Abstract
Background
As India’s accredited social health activist (ASHA) community health worker (CHW) programme enters its second decade, we take stock of the research undertaken and whether it examines the health systems interfaces required to sustain the programme at scale.
Methods
We systematically searched three databases for articles on ASHAs published between 2005 and 2016. Articles that met the inclusion criteria underwent analysis using an inductive CHW–health systems interface framework.
Results
A total of 122 academic articles were identified (56 quantitative, 29 mixed methods, 28 qualitative, and 9 commentary or synthesis); 44 articles reported on special interventions and 78 on the routine ASHA program. Findings on special interventions were overwhelmingly positive, with few negative or mixed results. In contrast, 55% of articles on the routine ASHA programme showed mixed findings and 23% negative, with few indicating overall positive findings, reflecting broader system constraints. Over half the articles had a health system perspective, including almost all those on general ASHA work, but only a third of those with a health condition focus. The most extensively researched health systems topics were ASHA performance, training and capacity-building, with very little research done on programme financing and reporting, ASHA grievance redressal or peer communication. Research tended to be descriptive, with fewer influence, explanatory or exploratory articles, and no predictive or emancipatory studies. Indian institutions and authors led and partnered on most of the research, wrote all the critical commentaries, and published more studies with negative results.
Conclusion
Published work on ASHAs highlights a range of small-scale innovations, but also showcases the challenges faced by a programme at massive scale, situated in the broader health system. As the programme continues to evolve, critical comparative research that constructively feeds back into programme reforms is needed, particularly related to governance, intersectoral linkages, ASHA solidarity, and community capacity to provide support and oversight.
Electronic supplementary material
The online version of this article (10.1186/s12961-019-0427-0) contains supplementary material, which is available to authorized users.
Keywords: Community health worker, Accredited social health activist, India, health policy and systems research, training and supervision, primary healthcare
Introduction
National community health worker (CHW) programmes are receiving renewed attention as mechanisms to help overcome health worker shortages, retain health workers in underserved areas, and provide culturally appropriate primary healthcare [1–3]. No longer seen as stop-gap or a temporary solution, they are now considered as part of long-term investments for responsive and community-oriented health systems [4, 5].
Despite such endorsement, several gaps in knowledge remain in ensuring that CHW programmes deliver at scale across diverse national contexts. There is ongoing discussion about how best to facilitate and sustain community and health systems support for CHW programmes [5], how CHWs should be remunerated [6–8]. and the role of CHW programmes in supporting or undermining health worker rights and gender equity [9–11]. Looking to the future, questions arise on how to support CHW programme evolution to meet changing health needs (e.g., increasing prevalence of non-communicable diseases), changing contexts (e.g., rapid urbanisation), and changing roles (e.g., engaging in service accountability) [12]. Reviews of the literature on CHW programmes have provided valuable insight into health system considerations of CHW programmes [3, 13, 14], including on supervision strategies [15, 16], the influence of context and programme features on CHW productivity [17–19], the extent to which CHW programmes provide equitable healthcare [20], cost effectiveness [21], and considerations for operating national, scaled up programmes [22, 23]. Country-specific literature reviews have been performed for Brazilian [24–26] and Ghanaian [27] CHW programmes; these reviews identified policy and research gaps and explored how CHW roles and identities bridge the gap between community and health services. The only existing review on CHW programmes in India focuses on the rights of CHWs themselves [9], identifying shortcomings in terms of remuneration and labour rights.
In 2005, India launched the accredited social health activist (ASHA) programme as a key component of their National Rural Health Mission to strengthen rural government service delivery, as well as community engagement and ownership in health programmes [28]. The ASHA programme involved the selection of one woman per village (approximately 1 per 1000 population) who would receive an initial 23 days of training on basic health topics and link community members to health services, provide basic first aid and supplies, and mobilise the community around water, sanitation, nutrition and health issues. In 2015, the programme matured into the National Health Mission and was extended to marginalised urban areas. With almost one million ASHAs now selected and trained, it has grown to become one of the largest CHW programmes in the world. As it enters its second decade, we take stock of the current knowledge base understand the nature of the research undertaken and whether it examines the health systems interfaces required to sustain and evolve such a large-scale programme.
Methods
Systematic mapping – rather than systematic review – was appropriate for our interest in identifying and describing all articles published on the topic. Systematic mapping enables the inclusion of the entire range of academic research on the topic of interest, rather than limiting inclusion to research that addresses a single, clearly defined systematic review question [29]. Since systematic mapping includes articles using any methodology, and since it seeks to define the landscape of work on the subject rather than present evidence on a specific narrow question, assessment of the quality of included research is not appropriate.
Search strategy
We searched the electronic databases PubMed, Embase and Scopus, which index the largest number of publications and most prominent journals in public health, biomedicine and the social sciences [30–32], for articles published between 1 January 2005 and 9 August 2016. The year 2005 was selected as the beginning date because that was when the ASHA programme was announced and launched. Searches were developed in consultation with an academic librarian at Johns Hopkins University. Searches incorporated keywords and free text for two concepts, namely CHWs (e.g. global terms such as ‘community health worker’ and ‘lay health worker’ as well as ‘accredited social health activist’, ‘ASHA’ and the state-specific names of the ASHA programme, such as Mitanin and Sahyogini) and India (e.g. India* and the names of all Indian states), with the two strings joined by the Boolean operator ‘AND’. See Additional file 1 for the full search strategy.
Eligibility criteria, screening and article selection
Articles were included if they (1) presented substantial information on India’s ASHA CHWs and (2) were academic empirical research or commentaries. We included articles that discussed multiple CHW programmes as long as they had meaningful content on the ASHA programme. We included full text manuscripts as well as published abstracts and short articles. We excluded research protocols as well as articles that did not directly mention ASHAs or mentioned them only in passing without information on their role. We also excluded articles about Indian CHW programmes that were not the government’s ASHA programme (e.g. smaller NGO programmes). One author reviewed all titles and abstracts. Potential bias was mitigated in two ways. First, the reviewing author took an inclusive approach in terms of article format and content, accepting article formats including research abstracts and commentaries, and only excluding articles that clearly had no meaningful content on the ASHA programme. Second, all borderline or unclear cases were discussed with the other authors to reach consensus on inclusion. Full texts of retained articles underwent a final screening for eligibility. We were willing to include articles in Hindi; however, no non-English articles were identified. Grey literature on the ASHA programme was beyond the scope of this review, as we were seeking to understand and synthesise the current academic research published on the programme.
Data extraction and synthesis
Detailed data were extracted by one researcher into a pilot-tested framework in Microsoft Excel, which included the following data extraction components and article assessments.
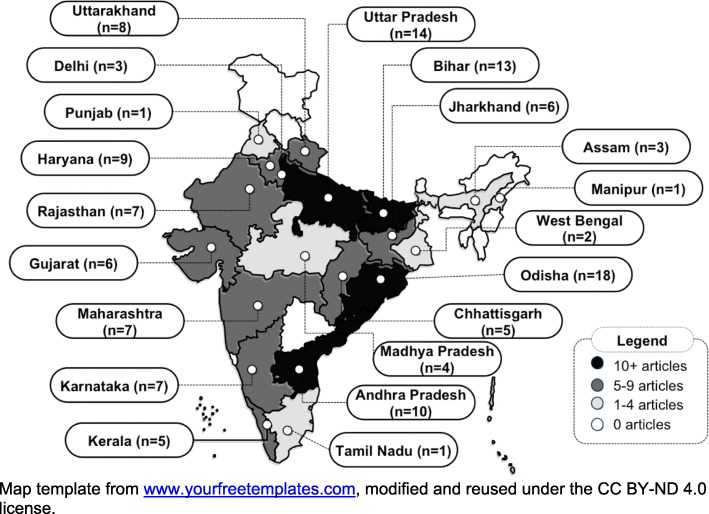
Location
We assessed the location of the research conducted on the ASHA programme to describe its geographical spread (presented in Fig. 3). To do so, we counted the number of studies in each Indian state. Studies conducted in multiple states were counted once for each state. We did not count articles that took a national perspective or that did not specify the state where their research was conducted.
Fig. 3.
Research on the ASHA programme, by state
Health condition focus
Articles that focused on a particular health condition were classified into the following categories: neonatal and child health, sexual and reproductive health, communicable diseases, and non-communicable diseases (Table 1). Any article that did not have a specific health condition focus was classified as ‘general ASHA work’.
Table 1.
Health condition focus of publications on ASHAs (n = 122)
| Health condition focus | Routine | Special | Total | Health policy and systems research |
|---|---|---|---|---|
| Neonatal and child health | 28 | 11 | ||
| • Integrated management of childhood illness [86, 88, 90, 156], pneumonia care [36], diarrhoea care [38, 39], other child health [105] | 5 | 4 | 9 | 4 |
| • Home-based neonatal care [63, 93, 119, 138], other newborn health [94, 144, 150] | 3 | 5 | 8 | 4 |
| • Immunisation [40, 46, 145, 148] | 4 | 0 | 4 | 2 |
| • Nutrition (breastfeeding, infant and young child feeding) [97, 106, 115, 129] | 1 | 3 | 4 | 0 |
| • Other: childhood developmental delay and disability [124], infant and maternal death tracking [113], pregnancy, delivery and infant death tracking [120] | 0 | 3 | 3 | 1 |
| Sexual and reproductive health, including maternal health | 27 | 12 | ||
| • Maternal healthcare, including pregnancy detection, antenatal care, pre-eclampsia, timely referral [37, 64, 87, 101, 114, 136, 141], institutional delivery [52, 55, 92, 132, 133, 137], maternal death investigation [134] | 12 | 3 | 15 | 11 |
| • Abortion and contraceptives [67, 107, 117, 118, 146] | 1 | 4 | 5 | 1 |
| • HIV [79–83] | 0 | 5 | 5 | 0 |
| • Others: uterine prolapse [95], cervical cancer screening [159] | 0 | 2 | 2 | 0 |
| Communicable diseases | 13 | 3 | ||
| • Malaria [49, 54, 60, 61, 139] | 3 | 2 | 5 | 3 |
| • Leprosy [48, 77, 78] | 1 | 2 | 3 | 0 |
| • Visceral Leishmaniasis (kala-azar) [72, 73, 76] | 1 | 2 | 3 | 0 |
| • Others: tuberculosis [104], filariasis [58] | 2 | 0 | 2 | 0 |
| Non-communicable diseases | 8 | 2 | ||
| • Mental health [91, 110] | 2 | 1 | 3 | 0 |
| • •Cardiovascular diseases [85, 125] | 1 | 1 | 2 | 1 |
| • Multiple non-communicable diseases [122, 123] | 0 | 2 | 2 | 1 |
| • Tobacco control [41] | 1 | 0 | 1 | 0 |
| Sub-total of all publications with a health focus | 37 | 39 | 76 | 28 |
| General ASHA work | 41 | 5 | 46 | 45 |
| Total | 78 | 44 | 122 | 73 |
Routine versus special intervention
We classified all articles according to whether they focused on the routine work of ASHAs within the national programme (e.g. assessments of typical ASHA practice) or were small-scale special interventions that engaged with ASHAs above and beyond their routine government work (e.g. pilot mHealth interventions or special surveys that used ASHAs as enumerators) (also presented in Table 1).
