Abstract
Background
Proper glenoid position in total shoulder arthroplasty (TSA) is important. However, traditional glenoid version (GV) measurements overestimate retroversion on radiographs (XR) and computed tomography (CT).
The fulcrum axis (FA) uses palpable surface landmarks and may be useful as an intra-operative guide. Also, the FA has not yet been validated on XR or CT in an arthritic population.
Methods
Four observers measured FA and GV on the XR, CT and three-dimensional CT (3DCT) of 40 patients who underwent TSA at a single institution from 2009 to 2015. Reliability and accuracy of FA and GV were calculated for XR and CT, using 3DCT as the gold standard.
Results
The mean FA and GV were 7.768° and 18.910° on XR; 6.23° and 12.920° on CT; and 8.100° and 7.740° on 3DCT, respectively. FA and GV were significantly different for XR and CT (p < 0.001) but not for 3DCT (p = 0.725). The inter-rater reliability, intra-rater reliability and accuracy of FA were not significantly different from GV and were 0.929 to 0.948, 0.779 to 0.974 and 0.674 to 0.705, respectively. However, the absolute difference of FA was closer to the gold standard (3DCT) than GV for XR (0.330° versus 11.172°) and CT (1.871° versus 5.178°) (p < 0.001).
Conclusions
FA showed comparable reliability and accuracy to GV. However, FA more accurately reflected the gold standard.
Keywords: accuracy, glenoid version, fulcrum axis, osteoarthritis, reliability, shoulder
Introduction
Total shoulder arthroplasty (TSA) is an effective and reliable treatment for severe glenohumeral osteoarthritis. Proper glenoid component positioning is necessary for optimal functional outcome1,2 and TSA longevity.3–6 Although glenoid retroversion in normal shoulders (defined as shoulders with no history of surgery or significant dysfunction or pain and no evidence of skeletal dysplasia or arthritis) is typically less than 10° (mean 1° to 3°),7,8 osteoarthritis may lead to eccentric glenoid wear and up to 50° of retroversion (mean 7° to 17°).8–12 As little as 10° to 15° of glenoid component retroversion can decrease TSA survival3,6,13 and >20° of retroversion is associated with poor clinical outcomes.1,2 Therefore, an accurate and reliable method to measure the pre-operative glenoid version is essential to properly plan eccentric glenoid component placement and correct the abnormal arthritic anatomy.
Pre-operative imaging
Plain radiographs (XR) are readily available and involve minimal radiation but quality varies widely and glenoid retroversion can vary by as much as 21° and is overestimated in 86% of cases.5,14 Computed tomography (CT) is more accurate that XR but involves more radiation. However, as little as 10° of scapular malrotation during image acquisition can lead to more than 10° error in the measured glenoid version.15–17 Magnetic resonance imaging has the advantages of additional soft-tissue evaluation and no radiation, although it is costly and also susceptible to error from scapular malrotation.18 Three-dimensional CT (3DCT) is the best available imaging modality for glenoid version measurement because errors as a result of scapular rotation during image acquisition are eliminated through post-processing rotation correction.8,15,19–21 3DCT has been recommended in several studies for TSA pre-operative planning.8,15,19–21 Specific software is required but with technology advancements 3DCT is becoming readily available and user-friendly.
Measuring glenoid version (GV)
Freidman et al.9 described a technique to measure GV that was independently validated22,23 and is in common use. The GV is measured at the mid-body of the glenoid on axial CT slices and is the angle between a line connecting the anterior and posterior lips of the glenoid face and a perpendicular from the line joining the middle of the glenoid face to the most medial point of the scapular body. However, there have been concerns with the accuracy of this technique on CT as a result of variations in scapular rotation during image acquisition as well as variable curvature of the scapular body.8,15,19–21,23
The fulcrum axis (FA) was described in 2008 by Braunstein et al.24 The FA was originally used to improve the quality of anteroposterior shoulder radiographs and is formed by a line connecting the anterior tip of the coracoid to the posterolateral corner of the acromion.24 The FA is close to parallel to the glenoid face [mean (SD) 1.8° (4.5°)] in normal shoulders25 and uses easily palpable surface anatomy landmarks. The FA is reproducible and has undergone preliminary studies as a potential intra-operative guide with promising results.26
Purpose
To our knowledge, FA has not previously been measured in arthritic shoulders, nor has it been compared with GV for accuracy on XR or CT or reliability on XR, CT or 3DCT. The present study aimed to describe the normal range of FA values in patients awaiting TSA, as well as its accuracy and reliability.
