Abstract
Background and Objectives:
Binge eating is prevalent and is associated with significant psychiatric and medical comorbidities. To date, the most effective psychological treatments for individuals who binge eat are not effective for all patients and they do not result in significant weight loss. Dual process theories suggest that implicit factors, such as attention bias, may influence behavior, even when the behavior is in opposition to long-term goals. Attention bias modification programs have been tested in other areas of psychopathology, and could be utilized to improve outcomes for people who binge eat. Thus, the aim of this open trial was to conduct a preliminary evaluation of an attention bias modification program (ABM-Food) designed to train attention away from food cues.
Methods:
Adults who binge eat and were overweight or obese enrolled in an 8-week ABM-Food program, which consisted of one session in the lab each week and two training sessions at home. Nine participants completed the ABM-Food training program and the post-treatment assessment, and 8 completed the 3-month post-treatment assessment. Results: Results showed that the ABM-Food program is a feasible and acceptable treatment for adults who binge eat. Initial effectiveness data showed decreases in weight, eating disorder symptoms, binge eating, loss of control and responsivity to food in the environment, as well as changes in attention bias. The majority of these effects remained at the 3-month follow-up time point.
Limitations:
This study is limited by the single-group open label trial, and the small sample size.
Conclusions:
This open trial provides initial evidence for the feasibility, acceptability and effectiveness of ABM-Food for individuals who binge eat and are overweight or obese.
Keywords: Binge eating, Obesity, Overeating, Attention bias, Attention bias modification, Weight loss
Overeating can be problematic, and is a factor in the development of obesity as well as in eating disorders. Recent data suggest that in the United States, 35.7 percent of adults are overweight and 33.1 percent are obese (Flegal, Carroll, Kit, & Ogden, 2012). By the year 2030, 51 percent of U.S. adults are predicted to be obese (Finkelstein et al., 2012). Obesity is associated with cardiovascular disease, Type II diabetes, cancer, osteoarthritis, psychological impairment, poor quality of life (Dixon, 2010) and all-cause mortality (Flegal & Kalantar-Zadeh, 2013). Rates of overeating, or eating beyond energy requirements, are especially high in overweight samples, with up to 80% of overweight adults regularly endorsing overeating (Thomas, Doshi, Crosby, & Lowe, 2011). Binge eating is a more extreme form of overeating, which is characterized by feelings of loss of control and the consumption of a large amount of food, typically within a discrete amount of time (American Psychiatric Association, 2013). Studies from treatment seeking populations using interview-based assessments suggest that 23%–46% of obese individuals report engaging in binge eating behavior (Spitzer et al., 1992; Dymek-Valentine, Rienecke-Hoste, & Alverdy, 2004; Gormally, Black, Daston, & Rardin, 1982; Marcus, Wing, & Lamparski, 1985). However, evidence from ecological momentary assessment studies suggests that binge eating among overweight individuals is more prevalent (66%–100%) than current research suggests (Greeno, Wing, & Shiffman, 2000; le Grange, Gorin, Catley, & Stone, 2001). Individuals with binge eating are at higher risk for psychiatric comorbidities, health problems, weight gain and poorer quality of life than individuals without binge eating (Rieger, Wilfley, Stein, Marino, & Crow, 2005; Wonderlich, Gordon, Mitchell, Crosby, & Engel, 2009). Not surprisingly, patients with binge eating have more modest weight losses during weight loss programs than those without binge eating (Grilo, Masheb, Wilson, Gueorguieva, & White, 2011; Reas & Grilo, 2008). Since binge eating is highly prevalent among obese individuals and a risk factor for poor treatment outcome, there is a critical need for new treatments designed to explicitly target overeating and binge eating. Directly treating overeating and binge eating could result in enhanced weight loss and weight loss maintenance in overweight adults.
The most well established treatments for individuals who binge eat include cognitive behavioral treatment (CBT) and interpersonal therapy (IPT) (Wilson, Wilfley, Agras, & Bryson, 2010; Devlin et al., 2005; Brownley, Berkman, Sedway, Lohr, & Bulik, 2007; Wilfley et al., 2002). CBT focuses on disrupting the restraint/binge cycle by improving maladaptive thoughts surrounding eating, shape, and weight, and encouraging healthy weight control behaviors (Iacovino, Gredysa, Altman, & Wilfley, 2012; Fairburn, Cooper, & Shafran, 2003). IPT addresses interpersonal difficulties that often accompany and may maintain the symptoms of Binge Eating Disorder (BED) (Rieger et al., 2010). These treatments produce remission rates of 40–60% and improvements in eating disorder psychopathology, but interestingly fail to produce significant weight loss (Grilo et al., 2011; Wilson et al., 2010). Conceptually, talk therapies such as CBT and IPT, assume that individuals can access and consciously control cognitive factors that contribute to and maintain binge eating behaviors. Dual process theories (Kahneman, 2003; Strack & Deutsch, 2004) suggest that implicit processes (i.e. attention and approach biases to food) may exert control over behavior, even when the behavior is in opposition to long-term goals. These implicit processes may not be adequately addressed in CBT or IPT, and may be contributing to the persistence of binge eating.
Calorically-dense foods cues can capture attention (Harrar, Toepel, Murray, & Spence, 2011), and certain individuals, such as those who are overweight or obese or who binge eat, could exhibit hyper-reactivity to the salient properties of food coupled with motivations to engage in appetitive behaviors (Davis et al., 2009). In the brain, responsiveness to food and the general processing of reward and pleasure is mediated by dopamine in the mesocorticolimbic system (Volkow, Wang, Fowler, Tomasi, & Baler, 2012; Berridge, Ho, Richard, & DiFeliceantonio, 2010). Dysregulated dopamine-based reward circuitry has been implicated in both binge eating and obesity (Volkow et al., 2012; Davis et al., 2013). Incentive sensitization theory (Berridge, 1996, 2009; Robinson & Berridge, 1993) suggests that incentive salience (i.e. drive to eat, wanting of food) develops through repeated pairings of food cues with food intake in vulnerable individuals. Over time, through associative conditioning, dopamine-based reward circuitry becomes hyper-sensitized to stimuli associated with food, resulting in biased processing of food-related cues. Food cues become attention grabbing and hyper-salient, triggering motivational states of craving, biased attention in the salience network, and increase the likelihood of consumption (Nijs & Franken, 2012). If cognitive processes are biased towards food temptations, it could become increasingly difficult to ignore and resist these temptations, even when trying to exert behavioral control.
