992[9] refuted the concept and concluded that the gingival health can be maintained independent of the dimensions of attached gingiva. Despite such a controversy, various techniques are employed for augmenting the width of attached gingiva, which includes Nabers in 1954,[10] pushback technique by Goldman et al. in 1956,[11] complete denudation and periosteal separation by Bohannan in 1962,[12,13] apical repositioned flap by Friedman in 1962,[14] and free gingival graft (FGG) by Bjorn in 1963.[15] Of these, most commonly used techniques include apically repositioned flap and FGG, which have various disadvantages such as apically repositioned flap technique left 3–5 mm of denuded bone in the coronal portion which has a risk of bone resorption.[7] Moreover, although FGG technique is considered the gold standard for gingival augmentation procedures, Agarwal et al.[16] and Carnio et al.[17] in 2015 stated several disadvantages in FGG technique such as postoperative discomfort, poor color match, and donor site morbidity.
To overcome these disadvantages, Carnio and Miller in 1999 described the modified apically repositioned flap (MARF) technique for increasing the width of attached gingiva for single tooth and perceived advantages includes ease of execution, predictable color match, decreased surgical time, and no need of the second surgical site.[18] Recently, Carnio and Camargo in 2006 have proposed MARF technique for multiple teeth.[19] Despite the fact that MARF is apparent and simple technique, the prerequisite factor should be a minimum of 0.5 mm of attached gingiva for performing surgery. This case series describes three cases in which augmentation of attached gingiva was done by MARF technique.
CASE REPORT
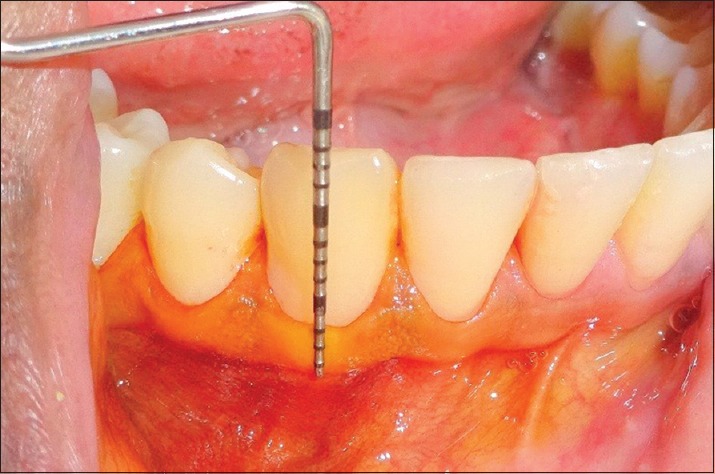
Three patients with an inadequate zone of attached gingiva were selected from the outpatient department of periodontics and implantology. Written informed consent was obtained from all three patients. Patients who were unable to perform routine oral hygiene measures, smokers, individuals with dehiscence and fenestration, bleeding tendencies, pregnancy/lactation, and immunocompromised patients were excluded from the study. Phase I therapy was performed for all the patients and postprophylaxis instructions were advised. At baseline, the clinical parameters such as the probing depth (PD), the width of keratinized tissue (KT), and the width of the attached gingiva were recorded [Figures 1–4]. When measuring apicocoronal dimension, the MGJ was visualized by Lugol's iodine solution. The PD subtracted from the total width of keratinized gingiva gives the dimension of attached gingiva. The apicocoronal distance from MGJ to the gingival margin is the width of KT. PD was measured using the University of North Carolina-15 periodontal probe from the gingival margin to base of the sulcus.
Figure 1.

Preoperative view (Case 1)
Figure 4.
Preoperative width of keratinized gingiva in relation to 43 (Case 3)
Figure 2.

Preoperative width of keratinized gingiva in relation to 43 (Case 1)
Figure 3.