Materials and Methods
Data collection
The radiographic records of all patients having undergone shoulder arthroplasty between 1 January 2009 and 31 October 2015 by three upper limb surgeons at a single institution were retrieved using a Picture Archiving and Communication System. The primary indication for arthroplasty was severe glenohumeral arthritis. Pre-operative XR and CT of the operated shoulder were retained for analysis. Cases with more than 6 months between XR and CT, with poor-quality axillary XR or with evidence of prior arthroplasty, coracoid fracture, acromial fracture or glenoid body fracture, were eliminated. An axillary XR was acceptable if five criteria were met: visible glenoid face; visible posterolateral acromion; visible coracoid; visible glenoid vault; and little to no overlap of the glenoid body with the ribcage. Examples of acceptable and unacceptable axillary XR are shown in Fig. 1.
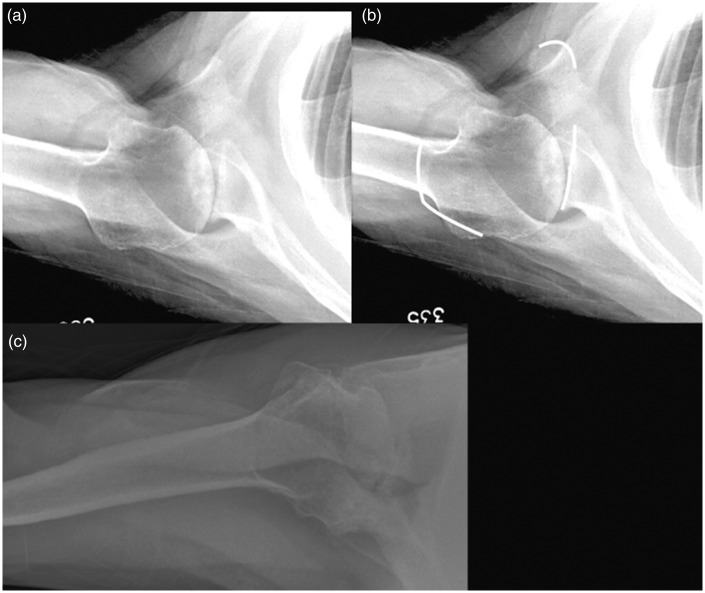
Figure 1.
(a) An acceptable axillary radiograph (XR). The posterolateral corner of the acromion, the anterior tip of the coracoid and the glenoid face are visible and are marked in white in (b). Most of the glenoid body is visible and there is minimal ribcage overlap. (c) An unacceptable axillary XR. The coracoid tip is not visible and the glenoid body is obscured by soft-tissue.
Institutional review board approval was obtained and all data and images were anonymized. Data recorded included the age of the patient, the delay between XR and CT and the Walch classification of the glenoid. Forty cases with an mean age of 71 years (range 32 years to 86 years) were retained for analysis.
Radiographic preparation
The imaging files were all standardized to the right side and converted to PDF format. The axillary XR required no additional modifications. The CT and 3DCT files were prepared as described below.
CT
Three axial cuts from each CT were superimposed: one with a clear slice of the posterolateral corner of the acromion; one showing the most anterior aspect of the tip of the coracoid; and one at the mid-point of the glenoid vault (within 10 mm inferior to the glenoid tip).9
3DCT
A 3DCT was created from each CT file using Aquarius-APS (TeraRecon, Foster City, CA, USA) and rotated to an axillary view.
Measuring the GV and the FA
Measurements were carried out on all XR, CT, and 3DCT images in PDF format using PixelStick (Plum Amazing LLC, Princeville, HI, USA) to calculate the GV and FA angles. The GV was measured using the technique described by Friedman et al.9 and the FA using the technique described by Braunstein et al.25 For the glenoid, the line connecting the anterior border to the posterior border of the glenoid face was used. Osteophytes were not included and Walch B227 glenoids were measured across the entire glenoid face (the neoglenoid was not measured separately). Examples of the GV and FA drawn on XR, CT and 3DCT are shown in Figs 2 to 4.