The research on attention bias to food cues and binge eating is in its infancy, relative to other disorders, such as anxiety. It is important to note that research on individuals who are obese without diagnosed BED indicates that weight exerts a differential influence on attention biases (Doolan, Breslin, Hanna, & Gallagher, 2015). Data on overweight patients with BED also shows that they have impaired attention biases compared to obese patients without BED. To date, there are five studies that have directly compared overweight BED participants to overweight non-BED participants (Svaldi, Tuschen-Caffier, Peyk, & Blechert, 2010; Schag et al., 2013; Schmitz, Naumann, Trentowska, & Svaldi, 2014; Svaldi, Naumann, Trentowska, & Schmitz, 2014; Seeley et al., 2007). Two studies evaluated initial orientation to food cues; one found that both BED and non-BED groups initially fixated on food versus neutral stimuli (Schag et al., 2013), while the other found an early stimulus orientation effect only among BED participants compared to overweight females without BED (Schmitz et al., 2014). BED participants correctly identified food stimuli targets presented shortly after neutral targets more than overweight non-BED controls, demonstrating increased (biased) food perception in BED (Svaldi et al., 2014). Two studies found differences in sustained attention processes among women with BED versus overweight women without BED using event related potentials and eye tracking methods (Svaldi et al., 2010; Schag et al., 2013), suggesting potentially heightened and longer attention processing of food stimuli. Similarly, one study showed individuals with BED had more difficulties disengaging from and inhibiting responses to food stimuli (Seeley et al., 2007). Furthermore, one study using the antisaccade task indicated that individuals with BED might be more “visually impulsive,” suggesting less control over their attention, than both obese non-BED and healthy weight participants (Schag et al., 2013). Interpretation of this research is limited by differing measures (eye tracking (Schag et al., 2013), antisaccade (Schag et al., 2013), ERP (Svaldi et al., 2010), clarification task (Schmitz et al., 2014), spatial cueing task (Schmitz et al., 2014)), small sample sizes, and varying motivational states (hunger vs satiety). However, this emerging body of data suggests that attention biases to food could be along a spectrum, with healthy weight participants having the least impaired and overweight patients with BED having the most impaired.
Considering that attention bias may play a role in maintaining the underlying motivational salience of food cues, it is possible that by reducing attention bias to approach foods, the drive to eat and binge eating will decrease. Cognitive researchers developed computer programs to train attention resources away from salient stimuli by implicitly training attention away from salient stimuli toward neutral stimuli. These Attention Bias Modification Programs (ABM) theoretically improve an individual’s ability to disengage attention from stimuli (MacLeod & Clarke, 2015; Kuckertz & Amir, 2015). ABM programs have been examined primarily in anxiety disorders and have been related to changes in activation of the prefrontal cortex to emotional stimuli, implying improved top down control of attention as a result of training (Browning, Holmes, Murphy, Goodwin, & Harmer, 2010). More recently, ABM programs have been developed for appetitive stimuli, including substance use disorders (McGeary, Meadows, Amir, & Gibb, 2014; Lopes, Pires, & Bizarro, 2014; Schoenmakers et al., 2010). However, there is very little research on ABM for food.
Meta analyses show that ABM programs have reliable effects in changing attention bias to engage salient cues in anxiety and depression (Beard, Sawyer, & Hofmann, 2012; Heeren, Mogoase, Philippot, & McNally, 2015; Linetzky, Pergamin-Hight, Pine, & Bar-Haim, 2015; Mogoaşe, David, & Koster, 2014). At this time, there are too few studies to conduct metanalyses for appetitive stimuli. Interestingly, recent research suggests that the direction of the contingency between probes and cues may not be as important as originally thought (Heeren, Mogoase, McNally, Schmitz, & Philippot, 2015; Klumpp & Amir, 2009). For example, one study assigned individuals with social anxiety disorder to one of three ABM conditions; training toward non-threat, training toward threat, or no-contingency condition (Heeren et al., 2015b). All groups showed decreases in self-report and behavioral indices of anxiety, suggesting that training attention in general may strengthen top-down attention control which can have an impact on anxiety. These and other questions will need to be evaluated in ABMs which target attention bias to food cues.
Only a few studies have evaluated ABMs with overeating and/or binge eating. Using a dot probe training, undergraduate women who like chocolate were trained to direct their attention toward or away from pictures of chocolate (Kemps, Tiggemann, Orr, & Grear, 2014). Attention biases increased in the ‘attend’ group and decreased in the ‘avoid’ group, and participants trained to avoid ate less chocolate on a taste test than those trained to attend. Using the same methodology, a single session training was compared with five weekly trainings (Kemps, Tiggemann, & Elford, 2015). Results showed decreased chocolate consumption for those trained to avoid in the 5-week training group only. Further training effects were maintained for 24 h and one week following the 5-week training and not the single session training, suggesting a need for repeated training. Similarly, in healthy weight females, modification of attention to chocolate using an anti-saccade training showed that participants trained to attend chocolate ate more chocolate than those trained to attend to shoes; however this effect was only apparent among those with high accuracy on the task (Werthmann, Field, Roefs, Nederkoorn, & Jansen, 2014). In another study, college women were either trained toward unhealthy food or toward healthy food using the dot probe task (Kakoschke, Kemps, & Tiggemann, 2014). Findings indicated that participants who were trained to attend to healthy food cues demonstrated an increased bias for those cues, and ate relatively more healthy snacks compared to the ‘unhealthy’ group on a subsequent taste test. We recently published a pilot study evaluating a one-session ABM training with 29 obese 8e12 year old children (Boutelle, Kuckertz, Carlson, & Amir, 2014). Our data showed that children who participated in one session of ABM training, compared to children who completed an attention control, decreased their attention bias toward food related stimuli and showed differential changes in overeating in the laboratory. Interestingly, the children in the control condition ate more in a laboratory evaluation of eating in the absence of hunger after completing the attention control computer program, while children in the ABM-Food training did not increase their overeating. A recent open label trial with 30 individuals with high trait food cravings using an approach-avoidance paradigm over 5 weeks showed that ten 15-min trainings reduced approach biases to food and reduced trait and cueelicited food craving (Brockmeyer, Hahn, Reetz, Schmidt, & Friederich, 2015). We believe that these programs will be more effective with adults who binge eat, because these individuals tend to have attention biases to food above and beyond those who are overweight, have more frequent and extreme binges, and are more distressed by their binge eating.
1. Method
1.1. Study design and procedure
This study is an open label trial with one treatment condition, adopting a single group pre–post design, to test the feasibility, acceptability and initial effectiveness of an ABM program for binge eating. Participants completed an initial screening for weight and binge eating over the phone. After the initial screening, participants attended an assessment visit and then an initial orientation to the program where they were taught about the role of food cue responsivity in overeating and how to work the computer program. Following the orientation visit, the participants attended in person visits in the clinic once a week to complete the ABM training and completed two trainings at home for a total of 8 weeks. Following the 8 weeks of ABM trainings, participants attended a post-treatment assessment and a 3-month follow-up assessment. Assessments included measurements of attention bias, weight, eating disorder symptoms, cravings, and food-cue reactivity. The post-treatment assessment also included an acceptability survey.