Evaluation outcomes
Among studies that presented evaluative findings, we assessed whether these findings were broadly positive (such as ASHAs having high knowledge or effectively performing a new skill), negative (such as ASHAs having poor knowledge or low motivation) or mixed (such as ASHAs facing significant challenges but also gaining self-esteem, effectively delivering some health services or benefitting from key support structures).
Health systems perspective
We considered an article to have taken a health systems perspective if it examined health systems elements, such as supervision, training, supply chain management, financing, motivation, etc., or if the article discussed linkages or repercussions between health systems dimensions such as how communities supported ASHAs or whether facility providers were responsive to ASHAs.
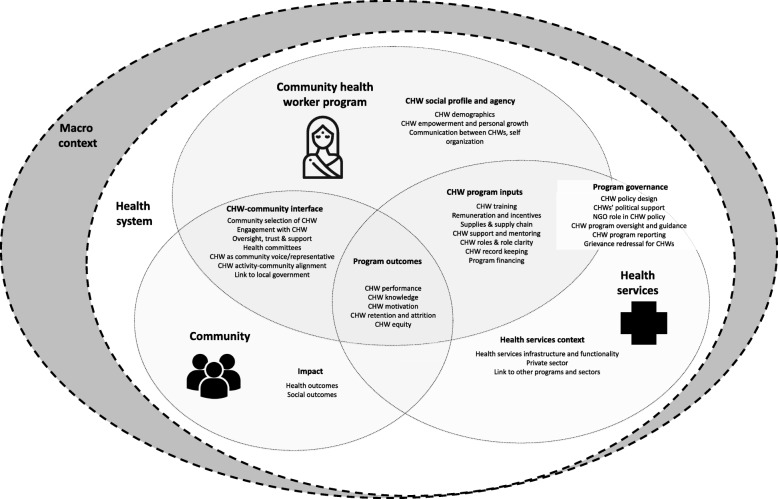
CHW–health systems interface
We developed a CHW–health system interface framework and assessed the number of publications providing information on the topics in the framework, specifically on CHW social profile and agency, CHW programme inputs, CHW–community interface, health services context, programme governance, programme outcomes, and programme impact (Fig. 1). The framework was developed through discussion among team members, review of existing CHW frameworks [5, 18, 19, 23, 33, 34], and during a workshop among Indian and African researchers. While reading each article, we extracted any meaningful content falling under each of the topics in the framework and then counted the number of articles providing information for each topic. For an article to be counted as providing meaningful information it had to present some new data or novel comment, critique or interpretation related to the topic. Thus, for example, under the topic ‘CHW programme inputs’ sub-topic ‘remuneration and incentives’ an article presenting a background description of the remuneration system for ASHAs would not be counted, whereas an article pilot testing an add-on incentive or presenting findings on how ASHAs feel about their remuneration would be counted. Table 2 presents details on how each topic applies to the ASHA programme and the number of articles with substantive content on each topic.
Fig. 1.
Community health worker – health system interface framework
Table 2.
CHW–health system interface topics discussed in publications on ASHAs
| Main topic | Sub-topics | Application to ASHA programme | Number of publications with content on sub-topic |
|---|---|---|---|
| Programme inputs | Training and capacity-building | Descriptions of training and capacity-building provided to ASHAs, challenges associated with ASHA training, how ASHAs feel about training, percentages of ASHAs receiving training | 62 |
| Supplies and supply chain | The type and amount of supplies ASHAs receive (including their routine drug kids and extra supplies from small scale interventions, such as mHealth programmes), how ASHAs feel about their supplies, issues of resupply and stock outs | 42 | |
| Support and monitoring | ASHA relationships with frontline workers (such as auxiliary nurse midwives, medical officers, ASHA facilitators), including how they work together and the extent to which they receive monitoring and supportive supervision (routinely and in small-scale interventions) | 41 | |
| Incentives and remuneration | Financial incentives provided and changes to them, timeliness and access to remuneration, ASHA satisfaction with remuneration | 38 | |
| Roles and role clarity | The roles ASHAs have been given, including the evolution of routine roles and roles given in special interventions, and the extent to which ASHAs understand their roles | 35 | |
| CHW record keeping | What records ASHAs maintain (such as monthly reports, village registers), how they feel about these records, challenges related to ASHA record keeping such as completeness and correctness | 16 | |
| Programme outcomes | CHW performance | Functionality, effectiveness, skills, practice – what services ASHAs provide, what tasks they perform, and/or how well they provide these services or perform these tasks, including coverage of services (but not in terms of equity or which households they cover, which is counted in ‘CHW equity’) | 79 |
| CHW knowledge | How much ASHAs know about various health topics | 30 | |
| CHW motivation | ASHA job satisfaction, how motivated ASHAs are to do their work, what their sources of motivation are (but not their motivation to continue working as an ASHA, which is counted below under ‘retention and attrition’) | 30 | |
| CHW equity | Which households ASHAs reach in terms of marginalisation, social distribution of services | 17 | |
| CHW retention and attrition | Intention to remain an ASHA, drop-out rates | 9 | |
| CHW–community interface | Community engagement with CHWs | Community knowledge of their ASHA, trust in their ASHA and satisfaction with their ASHA, factors that influence this relationship | 34 |
| Resonance of CHW activities | Extent to which ASHA activities align and resonate with community needs | 22 | |
| Community selection of CHW | Extent and manner through which the community was involved in deciding who should be their ASHA | 16 | |
| Link to local government | Involvement of the local government structure (panchayat) in any aspect of the ASHA programme | 15 | |
| Health committees | ASHA role in convening village health and sanitation committee meetings, activities undertaken by the committee in relation to the ASHA | 13 | |
| Community oversight of and support for CHW | Community oversight of the ASHA, ASHA accountability to the community, community provision of support for the ASHA | 10 | |
| CHW as community voice or representative | ASHA as a representative of the community’s perspectives, voices and needs to health system functionaries | 8 | |
| Programme governance | CHW policy design and development | Policy recommendations to strengthen the ASHA programme, discussions about how policy was set or should be set, critiques of ASHA-related policy | 27 |
| CHW programme oversight and guidance | Formal oversight and guidance systems to shape the ASHA programme, particularly the role of national and state health resource centres | 8 | |
| CHW political support | Political buy-in to the ASHA programme at the national and state levels; ASHA political engagement and advocacy, such as through unionisation | 7 | |
| Role of NGO actors in CHW policy | Role of NGO actors in shaping the ASHA programme, such as NGOs, academics and private sector interest groups | 6 | |
| Grievance redressal for CHWs | The development and functioning of formal government mechanisms through which ASHAs could register grievances | 5 | |
| Programme financing | How much money is budgeted to fund the ASHA programme and how these decisions are made, release of funding, comments on financing issues | 5 | |
| CHW programme reporting | Systematic programme management records that the government system creates about the ASHA programme (such as national or state level reports, annual nodal officer meeting minutes) | 2 | |
| CHW social profile and agency | CHW demographics | ASHA demographic information such as ASHA age, caste, marriage, and literacy statistics, or comments on these issues (e.g. caste dominance among ASHAs) | 41 |
| Empowerment and personal growth | Comments or research on ASHA well-being, personal growth, rights-related challenges and opportunities including for leadership, career progression or educational advancement | 14 | |
| Communication between CHWs | Opportunities and nature of ASHA-to-ASHA communication, such as through meetings, radio shows or newsletters | 3 | |
| Impact | Health outcomes | ASHA programme-related changes in community healthcare-seeking, health-related behaviour and knowledge, and wellbeing/illness outcomes (including the health-related outcomes of small-scale special interventions involving ASHAs) | 41 |
| Social outcomes | ASHA programme-related changes in non-health outcomes such as community-level environmental health and gender relations or programmatic/out-of-pocket costs (including the social-related outcomes of small-scale special interventions involving ASHAs) | 6 | |
| Health services context | Health system infrastructure and functionality | The quality and availability of drugs, transportation, diagnostics, infrastructure, and health workers in the government health sector, including behaviour of health workers towards patients, and how this context influences the ASHA’s work | 24 |
| Private sector | The quality and availability of the informal (such as traditional birth attendants) and formal private healthcare sector and how this influences the ASHA’s work, including public–private partnerships within the National Health Mission | 17 | |
| Linkages to other programmes | Intersectoral linkages between the ASHA programme (within the Ministry of Health and Family Welfare) and nutrition/anganwadi services through the Integrated Child Development Scheme, water and sanitation | 12 |
Research typology and methodology
We classified each study according to whether they were reflective commentaries or primary research. All primary studies were further classified according to a health policy and systems research typology [35], wherein ‘descriptive research’ describes a context, population or phenomena, enabling comparability with other contexts and experiences; ‘exploratory research’ builds initial understanding and early hypothesis; ‘explanatory research’ involves in-depth research often with triangulation and using and testing theory to explain causal mechanisms; ‘research to establish influence’ (adequacy, plausibility or probability) assesses the impact of one variable on another; ‘emancipatory research’ is used to jointly understand a problem, act on it, and learn from working collaboratively to address power; and ‘predictive research’ is used to anticipate the consequences of decisions.
Authorship
To analyse authorship, we assessed the institutional affiliation of the first author as domestic (based in India), foreign (any country other than India) or global (international bodies, including WHO, UNICEF and the World Bank). To understand collaboration and partnership between Indian and foreign institutions, we coded the affiliations of all authors as solely domestic (Indian), solely foreign, mixed domestic and foreign, or global.
Results
From 2786 unique references identified in our search, 122 articles met our inclusion criteria (Fig. 2), of which 56 were quantitative, 29 mixed methods, 28 qualitative, and 9 commentary or synthesis. Additional file 2 presents the complete references of included articles. Additional file 3 presents a sortable excel database of included articles. Additional files 4 and 5 provide an overview of article findings.
Fig. 2.
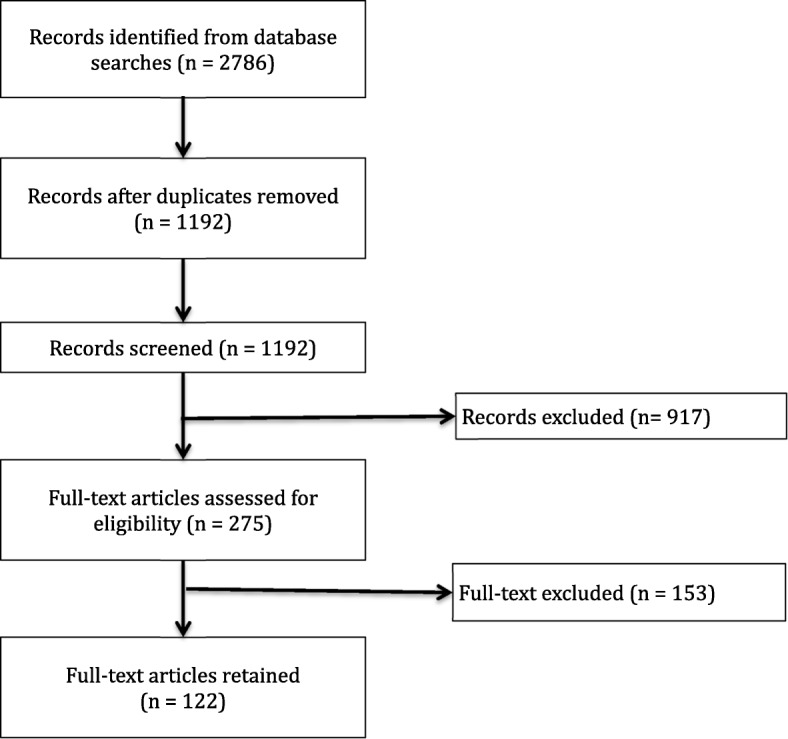
Diagram of article screening process
Location: where in India is research on the ASHA programme being performed?