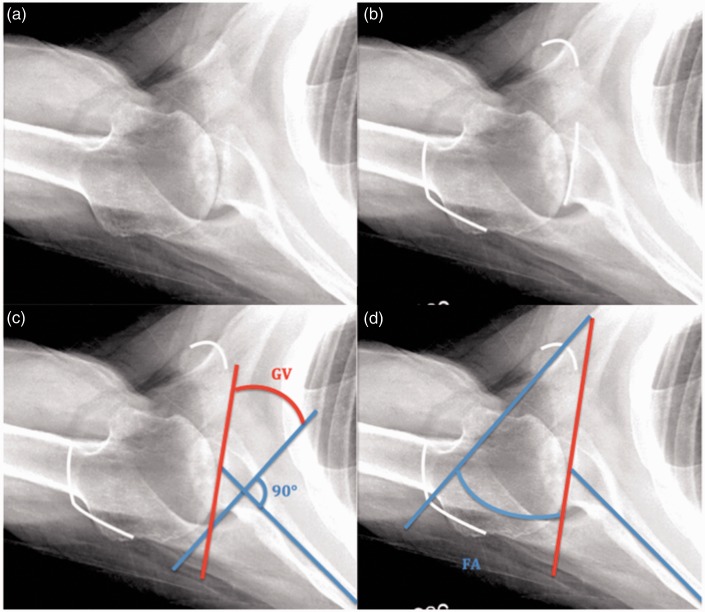
Figure 2.
An axillary radiograph of the right shoulder. (a) is unmarked; (b) is marked on the posterolateral corner of the acromion, the anterior tip of the coracoid and the glenoid face; (c) measurement of glenoid version (GV); and (d) measurement of the fulcrum axis (FA).
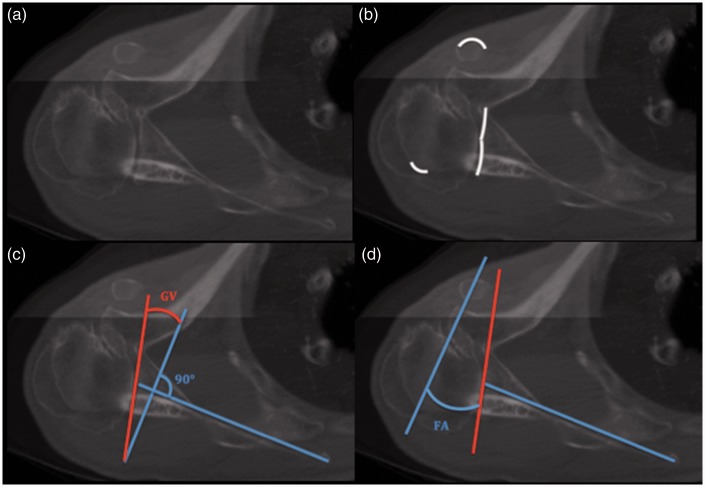
Figure 3.
A composite computed tomography of the right shoulder. (a) is unmarked; (b) is marked on the posterolateral corner of the acromion, the anterior tip of the coracoid and the glenoid face; (c) measurement of glenoid version (GV); and (d) measurement of the fulcrum axis (FA).