1.2. Participants
We recruited adult participants who were overweight or obese from listservs and advertisements in the community of San Diego, CA. The inclusion criteria for this study included: 1) overweight or obesity (25 < BMI < 40), 2) a minimum of 1 binge episode per week (by self-report). Exclusion criteria were assessed by self-report and included: 1) additional psychiatric disorders (including depression, anxiety, bipolar disorder, autism, language or speech disorder, severe brain injury, mental retardation, or psychosis) that would influence participation or limit ability to comply with the program 2) diagnoses of a serious physical disease which can influence weight, 3) medications that would influence weight and eating, 4) presence of another eating disorder (bulimia nervosa). Of note, the individual’s level of binge eating was not assessed using clinical interviews.
1.3. Procedure
Participants who responded to advertisements were screened by phone for eligibility criteria by the research coordinator. All participants attended an initial assessment that included a clinical interview, behavioral tasks, anthropomorphic measures, and self-report questionnaires. After the baseline assessment, participants returned for the first training visit and were given an orientation to the theoretical basis underlying attention training as well as the ABM-Food computer program. After completion of the 8 weeks of training (once a week at the clinic, twice a week at home), all participants attended a post-treatment assessment and a 3-month follow-up assessment.
1.4. Intervention
For this study, we used the Attention bias modification (ABM-Food) that was similar to our previous study with children (Boutelle et al., 2014). ABM-Food consisted of 24 word pairs consisting of matched food words (i.e. cake) and neutral words (i.e. pencil). Words were matched on length and readability. We chose food words rather than pictures as words have been shown to yield stronger training effects compared to picture stimuli (Hakamata et al., 2010). Participants were presented with 192 trials that consisted of balanced combinations of a probe type (“E” or “F”) and position of probe on the screen (top of bottom). At the beginning of each trial, participants were asked to focus their attention on a fixation cross, which appeared in the center of the screen for 500 ms. The fixation cross then disappeared and a word pair was presented vertically for 500 ms, following which a letter probe appeared in the location of the neutral word. The probe appeared on the screen until the participant identified the probe type. Participants were instructed to respond to the probe as quickly and as accurately as possible by pressing either the left mouse button (“E”) or right mouse (“F”) button to identify the letter. A 500 ms interval of a blank screen was presented before the onset of the next trial. We did not instruct participants to direct their attention away from the food words; instead, the position of the neutral word on the screen indicated the position of the subsequent probe, which acted as a contingency reinforcement such that the probe always appeared in the position of the neutral word (training attention away from food cues and toward neutral cues).
1.5. Clinic visits
Participants came into clinic one time per week to complete the training program. The first visit included an orientation to the theory behind the relationship between attention bias, incentive salience and binge eating. At this first visit, the participant was taught how to use the ABM-Food program and the ABM-Food program was loaded on his/her laptop. At the following 7 meetings, participants came into the clinic, completed an ABM-Food training, and were given a handout regarding cue reactivity and attention bias (for engagement and retention reasons). The topics included 1) How environment and biology lead to overeating, 2) The neurobiology of overeating, 3) How food cues in the environment can trigger cravings, 4) Marketing strategies and food cravings, 5) Mood and cravings, 6) Boredom and cravings. The handouts were not reviewed or discussed. All participants were instructed to complete the home sessions of ABM-Food at least twice during the week. To assure compliance, the participants were instructed to email the file of their completed training sessions to the research assistant once per week.
1.6. Measures
1.6.1. Eating disorders examination (EDE)
The EDE is a semi-structured interview-based eating disorder assessment (Cooper & Fairburn, 1987). The EDE assesses the frequency and occurrence of disordered attitudes and behaviors during the past 28 days related to eating, body-shape and weight, and diagnoses. Questions pertaining to objective binge episodes (consuming an objectively large amount of food with a sense of loss of control) was used for the purposes of this study. The EDE has demonstrated high internal consistency, discriminative validity, concurrent validity, and test-retest reliability (Cooper & Fairburn, 1987; Cooper, Cooper, & Fairburn, 1989; Grilo, Masheb, Lozano-Blanco, & Barry, 2004; Berg, Peterson, Frazier, & Crow, 2012). All interviews were completed by graduate students trained to competency and supervised by a Ph.D. level psychologist.
1.6.2. Eating disorders examination-questionnaire (EDE-Q)
The EDE-Q (Fairburn & Beglin, 1994) is a 28-item self-report questionnaire assessing disordered eating attitudes and behaviors over the past 28 days. It produces four subscales that reflect disordered eating attitudes: dietary restraint, eating concern, weight concern, and shape concern, as well as a global score (the average of the four subscale scores). Higher scores on the global score are indicative of greater overall eating psychopathology. The EDE-Q has demonstrated good internal consistency and test-retest reliability and concurrent validity (Berg et al., 2012; Mond, Hay, Rodgers, Owen, & Beumont, 2004). We report the total EDE-Q score as an indication of overall eating disorder symptoms. In the current study, internal consistency (Cronbach’s alpha) was 0.89 for the total score, 0.67 for restraint, 0.73 for eating concern, 0.66 for shape concern, and 0.63 for weight concern.
1.6.3. Binge eating scale (BES)
The BES (Gormally et al., 1982) is a 16-item questionnaire developed to assess the severity of binge eating in a continuous scale. The BES measures the behavioral features (ex. eating large amounts of food), cognitions, and emotions (ex. loss of control, guilt) related to binge eating. The BES produces a total score, with higher scores indicating increased binge eating severity. The scale has demonstrated construct validity and internal consistency (Gormally et al., 1982). Cronbach’s alpha for the BES total score was 0.88 in the present study.
1.6.4. Food cravings questionnaire-trait (FCQ-T)
The FCQ-T (Nijs, Franken, & Muris, 2007) is a 21-item self-report questionnaire designed to assess general (non-specific) desires to eat. It is composed of four scales: preoccupation with food (obsessive thoughts regarding food and eating), loss of control (tendency toward disinhibited behavior in response to food cues), positive outcome expectancy (expectancy that eating is positively or negatively reinforcing), and emotional craving (tendency to crave food when experiencing negative emotions). The FCQ-T has shown adequate construct validity and test-retest reliability (Nijs et al., 2007). In the current study, Cronbach’s alphas were 0.95 for preoccupation with food, 0.90 for loss of control, 0.91 for positive outcome expectancy, and 0.92 for emotional craving.
1.6.5. Power of food scale (PFS)
The PFS (Lowe et al., 2009; Cappelleri et al., 2009) is a 15-item self-report questionnaire that measures the drive to consume, rather than consumption of, palatable foods in the environment, at three levels of food proximity (food available, food present, and food tasted). It was originally validated in a sample of undergraduate students (Lowe et al., 2009) and has adequate internal consistency, convergent validity, and testeretest reliability (Lowe et al., 2009; Cappelleri et al., 2009). The total PFS scale is reported in this study. In the present study the Cronbach’s alphas were 0.90 for food available, 0.80 for food present, 0.85 for food tasted, and 0.89 for the total score.