Seventeen articles were about the ASHA programme as a national programme and thus did not have a specific research location. Of those articles that specified geographic location, while 13 involved comparative research conducted in multiple states [36–48], the great majority was conducted within a single state. Overall, research on the ASHA programme is concentrated in large northern states (Fig. 3), with most articles reporting research from Odisha (formerly Orissa) [42–44, 47, 49–62], then Uttar Pradesh [36, 38–40, 46, 63–71] and Bihar [36–39, 44, 46, 48, 72–77]. Significant numbers of published articles came from Andhra Pradesh [41, 44, 78–85], Haryana [86–94], Uttarakhand [40, 95–101], Maharashtra [37, 45, 102–106], Rajasthan [37, 40, 44, 45, 107–109], Karnataka [110–116], Jharkhand [42–44, 47, 117, 118], and Gujarat [38, 39, 41, 119–121]. In contrast, fewer articles were published on the ASHA programme in Kerala [44, 122–125], Chhattisgarh [126–130], Madhya Pradesh [131–134], Delhi [135–137], Assam [44, 138, 139], West Bengal [44, 48], Manipur [140], Punjab [141], and Tamil Nadu [37].
There is no research from the union territories,1 which are administrative areas with no legislative assemblies and have very few ASHAs. There was also no research from several small north-eastern states (Sikkim, Arunachal Pradesh, Meghalaya, Mizoram, Nagaland and Tripura), Jammu and Kashmir or from Telangana, which was created in 2014 and thus has only existed as a separate entity for a few years.
Health condition focus of articles
Out of 122 published articles, 76 (62%) focused on a particular health condition (Table 1). The most common health foci were neonatal and child health (n = 26) and sexual and reproductive health, including maternal health (n = 26), with fewer articles focusing on communicable (n = 13) and non-communicable diseases (n = 9). The more affluent southern Indian states of Kerala, Andhra Pradesh and Karnataka were frequently the research sites for innovative efforts to address non-communicable diseases [85, 110, 122, 123, 125]. In addition, all five of the publications on HIV are from one project in Andhra Pradesh on engaging with ASHAs to support women living with HIV [79–83].
Of the 46 articles (38%) without a specific health topic focus, many relate to cross-cutting functions that support the ASHA’s core role as maternal and child health promoters. These articles include research on the association between educational level and ASHA capacity (such as filling in the village health register tracking children and pregnant women) [65], the ASHA’s role in multiple reproductive, maternal and child health functions [50, 51, 56], in village health and nutrition days [59, 99], and in village health, sanitation and nutrition committees [43] (Table 1).
Routine versus special intervention focus
Of the 122 papers, 78 (64%) focused on the routine ASHA programme. Details of these publications are presented in Additional file 4. The remaining 44 (36%) were about special interventions that engaged ASHAs beyond their official roles and responsibilities such as pilot interventions. Details of these programmes are presented in Additional file 5.
Evaluation outcomes
Findings in the publications on the routine ASHA programme were mostly mixed (55%, n = 43/78) and negative (23%, n = 18/78), with few indicating overall positive findings (13%, n = 10/78). In contrast, findings in the publications on special interventions were overwhelmingly positive (77%, n = 34/44), with few negative (5%, n = 2/44) or mixed (9%, n = 4/44) results. Article-wise assessments of evaluation outcomes can be found in Additional files 4 and 5.
Health systems perspective
Over half the articles (60%, n = 73/122) took a health systems perspective when researching and discussing the ASHA programme (right-hand column of Table 1). While only one-third of the 76 studies with a health condition focus had a health systems perspective (37%, n = 28/76), almost all the 46 studies on general ASHA work did so (98%, n = 45/46). The only article on general ASHA work that did not take a health system perspective was an assessment of ASHA knowledge across a range of topics related to their expected areas of work [131].
CHW–health systems interface
When considering article content in relation to the CHW–health system interface framework (Fig. 1), across the 122 articles, ASHA performance (65%, n = 79/122) and ASHA training and capacity-building (51%, n = 62/122) were discussed across the largest number of publications (Table 2). At the other end of the spectrum, five or fewer articles discussed programme financing, programme reporting, grievance redressal for ASHAs, and communication between ASHAs (Table 2).
In terms of CHW programme inputs, most of the articles on ASHA training and capacity-building discussed these inputs alongside other health system concerns. Only two publications took training and capacity-building as their primary focus – one commentary on training [142] and one study reporting on an intervention to improve supportive supervision [71]. After training and capacity-building, programme inputs related to supply chains, incentives and remuneration, support and monitoring, and CHW roles and role clarity were all mentioned in a large number of publications (n = 35–42/122). Less attention was given to CHW record keeping (n = 16/122).
With regards to incentives and remuneration, 12 (10%) articles focused specifically on this topic, including research on the link between incentives and performance, the influence of introducing payment vouchers for home-based newborn care [138], how adding incentives influenced the Mitanin programme [127] and many studies examining aspects of the Janani Suraksha Yojana programme, which provides ASHAs and pregnant women with cash incentives to promote institutional delivery and postnatal care [52, 53, 55, 92, 132, 133, 137]. Those that had a specific focus on the support and monitoring relationship between ASHAs and frontline health workers included two that tried pairing ASHAs with male health workers [50, 51] and one on trust and teamwork [57].
Programme outcomes, and especially ASHA performance, were discussed in more than half of the articles, and was the focus of 11 (9%) articles, including research linking ASHA education or selection with ASHA performance [65, 66, 98, 112], mHealth to improve performance [64, 74, 120, 121], the tasks ASHAs perform and the extent to which they reach marginalised households [116], their motivation to perform [109], and issues of burn out [96]. Other aspects of programme outcomes, such as CHW knowledge and motivation, also received fair attention (25%, n = 30/122), in contrast to CHW equity (13%, n = 16/122) and CHW retention and attrition (7%, n = 9/122).
In terms of the CHW–community interface, the most frequently discussed sub-topics were community engagement with CHWs (28%, n = 34/122) and resonance of CHW activities with community members (18%, n = 22/122). However, few articles examined community selection of CHWs (13%, n = 16/122), links to local government (the Panchayati Raj institutions) (12%, n = 15/122), the role of health committees (11%, n = 13/122), community oversight and support for CHWs (8%, n = 10/122), and CHW as a community representative (7%, n = 8/122). Ten articles (8%) focused specifically on the CHW–community interface, including ASHA relationships with the community [36, 40, 69, 143], village health and nutrition days [59, 99], health committees [43, 144], a maternal health video dissemination intervention [70], and ASHA communication and leadership in their communities [68].
Most sub-topics within programme governance were rarely discussed in the literature. Although the programme policy’s design and development was commented on in 27 articles, few articles discussed CHW programme oversight and guidance (n = 8), CHW political support (n = 7), the role of NGO actors in CHW policy (n = 6), grievance redressal for CHWs (n = 5), programme financing (n = 5), or CHW programme reporting (n = 2).
Within CHW social profile and agency, many articles (34%, n = 41/122) included content on ASHA demographics but few discussed issues related to ASHA empowerment (11%, n = 14/122) or communication between ASHAs (2%, n = 3/122). Five articles focused specifically on ASHA rights and wellbeing, including taking gender- and rights-based perspectives on remuneration and employment conditions [9, 45, 102, 108] and other ASHA struggles related to supplies, training and payment [89].
Over one-third of the articles (34%, n = 41/122) provided information on health outcomes linked to the programme, but few (5%, n = 6/122) discussed social outcomes, such as on women’s empowerment [9, 108, 126] or cost effectiveness [49, 75, 90].
In terms of health services context, the link between the health system’s functionality and the ASHA programme was discussed in 24 articles (20%), while the private sector was only discussed in 17 articles (14%). Linkages between the ASHA programme and other programmes (such as for nutrition, water or sanitation) were only discussed in 12 (10%) articles.
Research design
The bulk of the research undertaken on the ASHA programme was descriptive (36%, n = 44/122), although a fairly large proportion aimed to evaluate the influence of particular factors on ASHAs (32%, n = 39/122). Fewer articles were exploratory (14%, n = 17/122) or explanatory (195, n = 23/122), and nine were reflective commentaries (7%, n = 9/122). There were no articles that were emancipatory or predictive. See Additional file 6 for a detailed classification of each article.
Among descriptive studies, the great majority, whether quantitative, qualitative or mixed, focused on the knowledge or performance of ASHAs on specific health conditions. Substantial numbers of descriptive surveys were undertaken by ASHAs to screen for health conditions, with the accuracy of such screening verified by other data sources in several studies. Outlier descriptive studies include a post-intervention survey to measure the effect of ASHAs in reducing obstetric delays [37], a mixed methods study that combined system-generated data with key informant interviews to assess health system readiness, including that of ASHAs, for malaria [54], and a formative study for an mHealth intervention inclusive of ASHAs [121].
Most influence research studies that assessed the effectiveness of ASHAs involved programme research with little consideration of health systems dimensions. Furthermore, findings on ASHAs were often subsumed among a range of frontline workers who were assessed. Outlier studies with health systems elements included a mixed methods evaluation on the impact of the Janani Suraksha Yojana programme on ASHA motivation and performance, among other factors [52]. Other studies sought to evaluate the effect of home-based neonatal care incentives on knowledge and practices [138], increasing knowledge of safe medical abortion on average monthly client load at health centres [118], and influence of ASHAs on immunisation coverage [145].
Among exploratory studies, two were quantitative in nature. One developed a scale to measure communication and leadership of ASHAs [68] and another developed a framework for mHealth adoption [74]. There was only one mixed methods exploratory study that sought to understand the underlying barriers to using emergency contraception among a range of providers, including ASHAs [146]. The majority of the qualitative exploratory studies sought to understand the underlying mechanisms of the ASHA programme [62, 89, 140], barriers to point-of-care testing, including by ASHAs [111], and the potential for new areas of work for ASHAs, whether cardiovascular health [125], non-communicable diseases [122], or treatment of child pneumonia [36]. Insightful health systems exploratory research included that exploring task-sharing of ASHAs with male workers [50, 51], coordination among frontline workers [109], and ethnographies by Mishra [56] and Nordfeldt and Roalkvam [40].
Explanatory mixed methods studies also discussed in more depth the underlying factors supporting overall programme performance of ASHAs [44], their role in health systems that fail women seeking obstetric care [134], mHealth interventions used by ASHAs [70, 85] and diarrhoea management including that of ASHAs [38]. Two studies focused on motivation and emotional labour, one using a Likert scale [53] and the other structural equation modelling [96]. Mixed methods explanatory studies also sought to understand questions of remuneration and the feminisation of labour [45, 102].