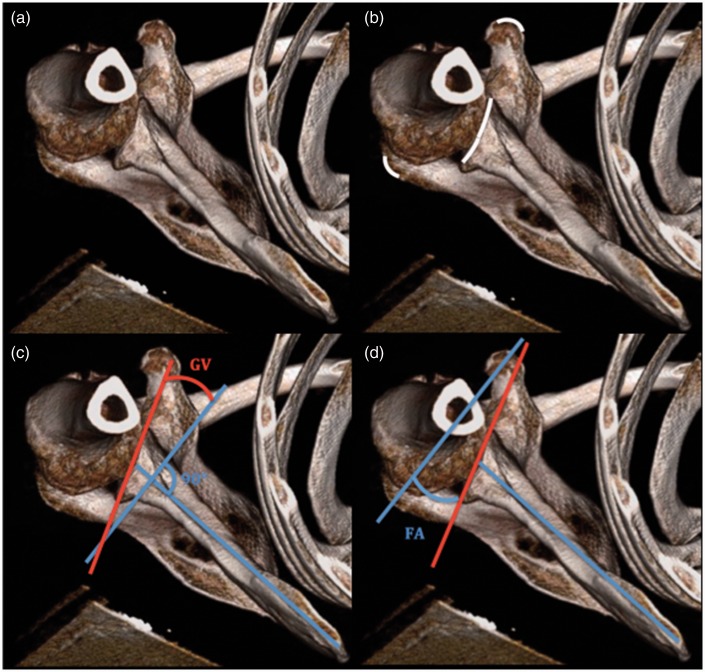
Figure 4.
A three-dimensional computed tomography of the right shoulder. (a) is unmarked; (b) is marked on the posterolateral corner of the acromion, the anterior tip of the coracoid and the glenoid face; (c) shows the measurement of glenoid version (GV); and (d) the measurement of the fulcrum axis (FA).
Measurements were taken by three fellowship-trained orthopaedic surgeons and one upper-extremity fellow (DN, TA, JM and CS). All measurements were taken twice with a minimal interval of 4 weeks.
Statistical analysis
Statistical analysis was performed using SPSS, version 23 (IBM Corp., Armonk, NY, USA). The mean GV and FA and their respective SD were calculated from measurements obtained on 3DCT. Inter-rater and intra-rater reliability was calculated for GV and FA on all imaging modalities.
Accuracy was determined using two methods. The first employed the intraclass coefficient (ICC) for each rater’s measurements using the corresponding 3DCT as the gold standard. The second calculated the difference, in degrees, of each FA and GV measurement on XR and CT from their corresponding 3DCT measurements. The mean and SD were reported as the average difference (AD). Statistical significance was achieved when p < 0.01. The reliability and ICC was considered poor at 0.01 to 0.20, fair at 0.21 to 0.40, moderate at 0.41 to 0.60, substantial at 0.61 to 0.80 and near-perfect at 0.81 to 1.00.
Finally, a post hoc analysis was performed using G*power statistical software (Heinrich-Heine-Universitāt Düsseldorf, Düsseldorf, Germany) to determine the power (1 – β) of the ICCs of FA and GV for XR, CT and 3DCT.
Results
A total of 40 radiographic series were retained for final analysis. Patients had a mean age of 71 years (range 32 years to 86 years) at the time of the axillary radiograph and a mean delay of 68 days to CT (range 2 days to 230 days). Twenty-four series involved the right side and 16 involved the left. Three cases showed evidence of avascular necrosis with collapse of the humeral head and the remaining 37 cases showed severe glenohumeral joint space loss and glenoid wear. The glenoid Walch classification27 was A in 14 cases, B in 21 cases and C in five cases.
The mean FA was fairly consistent across the imaging modalities (6.227° to 8.098°) and ranged from –45.772° to 45.830°. The mean GV across the imaging modalities was 7.738° to 18.910° of retroversion and ranged from –70.683° to 38.963°. Measurements of GV recorded greater retroversion on XR than measurements on CT or 3DCT (Table 1).
Table 1.
Fulcrum axis (FA) and glenoid version (GV) on radiograph (XR), computed tomography (CT) and three-dimensional CT (3DCT).
| FA (SD) | GV (SD) | p | |
|---|---|---|---|
| XR | 7.768 (13.418) | 18.910 (15.625) | <0.0001 |
| CT | 6.227 (14.476) | 12.916 (14.028) | <0.0001 |
| 3DCT | 8.098 (12.628) | 7.738 (13.210) | 0.725 |
The inter-rater reliability of FA and GV was 0.929 (0.881 to 0.960) and 0.957 (0.931 to 0.975) on XR; 0.958 (0.924 to 0.977) and 0.975 (0.959 to 0.986) on CT; and 0.948 (0.895 to 0.973) and 0.979 (0.962 to 0.989) on 3DCT, respectively. There were no statistically significant differences between FA and GV on XR, CT or 3DCT (Table 2).