1.6.6. Attention bias
The dot probe paradigm was used to assess attention bias. Participants were presented with 276 trials comprised of 24 food/neutral word pairs matched for length and readability. The assessment consisted of equal number of trials for probe type (“E” or “F”), location of probe (top or bottom), and location of food word (top or bottom). None of the assessment words were used in the ABM training program. Response latencies were recorded from the onset of the probe (“E” or “F”) to the button press. We then computed a food bias score by subtracting the response latency for probes following food related words from the response latency for probes that followed neutral words. Larger positive bias scores indicate an attention bias toward food related words, while larger negative bias scores indicate an attention bias away from food related words.
1.6.7. Stroop
The original Stroop task (Stroop, 1935) is a well-established measure of cognitive interference that assesses information processing biases. The modified Food Stroop measures differences in reaction times to naming the color of the text of food-related versus neutral words. Slower naming of food words are presumed to measure attention biases for food, because attention towards food words may interfere with the primary color-naming task. Twenty highly palatable food words (eg. cake, chips) and twenty neutral words (eg., chalk, desk) were selected by investigators. Food words and neutral words were matched on word length. The task began with a practice block, followed by 4 experimental blocks of 20 trials, during which each food and neutral word was presented four times in a different color on each trial. Words were presented in the center of the computer screen in one of four colors (yellow, red, green, blue). The inter-trial interval was 3000 ms. Participants were instructed to press the key that corresponded to the color of the word. If there was no response within 2000 msec after word onset, the next word was presented after 1000 ms. Response time and accuracy were measured. Response time of accurate trials to food words were compared to response time of accurate trials to neutral words and are presented.
1.6.8. Anthropometry
Participants’ height was measured using a standard stadiometer in duplicate and weight was measured in duplicate on a calibrated slide scale without jackets, outerwear or shoes. The average of the two values was used for analysis. Participants’ heights and weights were translated to BMI (kg/m2).
1.6.9. Acceptability questionnaire
An acceptability questionnaire was given at the post-treatment time point that included questions about how much the participants liked the program on a 5 point rating scale (“How much did you like the 12 week ABM program?” from 1 “Didn’t like” to 5 “Loved it”, how helpful the participants found the program” (“How helpful did you find the ABM program?” from 1 “Not at all helpful” to 5 “Extremely helpful”, if they would recommend the program to others (“I would recommend the program to others” from 1 “Strongly disagree” to 5 “Strongly agree”), and an open ended question asking what changes they noticed, if any.
1.7. Analyses
For the attention bias data, we removed incorrect response latencies and dropped the first two trials from each participant’s scores. Mean response latency was calculated for each participant for probes replacing food words and neutral words before and after training. Consistent with previous research, incorrect responses were removed from analysis (22.2% of trials). Trials with extreme values (<200 ms or > 2000 ms) were also removed (3.2% of trials).
We compared pre, post, and three-month follow-up assessment measures using linear and generalized linear mixed-effects models for repeated measures. All models included dummy-coded effects for comparing each assessment to corresponding baseline values. Additionally, we evaluated relationships between change in the main outcome variables (BMI and binge eating) and change in measures of attention and food cue reactivity.
2. Results
2.1. Feasibility and acceptability
We enrolled 15 participants who were overweight or obese, and 9 completed the ABM training program and the post-treatment assessment. Participants who withdrew from treatment were not significantly different than participants who completed the intervention (see Table 1). Unfortunately, none of the participants who withdrew gave feedback as to why they did not complete the protocol. Of the 6 participants who did not complete the program, one completed the first session, three completed the first two sessions, and two participants completed four sessions. See Fig. 1 for a flow chart of participants.
Table 1.
Demographics of the sample
| Full sample (n = 15) |
Participants who completed the intervention (n = 9) |
Participants who withdrew during the intervention (n = 6) |
|
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Body Mass Index (kg/m2) | 34.88 (4.83) | 33.74 (5.25) | 36.17 (4.26) |
| Age | 51.41 (11.12) | 54.22 (8.97) | 48.25 (13.00) |
| Percent Female | 88% | 100% | 75% |
| White Non-Hispanic | 80% | 89% | 67% |
Fig. 1.
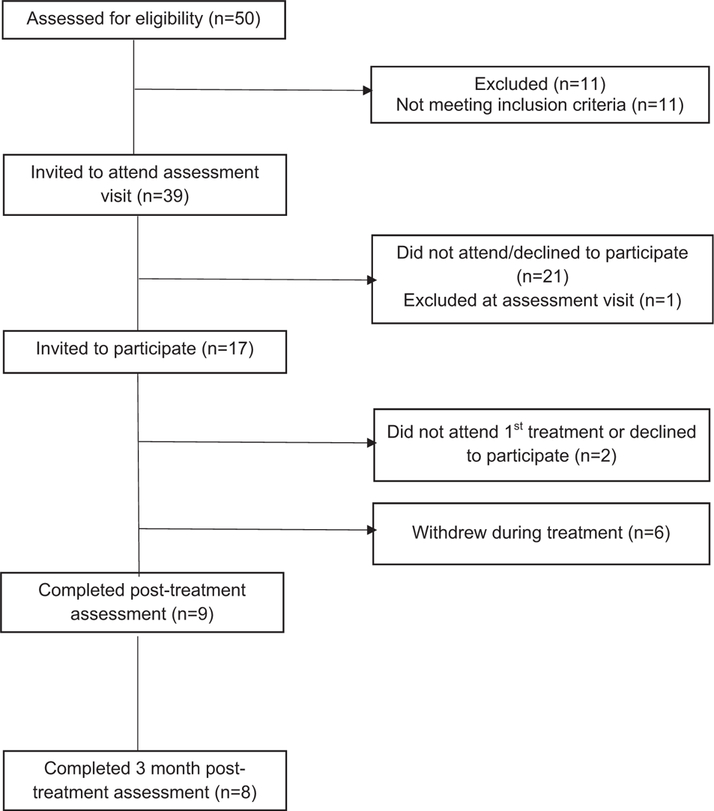
Subject enrollment and participation.
The participants who completed the program were an average age of 54.2 years, 100% were women, with a mean BMI of 33.7 (See Table 1). On average, participants who completed the program completed 99% of the expected 8 visits in the lab and 74% of the 16 visits at home. Participants had a mean accuracy rate of 75% at baseline, 79% at post-treatment and 85% at 3-month follow-up.
In terms of acceptability, 5 out of 9 of the participants liked the program; 6 out of the 9 participants said they found the program to be “moderately”, or “very”, or “extremely” successful in reducing their binge eating. In terms of changes the participants noticed in their eating behavior after completing the program, four said they became more aware and mindful of their eating habits.