Amongst qualitative explanatory studies, case study research was used for an in-depth understanding of the ASHA programme [100, 126, 130]. In-depth ethnographies included those on integration and teamwork [57], notions of citizenship [108], incentives [127] and community participation [103].
Various reviews provided insight on the ASHA programme. Some drew from previous CHW experiences in India to flag issues for the current ASHA programme [147], particularly with regards to rights of ASHAs [9]. Others drew from international experience to generate lessons for how best to use CHWs for immunisation in India [148], understand CHW scale-up [149], CHW remuneration [6] or systems integration [23].
Several reviews reflected health policy and systems issues relevant to the ASHA programme, whether related to community processes [143], system readiness for newborn care [150], HIV [79], or CHW scale-up in general [151]. Some reviews were particularly critical of previous government training efforts and the implications for the ASHA programme [142] and were concerned about the overall nature of the ASHA programme [152–155].
Authorship analysis: who is publishing on the ASHA programme?
Over half (59%, n = 72/122) of the papers were written by authors solely affiliated with domestic (Indian) institutions and over one-quarter (30%, n = 37/122) were produced by partnerships between domestic and foreign institutions. Only 11 (9%) were written by authors solely from foreign institutions. This pattern of strong domestic involvement in research either solo or in partnership with foreign organisations was further emphasised with first authorship. Almost three-quarters of the articles’ first authors are affiliated with Indian institutions (74%, n = 90/122), with the remaining first authors affiliated with foreign (24%, n = 29/122) and global (3%, n = 3/122) organisations. Among articles produced by partnership between domestic and foreign organisations, first authorship was 50% domestic and 50% foreign.
The location of authorship was associated with the article type. Negative findings represented a minority of the overall studies, but were largely reported by domestic first authors (20%, n = 18/90), as opposed to foreign first authors (7%, n = 2/29). In terms of research design and typology (Table 3), domestic first authors wrote all the reflective commentaries and the majority of the descriptive and explanatory research articles (89%, n = 39/44), while foreign first authors dominated review articles. With regards to influence studies, there was a shift from Indian first authors leading articles for simpler designs (adequacy and plausibility), with partnerships with foreign authors being more important for probability designs and exploratory studies.
Table 3.
Domestic versus foreign authorship by research typology
| Article typology | First author is: | Row total | ||
|---|---|---|---|---|
| Domestic | Foreign | Other | ||
| Descriptive | 39 | 4 | 1 | 44 |
| Explanatory | 13 | 4 | 0 | 17 |
| Explanatory (Review) | 1 | 5 | 0 | 6 |
| Exploratory | 10 | 7 | 0 | 17 |
| Influence: adequacy | 8 | 2 | 1 | 11 |
| Influence: plausibility | 4 | 1 | 0 | 5 |
| Influence: probability | 7 | 5 | 1 | 13 |
| Reflective commentary | 9 | 0 | 0 | 9 |
| Column total | 91 | 28 | 3 | 122 |
We assessed funding sources for research on the ASHA programme and found that 49 of the 122 articles (40%) did not disclose any information on funding, while for 8 articles the authors stated that they received no funding for their work. Of those that did disclose funding, foundations (such as the Bill and Melinda Gates Foundation) were the largest funders (15%, n = 18/122), bilateral organisations (such as USAID) funded 10 (8%), and the Government of India funded research that was published in 9 (7%) articles.
Discussion
Location
As expected, research proliferated in many of the states with the highest burden of maternal and child mortality, including the larger states, such as Bihar, Jharkhand, Madhya Pradesh, Odisha, Rajasthan, Uttar Pradesh and Chhattisgarh, and the smaller north-eastern states of Arunachal Pradesh, Assam and Manipur. Two large high-burden states did not feature in the published literature – Himachal Pradesh, where the ASHA programme started later, and Jammu and Kashmir, where security concerns likely hindered research. Many of the smaller states in north-eastern India (Meghalaya, Mizoram, Nagaland, Sikkim and Tripura) also did not feature, potentially due to lower interest from research donor organisations or access barriers. Several southern states with comparatively good maternal and child health indicators were also the sites of a number of studies (particularly Andhra Pradesh, Karnataka and Kerala), often featuring research on frontier areas for ASHAs, including mental health [110], cardiovascular disease [85, 125] and other non-communicable disease screening, prevention and management [122, 123]. While several studies that supported comparative research across several states were found, additional work of this nature would support generalisations for the national programme.
Health condition focus
Research on the routine programme tended to focus on maternal and child health, while the special interventions showcased a plethora of innovation, often emphasising special focus areas (HIV, childhood disability developmental delay, death tracking, abortion, contraceptives, uterine prolapse) that were beyond the initial purview of the ASHA programme. On the one hand, the proliferation of donor-funded pilot projects without a strong linkage to or consideration of the broader health system suggests a problematic allocation of resources to efforts unlikely to function at scale. In addition, publications that described using ASHAs merely as data collectors for other teams raise questions about coherence, permission and respecting ASHA time. On the other hand, some smaller scale studies, such as those focused on home-based newborn care, started as special interventions but were subsequently adopted into the routine programme.
Evaluation outcomes
While smaller scale special interventions were generally able to bring about positive outcomes, research on aspects of the routine ASHA programme more often showed mixed or negative outcomes. This indicates that, with significant inputs and resources, ASHAs can deliver positive results, but that these focused short-term engagements do not reflect the everyday operating reality of the large-scale routine programme. The routine programme grapples with the challenges of operating at scale and of integration with the resource-constrained government health system.
Both positive and negative outcomes associated with ASHAs at scale occurred in the context of the National Health Mission. Research findings from specific states have shown that ASHAs have been selected across most villages [145] according to recruitment norms [112], and have received most or all of their training [44, 54]. The majority have a reasonable grasp of core health concepts [41, 46, 76, 97, 104, 131, 136], are reasonably well known and trusted as a source of health information and referral in their communities [57, 62], and are providing a subset of households with health information and services [41, 44, 56, 58, 60, 75, 101, 140], particularly by encouraging antenatal care and institutional delivery [52, 55, 132] and childhood immunisation [116]. The ASHA programme at scale has been associated with improvements in neonatal health, some aspects of care-seeking, and increased immunisation and health-related awareness in certain areas [36, 86, 135, 141, 145, 156].
Negative research results from specific states identified ASHA knowledge gaps [36, 104, 105, 114, 119, 131], inadequacies in ASHA training or supervision [56, 57, 68, 93, 105, 109, 139, 146, 156], low community engagement with and awareness of ASHAs [134], challenges related to referrals (limited transportation, coordination and health facility resources) [55, 100, 111, 136, 140], dissatisfaction among ASHAs with their remuneration or support [9, 52, 53, 89, 102, 140], lack of supplies [54, 60, 89, 156], and subpar performance or coverage [41, 60, 65, 66, 75, 103, 112, 116, 145].
Chhattisgarh’s Mitanin programme emerged as a strong success story, wherein Mitanins performed as socio-political actors on the social determinants of health [126, 128, 130]. However, in other states, ASHAs have generally been more successful in performing a link-worker role, without significant action on community mobilisation or the social determinants of health [43, 44, 98, 100, 152].
Health systems perspective
The National Health Mission is a health system reform seeking to strengthen government service delivery through all the health system building blocks, including cross-cutting community engagement. However, health condition-focused research on the ASHA programme often took a narrow perspective, without accounting for the broader health system factors in which the programme operates. In comparison, studies on general ASHA work examined the programme in context and considered broader systemic or cross-cutting policy issues.
Health systems content
Many publications presented meaningful information on multiple topics in the CHW–health system framework (Fig. 1), reflecting that researchers frequently considered the ASHA programme within the broader health system context. However, a number of essential health system considerations, which are central to the programme’s vision, were rarely discussed in the published literature. In particular, there was little consideration of programme governance (programme oversight and guidance, CHW political support, the role of NGO actors in CHW policy, grievance redressal for CHWs, programme financing, and CHW programme reporting), community voice, community engagement in ASHA selection, and community collaboration with ASHAs through health committees. While many studies measured ASHA performance and knowledge, few discussed or used existing programme or health facility records, leaving the routine systems needed to monitor the programme unexplored. Additionally, while health outcomes associated with the ASHA programme or small-scale interventions engaging ASHAs were frequently assessed, social outcomes were rarely discussed. While the existing research on gender, motivation, ASHA agency, and relationships and linkages among different actors (auxiliary nurse midwives, Anganwadi workers, block and district managers) is welcome, far more research on these topics is required to truly understand the ASHA as an integrated member of the health system.
In the first decade of the programme, research assessing ASHA capacity and performance has played a valuable role in understanding early challenges and successes. However, as the ASHA programme enters its next decade, research on other aspects of the CHW–health system framework will be increasingly important to the programme’s capacity to adapt, sustain and achieve its broader goals around empowerment, community engagement and change across the social determinants of health. Future research should consider the upcoming challenges of running a mature CHW programme at scale, including recruitment and training for expanded roles in non-communicable diseases, ASHA social security, retention, aging, and ongoing knowledge retention and skills upgrade. Furthermore, echoing global gaps in research on CHW programmes [13], ongoing research is required on meeting the rights and needs of ASHAs, effective approaches to training and supervision, on realising the ASHA role as a community change agent, and on the influence of health system decentralisation, social accountability and governance.
Research typology and methodology
The academic literature on the ASHA programme showcases a rich range of research. It is noteworthy that research focusing directly on aspects of the ASHA programme itself tended to be descriptive and explanatory, while the more complex influence studies, including the randomised controlled trials, focused on broader health interventions, such as integrated management of childhood illness, with limited findings pertaining to ASHAs, who were just one of many providers.
The plethora of descriptive work offered important early feedback into the programme’s condition, including the extent to which it was implemented as intended and key issues of ASHA capacity and performance. However, as the programme moves forward into its next decade, policy-makers would benefit from stronger evidence on the programme’s impact on health and social outcomes, as well as on the optimal mechanisms for ASHA training, support and remuneration. Rigorous explanatory studies and health systems evaluations, such as mixed methods influence studies and realist evaluations, taking these areas of the ASHA programme as their focus, would enable increasingly evidence-informed policy-making, planning and advocacy. Furthermore, there is a need for emancipatory research that engages ASHAs as agents to identify and work towards addressing challenges, and predictive research that helps guide next steps. Ultimately, a complex, evolving and dynamic intervention such as the ASHA programme, which is implemented at scale as part of a larger system reform agenda, cannot be studied through a single research design. Research agendas at state and national levels are likely to be different and the various facets of the programme require different designs.
Authorship and funding
Indian authors and institutions have shown strong research leadership and critical engagement with the programme, and have also developed international partnerships to support complex research studies. The dominance of Indian authors, especially in critiques of the programme and research with negative and mixed findings, showcases a vibrant civil society space – and is a welcome contrast to other country contexts where critical research may be severely curtailed [157]. While the dominance of Indian-led academic work generates opportunities to disseminate and build upon the research findings in the same setting [158], there was repetition among descriptive studies and other areas of inquiry were largely neglected. Further engagement is needed between policy needs and research generation to ensure effective use of research investments.
