Abstract
Background
To evaluate the reliability of the Bare Spot (BS) as an anatomical landmark for the intra-operative definition of bone loss in anterior shoulder instability.
Methods
The distances from the BS to the anterior (BS-A), posterior (BS-P) and inferior margins of the glenoid cavity were determined both under arthroscopic visualization and by an open approach in 20 shoulders.
Results
The BS did not coincide with the centre of the glenoid cavity of the studied shoulders because the BS-P distance was greater than the BS-A distance (p < 0.05) and was located 40% closer to the anterior margin. The authors suggest a correction factor: BP-A × 1.25/BP-P = 1.
Conclusions
The BS is located at a mean distance of 40% of the joint diameter, relative to the anterior margin of the glenoid. This point may be used as a landmark, using a correction factor of its mostly anterior positioning. Arthroscopy was reliable for bone measurements of the shoulder joint.
Keywords: cadaver, human, joint instability/pathology, joint instability/surgery, shoulder joint/pathology, shoulder joint/surgery
Introduction
Shoulder dislocation is a frequently encountered disorder in orthopaedic practice, corresponding to approximately 2% of traumatic lesions of the upper limb, with anterior displacement occurring most frequently (85% to 90%).1 Dislocation recurrence, the degree of soft tissue injury and the occurrence of bone injury (on the humeral head or on the anterior margin of the glenoid cavity of the scapula) determine joint instability.1 Because it affects young adults in their productive years, shoulder instability has a direct impact on the career of a professional athlete or on the work capacity of an employee.1,2
The anatomical and pathological knowledge of shoulder instability and its treatment has continually evolved. The advent of imaging and surgical technologies allowed the improved treatment of this injury.2,3 The recognition of the essential lesion by Bankart in 1923 was a great advance in the treatment of glenohumeral instability and serves as a pillar to this day.1,2,4,5
Several surgical techniques exist to treat shoulder instability. Reconstruction of the anteroinferior glenoid lip by an arthroscopic approach is the most commonly used technique; however, it has a high rate of relapse (65%) in patients with greater than 25% bone loss at the anterior margin of the glenoid cavity.3–5 In these cases, surgery with a bone block procedure, such as coracoid process transfer, may be a better option.5,6 Therefore, the precise definition of the residual bone portion in the glenoid cavity is fundamental for appropriate treatment.3,4,6,7
In 2002, Burkhart et al.2 published a study on the quantification of bone loss and suggested the need to determine a consistent anatomical landmark present in the glenoid cavity that would allow a defined bone loss necessary to produce the inverted pear. In that study, the Bare Spot (BS) was defined as an anatomical structure that is easy to visualize arthroscopically, located in the centre of the inferior glenoid cavity, which may serve as a parameter for the measurement of the bone loss at the anteroinferior margin. The BS would be equidistant from the inferior, anteroinferior and posteroinferior margins of the cavity. Thus, during the surgical procedure, the identification of this reference point would allow a reliable bone loss measurement, which would directly affect the treatment.2–4,6,7
Burkhart’s study triggered a series of other studies that aimed to demonstrate the usefulness of the BS, to anatomically redefine it or to refute it as the central landmark of the cavity.2,4,5,8–11
Consensus exists regarding the importance of quantifying the bone loss to define the best course of action for each case.10,11,12 However, because the determination of the BS is not reproducible, the feasibility of its use as an anatomical landmark remains controversial.10–15
The objective of the present study was to anatomically locate the BS and to determine its reliability for measuring bone loss.
Materials and methods
The present study was approved by the Ethics Committee (CAAE 54343916.2.0000.5258) and conducted under the care of the Anatomy Department of the University. Twenty shoulders (six of female cadavers, 10 of male cadavers and four of already dissected pieces), where the sex was not possible to determine, were analyzed. All of the cadavers (16 shoulders) were adults aged older than 60 years at the time of death. Ten shoulders on the right side and 10 shoulders on the left side were used. Cadavers showing glenohumeral arthrosis, bone deformity, shoulder girdle fractures that indicated the possibility of shoulder dislocation and non-identification of the BS were excluded. These specimens were replaced so that the sample number (n) remained as 20. Six shoulders were replaced. Four were male and two were female. All of them were aged older than 60 years. We replaced them for shoulders with same side, age and sex, although without deformities.