2.2. Initial effectiveness
Table 2 presents the initial effectiveness data on binge eating, eating disorder symptoms, weight, attention bias, power of food and food cravings at baseline, post-treatment, and 3-months post-treatment. There were significant within subject treatment effects from baseline to post-treatment with reductions in total binge episodes, binge eating scale scores, eating disorder symptoms and on BMI (p’s < 0.05). The weight loss and BMI change data for the nine participants is shown in Fig. 2. These effects were largely maintained through the follow-up assessment although some effects fell below traditional levels of statistical significance. We also observed significant shifts in attention bias towards food, decrease in power of food, decreased loss of control with food cravings, and a trend toward decreased emotional craving (p’s < 0.05e0.07). These changes also were largely maintained through the 3-month follow-up assessment with two of the four retaining statistical significance and all four suggesting only slightly reduced effects. We did not observe significant changes in objective bulimic episodes, and the Food Stroop measure of attention bias (p’s > 0.05).
Table 2.
Baseline, post-treatment and 3-month follow-up scores on study outcome variables (n = 9).
| Observed measurements |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline |
Post-treatment |
3-month follow-up |
Post-treatment (95% CI) |
3-month follow-up (95% CI) |
|||||
| Mean (SD) | Mean (SD) | Mean (SD) | Effect | Lower | Upper | Effect | Upper | Lower | |
| Binge eating symptoms | |||||||||
| Total Binge Episodesa | 10.89 (9.62) | 3.33 (6.78) | 1.88 (3.76) | −1.50** | −1.51 | −1.49 | −1.91** | −1.93 | −1.90 |
| Binge Eating Scale | 24.33 (8.87) | 15.89 (6.19) | 17.62 (10.47) | −8.44* | −14.11 | −2.77 | −6.35* | −12.25 | −0.45 |
| Eating Disorder symptoms | |||||||||
| EDE-Q-Global score | 3.88 (0.88) | 2.98 (1.27) | 2.74 (1.12) | −0.90** | −1.39 | −0.42 | −1.08** | −1.58 | −0.57 |
| Weight | |||||||||
| Body Mass Index (kg/m2) | 33.74 (5.25) | 32.97 (5.17) | 32.15 (4.87) | −0.77* | −1.45 | −0.08 | −0.77* | −1.49 | −0.06 |
| Attention Bias | |||||||||
| Dot-probe: Food bias | −23.00 (27.74) | 35.06 (62.90) | 20.91 (34.30) | 58.43* | 17.97 | 98.89 | 44.44 | 2.65 | 86.23 |
| Food Stroop difference score | 34.00 (38.12) | 16.77 (30.36) | 35.60 (60.60) | −17.22 | −52.46 | 18.01 | 2.23 | −34.31 | 38.76 |
| Food cue reactivity | |||||||||
| Power of Food Scale-Food Available | 3.78 (1.21) | 3.11 (1.20) | 2.52 (1.11) | −0.67* | −1.27 | −0.06 | −1.16** | −1.79 | −0.53 |
| Power of Food Scale-Food Present | 4.33 (0.73) | 3.33 (0.95) | 3.13 (1.42) | −1.00* | −1.75 | −0.25 | −1.16* | −1.94 | −0.38 |
| Power of Food Scale-Food Tasted | 3.03 (0.93) | 2.56 (0.98) | 2.15 (0.74) | −0.57* | −0.92 | −0.21 | −0.74** | −1.12 | −0.37 |
| Food Cravings | |||||||||
| Preoccupation w/Food | 3.98 (1.57) | 3.44 (1.04) | 3.06 (1.28) | −0.54 | −1.31 | −0.23 | −0.81 | −1.62 | −0.01 |
| Loss of Control | 4.46 (1.21) | 3.74 (0.79) | 2.92 (1.06) | −0.72* | −1.25 | −0.20 | −1.39** | −1.94 | −0.85 |
| Emotional Craving | 4.44 (1.13) | 3.78 (1.08) | 3.69 (1.47) | −0.67 | −1.33 | −0.00 | −0.61 | −1.30 | 0.09 |
| Positive Expectancy | 2.69 (1.09) | 2.80 (0.94) | 2.43 (0.68) | 0.11 | −0.56 | −0.78 | −0.07 | −0.65 | 0.50 |
p < 0.05
p < 0.01
= over past 28 days.
Fig. 2.
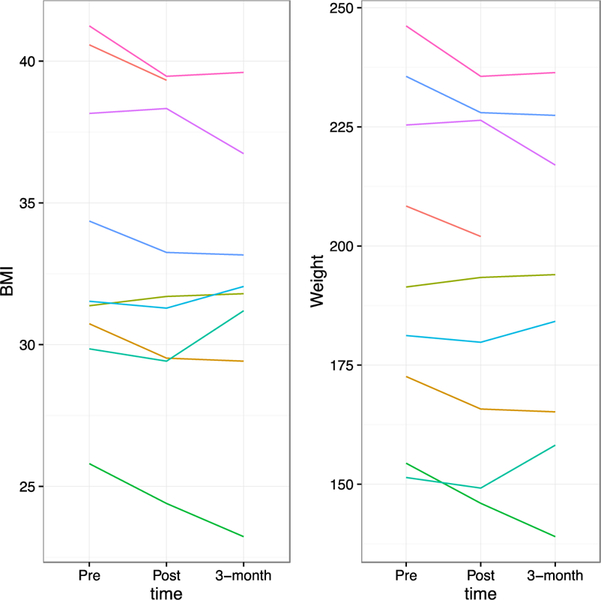
Individual participant’s weight and BMI data at baseline, post-treatment and 3-months post-treatment.
The number of ABM-Food sessions completed (median = 20 sessions, 25th–75th = 16–22 sessions) was positively associated with observed decreases in BMI at the 3-month follow-up (number of sessions*time b = –0.11; SE = 0.05, p = 0.05), but was not as strongly related at the 12-week assessment given high degree of variability (number of sessions*time = –0.06; SE = 0.05, p = 0.28). The average BMI loss for those with less than 20 sessions was 0.61 (sd = 0.71) and –0.17 (sd = 1.29) for the post and 3-month assessments, and for those with more than 20 sessions was –0.90 (sd = 0.82) and –1.28 (sd = 1.30).
We also examined change in bias scores among those above compared to those below a median split for weight loss at the end of treatment (BMI decrease≥1.1). We used linear mixed effects models to assess bias measures at two time points, post-treatment and 3-month follow-up. In the model we added a covariate term for baseline level of bias and a dummy coded index that identified participants either above or below the median weight lost at the end of treatment. We did not observe statistically significant differences in changes in bias scores among participants above or below the median for weight lost, (p = 0.30). Average increases in bias scores from baseline values were 68.5 (sd = 71.1) and 54.2 (sd = 24.8) for participants above and below the median for weight lost, respectively. These results suggest a potential greater increase in bias among participants that had greater degree of weight loss (within subjects effect size d = |(68.5–54.2)|/27.74 = 0.52).