The high percentage of papers that did not disclose their source of funding is concerning, as it could obscure power dynamics guiding research priority topics, regions and institutions. It is also noteworthy that research commissioned and funded by the government was largely absent from the published literature, although we note that this research may be conducted and disseminated internally or published in the grey literature. A mature CHW programme requires government leadership in funding research that addresses policy-maker needs, including large scale evaluations. Ensuring that this research is peer reviewed and published in journals will help to inform national and international conversations on CHWs.
Limitations
This overview of published literature on the ASHA programme has several limitations. We only considered published studies listed in prominent journal databases (PubMed, Scopus and Embase). We did not include the extensive grey literature published on the programme, including important NGO and government reports. While we also gathered and analysed all government documents in the public domain, the findings from that area of work are reported on elsewhere [11] and are beyond the scope of this paper.
Authorship, while classified as domestic, foreign and other, hides those of Indian origin based in foreign institutions, or who may have subsequently moved back to India. Some included articles significantly involved ASHAs in their studies but had limited findings relevant to the ASHA programme (e.g. studies that used ASHAs as data collectors to assess the prevalence of a health issue, but were not ultimately assessing or commenting on the ASHA role or capacity). Other studies did not disaggregate ASHAs from other frontline health workers.
We did not assess the methodological quality of the included articles because there was such a wide range of research typologies used. This limits our ability to comment on the strength of research being done and on how trustworthy, robust, and meaningful these academic contributions are. The wide range in complexity, insight, and rigor across the included manuscripts is not analysed in this paper.
Conclusion
Academic work on the ASHA programme highlights a range of special interventions, but also showcases the challenges faced by a programme at massive scale, situated in the broader health system. As the programme continues to evolve, ongoing research and continued domestic critical leadership is vital to address key knowledge gaps and provide insight into ground realities, including on programme governance, intersectoral linkages, ASHA solidarity, and community capacity to provide support and oversight.
Additional files
Search terms on the ASHA community health worker programme. (DOCX 18 kb)
Reference list of all included articles. (DOCX 31 kb)
Database of included articles and their characteristics. (XLSX 73 kb)
Summary of research on the main ASHA programme. (DOCX 71 kb)
Summary of smaller scale interventions that engaged ASHAs. (DOCX 44 kb)
Research on ASHAs, by typology and methodology. (DOCX 133 kb)
Acknowledgements
Not applicable.
Funding
Asha George is supported by Health Systems Extra-Mural Unit funded by the South African Medical Research Council and the South African Research Chair's Initiative of the Department of Science and Technology and National Research Foundation of South Africa (Grant No 82769). Any opinion, finding and conclusion or recommendation expressed in this material is that of the author and the National Research Foundation does not accept any liability in this regard.
This research was made possible in part by the generous support of the American people through the United States Agency for International Development (USAID), under the terms of the Cooperative Agreement AID-OAA-A-14-00028. The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government. The National Health Systems Resource Centre, New Delhi, India, provided in kind funding support.
Availability of data and materials
The datasets generated during this study are included in this published article (Additional files 2, 3, 4, 5 and 6).
Abbreviations
- ASHA
Accredited social health activist
- CHW
Community health worker
- HIV
Human immunodeficiency virus
Authors’ contributions
ASG, KS and RRV conceptualised the study. KS conducted the literature searches, article screening and data extraction. KS and ASG analysed the data and drafted the manuscript. RRV provided critical guidance and feedback throughout the process. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
KS and ASG declare that they have no competing interests. RV is executive director of the National Health Systems Resource Centre, which provides technical assistance to the National Health Mission within the Indian Ministry of Health and Family Welfare, including on the ASHA programme.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Chandigarh, Dadra and Nagar Haveli, Daman and Diu, Lakshadweep, Puducherry, Andaman and Nicobar Islands.
Contributor Information
Kerry Scott, Email: kscott26@jhu.edu.
Asha S. George, Email: asgeorge@uwc.ac.za
Rajani R. Ved, Email: rajani.ved@gmail.com
References
- 1.World Health Organization . Global Strategy on Human Resources for Health Workforce 2030. Draft for the 69th World Health Assembly. Geneva: WHO; 2016. [Google Scholar]
- 2.Tulenko K, Møgedal S, Afzal MM, Frymus D, Oshin A, Pate M, et al. Community health workers for universal health-care coverage: from fragmentation to synergy. Bull World Health Organ. 2013;91(11):847–852. doi: 10.2471/BLT.13.118745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schneider H, Okello D, Lehmann U. The global pendulum swing towards community health workers in low- and middle-income countries: a scoping review of trends, geographical distribution and programmatic orientations, 2005 to 2014. Hum Resour Health. 2016;14(1):65. doi: 10.1186/s12960-016-0163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naimoli JF, Perry HB, Townsend JW, Frymus DE, McCaffery JA. Strategic partnering to improve community health worker programming and performance: features of a community-health system integrated approach. Hum Resour Health. 2015;13(1):46. doi: 10.1186/s12960-015-0041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider H, Lehmann U. From community health workers to community health systems: time to widen the horizon? Health Syst Reform. 2016;2(2):112–118. doi: 10.1080/23288604.2016.1166307. [DOI] [PubMed] [Google Scholar]
- 6.Singh D, Negin J, Otim M, Orach CG, Cumming R. The effect of payment and incentives on motivation and focus of community health workers: five case studies from low- and middle-income countries. Hum Resour Health. 2015;13:58. doi: 10.1186/s12960-015-0051-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maes KC, Kohrt BA, Closser S. Culture, status and context in community health worker pay: Pitfalls and opportunities for policy research. A commentary on Glenton et al. (2010) Soc Sci Med. 2010;71(8):1375–1378. doi: 10.1016/j.socscimed.2010.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glenton C, Scheel IB, Pradhan S, Lewin S, Hodgins S. The female community health volunteer programme in Nepal: decision makers’ perceptions of volunteerism, payment and other incentives. Soc Sci Med. 2010;70(12):1920–1927. doi: 10.1016/j.socscimed.2010.02.034. [DOI] [PubMed] [Google Scholar]
- 9.Bhatia K. Community health worker programs in India: a rights-based review. Perspect Public Health. 2014;134(5):276–282. doi: 10.1177/1757913914543446. [DOI] [PubMed] [Google Scholar]
- 10.Kane S, Kok M, Ormel H, Otiso L, Sidat M, Namakhoma I, et al. Limits and opportunities to community health worker empowerment: A multi-country comparative study. Soc Sci Med. 2016;164:27–34. doi: 10.1016/j.socscimed.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 11.Ved R, Scott K, Gupta G, Ummer O, Singh S, Srivastava A, et al. How are gender inequalities facing India’s one million ASHAs being addressed? Policy origins and adaptations for the world’s largest all-female community health worker programme. Hum Resour Health. 2019;17(1):3. doi: 10.1186/s12960-018-0338-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schaaf M, Fox J, Topp S, Warthin C, Freedman LPLP, Robinson RSRS, et al. Community health workers and accountability: reflections from an international “think-in”. Int J Equity Health. 2018;17(66):1–5. doi: 10.1186/s12939-018-0781-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott K, Beckham S, Gross M, Pariyo G, Rao K, Cometto G, et al. What do we know about community-based health programs? A systematic review of existing reviews on community health workers and their integration with health systems. Hum Resour Health. 2018;16(1):39. doi: 10.1186/s12960-018-0304-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization, Global Health Workforce Alliance . Global Experience of Community Health Workers for Delivery of Health Related Millennium Development Goals. 2010. [Google Scholar]
- 15.Bosch-Capblanch X, Liaqat S, Garner P. Managerial supervision to improve primary health care in low- and middle-income countries. Cochrane Database Syst Rev. 2011;9:CD006413. doi: 10.1002/14651858.CD006413.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hill Z, Dumbaugh M, Benton L, Ka K, Strachan DL, Asbroek A, et al. Supervising communtiy health workers n low-income countries- a review of impact and implementation issues. Glob Health Action. 2014;7:1–10. doi: 10.3402/gha.v7.24085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jaskiewicz W, Tulenko K. Increasing community health worker productivity and effectiveness: a review of the influence of the work environment. Hum Resour Health. 2012;10(1):38. doi: 10.1186/1478-4491-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kok MC, Dieleman M, Taegtmeyer M, Broerse JEW, Kane S, Ormel H, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plan. 2015;30(9):1207–1227. doi: 10.1093/heapol/czu126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kok MC, Kane S, Tulloch O, Ormel H, Theobald S, Dieleman M, et al. How does context influence performance of community health workers in low- and middle-income countries? Evidence from the literature. Health Res Policy Syst. 2015;13(1):13. doi: 10.1186/s12961-015-0001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCollum R, Gomez W, Theobald S, Taegtmeyer M. How equitable are community health worker programmes and which programme features influence equity of community health worker services? A systematic review. BMC Public Health. 2016;16:419. doi: 10.1186/s12889-016-3043-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaughan K, Kok MC, Witter S, Dieleman M. Costs and cost-effectiveness of community health workers: evidence from a literature review. Hum Resour Health. 2015;13(1):71. doi: 10.1186/s12960-015-0070-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pallas SW, Minhas D, Pérez-Escamilla R, Taylor L, Curry L, Bradley EH, et al. Community health workers in low- and middle-income countries: what do we know about scaling up and sustainability? Am J Public Health. 2013;103(7):74–82. doi: 10.2105/AJPH.2012.301102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zulu JM, Kinsman J, Michelo C, Hurtig AK. Integrating national community-based health worker programmes into health systems: a systematic review identifying lessons learned from low- and middle-income countries. BMC Public Health. 2014;14(987):1–17. doi: 10.1186/1471-2458-14-987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giugliani C, Harzheim E, Duncan MS, Duncan BB. Effectiveness of community health workers in Brazil: a systematic review. J Ambul Care Manage. 2011;34(4):326–338. doi: 10.1097/JAC.0b013e31822cbdfd. [DOI] [PubMed] [Google Scholar]
- 25.Bornstein VJ, Stotz EN. Concepções que integram a formação e o processo de trabalho dos agentes comunitários de saúde: uma revisão da literatura. Cien Saude Colet. 2008;13(1):259–268. doi: 10.1590/s1413-81232008000100029. [DOI] [PubMed] [Google Scholar]
- 26.Pereira IC, Oliveira MAC. O trabalho do agente comunitário na promoção da saúde : revisão integrativa da literatura. Rev Bras Enferm. 2013;66(3):412–419. doi: 10.1590/s0034-71672013000300017. [DOI] [PubMed] [Google Scholar]
- 27.Baatiema L, Sumah AM, Tang PN, Ganle JK. Community health workers in Ghana: the need for greater policy attention. BMJ Glob Heal. 2016;1(4):e000141. doi: 10.1136/bmjgh-2016-000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ministry of Health and Family Welfare India. National Rural Health Mission (2005–2012): Mission Document. New Delhi: Government of India; 2005.
- 29.Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev. 2012;1(1):28. doi: 10.1186/2046-4053-1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.PubMed . PubMed Help. 2019. [Google Scholar]
- 31.Elsevier . Embase. 2019. [Google Scholar]
- 32.Scopus . What is Scopus? 2018. [Google Scholar]
- 33.Naimoli JF, Frymus DE, Wuliji T, Franco LM, Newsome MH. A community health worker “logic model”: towards a theory of enhanced performance in low- and middle-income countries. Hum Resour Health. 2014;12(1):56. doi: 10.1186/1478-4491-12-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Community Health Network. Hot Topics, Fresh Insights, and Ways Forward. Meeting Report. Washington, DC; 2011. https://coregroup.org/wp-content/uploads/media-backup/Meetings/Spring_Meeting_2011/CORE_Group_Spring_Meeting_2011_report_6_16_11_2.pdf. Accessed 9 Mar 2019.
