Abstract
Until recently, WHO operationally defined unsafe abortion as illegal abortion. In the past decade, however, the incidence of abortion by misoprostol administration has increased in countries with restrictive abortion laws. Access to safe surgical abortions has also increased in many such countries. An important effect of these trends has been that, even in an illegal environment, abortion is becoming safer, and an updated system for classifying abortion in accordance with safety is needed. Numerous factors aside from abortion method or legality should be taken into consideration in developing such a classification system. An Expert Meeting on the Definition and Measurement of Unsafe Abortion was convened in London, UK, on January 9–10, 2014, to move toward developing a classification system that both reflects current conditions and acknowledges the gradient of risk associated with abortion. The experts also discussed the types of research needed to monitor the incidence of abortion at each level of safety. These efforts are urgently needed if we are to ensure that preventing unsafe abortion is appropriately represented on the global public health agenda. Such a classification system would also motivate investment in research to accurately measure and monitor abortion incidence across categories of safety.
Keywords: Illegal abortion, Induced abortion incidence, Unsafe abortion, Misoprostol
1. Background
Unsafe abortions are defined by WHO as those performed either by individuals lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both [1]. In practice, global estimates of the incidence of unsafe abortion, developed periodically from the early 1990s until 2008, have largely comprised procedures done in countries with restrictive abortion laws and those performed outside the bounds of the law in countries with liberal laws. Thus, unsafe abortion was operationally defined as illegal abortion [2].
This approach was perhaps justified when this definition was developed. Since then, however, access to misoprostol, which can be used with or without mifepristone to medically induce an abortion, has increased in many countries, including those with restrictive abortion laws [3]. The number of providers trained in manual vacuum aspiration—a recommended procedure both for early surgical abortion and for treatment of incomplete and missed abortion—has also increased substantially in countries with restrictive abortion laws [4]. An important effect of these trends has been that abortion is becoming safer even in illegal environments.
Against this backdrop, an Expert Meeting on the Definition and Measurement of Unsafe Abortion was convened in London, UK, on January 9–10, 2014, to examine the prevailing conceptual and operational definitions of unsafe abortion and move toward developing definitions in line with current conditions [5]. In addition, in early 2014, Ganatra et al. [6] from WHO issued an editorial in which they clarified the conceptualization and interpretation of the WHO definition of unsafe abortion and proposed that the safety of abortion should be characterized along a continuum of risk rather than as a binary measure; they discussed many factors that merit consideration for inclusion in an operational definition of unsafe abortion, including whether the abortion is performed in accordance with WHO guidelines and broader contextual factors such as the social and legal setting in which an abortion takes place.
Here, we build on this discussion by describing insights from the Expert Meeting regarding both factors to consider in developing a new measure of unsafe abortion and the broad areas of research that would be needed to estimate the incidence of abortion across categories of safety.
2. Operationally defining unsafe abortion
There was much discussion at the meeting about whether the operational definition of unsafe abortion should focus on the circumstances under which an abortion is obtained or the outcome of the procedure. In essence, a classification system that focuses on only one of these considerations would be incomplete.
An outcomes-based definition, such as one that identifies unsafe abortions as those that result in complications or death, might be more straightforward because such abortions are easier to identify and document. But not all abortions performed under unsafe conditions will put the woman's physical health at risk or lead to complications. If unsafe abortions comprise only those procedures that lead to physical complications, the incidence of unsafe abortion will be underestimated.
A process-based definition, such as one that identifies unsafe abortions as those that are not done in accordance with WHO guidelines [7], implicitly encompasses information on likely outcomes, because it is grounded in evidence that certain types of abortion are associated with a higher risk of poor outcomes. But a process-based definition alone would not account for the fact that there is a spectrum of risk associated with procedures that do not comply with guidelines; among these, procedures that lead to complications might be considered more unsafe than those that are done without complication.
A reasonable approach, therefore, would be to consider all abortions that do not comply with WHO guidelines as unsafe, and to further differentiate unsafe abortions according to their outcome. It should also be recognized that complications can range from mild (e.g. prolonged mild bleeding) to severe (e.g. sepsis or damage to internal organs). Abortions that result in severe complications or death would be the most unsafe procedures.
All medical procedures carry some risk but, when performed under proper conditions by skilled providers using correct medical techniques and drugs, induced abortion presents minimal risk to a woman's physical health [8]. The meeting participants noted, however, that procedures performed in accordance with recommended guidelines can carry additional risks (including nonmedical risks) when they are highly restricted by law or highly stigmatized. In such contexts, women might delay seeking care and obtain abortion at a fairly late stage and under stressful conditions, thereby increasing the risk of physical or psychological complications. Furthermore, they might not receive information or counseling, including family planning counseling; and the quality of a woman's relationships and the strength of her social support network might be compromised either because she shared the fact of her abortion or because she refrained from sharing it with loved ones. Thus, a gradient of safety exists even among abortions that comply with guidelines.