3. Discussion
This is the first study to evaluate the feasibility, acceptability and initial effectiveness of a computer program targeting changes in attention bias to food cues with adults who are overweight or obese and who binge eat. We found that a minimal intervention, such as an ABM-Food program, was feasible and acceptable to the majority of the participants. Furthermore, this case series suggests that 8 weeks of ABM-Food, on average, resulted in weight loss, changes in attention bias, decreases in eating disorder symptoms, and decreases in the influence that the food environment has on them. It is especially remarkable that 5 participants lost more than 6 pounds over the 8 weeks of the ABM training, with no diet or exercise recommendations. We hypothesize that the ABM-Food training program functions by decreasing attention resources to food cues, resulting in an improved ability to inhibit binge eating and overeating. However, it must also be considered that training attention in general may have improved executive control of attention and behavior, which also could have contributed to the results in this study.
Interestingly, the dot probe measurement of attention bias moved from a higher level of attention to neutral cues at baseline to greater attention to food cues at post-treatment, which was consistent for all of the cases. However, the Food Stroop measure of attention bias moved from greater attention to food cues to less attention to food cues, although it was not statistically significant. The Food Stroop results are more consistent with our hypothesis, while the dot probe results are the opposite of what we expected. It is important to recognize that attention is a complex process and neither the dot probe nor the Stroop can capture all of the intricate components of attention. The available research suggests that individuals who are overweight/obese with BED exhibit increased attention processing and engagement with food stimuli above and beyond their obese counterparts. However, as we learn more about attention biases, we are beginning to understand the nuances, and it is possible that the changes on the dot probe assessment could be consistent with an approach-avoid pattern of attention (Werthmann et al., 2011). Additionally, it is possible that the participants were initially avoiding directing attention resources to food cues at baseline, as it was their only coping mechanism. We may have trained them to further avoid, which may have made this coping mechanism more effective, resulting in the changes in the dot-probe measurements. Finally, our dot probe measure assessed reaction time at 500 ms, which is neither a measure of initial orientation nor sustained attention processes. Future studies should evaluate assessments of orientation and sustained attention, to assist in understanding the complexities of binge eating, weight and attention bias to food cues.
Noteably, participants in this study not only decreased their binge eating, but they also decreased their weight. On average, participants in this study lost 4.5 pounds over 8 weeks (range = +2 to –12.6). If this rate of weight loss continued for a year, the resulting weight loss would surpass studies of behavioral weight loss with participants who binge eat, also surpassing the observed weight losses in CBT and IPT (Grilo et al., 2011). This is remarkable for a number of reasons. The ABM program did not include a diet or physical activity component; we specifically targeted only attention bias to food. Our hypothesis is that the decrease in weight could be attributed to decreased caloric consumption associated with the changes in attention bias, although we did not measure nutritional intake in this study. Although not conclusive, the reductions in binge eating and weight loss resulting from the 8 week ABM-Food program support the potential impact of targeting implicit cognitive mechanisms, such as attention bias, to develop novel interventions.
As in all studies, there are limitations that must be noted. First and foremost, this is a case series, and there is no control group, so we cannot rule out a placebo effect, or compare the effects of an attention control without a training contingency. Improvements on some outcomes could have reflected test-retest effects, although test-retest reliability is acceptable for EDE and self-report measures used in this study (Grilo et al., 2004; Nijs et al., 2007; Lowe et al., 2009; Reas, Grilo, & Masheb, 2006; Timmerman, 1999). Additionally, participants were informed of the purpose of the study. A recent study found that informing participants of training contingencies and encouraging respective attentional selectivity may diminish the impact on subsequent anxiety reactivity, while still moderating attention bias on the dot-probe (Grafton, Mackintosh, Vujic, & McLeod, 2014). While we cannot rule out the possibility that experimental demand influenced the pattern of results, participants were not explicitly informed of the probe contingencies, nor were they instructed to actively direct attention away from food cues during training. We hypothesize that these factors decreased the likelihood of participants’ understanding of demand characteristics, and specifically how to execute such demands via task performance. Of note, CBT and IPT for binge eating, and behavioral weight loss for obesity, target overeating and/or binge eating explicitly. If the results of this ABM study were due to demand characteristics, the same demand characteristics would function in talk therapies.
Importantly, there was significant dropout in this study. We hypothesize that the ABM-Food program was too novel for those who wanted more traditional binge eating or weight loss programs, was not engaging enough, was perceived as having low face validity, or was not effective in those who withdrew. It is possible that participants who withdrew did not accept the rationale of the ABM-Food training program and its potential impact on binge eating and weight loss, reducing motivation to continue in the program. More research is needed to investigate whether and to what extent informing participants about the task (purpose, probe contingencies) influences task performance on training attention bias to food cues. Efforts will need to be directed to identifying how to engage participants without influencing demand characteristics, which is incredibly challenging when recruiting clinical populations who want to reduce binge eating and/or weight. However, despite the inherent limitations of a case series, these data suggest that the utilization of ABM-Food to decrease binge eating and weight is plausible and worth additional larger-scale trials.
This is the first study to evaluate an ABM-Food program to decrease binge eating and weight in individuals who are overweight/obese. The ABM-Food intervention is a minimal intervention, and includes 24 10-min computer sessions over 8 weeks, with the majority at home. These sessions were completed mostly accurately, were acceptable to participants, and required minimal time, training and resources from clinicians and participants. Given these features, ABM interventions could have the potential to impact a greater proportion of the adults who binge eat if these studies are replicated in randomized controlled trials. As discussed, many participants do not respond to CBT or IPT and the majority of participants in CBT or IPT do not lose weight, and still experience the medical comorbidities associated with obesity. Brief, easily-disseminated cognitive bias modification interventions may reduce barriers to accessing evidence-based care for binge eating, and provide additional treatment options to overweight participants with binge eating that could result in weight loss.
Acknowledgements
This project was funded by K02HL112042 to the first author and by R01MH087623 and R34 MH073004 to the last author.
Dr. Amir is part owner of a company that market anxiety relief products. The procedures used in the current study are not related to the products marketed by that company.
There are no additional acknowledgements.