The specimens were placed in the lateral decubitus position, with the upper limb abducted at 30°. The posterior angle of the acromion was identified. The posterior portal was established 2 cm inferior and 2 cm medial to the vertex of the angle. Through the posterior portal, an arthroscopic inspection of the joint was performed using Smith & Nephew® equipment (direct vision arthroscope 4.0 mm × 160.0 mm 30°; 560 H series camera, Gemini 5 mm fibre optic cable; Smith & Nephew, London, UK).
The Bare Spot (BS point) of the glenoid cavity was identified. From the intra-articular environment, we established the anterior portal (inside-out) by introducing the probe through the posterior portal and progressing perpendicular to the anterior margin of the glenoid cavity, in alignment with the BS, progressing to the skin. Through the anterior portal, a millimetre probe was introduced. With the tip of the probe, the BS was marked (Fig. 1). The distances from the BS to the posterior margin of the cavity (BS-P arthroscopy) and from the anterior margin of the glenoid cavity to the BS (BS-A arthroscopy) and from the BS to the inferior margin (BS-I arthroscopy) were measured. The measurements were performed by two independent evaluators.
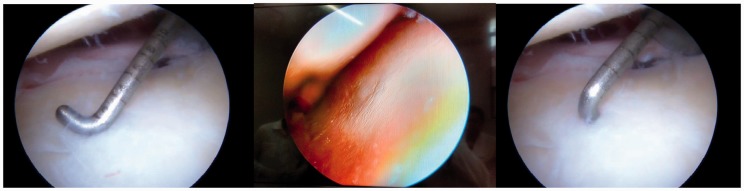
Figure 1.
Measurement of the distances from the Bare Spot to the anterior (BS-A) and posterior (BS-P) margins of the glenoid cavity under arthroscopic visualization.
Next, the cadavers were dissected. Through a deltopectoral surgical approach and with tenotomy of the subscapularis and the long tendon of the biceps, the glenoid cavity was exposed. The BS point was identified again. The measurements of the distances from the BS to the posterior margin of the cavity (BS-P open) and from the anterior margin of the glenoid cavity to the BS (BS-A open) were again determined (Fig. 2). The measurements were performed by independent evaluators who were unaware of the results obtained by the surgeons responsible for the arthroscopy.
Figure 2.
Open measurement of the distances from the Bare Spot to the anterior (BS-A) and posterior (BS-P) margins of the glenoid cavity by a deltopectoral surgical approach.
The data were analyzed statistically through the physics online program of St John’s University (Queens, NY, USA). A two-tailed paired Student’s t-test and a Kolmogorov–Smirnov test were used to determine the statistical correlation. p < 0.05 was considered statistically significant.