Preoperative width of keratinized gingiva in relation to 34 (Case 2)
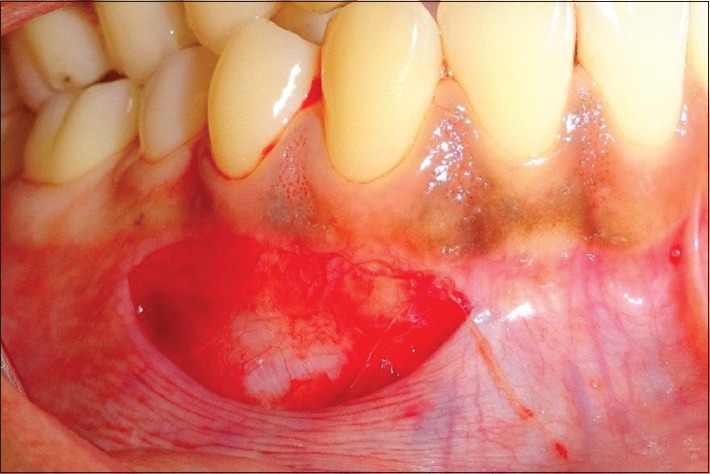
Modified apically repositioned flap procedure
The surgical procedure was performed according to the protocol given by Carnio and Camargo in 2006.[19] After administration of local anesthesia, no. 15 Bard-Parker blade was used to give a horizontal bevel incision with its bevel away from the crest of alveolar bone, and this incision was given at a distance of 0.5 mm from MGJ toward attached gingiva so that this tissue remains intact with flap. To avoid the vertical releasing incisions, a horizontal incision was extended mesiodistally parallel to MGJ till the midbuccal region of the adjacent teeth. A partial-thickness flap was raised so that the flap can be moved apically and simple interrupted absorbable sutures with Vicryl 4-0 were placed for securing the flap to the periosteum. For preventing dead space between the flap and periosteal bed, a gentle finger pressure was applied and the periodontal pack was placed. The surgical procedure is depicted in Figures 5–7.
Figure 5.
Horizontal bevel incision is given (Case 1)
Figure 7.

Periodontal pack placed (Case 1)
Figure 6.

The flap was positioned apically and sutured with 4-0 Vicryl (Case 1)
Postoperative care
Postoperative instructions and medications were given to all the patients. Amoxicillin (500 mg thrice daily for 5 days) and aceclofenac (100 mg thrice daily for 3 days) were given. Patients were instructed to avoid brushing, flossing, manipulating the surgical site with tongue, lips, and fingers for 6 weeks and use 0.12% chlorhexidine mouthrinse twice daily for 3 weeks. Suture removal was done after 2 weeks. All the clinical parameters were recorded at 6 months [Figures 8–11].
Figure 8.

Postoperative view after 6 months (Case 1)
Figure 11.

Postoperative width of keratinized gingiva in relation to 43 at 6 months (Case 3)
Figure 9.

Postoperative width of keratinized gingiva (Case 1)
Figure 10.