Footnotes
None of the other authors have anything to declare.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington DC: Author. [Google Scholar]
- Beard C, Sawyer AT, & Hofmann SG (2012). Efficacy of attention bias modification using threat and appetitive stimuli: a meta-analytic review. Behavior Therapy, 43(4), 724–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, & Crow SJ (2012). Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. International Journal of Eating Disorders, 45(3), 428–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC (1996). Food reward: brain substrates of wanting and liking. Neuroscience & Biobehavioral Reviews, 20(1), 1–25. [DOI] [PubMed] [Google Scholar]
- Berridge KC (2009). ‘Liking’ and ‘wanting’ food rewards: brain substrates and roles in eating disorders. Physiology & Behaviour, 97(5), 537–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC, Ho CY, Richard JM, & DiFeliceantonio AG (2010). The tempted brain eats: pleasure and desire circuits in obesity and eating disorders. Brain Research, 1350, 43–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutelle KN, Kuckertz JM, Carlson J, & Amir N (2014). A pilot study evaluating a one-session attention modification training to decrease overeating in obese children. Appetite, 76, 180–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockmeyer T, Hahn C, Reetz C, Schmidt U, & Friederich H-C (2015). Approach bias modification in food cravingda proof-of-concept study. European Eating Disorders Review, 23(5), 352–360. [DOI] [PubMed] [Google Scholar]
- Browning M, Holmes EA, Murphy SE, Goodwin GM, & Harmer CJ (2010). Lateral prefrontal cortex mediates the cognitive modification of attentional bias. Biological Psychiatry, 67(10), 919–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownley KA, Berkman ND, Sedway JA, Lohr KN, & Bulik CM (2007). Binge eating disorder treatment: a systematic review of randomized controlled trials. International Journal of Eating Disorders, 40(4), 337–348. [DOI] [PubMed] [Google Scholar]
- Cappelleri JC, Bushmakin AG, Gerber RA, Leidy NK, Sexton C, Karlsson J, et al. (2009). Evaluating the Power of Food Scale in obese subjects and a general sample of individuals: development and measurement properties. International Journal of Obesity, 33(8), 913–922. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Cooper PJ, & Fairburn CG (1989). The validity of the eating disorder examination and its subscales. The British Journal of Psychiatry, 154, 807–812. [DOI] [PubMed] [Google Scholar]
- Cooper Z, & Fairburn C (1987). The eating disorder examination - a semistructured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders, 6(1), 1–8. [Google Scholar]
- Davis CA, Levitan RD, Reid C, Carter JC, Kaplan AS, Patte KA, et al. (2009). Dopamine for “wanting” and opioids for “liking”: a comparison of obese adults with and without binge eating. Obesity, 17(6), 1220–1225. [DOI] [PubMed] [Google Scholar]
- Davis C, Loxton NJ, Levitan RD, Kaplan AS, Carter JC, & Kennedy JL (2013). ‘Food addiction’ and its association with a dopaminergic multilocus genetic profile. Physiology & Behavior, 118, 63–69. [DOI] [PubMed] [Google Scholar]
- Devlin MJ, Goldfein JA, Petkova E, Jiang H, Raizman PS, Wolk S, et al. (2005). Cognitive behavioral therapy and fluoxetine as adjuncts to group behavioral therapy for binge eating disorder. Obesity Research, 13(6), 1077–1088. [DOI] [PubMed] [Google Scholar]
- Dixon JB (2010). The effect of obesity on health outcomes. Molecular and Cellular Endocrinology, 316(2), 104–108. [DOI] [PubMed] [Google Scholar]
- Doolan KJ, Breslin G, Hanna D, & Gallagher AM (2015). Attentional bias to food-related visual cues: is there a role in obesity? Proceedings of the Nutrition Society, 74(01), 37–45. [DOI] [PubMed] [Google Scholar]
- Dymek-Valentine M, Rienecke-Hoste R, & Alverdy J (2004). Assessment of binge eating disorder in morbidly obese patients evaluated for gastric bypass: SCID versus QEWP-R. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 9(3), 211–216. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: interview or self-report questionnaire? International Journal of Eating Disorders, 16, 363–370. [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R (2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41(5), 509–528. [DOI] [PubMed] [Google Scholar]
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, et al. (2012). Obesity and severe obesity forecasts through 2030. American Journal of Preventive Medicine, 42(6), 563–570. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, & Ogden CL (2012). Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA, 307(5), 491–497. [DOI] [PubMed] [Google Scholar]
- Flegal KM, & Kalantar-Zadeh K (2013). Overweight, mortality and survival. Obesity, 21(9), 1744–1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gormally J, Black S, Daston S, & Rardin D (1982). The assessment of binge eating severity among obese persons. Addictive Behaviors, 7(1), 47–55. [DOI] [PubMed] [Google Scholar]
- Grafton B, Mackintosh B, Vujic T, & McLeod C (2014). When ignorance is bliss: explicit instruction and the efficacy of CBM-A for anxiety. Cognitive Therapy and Research, 38(2), 172–188. [Google Scholar]
- le Grange D, Gorin A, Catley D, & Stone AA (2001). Does momentary assessment detect binge eating in overweight women that is denied at interview? European Eating Disorders Review, 9(5), 309–324. [Google Scholar]
- Greeno CG, Wing RR, & Shiffman S (2000). Binge antecedents in obese women with and without binge eating disorder. Journal of Consulting and Clinical Psychology, 68(1), 95–102. [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, & Barry DT (2004). Reliability of the eating disorder examination in patients with binge eating disorder. International Journal of Eating Disorders, 35(1), 80–85. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT, Gueorguieva R, & White MA (2011). Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: a randomized controlled trial. Journal of Consulting and Clinical Psychology, 79(5), 675–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, et al. (2010). Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biological Psychiatry, 68, 982–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrar V, Toepel U, Murray MM, & Spence C (2011). Food’s visually perceived fat content affects discrimination speed in an orthogonal spatial task. Experimental Brain Research, 214(3), 351–356. [DOI] [PubMed] [Google Scholar]
- Heeren A, Mogoase C, McNally RJ, Schmitz A, & Philippot P (2015). Does attention bias modification improve attentional control? A double-blind randomized experiment with individuals with social anxiety disorder. Journal of Anxiety Disorders, 29, 35–42. [DOI] [PubMed] [Google Scholar]
- Heeren A, Mogoas¸ e C, Philippot P, & McNally RJ (2015). Attention bias modification for social anxiety: a systematic review and meta-analysis. Clinical Psychology Review, 40, 76–90. [DOI] [PubMed] [Google Scholar]
- Iacovino JM, Gredysa DM, Altman M, & Wilfley DE (2012). Psychological treatments for binge eating disorder. Current Psychiatry Reports, 14(4), 432–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D (2003). A perspective on judgment and choice: mapping bounded rationality. American Psychologist, 58(9), 697–720. [DOI] [PubMed] [Google Scholar]
- Kakoschke N, Kemps E, & Tiggemann M (2014). Attentional bias modification encourages healthy eating. Eating Behaviors, 15(1), 120–124. [DOI] [PubMed] [Google Scholar]