Results
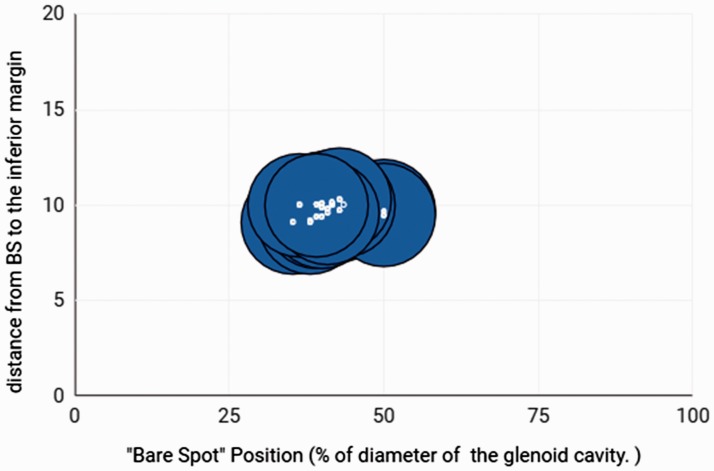
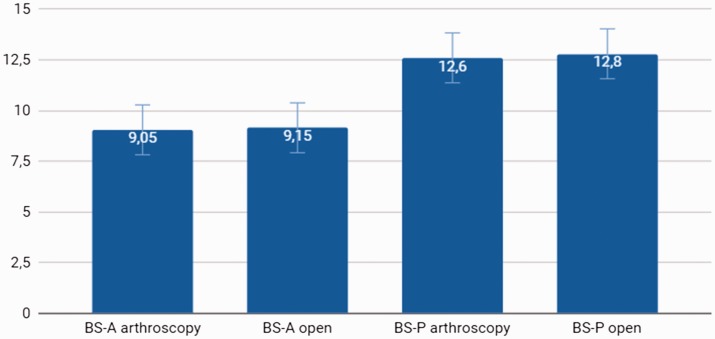
The mean distance from the BS to the posterior margin (BS-P arthroscopy) evaluated by arthroscopy was 12.6 mm, with a median of 13 mm, ranging from 10 mm to 14 mm, and with a 95% confidence interval (CI) of 12.02 mm to 13.18 mm. The distance from the BS to the anterior margin averaged (BS-A arthroscopy) 9.05 mm (95% CI = 8.363 mm to 9.373 mm), with a median of 9 mm, ranging from 7 mm to 12 mm (Fig. 3). The distance from the BS to the inferior margin (BS-I arthroscopy) averaged 11.2 mm, with a median of 11 mm, ranging from 9.5 mm to 12 mm. After dissection, the mean distance from the BS to the anterior glenoid (BS-A open) margin was 9.15 mm (95% CI = 8.466 mm to 9.834 mm), from the BS to the posterior margin (BS-P open) was 12.8 mm (95% CI = 12.28 mm to 13.32 mm) and from the BS to the inferior margin (BS-I open) was 11.1 mm (95% CI = 9 mm to 12 mm) (Table 1). The measurements were performed by two different evaluators and compared. The measurements obtained under arthroscopic visualization and by the open approach were also independently analyzed. No significant difference was observed between the measurements made by the two evaluators (p > 0.05) (Fig. 4). Similarly, no significant difference was observed between the measurements from the BS to the anterior margin obtained by the open approach or by arthroscopy (p > 0.05). The open approach and arthroscopic visualization measurements of the posterior radius of the distance from the BS to the posterior margin also showed no significant difference.
Figure 3.
Position of the Bare Spot (BS) in relation to the centre of the glenoid cavity. The origin of the abscissa represents the anterior margin of the glenoid cavity. The 100% position represents the posterior margin. The 50% position represents half the diameter of the inferior margin of the glenoid cavity. The BS is located in an anterior position.
Table 1.
Statistical data of the samples.
| Mean | Median | SD | 95% confidence interval | Measurements (mm) | p | |
|---|---|---|---|---|---|---|
| BS-A arthroscopy | 9.05 | 9.0 | 1.47 | 8.363 to 9.737 | 7 to 12 | 0.07 |
| BS-A open | 9.15 | 9.0 | 1.46 | 8.466 to 9.834 | 6 to 12 | 0.034 |
| BS-P arthroscopy | 12.6 | 13.0 | 1.23 | 12.02 to 13.18 | 10 to 14 | 0.04 |
| BS-P open | 12.8 | 13.0 | 1.11 | 12.28 to 13.32 | 11 to 14 | 0.04 |
Measurements from the Bare Spot (BS) to the anterior (BS-A) and posterior (BS-P) margins of the glenoid cavity under arthroscopic visualization (arthroscopy) or after dissection. The distances from the BS to the BS-A tended to be less than the distances from the BS to the BS-P of the cavity.