The use of medical abortion is an important and new consideration with respect to the classification of abortions that are not done in accordance with guidelines. Medical abortions using misoprostol with or without mifepristone, even in low-resource settings and in countries with restrictive abortion laws, seem to pose few health risks when used correctly [9]. The use of medical abortion—obtained through various channels—has increased substantially in the past decade and has been implicated as a cause of the decline in severe abortion-related morbidity and mortality [10]. Some women who use misoprostol could experience mild complications, including incomplete abortion or prolonged bleeding, if they do not use the method correctly, and others could seek follow-up care even in the absence of a complication because they do not have accurate information on what to expect, including the possible duration of bleeding. A classification system should account for the incidence of such abortions and the types of outcome that are associated with them.
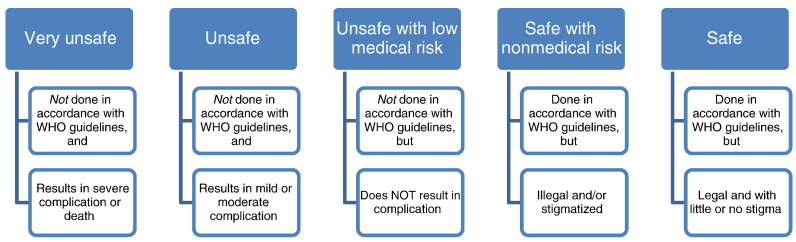
Overall, a classification system would ideally incorporate the multiple factors that influence the safety of abortion: namely, the social and legal context in which the abortion takes place, the qualifications of the person performing the abortion, the method used, and indicators such as the presence or absence of complications and the severity of complications if they do occur. A purely illustrative example of such a system is presented in Fig. 1. In this framework, procedurally safe abortions that are done in an environment where abortions are largely illegal or stigmatized are distinguished from safe abortions done in the context of liberal abortion laws and little or no abortion stigma. Unsafe abortions are defined as those that do not comply with WHO recommended guidelines, and are further divided into those that do not lead to complications, those that lead to mild or moderate complications, and those that lead to severe complications (including the woman's death). Additional refinements to this framework might further differentiate unsafe abortions according to whether they take place in settings with restrictive abortion laws or where abortion is highly stigmatized. Alternatively, two separate spectrums of risk might be considered: one that reflects the medical risks associated with the procedure, and one that represents nonmedical effects on the woman's wellbeing.
Fig. 1.
Illustrative example of conceptual definitions of abortion safety classification and measurement approach.
As Ganatra et al. [6] have noted, using WHO guidelines as a factor in this classification system means that the definition of a safe abortion can evolve as the methods of inducing abortion, as well as evidence about their safety, change over time. This is largely an advantage of such a classification system, although it also means that abortions that are classified as safe at one point in time might eventually be classified as unsafe when better methods become available, or that some methods will be classified as unsafe before they undergo study and approval.
3. Quantifying unsafe abortion
Whatever classification system is ultimately adopted by researchers and other stakeholders in the field, research quantifying the incidence of abortion at each level of safety will be necessary to operationalize it, and this represents the more difficult task by far. At present, the data that would be needed to measure the distribution of abortions across the suggested categories do not exist for most countries.
If the incidence of complications from induced abortion across settings and over time is to be evaluated, consistent definitions and data collection tools are needed. A recent systematic review [11] underscored the differences in definitions of abortion morbidity used in research and their effects on estimates, and urged for standardization of case definitions and methodologies across studies.
Qualitative research on the impact of stigma and risk of criminal sanctions on the well-being of women who obtain an abortion where it is illegal or stigmatized can help to justify the incorporation of these factors in a classification system. But differences in the prevalence and strength of stigma are difficult to measure across countries. A data collection tool that focuses specifically on measuring abortion stigma has recently been developed and tested in two African countries [12]. By developing questions that can be included in nationally representative surveys, or identifying easily measured factors that are associated with abortion-related stigma, we can approach a standardized, operational definition of stigma that can be used across countries.
Possibly, the most critical area of research is the incidence of medical abortion and the rate and severity of complications following medical abortion when incorrect regimens are used. The challenges inherent in this research include measuring the incidence of a clandestine practice that can be done without the help of medically trained professionals, and differentiating between women who obtain follow-up care for non-complicated abortions and those who experience complications. An added challenge is the fact that medical abortion often has a clinical presentation similar to that of spontaneous abortion. In the absence of a gold standard, methods for addressing these research questions must be tested and compared against each other. Research methods developed to study other clandestine behaviors might offer novel approaches to studying the incidence and outcomes of these procedures.