Postoperative width of keratinized gingiva in relation to 34 at 6 months (Case 2)
RESULTS
Table 1 represents the differences in clinical parameters from baseline to 6 months in the three cases. Mean change in the PD, the width of KT, and the width of the attached gingiva were 0.15 mm, 3.66 mm, and 3.91 mm, respectively, from baseline to 6 months.
Table 1.
Changes in the clinical parameters from baseline to 6 months
| Cases | Clinical parameters at baseline and at 6 months | |||||
|---|---|---|---|---|---|---|
| At baseline | At 6 months | |||||
| Probing depth | Keratinized tissue | Attached gingiva | Probing depth | Keratinized tissue | Attached gingiva | |
| 1 | 1.16 | 2 | 1 | 1 | 6.5 | 5.5 |
| 2 | 1 | 2.25 | 1.25 | 1 | 6.25 | 5.25 |
| 3 | 1.29 | 2.5 | 0.75 | 1 | 5 | 4 |
DISCUSSION
The attached gingiva plays an important role in protecting periodontal structures as it is composed of keratinized epithelium and dense collagen fibers which provide resistance to mechanical trauma caused by improper brushing technique and facilitate plaque control.[19] When the width of attached gingiva is inadequate, subgingival plaque accumulation occurs because of improper pocket closure and causes loss of attachment and gingival recession due to an apical spread of inflammation. Hence, to maintain periodontal health, an adequate zone of attached gingiva is required. Usually, compared to posteriors, incisors have a greater width of attached gingiva and the premolars have the least width. According to Maynard et al. in 1979, physiological dimensions of about 5 mm of KT with 3 mm of attached gingiva are needed for maintaining gingival health when planning for subgingival restorations.[20] Hall stated that areas with <2 mm of attached gingiva should be monitored for active recession.[21] In situ ations where there is a lack of attached gingiva, a variety of surgical procedures are employed to augment the width of attached gingiva.[2] A rationale for selecting MARF in this case series was that it increases the apicocoronal dimension of attached gingiva with minimal trauma and color match with adjacent tissues.[22]
Lugol's iodine solution was used to visualize the changes in the attached gingiva which eliminates the interoperative discrepancy. If the distance between the bottom of the pocket and the crest of the bone is >2.0 mm, MARF technique is not advisable, as there is a chance of postoperative recession to occur because of the bone dehiscence.[17]
In the postoperative follow-up period of 1 week to 10 days, there is a healthy granulation tissue over the surgical site and was minimally painful for the patients. By the end of 1 month, the treated areas were covered with tissue that was similar to adjacent tissue in terms of color and consistency and became clinically indistinguishable by 6-month follow-up.
In the present case series, a mean change in the PD, width of KT, and width of the attached gingiva was 0.15 mm, 3.66 mm, and 3.19 mm, respectively, and the width of attached gingiva was increased from an average of 1 mm to 4.91 mm from baseline to 6 months. This change was attributed to the fact that epithelial cells on the wound edges will migrate over exposed periosteum. As the surgical area is surrounded by KT, this serves as a source of cells of keratinized phenotype and prevents nonkeratinized epithelial cells originating from the oral mucosa proliferating onto the surgical area. The connective tissue and keratinized epithelial cells surrounding the wound migrate from the margins to cover the exposed surgical site, resulting in augmentation of the attached gingiva.[23]
Carnio and Miller et al. in 1999 conducted a study at 54 single buccal areas with a postoperative follow-up of 72 weeks. This study demonstrated that MARF is an effective method to create new KT for use as a donor site for lateral pedicle flap and can be used as a marginal collar; this prevents marginal tissue recession.[18]
Similarly, Carnio in 2014 showed a gain of KT at donor site before performing laterally positioned flap procedure from 2.78 to 5.07 mm at 8 weeks, and after performing lateral pedicle flap, the width of KT was maintained at 3.28 mm after a follow-up of 18 months.[22]
Results of the present case series were in concordance with the studies conducted by Carnio et al. in 2006[19] and 2007[2] which demonstrated an increase in attached gingiva from baseline to 6 months with MARF technique. Carnio et al. in 2014 conducted a study to evaluate the ability of MARF to gain keratinized gingiva in the donor site before employing a laterally positioned flap and observed that width of keratinized gingiva increased from 2.75 mm to 5.01 mm after 8 weeks.[22]
The limitation of MARF is that it requires the presence of ≥0.5 mm of attached gingiva preoperatively so that it allows the surgical wound to be completely surrounded by KT, which ultimately results in the production of the granulation tissue during healing.[2] However, recently, Carnio et al. in 2017 conducted a clinical and histological evaluation of attached gingiva using MARF and concluded that even in the areas that lack KT, MARF technique can be done for augmenting attached gingiva.[24]
CONCLUSION