- 35.George AS, Campbell J, Ghaffar A, HPSR HRH Reader Collaborators Advancing the science behind human resources for health: highlights from the Health Policy and Systems Research Reader on Human Resources for Health. Health Res Policy Syst. 2018;16(1):80. doi: 10.1186/s12961-018-0346-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Awasthi S, Nichter M, Verma T, Srivastava NM, Agarwal M, Singh JV, et al. Revisiting community case management of childhood pneumonia: Perceptions of caregivers and grass root health providers in Uttar Pradesh and Bihar, Northern India. PLoS One. 2015;10(4):1–19. doi: 10.1371/journal.pone.0123135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deshpande S, Bhanot A, Maknikar S. Assessing the influence of a 360-degree marketing communications campaign with 360-degree feedback. Soc Mar Q. 2015;21(3):142–151. [Google Scholar]
- 38.Kumar S, Roy R, Dutta S. Scaling-up public sector childhood diarrhea management program: Lessons from Indian states of Gujarat, Uttar Pradesh and Bihar. J Glob Health. 2015;5(2):020414. doi: 10.7189/jogh.05.020414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lamberti LM, Walker CLF, Taneja S, Mazumder S, Black RE. The association between provider practice and knowledge of ORS and zinc supplementation for the treatment of childhood diarrhea in Bihar, Gujarat and Uttar Pradesh, India: a multi-site cross-sectional study. PLoS One. 2015;10(6):1–17. doi: 10.1371/journal.pone.0130845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nordfeldt C, Roalkvam S. Choosing vaccination: negotiating child protection and good citizenship in modern India. Forum Dev Stud. 2010;37(3):327–347. [Google Scholar]
- 41.Persai D, Panda R, Mathur MR. Self-reported practices and attitudes of community health workers (accredited social health activist) in tobacco control - findings from two states in India. Int J Prev Med. 2015;6:48. doi: 10.4103/2008-7802.158177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rath SSSSS, Nair N, Tripathy PK, Barnett S, Rath SSSSS, Mahapatra R, et al. Explaining the impact of a women’s group led community mobilisation intervention on maternal and newborn health outcomes: the Ekjut trial process evaluation. BMC Int Health Hum Rights. 2010;10(1):25. doi: 10.1186/1472-698X-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Srivastava A, Gope R, Nair N, Rath S, Rath S, Sinha R, et al. Are village health sanitation and nutrition committees fulfilling their roles for decentralised health planning and action? A mixed methods study from rural eastern India. BMC Public Health. 2016;16(1):59. doi: 10.1186/s12889-016-2699-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sundararaman T, Ved R, Gupta G, Samatha M. Determinants of functionality and effectiveness of community health workers: results from evaluation of ASHA program in eight Indian states. BMC Proc. 2012;6(Suppl 5):O30. [Google Scholar]
- 45.Swaminathan P. The formal creation of informality, and therefore, gender injustice: Illustrations from India’s social sector. Indian J Labour Econ. 2015;58(1):23–42. [Google Scholar]
- 46.Thacker N, Choudhury P, Gargano LM, Weiss PS, Pazol K, Vashishtha VM, et al. Attitudes and practices of auxiliary nurse midwives and accredited social health activists in uttar pradesh and bihar regarding polio immunization in india. J Trop Pediatr. 2013;59(4):266–273. doi: 10.1093/tropej/fmt008. [DOI] [PubMed] [Google Scholar]
- 47.Tripathy P, Nair N, Sinha R, Rath S, Gope RK, Rath S, et al. Effect of participatory women’s groups facilitated by accredited social health activists on birth outcomes in rural eastern India: a cluster-randomised controlled trial. Lancet Glob Heal. 2016;4(2):e119–e128. doi: 10.1016/S2214-109X(15)00287-9. [DOI] [PubMed] [Google Scholar]
- 48.Verma C, Rao P. Determinants of rural women’s participation in india’s National Leprosy Eradication Programme. Indian J Lepr. 2014;86:105–110. [PubMed] [Google Scholar]
- 49.Das A, Friedman J, Kandpal E, Ramana GNV, Gupta RKD, Pradhan MM, et al. Strengthening malaria service delivery through supportive supervision and community mobilization in an endemic Indian setting: an evaluation of nested delivery models. Malar J. 2014;13(1):482. doi: 10.1186/1475-2875-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elazan SJ, Higgins-Steele AE, Fotso JC, Rosenthal MH, Rout D. reproductive, maternal, newborn, and child health in the community: task-sharing between male and female health workers in an Indian rural context. Indian J Community Med. 2016;41(1):34–38. doi: 10.4103/0970-0218.170963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fotso JC, Higgins-Steele A, Mohanty S. Male engagement as a strategy to improve utilization and community-based delivery of maternal, newborn and child health services: evidence from an intervention in Odisha, India. BMC Health Serv Res. 2015;15 Suppl 1(Suppl 1):S5. doi: 10.1186/1472-6963-15-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gopalan SS, Durairaj V. Addressing maternal healthcare through demand side financial incentives: experience of Janani Suraksha Yojana program in India. BMC Health Serv Res. 2012;12(1):319. doi: 10.1186/1472-6963-12-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gopalan SS, Mohanty S, Das A. Assessing community health workers’ performance motivation: a mixed-methods approach on India’s accredited social health activists (ASHA) programme. BMJ Open. 2012;2(5):e001557. doi: 10.1136/bmjopen-2012-001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hussain MA, Dandona L, Schellenberg D. Public health system readiness to treat malaria in Odisha State of India. Malar J. 2013;12(1):351. doi: 10.1186/1475-2875-12-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Malini S, Tripathi RM, Khattar P, Nair KS, Tekhre YL, Dhar N, et al. A Rapid Appraisal on Functioning of Janani Suraksha Yojana in South Orrisa. http://www.nihfw.org/pdf/RAHI-I%20Reports/Berhampur/Berhampur.pdf. Accessed 5 Mar 2019.
- 56.Mishra A. The role of the Accredited Social Health Activists in effective health care delivery: evidence from a study in South Orissa. BMC Proc. 2012;6(Suppl 1):P1. [Google Scholar]
- 57.Mishra A. ‘Trust and teamwork matter’: community health workers’ experiences in integrated service delivery in India. Glob Public Health. 2014;9(8):960–974. doi: 10.1080/17441692.2014.934877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mishra A, Kar K, Satapathy D. Mass drug administration against filariasis - a study on coverage and compliance, in a coastal district of Odisha. J Commun Dis. 2015;47(4):13–18. [Google Scholar]
- 59.Panigrahi S, Mohapatra B, Mishra K. Awareness, perception and practice of stakeholders in India regarding Village Health and Nutrition Day. J Fam Med Prim Care. 2015;4(2):244. doi: 10.4103/2249-4863.154663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sahu SS, Rao SP, Dash S. Performance of Accredited Social Health Activists (ASHAs) in diagnosis and treatment of Malaria in Eight Falciparum Endemic Tribal Districts of Southern Odisha, India. J Commun Dis. 2016;48(2):12–19. [Google Scholar]
- 61.Valadez JJ, Devkota B, Pradhan MM, Meherda P, Sonal GS, Dhariwal A, et al. Improving malaria treatment and prevention in India by aiding district managers to manage their programmes with local information: a trial assessing the impact of Lot Quality Assurance Sampling on programme outcomes. Tropical Med Int Health. 2014;19(10):1226–1236. doi: 10.1111/tmi.12354. [DOI] [PubMed] [Google Scholar]
- 62.Swain S, Swain P, Nair KS, Dhar N, Gupta S, Nandan D. A rapid appraisal of functioning of ASHA under NRHM in Orissa. Health Popul Perspect Issues. 2008;31(2):73–79. [Google Scholar]
- 63.Das E, Panwar DS, Fischer EA, Bora G, Carlough MC. Performance of accredited social health activists to provide home-based newborn care: a situational analysis. Indian Pediatr. 2014;51(2):142–144. doi: 10.1007/s13312-014-0349-4. [DOI] [PubMed] [Google Scholar]
- 64.DeRenzi B, Wacksman J, Dell N, Lee S, Lesh N, Borriello G, et al. Closing the feedback loop: a 12-month evaluation of ASTA, a self-tracking application for ASHAs. ICTD’16 Proceedings of the Eighth International Conference on Information and Communication Technologies and Development; 2016. Article 22. http://doi.acm.org/10.1145/2909609.2909652.
- 65.Kansal S, Kumar S, Kumar A. Is educational level of ASHA matters for their effective functioning? A cross- sectional study in eastern Uttar Pradesh. Indian J Community Heal. 2012;24(1):41–44. [Google Scholar]
- 66.Kumar S, Kaushik A, Kansal S. Factors influencing the work performance of ASHA under NRHM a cross sectional study from eastern Uttar Pradesh. Indian J Commun Health. 2012;24:325–331. [Google Scholar]
- 67.Sebastian MP, Khan ME, Kumari K, Idnani R. Increasing postpartum contraception in rural India: Evaluation of a community-based behavior change communication intervention. Int Perspect Sex Reprod Health. 2012;38(2):68–77. doi: 10.1363/3806812. [DOI] [PubMed] [Google Scholar]
- 68.Shrivastava A, Srivastava A. Measuring communication competence and effectiveness of ASHAs (accredited social health activist) in their leadership role at rural settings of Uttar Pradesh (India) Leadersh Health Serv. 2016;29(1):69–81. doi: 10.1108/LHS-12-2014-0079. [DOI] [PubMed] [Google Scholar]
- 69.Srivastava D, Prakash S, Ashish V, Nair K, Gupta S, Nandan D. A study of interface of ASHA with the community and the service providers in eastern Uttar Pradesh. Indian J Public Health. 2009;53(3):133. [PubMed] [Google Scholar]
- 70.Vashistha A, Kumar N, Mishra A, Anderson R. Mobile Video Dissemination for Community Health. ICTD’16 Proceedings of the Eighth International Conference on Information and Communication Technologies and Development. 2016. p. Article 20. [Google Scholar]
- 71.Panwar DS, Naidu V, Das E, Verma S, Khan AA. Strengthening support mechanisms for Accredited Social Health Activists in order to improve home-based newborn care in Uttar Pradesh, India. BMC Proc. 2012;6(Suppl 5):O33. [Google Scholar]
- 72.Das VNR, Pandey RN, Pandey K, Singh V, Kumar V, Matlashewski G, et al. Impact of ASHA training on active case detection of visceral leishmaniasis in Bihar, India. PLoS Negl Trop Dis. 2014;8(5):1–5. doi: 10.1371/journal.pntd.0002774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Das VNR, Pandey RN, Kumar V, Pandey K, Siddiqui NA, Verma RB, et al. Repeated training of accredited social health activists (ASHAs) for improved detection of visceral leishmaniasis cases in Bihar, India. Pathog Glob Health. 2016;110(1):33–35. doi: 10.1080/20477724.2016.1156902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kaphle S, Chaturvedi S, Chaudhuri I, Krishnan R, Lesh N. Adoption and usage of mHealth technology on quality and experience of care provided by frontline workers: observations from rural India. JMIR mHealth uHealth. 2015;3(2):e61. doi: 10.2196/mhealth.4047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kosec K, Avula R, Holtemeyer B, Tyagi P, Hausladen S, Menon P. Predictors of essential health and nutrition service delivery in Bihar, India: results from household and frontline worker surveys. Glob Heal Sci Pract. 2015;3(2):255–273. doi: 10.9745/GHSP-D-14-00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Malaviya P, Hasker E, Singh RP, Van Geertruyden JP, Boelaert M, Sundar S. Village health workers in Bihar, India: an untapped resource in the struggle against kala-azar. Trop Med Int Health. 2013;18(2):188–193. doi: 10.1111/tmi.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tiwari SN, Pandey SC, Chandra U. Disability control by self-care at home in Bihar. Indian J Lepr. 2012;84:108. [Google Scholar]
- 78.Jonnalagada S, Rao K, Chary R, M S, Rao R. A focused approach to detect leprosy in high burden tribal mandals of Adilabad district, Andhra Pradesh, India. Indian J Leprosy. 2012;84:87.