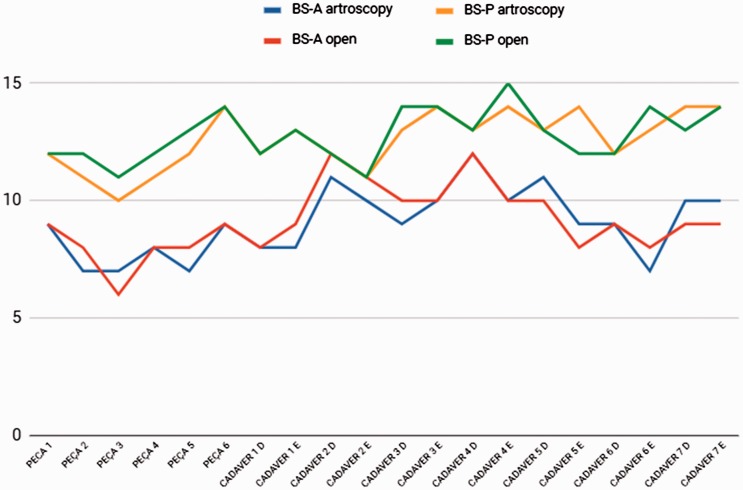
Figure 4.
Variation of the measurements from the Bare Spot to the anterior (BS-A) and posterior (BS-P) margins under arthroscopic visualization or by an open approach.
The comparison between the measurements of the anterior radius (i.e., BS-A arthroscopy and open) and the posterior radius (i.e. BS-P arthroscopy and open) showed a significant difference, with the BS-A measurement less than the BS-P measurement. The BS-A was less than the BS-P (Fig. 5) when measured both by the open approach and by arthroscopic visualization.
Figure 5.
Measurements of Bare Spot to the anterior (BS-A) and posterior (BS-P) distances under arthroscopic visualization and by an open approach.
Discussion
Anterior instability of the shoulder is relatively common, and its prevalence has been increasing, mainly as a result of the growing sports demands for athletes and non-athletes. Several treatments are available, each with its precise indications, advantages and disadvantages. One of the central issues in its therapeutic assessment is to determine the bone loss at the anteroinferior margin of the glenoid cavity. In 2000, Burkhart and DeBeer3 published a retrospective study evaluating the causes of failure of the Bankart lesion repair under arthroscopic visualization. In that study, the inverted pear concept was introduced and it was concluded that bone losses greater than 25% of the cavity diameter modifies this pattern, leading to dislocation recurrence after Bankart repair.13
Subsequently, quantification of the bone loss became fundamental to guide the therapeutic management. In 2002, Burkhart et al.2 concluded that the BS might be used as a reference of the reliable anatomical landmark of the inferior glenoid centre, thus allowing the arthroscopic measurement of the anterior and posterior radii of the glenoid cavity, facilitating bone loss quantification. In 2004, Lo et al.4 performed a retrospective study using the BS to identify the glenoid centre during arthroscopy, thus estimating bone loss.
Several studies attempted to replicate the results obtained by Burkhart2 but were unsuccessful. De Wilde et al.5 described the BS or tubercle of Assaki as a thinning of the subchondral bone. Vogt et al.6 described a point of origin of the eccentric distribution of the collagen fibrils of the glenoid cartilage. Fealy et al.7 proposed that the BS is not present in immature skeletons, suggesting that this point is not a consistent anatomical landmark.
In 2004, Aigner et al.8 attempted to confirm Burkhart’s2,3 findings by dissecting 10 cadavers. In their study, they found that the BS was not present in all specimens. Additionally, they concluded that the BS diverged significantly from the glenoid centre. The distance from the BS to the anterior margin of the glenoid (9.7 mm) was significantly less than the distance to the posterior margin (13.71 mm).
In 2006, Huysmans et al.9 analyzed 40 scapulae from skeletally mature cadavers and found that the BS was present in 35 of the 40 glenoids. They also observed a significant difference between the distances from the BS centre to the anterior and posterior margins of the glenoid. In their study, the mean distances from the BS to the anterior and posterior margins were 11.04 mm and 12.96 mm, respectively.
Kralinger et al.,10 in 2006, evaluated 20 scapulae through multi-slice computed tomography and concluded that the distance from the BS to the anterior margin was 9.7 mm (6.5 mm to 13.7 mm), from the BS to the inferior margin was 10.9 mm (9.1 mm to 13.8 mm) and from the BS to the posterior margin was 13.7 mm (11.3 mm to 19.2 mm).