Table 2.
Inter-rater reliability of fulcrum axis (FA) and glenoid version (GV) on radiograph (XR), computed tomography (CT) and three-dimensional CT (3DCT).
| FA (range) | GV (range) | |
|---|---|---|
| XR | 0.929 (0.881 to 0.960) | 0.957 (0.931 to 0.975) |
| CT | 0.958 (0.924 to 0.977) | 0.975 (0.959 to 0.986) |
| 3DCT | 0.948 (0.895 to 0.973) | 0.979 (0.962 to 0.989) |
The intra-rater reliability of FA and GV ranged from 0.842 to 0.958 and 0.895 to 0.972 on XR; from 0.913 to 0.956 and 0.919 to 0.982 on CT; and from 0.779 to 0.974 and 0.904 to 0.989 on 3DCT, respectively. There were no statistically significant differences between FA and GV on XR, CT or 3DCT (Table 3).
Table 3.
Intra-rater reliability of fulcrum axis (FA) and glenoid version (GV) on radiograph (XR), computed tomography (CT) and three-dimensional CT (3DCT).
| Observer 1 | Observer 2 | Observer 3 | Observer 4 | ||
|---|---|---|---|---|---|
| XR | FA | 0.842 | 0.958 | 0.899 | 0.889 |
| GV | 0.895 | 0.972 | 0.933 | 0.967 | |
| CT | FA | 0.913 | 0.915 | 0.956 | 0.929 |
| GV | 0.982 | 0.919 | 0.960 | 0.974 | |
| 3DCT | FA | 0.973 | 0.969 | 0.779 | 0.974 |
| GV | 0.989 | 0.981 | 0.904 | 0.968 | |
The accuracy of FA and GV on XR and CT was calculated using 3DCT as the gold standard by two methods, as described in the Materials and methods. The ICC for FA and GV was 0.674 (0.623 to 0.748) and 0.578 (0.315 to 0.688) on XR and 0.705 (0.616 to 0.802) and 0.740 (0.536 to 0.0830) on CT, respectively (Table 4). The mean (SD) AD for FA and GV was 0.330° (10.418°) and 11.172° (9.748°) on XR and 1.871° (10.146°) and 5.178° (8.604°) on CT, respectively. The accuracy as measured by AD was significantly better for FA than GV on both XR (p < 0.0001) and CT (p < 0.0001). The GV overestimated glenoid retroversion, by approximately 11° on XR and 5° on CT (Table 5).
Table 4.
Accuracy of fulcrum axis (FA) and glenoid version (GV) on radiograph (XR) and computed tomography (CT) as measured by intraclass coefficient, using three-dimensional CT as the gold standard.
| FA (range) | GV (range) | |
|---|---|---|
| XR | 0.674 (0.623 to 0.748) | 0.578 (0.315 to 0.688) |
| CT | 0.705 (0.616 to 0.802) | 0.740 (0.536 to 0.830) |
Table 5.
Accuracy of fulcrum axis (FA) and glenoid version (GV) on on radiograph (XR) and computed tomography (CT) as measured by average difference, using three-dimensional CT as the gold standard.
| FA (SD) | GV (SD) | p | |
|---|---|---|---|
| XR | 0.330 (10.418) | 11.172 (9.748) | <0.0001 |
| CT | 1.871 (10.146) | 5.178 (8.604) | <0.0001 |
A post hoc analysis using the ICCs for FA and GV on XR, CT and 3DCT showed powers (1 – β) of 0.85, 0.99 and 0.93, respectively.
Discussion
In the present study, we have described the mean FA and range on 3DCT (mean 8.098°, range –27.940° to 45.830°) in an arthritic population. To the best of our knowledge, the FA has only previously been reported in a non-arthritic population.24,25 Using the measured GV on 3DCT (7.737° mean GV on 3DCT) to ‘correct the version to neutral’ (i.e. 8.098° – 7.737° = 0.361°), we obtain a value of 0.361° from the ‘ideal glenoid plane’. This is very similar to the 1.8° FA as reported by Braunstein et al.25 in non-arthritic shoulders. In other words, the FA, which uses easily palpable landmarks,24 is close to parallel to the plane of a glenoid component placed in neutral position (perpendicular to the axis of the scapular body). Importantly, this near-parallel relationship, which exists in normal shoulders,25 persists in arthritic shoulders despite the significant bony changes that occur with severe glenohumeral arthritis.