- 79.Nyamathi A. Engaging community health workers in HIV/AIDS care: a case exemplar among rural Indian women living with AIDS. J HIV AIDS Soc Serv. 2014;13(4):330–336. [Google Scholar]
- 80.Nyamathi A, Hanson AY, Salem BE, Sinha S, Ganguly KK, Leake B, et al. Impact of a rural village women (ASHA) intervention on adherence to antiretroviral therapy in southern India. Nurs Res. 2012;61(5):353–362. doi: 10.1097/NNR.0b013e31825fe3ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nyamathi A, Salem B, Meyer V, Ganguly K, Sinha S, Ramakrishnan P. Impact of an ASHA intervention on depressive symptoms among rural women living with AIDS in India: comparison of the ASHA life and usual care program. AIDS Educ Prev. 2013;24(3):280–293. doi: 10.1521/aeap.2012.24.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nyamathi A, Ekstrand M, Salem BE, Sinha S, Ganguly KK, Leake B. Impact of ASHA intervention on stigma among rural Indian women with AIDS. West J Nurs Res. 2013;35(7):867–883. doi: 10.1177/0193945913482050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nyamathi A, Sinha S, Ganguly KK, Ramakrishna P, Suresh P, Carpenter CL. Impact of protein supplementation and care and support on body composition and CD4 count among HIV-infected women living in rural India: Results from a randomized pilot clinical trial. AIDS Behav. 2013;17(6):2011–2021. doi: 10.1007/s10461-013-0420-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Parveen K. Performance Evaluation of Community Health Workers during CCSP Training Programme. Indian J Public Health Res Dev. 2016;7(1):91–94. [Google Scholar]
- 85.Praveen D, Patel A, Raghu A, Clifford GD, Maulik PK, Mohammad Abdul A, et al. SMARTHealth India: development and field evaluation of a mobile clinical decision support system for cardiovascular diseases in rural India. JMIR mHealth uHealth. 2014;2(4):e54. doi: 10.2196/mhealth.3568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bhandari N, Mazumder S, Taneja S, Sommerfelt H, Strand TA, IMNCI Evaluation Study Group Effect of implementation of Integrated Management of Neonatal and Childhood Illness (IMNCI) programme on neonatal and infant mortality: cluster randomised controlled trial. BMJ. 2012;344:1634. doi: 10.1136/bmj.e1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Goel S, Gupta P, Aggarwal AK, Patro BK, Kaur J, Aggarwal N. Evaluation of Nischay scheme in improving antenatal care in a northern state of India. Arch Gynecol Obstet. 2013;288(4):815–819. doi: 10.1007/s00404-013-2795-y. [DOI] [PubMed] [Google Scholar]
- 88.Mazumder S, Taneja S, Bahl R, Mohan P, Strand TA, Sommerfelt H, et al. Effect of implementation of integrated management of neonatal and childhood illness programme on treatment seeking practices for morbidities in infants: cluster randomised trial. BMJ. 2014;349:g4988. doi: 10.1136/bmj.g4988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pala S, Kumar D, Jeyashree K, Singh A. Preliminary evaluation of the ASHA scheme in Naraingarh block, Haryana. Natl Med J India. 2011;24(5):315–316. [PubMed] [Google Scholar]
- 90.Prinja S, Mazumder S, Taneja S, Bahuguna P, Bhandari N, Mohan P, et al. Cost of delivering child health care through community level health workers: how much extra does IMNCI program cost? J Trop Pediatr. 2013;59(6):489–495. doi: 10.1093/tropej/fmt057. [DOI] [PubMed] [Google Scholar]
- 91.Salve HR, Babu S, Rai SK, Sagar R, Kant S. Attitude about mental illness of health care providers and community leaders in rural. Indian J Commun Helth. 2014;26(4):374–378. [Google Scholar]
- 92.Silan V, Kant S, Archana S, Misra P, Rizwan SA. Determinants of underutilisation of free delivery services in an area with high institutional delivery rate: a qualitative study. N Am J Med Sci. 2014;6(7):315–320. doi: 10.4103/1947-2714.136906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sinha LN, Kaur P, Gupta R, Dalpath S, Goyal V, Murhekar M. Newborn care practices and home-based postnatal newborn care programme - Mewat, Haryana, India, 2013. J WPSAR. 2014;5(3). 10.5365/wpsar.2014.5.1.006. [DOI] [PMC free article] [PubMed]
- 94.Stalin P, Krishnan A, Rai SK, Agarwal RK. ASHA’s involvement in newborn care: a feasibility study. Indian Pediatr. 2011;48(11):897–899. doi: 10.1007/s13312-011-0138-2. [DOI] [PubMed] [Google Scholar]
- 95.Bijalwan RP, Bhagavatula M, Semwal VD, Rawat P, Anand V. Morbidity of uterine prolapsed among the women in the Chakrata block of Dehradun District. Indian J Community Heal. 2015;27(1):103–109. [Google Scholar]
- 96.Pandey J, Singh M. Donning the mask: effects of emotional labour strategies on burnout and job satisfaction in community healthcare. Health Policy Plan. 2016;31(5):551–562. doi: 10.1093/heapol/czv102. [DOI] [PubMed] [Google Scholar]
- 97.Saxena V, Kumari R. Infant and young child feeding - knowledge and practices of ASHA workers of Doiwala block, Dehradun District. Indian J Community Health. 2014;26(1):68–75. [Google Scholar]
- 98.Saxena V, Kakkar R, Semwal VD. A study on ASHA - a change agent of the society. Indian J Community Health. 2012;24(1):15–18. [Google Scholar]
- 99.Saxena V, Kumari R, Kumar P, Nath B, Pal R. Planning and preparation of VHND through convergence: sharing experiences from Uttarakhand. Clin Epidemiol Glob Health. 2015;3(3):125–131. doi: 10.1016/j.cegh.2014.11.001. [DOI] [Google Scholar]
- 100.Scott K, Shanker S. Tying their hands? Institutional obstacles to the success of the ASHA community health worker programme in rural north India. AIDS Care. 2010;22 Suppl 2(931159996):1606–1612. doi: 10.1080/09540121.2010.507751. [DOI] [PubMed] [Google Scholar]
- 101.Shukla A, Bhatnagar T. Accredited Social Health Activists and pregnancy related services in Uttarakhand, India. BMC Proc. 2012;6(Suppl 1):P4. [Google Scholar]
- 102.Bhatia K. Performance based incentives of the ASHA Scheme: Stakeholders’ Perspectives. Econ Polit Wkly. 2014;49(22):145. [Google Scholar]
- 103.Joshi S, George M. Healthcare through community participation: role of ASHA. Econ Polit Wkly. 2012;47(10):70–76. [Google Scholar]
- 104.Sagare SM, Bogam RR, Murarkarsujata SK, Patil UP, Ghate MM. Knowledge, attitude and practices of ASHAs regarding tuberculosis and DOTS. Indian J Sci Technol. 2012;5(3):2401–2404. [Google Scholar]
- 105.Shrivastava SR, Shrivastava PS. Evaluation of trained Accredited Social Health Activist (ASHA) workers regarding their knowledge, attitude and practices about child health. Rural Remote Health. 2012;12(4):1–7. [PubMed] [Google Scholar]
- 106.Thakre SS, Thakre SB, Thakre AD, Golawar SH, More SM, Humne AY. Effectiveness of the training course of ASHA on infant feeding practices at a rural teaching hospital: a cross sectional study. J Clin Diagnostic Res. 2012;6(6):1038–1040. [Google Scholar]
- 107.Johnston HB, Ganatra B, Nguyen MH, Habib N, Afework MF, Harries J, et al. Accuracy of assessment of eligibility for early medical abortion by community health workers in Ethiopia, India and South Africa. PLoS One. 2016;11(1):e0146305. doi: 10.1371/journal.pone.0146305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Roalkvam S. Health governance in India: citizenship as situated practice. Glob Public Health. 2014;9(8):910–926. doi: 10.1080/17441692.2014.941900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sharma R, Webster P, Bhattacharyya S. Factors affecting the performance of community health workers in India: a multi-stakeholder perspective. Glob Health Action. 2014;7(1):1–8. doi: 10.3402/gha.v7.25352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Armstrong G, Kermode M, Raja S, Suja S, Chandra P, Jorm A. A mental health training program for community health workers in India: impact on knowledge and attitudes. Int J Ment Health Syst. 2011;5(17):1–11. doi: 10.1186/1752-4458-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Engel N, Ganesh G, Patil M, Yellappa V, Pai NP, Vadnais C, et al. Barriers to point-of-care testing in India: results from qualitative research across different settings, users and major diseases. PLoS One 2015;10(8):e0135112. doi: 10.1371/journal.pone.0135112 [DOI] [PMC free article] [PubMed]
- 112.Fathima FN, Raju M, Varadharajan KS, Krishnamurthy A, Ananthkumar SR, Mony PK. Assessment of “Accredited Social Health Activists” -- a national community health volunteer scheme in Karnataka State, India. J Health Popul Nutr. 2015;33(1):137–145. [PMC free article] [PubMed] [Google Scholar]
- 113.Raju M. Validating infant and maternal mortality reporting in Doddaballapur Taluk of Bangalore Rural District – a pilot study. BMC Proc. 2012;6(Suppl 5):O23. [Google Scholar]
- 114.Ramadurg U, Vidler M, Charanthimath U, Katageri G, Bellad M, Mallapur A, et al. Community health worker knowledge and management of pre-eclampsia in rural Karnataka State, India. Reprod Health. 2016;13(Suppl 2):113. doi: 10.1186/s12978-016-0219-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Shashikala N, Kulkarni P, Renuka M, Sunil D. Strategising the educational interventional methods on infant feeding practices: an exploratory study among primary care workers in rural Mysore. Indian J Public Health Res Devel. 2016;7(3):165–170. [Google Scholar]
- 116.Mony P, Raju M. Evaluation of ASHA programme in Karnataka under the National Rural Health Mission. BMC Proc. 2012;6(Suppl 5):P12. [Google Scholar]
- 117.Gogoi A, Parmar S, Katoch M, Ziauddin M. Addressing the reproductive health needs and rights of married adolescent couples. 14th Congr Eur Soc Contracept Reprod Health. 2016;A–075:80.