In 2013, Gagliardi et al.14 conducted a retrospective study by reviewing the tomographic images of 50 patients and found that the BS was not present in skeletally immature individuals younger than 10 years. Imaging of a 14-year-old patient appeared to allow identification of the BS.
Miyatake et al.,15 in 2014, published a study in which the involved shoulders of 40 patients diagnosed with anterior glenohumeral instability and recurrent dislocations were evaluated, which compared the intra-operative arthroscopic measurements and computed tomography. They concluded that the BS did not coincide with the centre of the inferior glenoid cavity and that the bone loss measurement obtained under arthroscopic visualization was inaccurate, suggesting that computed tomography with three-dimensional reconstruction might be the most accurate way to define the bone loss16-18.
In the present study, 20 shoulders were analyzed. The measurements of the distance from the BS to the anterior and posterior margins were performed under arthroscopic visualization and by an open approach. We found no significant difference between the arthroscopic and open measurements (p < 0.05). These data suggest that the portals used did not influence the measurement of the cavity radius. By establishing the anterior portal coinciding with the radius and perpendicular to the margin, we minimized the influence of the portal angulation in the measurement of distances. This measurement was only possible because this was a cadaver study, in which the portal location on the surface was not a concern, only the alignment with the cavity axis.
However, considering the anterior and posterior distances, the BS modestly approaches the anterior margin, with the BS-P measurement (12.8 mm) slightly greater than the BP-A measurement (9.15 mm), which suggests a more anterior positioning of the BS, thus not coinciding with the centre of the glenoid cavity. These data are compatible with the current literature and corroborate the results of the aforementioned studies.
When comparing the measurements obtained under arthroscopic visualization and by the open approach, no difference was observed, showing that arthroscopy did not generate image distortion that might have compromised the measurements and that such a measurement method during direct visualization of the joint was reliable.
When analyzing the measurements obtained, we observed that the anterior location of the BS was consistent, which suggests that this point, although not located in the cavity centre, maintains the relative ratio of the BS-A and BS-P distances. Thus, we calculated the percentage ratio between the distances through the difference between the measurements in relation to the diameter. We observed that the BS was located, on average, 41.65% from the cavity diameter (95% CI = 39.99% to 43.3%, median 41.67%) when evaluating the video measurement results. From the measurements obtained after shoulder dissection, we observed a mean of 41.61% (95% CI = 39.8% to 43.42%, median 40.45%). Comparing these results, we obtained a p-value of 0.164.
Although the result was not significant, the anterior location at 41% of the glenoid cavity diameter suggests that this point is consistent and, although located anteriorly and not coincident with the cavity centre as initially suggested by Burkhart, it may be a reproducible landmark usable as a reference for the bone loss at the anterolateral margin of the glenoid.
The present study is pertinent because without this information, the surgeon may overestimate bone loss because the BS-A distance is by nature slightly less than the BS-P distance. This difference may cause the specialist to adopt a more aggressive approach, opting for trans-subscapularis osteotendinous transfer over the arthroscopic labral repair technique; thus, a correction factor should always be used to correctly evaluate this measurement. When associated with the Hill–Sachs lesion, the definition of the bone loss at the anterior margin of the glenoid cavity becomes crucial. In cases of off-track bipolar bone loss, precise quantification of the bone remnant in the glenoid cavity is essential for correct treatment and relapse prevention.
As a practical example, if the surgeon finds that the distance from the BS to the anterior margin was 8 mm and the distance from BS to posterior margin was 10 mm, we can infer from this information that no significant bone loss occur during dislocation. In another example, if the surgeon finds that the distance from the BS to the anterior margin is 6 mm and to the posterior margin was 10 mm, this suggests that a bone loss greater than 25% occurred, even considering the anterior location of BS. In this case, Latarjet surgery should be indicated.