MARF is a reliable technique to increase the width of attached gingiva. MARF is a simple surgical procedure when compared to other mucogingival procedures for gingival augmentation. It offers considerable advantages such as good esthetic results and no requirement of a second surgical site. MARF can be used as an alternative to other invasive procedures such as FGG with comparable and reliable results and minimal patient discomfort. Within the limitations of this study, MARF technique has shown predictable results by increasing the width of attached gingiva in a 6-month follow-up period. Definitely, more number of cases are needed to ensure the predictability and success of this technique.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fiorellini JP, Kim DM, Ishikawa SO. The gingiva. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, editors. Textbook of Clinical Periodontology. 10th ed. Missouri: Elsevier Publishers; 2010. pp. 46–7. [Google Scholar]
- 2.Carnio J, Camargo PM, Passanezi E. Increasing the apico-coronal dimension of attached gingiva using the modified apically repositioned flap technique: A case series with a 6-month follow-up. J Periodontol. 2007;78:1825–30. doi: 10.1902/jop.2007.060414. [DOI] [PubMed] [Google Scholar]
- 3.Consensus report. Mucogingival therapy. Ann Periodontol. 1996;1:702–6. doi: 10.1902/annals.1996.1.1.702. [DOI] [PubMed] [Google Scholar]
- 4.Nabers JM. Extension of the vestibular fornix utilizing a gingival graft – Case history. Periodontics. 1966;4:77–9. [PubMed] [Google Scholar]
- 5.Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972;43:623–7. doi: 10.1902/jop.1972.43.10.623. [DOI] [PubMed] [Google Scholar]
- 6.Ochsenbein C, Maynard JG. The problem of attached gingiva in children. ASDC J Dent Child. 1974;41:263–72. [PubMed] [Google Scholar]
- 7.Matter J. Free gingival grafts for the treatment of gingival recession. A review of some techniques. J Clin Periodontol. 1982;9:103–14. doi: 10.1111/j.1600-051x.1982.tb01226.x. [DOI] [PubMed] [Google Scholar]
- 8.Lindhe J, Nyman S. Alterations of the position of the marginal soft tissue following periodontal surgery. J Clin Periodontol. 1980;7:525–30. doi: 10.1111/j.1600-051x.1980.tb02159.x. [DOI] [PubMed] [Google Scholar]
- 9.Freedman AL, Salkin LM, Stein MD, Green K. A 10-year longitudinal study of untreated mucogingival defects. J Periodontol. 1992;63:71–2. doi: 10.1902/jop.1992.63.2.71. [DOI] [PubMed] [Google Scholar]
- 10.Nabers CL. Repositioning the attached gingiva. J Periodontol. 1954;25:38–9. [Google Scholar]
- 11.Goldman HM, Schluger S, Fox L. St. Louis: C.V. Mosby Co; 1956. Periodontal Therapy; pp. 301–11. [Google Scholar]
- 12.Bohannan HM. Studies in the alteration of vestibular depth. I. Complete denudation. J Periodontol. 1962;33:120–8. [Google Scholar]
- 13.Bohannan HM. Studies in the alteration of vestibular depth. II. Periosteum retention. J Periodontol. 1962;33:354–9. [Google Scholar]
- 14.Friedman N. Mucogingival surgery: The apically repositioned flap. J Periodontol. 1962;33:328–40. [Google Scholar]
- 15.Bjorn H. Free transplantation of gingiva propria. Sven Tandlak Tidskr. 1963;22:684–9. [Google Scholar]
- 16.Agarwal C, Tarun Kumar AB, Mehta DS. Comparative evaluation of free gingival graft and alloDerm(®) in enhancing the width of attached gingival: A clinical study. Contemp Clin Dent. 2015;6:483–8. doi: 10.4103/0976-237X.169838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carnio J, Camargo PM, Pirih PQ. Surgical techniques to increase the apicocoronal dimension of the attached gingiva: A 1-year comparison between the free gingival graft and the modified apically repositioned flap. Int J Periodontics Restorative Dent. 2015;35:571–8. doi: 10.11607/prd.2386. [DOI] [PubMed] [Google Scholar]
- 18.Carnio J, Miller PD., Jr Increasing the amount of attached gingiva using a modified apically repositioned flap. J Periodontol. 1999;70:1110–7. doi: 10.1902/jop.1999.70.9.1110. [DOI] [PubMed] [Google Scholar]
- 19.Carnio J, Camargo PM. The modified apically repositioned flap to increase the dimensions of attached gingiva: The single incision technique for multiple adjacent teeth. Int J Periodontics Restorative Dent. 2006;26:265–9. [PubMed] [Google Scholar]
- 20.Maynard JG, Jr, Wilson RD. Physiologic dimensions of the periodontium significant to the restorative dentist. J Periodontol. 1979;50:170–4. doi: 10.1902/jop.1979.50.4.170. [DOI] [PubMed] [Google Scholar]
- 21.Hall WB, editor. Critical Decisions in Periodontology. 4th ed. Hamilton, Ontario: B.C. Decker Inc; 2003. Establishing the adequacy of attached gingiva; p. 106. [Google Scholar]
- 22.Carnio J. Modified apically repositioned flap technique: A surgical approach to enhance donor sites prior to employing a laterally positioned flap. Int J Periodontics Restorative Dent. 2014;34:423–9. doi: 10.11607/prd.1562. [DOI] [PubMed] [Google Scholar]
- 23.Karring T, Lang NP, Löe H. The role of gingival connective tissue in determining epithelial differentiation. J Periodontal Res. 1975;10:1–11. doi: 10.1111/j.1600-0765.1975.tb00001.x. [DOI] [PubMed] [Google Scholar]
- 24.Carnio J, Camargo PM, Klokkevold PR, Lin YL, Pirih FQ. Use of the modified apically repositioned flap technique to create attached gingiva in areas of no keratinized tissue: A Clinical and histologic evaluation. Int J Periodontics Restorative Dent. 2017;37:363–9. doi: 10.11607/prd.2824. [DOI] [PubMed] [Google Scholar]