- 118.Singh R. Community outreach to improve medical abortion access in India. Int J Gynecol Obstet. 2009;107:S77. [Google Scholar]
- 119.Bansal SC, Nimbalkar SM, Shah NA, Shrivastav RS, Phatak AG. Evaluation of knowledge and skills of home based newborn care among Accredited Social Health Activists (ASHA) Indian Pediatr. 2016;53(8):689–691. doi: 10.1007/s13312-016-0911-3. [DOI] [PubMed] [Google Scholar]
- 120.Modi D, Patel J, Desai S, Shah P. Accessing completeness of pregnancy, delivery, and death registration by Accredited Social Health Activists [ASHA] in an innovative mHealth project in the tribal areas of Gujarat: a cross-sectional study. J Postgrad Med. 2016;62(3):170–172. doi: 10.4103/0022-3859.183168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Modi D, Gopalan R, Shah S, Venkatraman S, Desai G, Desai S, et al. Development and formative evaluation of an innovative mHealth intervention for improving coverage of community-based maternal, newborn and child health services in rural areas of India. Glob Health Action. 2015;8(1):26769. doi: 10.3402/gha.v8.26769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jose R, Pisharady R, Benny PV, Nujum ZT, Rema Devi S, Varghese S, et al. Evaluation of non communicable disease control pilot programme of National Rural Health Mission in Thiruvananthapuram district. Clin Epidemiol Glob Health. 2015;3(1):17–23. doi: 10.1016/j.cegh.2013.08.004.. [DOI] [Google Scholar]
- 123.Menon J, Joseph J, Thachil A, Attacheril TV, Banerjee A. Surveillance of noncommunicable diseases by community health workers in Kerala: The Epidemiology of Noncommunicable Diseases in Rural Areas (ENDIRA) study. Glob Heart. 2014;9(4):409–417. doi: 10.1016/j.gheart.2014.07.003.. [DOI] [PubMed] [Google Scholar]
- 124.Nair MKC, Princly P, Leena ML, Swapna S, Kumari IL, Preethi R, et al. CDC Kerala 17: early detection of developmental delay / disability among children below 3 y in Kerala - a cross sectional survey. Indian J Pediatr. 2014;81(2):156–160. doi: 10.1007/s12098-014-1579-0. [DOI] [PubMed] [Google Scholar]
- 125.Smith R, Menon J, Rajeev JG, Feinberg L, Kumar RK, Banerjee A. Potential for the use of mHealth in the management of cardiovascular disease in Kerala: a qualitative study. BMJ Open. 2015;5(11):e009367. doi: 10.1136/bmjopen-2015-009367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Nandi S, Schneider H. Addressing the social determinants of health: a case study from the Mitanin (community health worker) programme in India. Health Policy Plan. 2014;29:ii71–ii81. doi: 10.1093/heapol/czu074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Som M. Volunteerism to incentivisation: changing priorities of Mitanins work in Chhattisgarh. Indian J Gend Stud. 2016;23(1):26–42. [Google Scholar]
- 128.Sundararaman T. Community health-workers: scaling up programmes. Lancet. 2007;369(9579):2058–2059. doi: 10.1016/S0140-6736(07)60326-2. [DOI] [PubMed] [Google Scholar]
- 129.Vir SC, Kalita A, Mondal S, Malik R. Impact of community-based mitanin programme on undernutrition in rural Chhattisgarh State, India. Food Nutr Bull. 2014;35(1):83–91. doi: 10.1177/156482651403500110. [DOI] [PubMed] [Google Scholar]
- 130.Nambiar D, Sheikh K, Verma N. Scale-up of community action for health: lessons from a realistic evaluation of the Mitanin program in Chhattisgarh, India. BMC Proc. 2012;6(Suppl 5):O26. [Google Scholar]
- 131.Kori S, Bhatia M, Mishra A. A cross-sectional assessment of knowledge of ASHA workers. J Krishna Inst Med Sci Univ. 2015;4(4):57–63. [Google Scholar]
- 132.Sidney K, Tolhurst R, Jehan K, Diwan V, De Costa A. “The money is important but all women anyway go to hospital for childbirth nowadays” - a qualitative exploration of why women participate in a conditional cash transfer program to promote institutional deliveries in Madhya Pradesh, India. BMC Pregnancy Childbirth. 2016;16(1):47. doi: 10.1186/s12884-016-0834-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sidney K, Diwan V, El-Khatib Z, de Costa A. India’s JSY cash transfer program for maternal health: Who participates and who doesn’t - a report from Ujjain district. Reprod Health. 2012;9(1):2. doi: 10.1186/1742-4755-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Balasubramaniam SS, Sarojini N, Khanna R. An investigation of maternal deaths following public protests in a tribal district of Madhya Pradesh, central India. Reprod Health Matters. 2012;20(39):11–20. doi: 10.1016/S0968-8080(12)39599-2. [DOI] [PubMed] [Google Scholar]
- 135.Bhargavi CN, Sharma A. MCH services in Delhi in terms of beneficiaries’ awareness, coverage and satisfaction. Nurs J India. 2014;105(4):186–190. [PubMed] [Google Scholar]
- 136.Kohli C, Kishore J, Sharma S, Nayak H. Knowledge and practice of Accredited Social Health Activists for maternal healthcare delivery in Delhi. J Fam Med Prim Care. 2015;4(3):359–363. doi: 10.4103/2249-4863.161317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Vikram K, Sharma AK, Kannan AT. Beneficiary level factors influencing Janani Suraksha Yojana utilization in urban slum population of trans-Yamuna area of Delhi. Indian J Med Res. 2013;138(SEP):340–346. [PMC free article] [PubMed] [Google Scholar]
- 138.Mahanta TG, Islam S, Sudke AK, Kumari V, Gogoi P, Rane T, et al. Effectiveness of introducing home-based newborn care (HBNC) voucher system in Golaghat District of Assam. Clin Epidemiol Glob Heal. 2016;4(2):69–75. [Google Scholar]
- 139.Prasad H. Evaluation of malaria control programme in three selected districts of Assam, India. J Vector Borne Dis. 2009;46(4):280–287. [PubMed] [Google Scholar]
- 140.Saprii L, Richards E, Kokho P, Theobald S, Greenspan J, McMahon S, et al. Community health workers in rural India: analysing the opportunities and challenges Accredited Social Health Activists (ASHAs) face in realising their multiple roles. Hum Resour Health. 2015;13(1):95. doi: 10.1186/s12960-015-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Padda P, Devgun S, Gupta V, Chaudhari S, Singh G. Role of ASHA in improvement of maternal health status in northern India: An urban rural comparison. Indian J Community Heal. 2013;25(4):465–471. [Google Scholar]
- 142.Kapil U. National rural health mission: training of health functionaries. Indian J Pediatr. 2006;73:248. doi: 10.1007/BF02825494. [DOI] [PubMed] [Google Scholar]
- 143.Nandan D. National Rural Health Mission -- rhetoric or reality. Indian J Public Health. 2005;49(3):168–170. [PubMed] [Google Scholar]
- 144.Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, et al. Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. 2010;375(9721):1182–1192. doi: 10.1016/S0140-6736(09)62042-0. [DOI] [PubMed] [Google Scholar]
- 145.Wagner AL, Bettampadi D, Porth JM, Boulton ML. The impact of increased use of ASHAs on rural immunization coverage in India. 17th Int Congr Infect Dis [Poster] 2016;45:209–210. doi: 10.1016/j.ijid.2016.02.478. [DOI] [Google Scholar]
- 146.Dixit A, Khan ME, Bhatnagar I. Mainstreaming of emergency contraception pill in India: challenges and opportunities. Indian J Commun Med. 2015;40(1):49–55. doi: 10.4103/0970-0218.149271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Eble A. Child mortality in rural India: how the ASHA program works, and how it might fail. In: Miklian J, Kolas A, editors. India’s Human Security: Lost Debates, Forgotten People, Intractable Challenges. Oxon: Routledge; 2014. pp. 168–183. [Google Scholar]
- 148.Patel AR, Nowalk MP. Expanding immunization coverage in rural India: a review of evidence for the role of community health workers. Vaccine. 2010;28(3):604–613. doi: 10.1016/j.vaccine.2009.10.108. [DOI] [PubMed] [Google Scholar]
- 149.Liu A, Sullivan S, Khan M, Sachs S, Singh P, Lui A, et al. Community health workers in global health: scale and scalability. Mt Sinai J Med. 2011;78(3):419–435. doi: 10.1002/msj.20260. [DOI] [PubMed] [Google Scholar]
- 150.Paul VK. Newborn healthcare in India: the road ahead. J Neonatol. 2009;23(3):191–198. [Google Scholar]
- 151.Ray SK. National rural health mission -- opportunity for Indian Public Health Association. Indian J Public Health. 2005;49(3):171–174. [PubMed] [Google Scholar]
- 152.Bajpai V, Saraya A. NRHM - The panacea for rural health in India: a critique. Indian J Public Heal Res Dev. 2013;4(1):241–244. [Google Scholar]
- 153.Mudur G. India launches national rural health mission. BMJ. 2005;330(7497):920. doi: 10.1136/bmj.330.7497.920-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Shukla A. National rural health mission--hope or disappointment? Indian J Public Health. 2005;49(3):127–132. [PubMed] [Google Scholar]
- 155.Taneja DK. National Rural Health Mission - a critical review. Indian J Public Health. 2005;49(3):152–155. [PubMed] [Google Scholar]
- 156.Mohan P, Kishore B, Singh S, Bahl R, Puri A, Kumar R. Assessment of implementation of integrated management of neonatal and childhood illness in India. J Heal Popul Nutr. 2011;29(6):629–638. doi: 10.3329/jhpn.v29i6.9900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Østebø MT, Cogburn MD, Mandani AS. The silencing of political context in health research in Ethiopia: why it should be a concern. Health Policy Plan. 2018;33:258–270. doi: 10.1093/heapol/czx150. [DOI] [PubMed] [Google Scholar]
- 158.Chersich MF, Blaauw D, Dumbaugh M, Penn-kekana L, Dhana A, Thwala S, et al. Local and foreign authorship of maternal health interventional research in low- and middle-income countries : systematic mapping of publications 2000–2012. Global Health 2016;12(1):35. doi: 10.1186/s12992-016-0172-x [DOI] [PMC free article] [PubMed]
- 159.Singh N. To evaluate the role of training session on ‘Cervical Cancer Screening’ in improving knowledge and attitude of Accredited Social Health Activists (ASHA) in North Indian population. Ann Oncol. 2015;26(Supplement 9):ix80–ix84. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search terms on the ASHA community health worker programme. (DOCX 18 kb)
Reference list of all included articles. (DOCX 31 kb)
Database of included articles and their characteristics. (XLSX 73 kb)
Summary of research on the main ASHA programme. (DOCX 71 kb)
Summary of smaller scale interventions that engaged ASHAs. (DOCX 44 kb)
Research on ASHAs, by typology and methodology. (DOCX 133 kb)
Data Availability Statement
The datasets generated during this study are included in this published article (Additional files 2, 3, 4, 5 and 6).