Correction factor: (BP-A measurement × 1.25/BP-P measurement = 1)
Conclusions
The present study suggests the following:
The BS is located at a mean distance of 40% of the joint diameter relative to the anterior margin.
This point may be used as a landmark, using a correction factor for its mostly anterior positioning.
Arthroscopy is reliable for bone measurements of the shoulder joint.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical review and patient consent
The study was approved by the ethical committee of the University.
References
- 1.Lech O, Freitas JR, Piluski P, Severo A. Luxação recidivante do ombro: do papiro de Edwin Smith à capsuloplastia térmica [shoulder recurrent dislocation: from Edwin Smith papyrus to thermal capsuloplasty]. Rev Bras Ortop 2005; 40: 625–637. [Google Scholar]
- 2.Burkhart SS, DeBeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 2002; 18: 488–491. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart SS, DeBeer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill–Sachs lesion. Arthroscopy 2000; 16: 677–694. [DOI] [PubMed] [Google Scholar]
- 4.Lo IKY, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy 2004; 20: 169–174. [DOI] [PubMed] [Google Scholar]
- 5.De Wilde LF, Berghs BM, Audenaert E, Sys G, Van Maele GO, Barbaix E. About the variability of the shape of the glenoid cavity. Surg Radiol Anat 2004; 26: 54–59. [DOI] [PubMed] [Google Scholar]
- 6.Vogt S, Eckstein F, Scon M, Putz R. Preferential direction of the collagen fibrils in the subchondral bone of the hip and shoulder joint. Ann Anat 1999; 181: 181–189. [DOI] [PubMed] [Google Scholar]
- 7.Fealy S, Rodeo SA, Dicarlo EF, O’Brien SJ. The developmental anatomy of the neonatal glenohumeral joint. J Shoulder Elbow Surg 2000; 9: 217–222. [PubMed] [Google Scholar]
- 8.Aigner F, Longato S, Fritsch H, Kralinger F. Anatomical considerations regarding the ‘Bare Spot’ of the glenoid cavity. Surg Radiol Anat 2004; 26: 308–311. [DOI] [PubMed] [Google Scholar]
- 9.Huysmans PE, Haen PS, Kidd M, Dhert WJ, Willems JW. The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elbow Surg 2006; 15: 759–763. [DOI] [PubMed] [Google Scholar]
- 10.Kralinger F, Aigner F, Longato S, Rieger M, Wambacher M. Is the Bare Spot a consistent landmark? Arthroscopy 2006; 4: 428–432. [DOI] [PubMed] [Google Scholar]
- 11.Calandra JJ, Baker CL, Uribe J. The incidence of Hill–Sachs lesions in initial anterior shoulder dislocations. Arthroscopy 1989; 5: 254–257. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart SS, DeBeer JF, Barth JR, Criswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anterior instability and significant bone loss. Arthroscopy 2007; 23: 1033–1041. [DOI] [PubMed] [Google Scholar]
- 13.Shibata H, Gotoh M, Mitsui Y, et al. Risk factors for shoulder re-dislocation after arthroscopic Bankart repair. J Orthop Surg Res 2014; 9: 53–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gagliardi JA, Carino M. Glenoid Bare Spot. Applied Radiol 2013; 10: 29–31. [Google Scholar]
- 15.Miyatake K, Takeda Y, Fujii K, Takasago T, Iwame T. Validity of arthroscopic measurement of glenoid bone loss using the Bare Spot. Open Access J Sports Med 2014; 5: 37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin SJ. Estimation of anterior glenoid bone loss area using the ratio of bone defect length to the distance from posterior glenoid rim to the centre of the glenoid. Knee Surg Sports Traumatol Arthrosc 2018; 26: 48–55. [DOI] [PubMed] [Google Scholar]
- 17.Tennent DJ, Donohue MA, Posner MA. Bone loss and glenohumeral instability. Sports Med Arthrosc Rev 2017; 25: 131–135. [DOI] [PubMed] [Google Scholar]
- 18.Shin SJ. Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic bankart repair. Am J Sports Med 2017; 45: 1975–1981. [DOI] [PubMed] [Google Scholar]