There were no significant differences in reliability (intra-rater or inter-rater) between FA or GV for XR, CT or 3DCT. However, FA more accurately reflected the gold standard (3DCT) than GV and this was statistically significant (p < 0.0001). Retroversion is overestimated by GV by 11.172° on XR and 5.178° on CT. This is consistent with the current literature on GV measurements on XR/CT with errors of 5° to 15°15,16,19 and an overestimation of retroversion in 86% of cases and by a mean of 6.5°.21 The FA, in contrast, was within 2° and 1° of the gold standard on XR and CT, respectively.
A strength of the present study is the use of images of a series of patients who went on to TSA, rather than an artificial model. Our inclusion of all cases with adequate imaging is representative of average practice awaiting TSA. As a result, however, some of the results in the present study may differ slightly from those found in literature isolated to primary glenohumeral osteoarthritis. The mean glenoid version on 3DCT, for example, was 7.74° retroversion in the present study, which is slightly less than the previously reported 11° to 12.1° of retroversion.8,9 The inclusion of cases with AVN could have contributed to lowering the mean because AVN does not typically result in significant posterior wear. Additionally, the studied population involved a combination of dominant and nondominant shoulders. A greater proportion of nondominant shoulders in the present study compared to those reported in the literature could also contribute to a lowered mean retroversion.7
A limitation of the present study is the delay between XR and CT of 68 days on average. It is possible that glenoid wear progressed during the imaging delay even though this is unlikely to a significant degree given the chronic and nonweight-bearing nature of glenohumeral osteoarthritis. Radiographic follow-up studies in young patients with glenohumeral arthritis undergoing hemiarthroplasty have shown a rate of glenoid wear of 0.75 mm year−1 to 0.9 mm year−1 and increased glenoid erosion at a mean of 10.7 years.28–30 This delay between XR and CT would also have had no effect on the comparisons between CT and 3DCT. Another weakness is the need to superimpose images for the measurement of FA on CT. This is labour-intensive and a potential source of error that was eliminated as a result of the conversion of the imaging files to PDF. This was considered necessary for portability, as well as anonymity, and had no effect on measurements performed on XR or 3DCT.
The FA has been previously evaluated as an intra-operative guide.26 This may represent a very interesting future avenue of research given the improved accuracy of FA over GV, as shown in the present study. Current standard instrumentation deviates as much as 12° from planned glenoid component positioning1,31,32 and, even in experienced hands, only 82% of glenoids are placed between neutral version and 20° of retroversion.2 Negative clinical and radiological outcomes have been reported with >20° of retroversion1,2 and decreased TSA survival is a concern at >10° to 15° of retroversion.3,6,13 Le et al.26 tested a new glenoid aiming guide for TSA based on the FA and showed that it was both accurate and reliable in placing the glenoid within 5° of ideal version.26 These results are encouraging and the FA-based guide may show advantages over patient-specific or navigated instrumentation in terms of cost, ease-of use and speed.
Conclusions
FA showed comparable reliability to GV on XR, CT and 3DCT. However, FA was significantly more accurate than GV on both XR and CT when using 3DCT as the gold standard. Additionally, the FA was shown to be near-parallel to the ‘ideal’ glenoid plane, a relationship that is true in osteoarthritic as well as normal shoulders.25
The present study shows that the FA is simple, reliable and accurate. It uses easily palpable landmarks and has the potential for use in pre-operative planning, intra-operative guidance, and radiographic follow-up.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Institutional review board approval was obtained prior to commencement of the study. All patient information was removed/anonymized, and consent was deferred.
References
- 1.Gregory TM, Sankey A, Augereau B, et al. Accuracy of glenoid component component placement in total shoulder arthroplasty and its effect on clinical and radiological outcome in a retrospective, longitudinal, monocentric open study. PLoS ONE 2013; 8: e75791–e75791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moska MJ, Duckworth D, Matsen FA. Contrasting the position of prosthetic joint surfaces in successful and failed shoulder arthroplasties. Paper presented at the Seventh International Congress on Shoulder Surgery, Sydney, Australia, 1998:5–8.