4. Final points
While we recognize that safety is a function of more than whether a woman experiences a medical complication, it cannot be denied that unsafe abortion that results in unnecessary complications is of grave public health importance. It has been estimated that at least 6.9 million women experience complications of an abortion each year [13]. Moving toward a definition that reflects the spectrum of abortion safety would help us to acknowledge the other consequences that women experience when they obtain an abortion outside optimal settings; it might also compel prioritization of investments in research to more accurately measure the incidence of abortion across categories of safety, and in programs and policies to reduce the incidence of unsafe abortion. As we enter an era in which new global health goals, indicators, and targets are being forged, establishing well-defined and measurable dimensions of unsafe abortion is essential if we are to ensure that preventing unsafe abortion is on the global public health agenda.
Acknowledgments
The Expert Meeting on which this report is based was funded by the UK through the STEP UP (Strengthening Evidence for Programming on Unintended Pregnancy) Research Programme Consortium, and through a grant to the Guttmacher Institute. One of the participants of the Expert Meeting and coauthors of the report (S.M.) is a representative of the Department for International Development. The views presented here are those of the authors, and not necessarily those of the donor agency or the institutions with which the coauthors are affiliated.
Conflicts of interest
The authors have no conflicts of interest.
References
- 1.World Health Organization . WHO; Geneva: 1993. The prevention and management of unsafe abortion. [Google Scholar]
- 2.Sedgh G., Singh S., Shah I.H., Ahman E., Henshaw S.K., Bankole A. Induced abortion: incidence and trends worldwide from 1995 to 2008. Lancet. 2012;379(9816):625–632. doi: 10.1016/S0140-6736(11)61786-8. [DOI] [PubMed] [Google Scholar]
- 3.Winikoff B., Sheldon W. Use of medicines changing the face of abortion. Int Perspect Sex Reprod Health. 2012;38(3):164–166. doi: 10.1363/3816412. [DOI] [PubMed] [Google Scholar]
- 4.Grimes D.A., Benson J., Singh S., Romero M., Ganatra B., Okonofua F.E. Unsafe abortion: the preventable pandemic. Lancet. 2006;368(9550):1908–1919. doi: 10.1016/S0140-6736(06)69481-6. [DOI] [PubMed] [Google Scholar]
- 5.Owolabi O. Expert meeting on the definition and measurement of unsafe abortion. Strengthening Evidence for Programming on Unintended Pregnancy (STEP UP) and Guttmacher Institute meeting. http://www.popcouncil.org/uploads/pdfs/2014STEPUP_UnsafeAbortionMeetingReport.pdf. Published 2014. Accessed July 18, 2015.
- 6.Ganatra B., Tuncalp O., Johnston H.B., Johnson B.R., Jr, Gulmezoglu A.M., Temmerman M. From concept to measurement: operationalizing WHO's definition of unsafe abortion. Bull World Health Organ. 2014;92(3):155. doi: 10.2471/BLT.14.136333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . 2nd ed. World Health Organization; Geneva: 2012. Safe abortion: technical and policy guidance for health systems. [PubMed] [Google Scholar]
- 8.Bartlett L.A., Berg C.J., Shulman H.B., Zane S.B., Green C.A., Whitehead S. Risk factors for legal induced abortion-related mortality in the United States. Obstet Gynecol. 2004;103(4):729–737. doi: 10.1097/01.AOG.0000116260.81570.60. [DOI] [PubMed] [Google Scholar]
- 9.Miller S., Lehman T., Campbell M., Hemmerling A., Anderson S.B., Rodriguez H. Misoprostol and declining abortion-related morbidity in Santo Domingo, Dominican Republic: a temporal association. BJOG. 2005;112(9):1291–1296. doi: 10.1111/j.1471-0528.2005.00704.x. [DOI] [PubMed] [Google Scholar]
- 10.Baggaley R.F., Burgin J., Campbell O.M. The potential of medical abortion to reduce maternal mortality in Africa: what benefits for Tanzania and Ethiopia? PLoS One. 2010;5(10) doi: 10.1371/journal.pone.0013260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adler A.J., Filippi V., Thomas S.L., Ronsmans C. Quantifying the global burden of morbidity due to unsafe abortion: magnitude in hospital-based studies and methodological issues. Int J Gynecol Obstet. 2012;118(Suppl. 2):S65–S77. doi: 10.1016/S0020-7292(12)60003-4. [DOI] [PubMed] [Google Scholar]
- 12.Shellenberg K.M., Hessini L., Levandowski B.A. Developing a scale to measure stigmatizing attitudes and beliefs about women who have abortions: results from Ghana and Zambia. Women Health. 2014;54(7):599–616. doi: 10.1080/03630242.2014.919982. [DOI] [PubMed] [Google Scholar]
- 13.Singh S, Maddow-Zimet I. Facility-based treatment for medical complications resulting from unsafe pregnancy termination in the developing world, 2012: a review of evidence from 26 countries [published online ahead of print August 19, 2015]. BJOG. doi:10.1111/1471-0528.13552 [DOI] [PMC free article] [PubMed]