- Kemps E, Tiggemann M, & Elford J (2015). Sustained effects of attentional retraining on chocolate consumption. Journal of Behavior Therapy and Experimental Psychiatry, 49 Part A:94–100. [DOI] [PubMed] [Google Scholar]
- Kemps E, Tiggemann M, Orr J, & Grear J (2014). Attentional retraining can reduce chocolate consumption. Journal of Experimental Psychology-Applied, 20(1), 94–102. [DOI] [PubMed] [Google Scholar]
- Klumpp H, & Amir N (2009). Examination of vigilance and disengagement of threat in social anxiety with a probe detection task. Anxiety, Stress & Coping, 22(3), 283–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuckertz JM, & Amir N (2015). Attention bias modification for anxiety and phobias: current status and future directions. Current Psychiatry Reports, 17(2), 1–8. [DOI] [PubMed] [Google Scholar]
- Linetzky M, Pergamin-Hight L, Pine DS, & Bar-Haim Y (2015). Quantitative evaluation of the clinical efficacy of attention bias modification treatment for anxiety disorders. Depression and Anxiety, 32(6), 383–391. [DOI] [PubMed] [Google Scholar]
- Lopes FM, Pires AV, & Bizarro L (2014). Attentional bias modification in smokers trying to quit: a longitudinal study about the effects of number of sessions. Journal of Substance Abuse Treatment, 47(1), 50–57. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Butryn ML, Didie ER, Annunziata RA, Thomas JG, Crerand CE, et al. (2009). The power of food scale. a new measure of the psychological influence of the food environment. Appetite, 53(1), 114–118. [DOI] [PubMed] [Google Scholar]
- MacLeod C, & Clarke PJF (2015). The attentional bias modification approach to anxiety intervention. Clinical Psychological Science, 3(1), 58–78. [Google Scholar]
- Marcus MD, Wing RR, & Lamparski DM (1985). Binge eating and dietary restraint in obese patients. Addictive Behaviors, 10(2), 163–168. [DOI] [PubMed] [Google Scholar]
- McGeary JE, Meadows SP, Amir N, & Gibb BE (2014). Computer-delivered, home-based, attentional retraining reduces drinking behavior in heavy drinkers. Psychology of Addictive Behaviors, 28(2), 559–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogoaşe C, David D, & Koster EH (2014). Clinical efficacy of attentional bias modification procedures: an updated meta-analysis. Journal of Clinical Psychology, 70(12), 1133–1157. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C, & Beumont PJ (2004). Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy, 42(5), 551–567. [DOI] [PubMed] [Google Scholar]
- Nijs IM, & Franken IH (2012). Attentional processing of food cues in overweight and obese individuals. Current Obesity Reports, 1(2), 106–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijs IM, Franken IH, & Muris P (2007). The modified trait and state food-cravings questionnaires: development and validation of a general index of food craving. Appetite, 49(1), 38–46. [DOI] [PubMed] [Google Scholar]
- Reas DL, & Grilo CA (2008). Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity, 16(9), 2024–2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reas DL, Grilo CM, & Masheb RM (2006). Reliability of the eating disorder examination-questionnaire in patients with binge eating disorder. Behaviour Research and Therapy, 44(1), 43–51. [DOI] [PubMed] [Google Scholar]
- Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, & Wilfley DE (2010). An eating disorder-specific model of interpersonal psychotherapy (IPTED): causal pathways and treatment implications. Clinical Psychology Review, 30(4), 400–410. [DOI] [PubMed] [Google Scholar]
- Rieger E, Wilfley DE, Stein RI, Marino V, & Crow SJ (2005). A comparison of quality of life in obese individuals with and without binge eating disorder. International Journal of Eating Disorders, 37(3), 234–240. [DOI] [PubMed] [Google Scholar]
- Robinson TE, & Berridge KC (1993). The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Research Reviews, 18(3), 247–291. [DOI] [PubMed] [Google Scholar]
- Schag K, Teufel M, Junne F, Preissl H, Hautzinger M, Zipfel S, et al. (2013). Impulsivity in binge eating disorder: food cues elicit increased reward responses and disinhibition. PLoS One, 8(10), e76542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz F, Naumann E, Trentowska M, & Svaldi J (2014). Attentional bias for food cues in binge eating disorder. Appetite, 80, 70–80. [DOI] [PubMed] [Google Scholar]
- Schoenmakers TM, de Bruin M, Lux IF, Goertz AG, Van Kerkhof DH, & Wiers RW (2010). Clinical effectiveness of attentional bias modification training in abstinent alcoholic patients. Drug and Alcohol Dependence, 109(1–3), 30–36. [DOI] [PubMed] [Google Scholar]
- Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. (2007). Dissociable intrinsic connectivity networks for salience processing and executive control. The Journal of Neuroscience, 27(9), 2349–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Devlin MJ, Walsh BT, Spitzer RL, Devlin MJ, Walsh BT, et al. (1992). Binge eating disorder: a multisite field trial of the diagnostic criteria. International Journal of Eating Disorders, 11(3), 191–203. [Google Scholar]
- Strack F, & Deutsch R (2004). Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review, 8(3), 220–247. [DOI] [PubMed] [Google Scholar]
- Stroop JR (1935). Studies of interference in serial verbal reactions. Journal of Experimental Psychology, 18(6), 643–662. [Google Scholar]
- Svaldi J, Naumann E, Trentowska M, & Schmitz F (2014). General and food-specific inhibitory deficits in binge eating disorder. International Journal of Eating Disorders, 47(5), 534–542. [DOI] [PubMed] [Google Scholar]
- Svaldi J, Tuschen-Caffier B, Peyk P, & Blechert J (2010). Information processing of food pictures in binge eating disorder. Appetite, 55(3), 685–694. [DOI] [PubMed] [Google Scholar]
- Thomas JG, Doshi S, Crosby RD, & Lowe MR (2011). Ecological momentary assessment of obesogenic eating behavior: combining person-specific and environmental predictors. Obesity, 19(8), 1574–1579. [DOI] [PubMed] [Google Scholar]
- Timmerman G (1999). Binge eating scale: further assessment of validity and reliability. Journal of Applied Biobehavioral Research, 4(1), 1–12. [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Tomasi D, & Baler R (2012). Food and drug reward: overlapping circuits in human obesity and addiction. Current Topics in Behavioral Neurosciences, 11, 1–24. [DOI] [PubMed] [Google Scholar]
- Werthmann J, Field M, Roefs A, Nederkoorn C, & Jansen A (2014). Attention bias for chocolate increases chocolate consumption - an attention bias modification study. Journal of Behavior Therapy and Experimental Psychiatry, 45(1), 136–143. [DOI] [PubMed] [Google Scholar]
- Werthmann J, Roefs A, Nederkoorn C, Mogg K, Bradley BP, & Jansen A (2011). Can(not) take my eyes off it: attention bias for food in overweight participants. Health Psychology, 30(5), 561–569. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, et al. (2002). A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of General Psychiatry, 59(8), 713–721. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Wilfley DE, Agras WS, & Bryson SW (2010). Psychological treatments of binge eating disorder. Archives of General Psychiatry, 67(1), 94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, & Engel SG (2009). The validity and clinical utility of binge eating disorder. International Journal of Eating Disorders, 42(8), 687–705. [DOI] [PubMed] [Google Scholar]