- 3.Farron A, Terrier A, Buchler P. Risks of loosening of a prosthetic glenoid implanted in retroversion. J Shoulder Elbow Surg 2006; 15: 521–526. [DOI] [PubMed] [Google Scholar]
- 4.Hopkins AR, Hansen UN, Amis AA, Emery R. The effects of glenoid component alignment variations on cement mantle stresses in total shoulder arthroplasty. J Shoulder Elbow Surg 2007; 16: 90–95. [DOI] [PubMed] [Google Scholar]
- 5.Nyffeler RW, Sheikh R, Atkinson TS, Jacob HA, Favre P, Gerber C. Effects of glenoid component version on humeral head displacement and joint reaction forces: an experimental study. J Shoulder Elbow Surg 2006; 15: 625–629. [DOI] [PubMed] [Google Scholar]
- 6.Shapiro TA, McGarry MH, Gupta R, Lee YS, Lee TQ. Biomechanical effects of glenoid retroversion in total shoulder arthroplasty. J Shoulder Elbow Surg 2007; 16(3 Suppl): S90–S95. [DOI] [PubMed] [Google Scholar]
- 7.Matsumara N, Ogawa K, Kobayashi S, et al. Morphologic features of humeral head and glenoid version in the normal glenohumeral joint. J Shoulder Elbow Surg 2014; 23: 1724–1730. [DOI] [PubMed] [Google Scholar]
- 8.Moineau G, Levigne C, Boileau P, Young A, Walch G. The French Society for Shoulder and Elbow (SOFEC). Three-dimensional measurement of arthritis glenoid cavity morphology: feasibility and reproducibility. Orthop Trauma 2012; 985: 5139–5145. [DOI] [PubMed] [Google Scholar]
- 9.Friedman RJ, Hawthorn KB, Genez BM. The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am 1992; 74: 1032–1037. [PubMed] [Google Scholar]
- 10.Richetti ET, Hendel MD, Collins DN, Ianotti JP. Is premorbid glenoid anatomy altered in patients with glenohumeral arthritis. Clin Orthop Relat Res 2013; 471: 2932–2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sabesan VJ, Callanan M, Youderian A, Iannotti JP. 3D CR assessment of the relationship between humeral head alignment and glenoid retroversion in glenohumeral osteoarthritis. J Bone Joint Surg Am 2014; 96: e64–e64. [DOI] [PubMed] [Google Scholar]
- 12.Terrier A, Ston J, Larrea X, Farron A. Measurements of three-dimensional glenoid erosion when planning the prosthetic replacement of osteoarthritic shoulders. Bone Joint J 2014; 96B: 513–518. [DOI] [PubMed] [Google Scholar]
- 13.Ho JC, Sabesan VJ, Iannotti JP. Glenoid component retroversion is associated with osteolysis. J Bone Joint Surg Am 2013; 95: e82–e82. [DOI] [PubMed] [Google Scholar]
- 14.Ho JC, Youderian A, Davidson IU, Bryan J, Iannotti JP. Accuracy and reliability of postoperative radiographic measurements of glenoid anatomy and relationships in patients with total shoulder arthroplasty. J Shoulder Elbow Surg 2013; 22: 1068–1077. [DOI] [PubMed] [Google Scholar]
- 15.Budge MD, Lewis GS, Shaefer E, Coquia S, Flemming DJ, Armstrong AD. Comparison of standard two-dimensional and three-dimensional corrected glenoid version measurements. J Shoulder Elbow Surg 2001; 20: 577–583. [DOI] [PubMed] [Google Scholar]
- 16.Bryce CD, Davison AC, Lewis GS, Wang L, Flemming DJ, Armstrong AD. Two-dimensional glenoid version measurements vary with coronal and sagittal scapular rotation. J Bone Joint Surg Am 2010; 92: 692–699. [DOI] [PubMed] [Google Scholar]
- 17.Bokor D, O’Sullivan M, Hazan G. Variability of measurement of glenoid version on computed tomography scan. J Shoulder Elbow Surg 1999; 8: 595–598. [DOI] [PubMed] [Google Scholar]
- 18.Raymond AC, McCann PA, Sarangi PP. Magnetic resonance scanning vs axillary radiography in the assessment of glenoid version for osteoarthritis. J Shoulder Elbow Surg 2013; 22: 1078–1083. [DOI] [PubMed] [Google Scholar]
- 19.Hoenecke HR, Jr, Hermida JC, Flores-Hernandez CD, Lima DD. Accuracy of CT-based measurements of glenoid version for total shoulder arthroplasty. J Shoulder Elbow Surg 2010; 19: 166–171. [DOI] [PubMed] [Google Scholar]
- 20.Iannotti JP, Ricchetti ET, Rodriguez EJ, Bryan JA. Development and validation of a new method of 3-dimensional assessment of glenoid and humeral component position after total shoulder arthroplasty. J Shoulder Elbow Surg 2013; 22: 1413–1422. [DOI] [PubMed] [Google Scholar]
- 21.Nyffeler RW, Jost B, Pfirrmann CWA, Gerber C. Measurement of glenoid version: conventional radiographs versus computed tomography scans. J Shoulder Elbow Surg 2003; 12: 493–496. [DOI] [PubMed] [Google Scholar]
- 22.Bouchaib J, Clavert P, Kempf J-F, Kahn J-L. Morphological analysis of the glenoid version in the axial plane according to age. Surg Radiol Anat 2014; 36: 579–585. [DOI] [PubMed] [Google Scholar]
- 23.Rouleau DM, Kidder JF, Pons-Villanueva J, Dynamiditis S, Defranco M, Walch G. Glenoid version: How to measure it? Validity of different methods in two-dimensional computed tomography scans. J Shoulder Elbow Surg 2010; 19: 1230–1237. [DOI] [PubMed] [Google Scholar]
- 24.Braunstein V, Kirchoff C, Ockert B, et al. Use of the fulcrum axis improves the accuracy of true anteroposterior radiographs of the shoulder. J Bone Joint Surg (Br) 2009; 91B: 1049–1053. [DOI] [PubMed] [Google Scholar]
- 25.Braunstein V, Korner M, Brunner U, Mutschker W, Biberthaler P, Wiedemann E. The fulcrum axis: a new method for determining glenoid version. J Shoulder Elbow Surg 2008; 17: 819–824. [DOI] [PubMed] [Google Scholar]
- 26.Le SV, Conrad B, Wright TW. Application of the fulcrum axis to estimate the central scapular axis. J Shoulder Elbow Surg 2014; 23: 1143–1149. [DOI] [PubMed] [Google Scholar]
- 27.Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty 1999; 14: 756–760. [DOI] [PubMed] [Google Scholar]
- 28.Rispoli DM, Sperling JW, Athwal GS, et al. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am 2006; 88: 2637–2644. [DOI] [PubMed] [Google Scholar]
- 29.Ohl X, Nerot C, Saddiki R, Dehoux E. Shoulder hemi arthroplasty radiological and clinical outcomes at more that two years follow-up. Orthop Traumatol Surg Res 2010; 96: 208–215. [DOI] [PubMed] [Google Scholar]
- 30.Parsons IM, Millett PJ, Warner JJ. Glenoid wear after shoulder hemiarthroplasty: quatitative radiographic analysis. Clin Orthop Relat Res 2004; 421: 120–125. [DOI] [PubMed] [Google Scholar]
- 31.Hendel MD, Bryans JA, Barsoum WK, et al. Comparison of patient-specific instruments with standard surgical instruments in determining glenoid component position – a randomized prospective clinical trial. J Bone Joint Surg Am 2012; 94: 2167–2175. [DOI] [PubMed] [Google Scholar]
- 32.Walch G, Vezeridis PS, Boileau P, Deransart P, Chaoui J. Three-dimensional planning and use of patient-specific guides improve glenoid component position: an in vitro study. J Shoulder Elbow Surg 2015; 24: 302–309. [DOI] [PubMed] [Google Scholar]