Abstract
Cancer is a major public health problem, and is now the world’s leading cause of death. Traditional Chinese medicine (TCM)-combination therapy is a new treatment approach and a vital therapeutic strategy for cancer, as it exhibits promising antitumor potential. Nano-targeted drug-delivery systems have remarkable advantages and allow the development of TCM-combination therapies by systematically controlling drug release and delivering drugs to solid tumors. In this review, the anticancer activity of TCM compounds is introduced. The combined use of TCM for antitumor treatment is analyzed and summarized. These combination therapies, using a single nanocarrier system, namely codelivery, are analyzed, issues that require attention are determined, and future perspectives are identified. We carried out a systematic review of >280 studies published in PubMed since 1985 (no patents involved), in order to provide a few basic considerations in terms of the design principles and management of targeted nanotechnology-based TCM-combination therapies.
Keywords: cancer, codelivery, combination therapy, nanotargeted drug-delivery system, tumor targeting, TCM
Introduction
Cancer is the leading cause of disease-associated death in China,1 and is now the world’s leading cause of death.2 According to the Global Cancer Report 2018 on the trend of 36 cancers in 185 countries worldwide by the WHO, the global burden of cancer is increasing at an alarming rate (one in eight deaths on average are due to cancer). The report also pointed out that the incidence and mortality rate of cancer continues to rise each year, with developing countries accounting for approximately 60% of the world’s new cases and 70% of annual deaths. In 2018, nearly half the world’s new cases of cancer occurred in Asia, most of which occurred in China.3 Bray et al2 provided a status report on the global burden of cancers using GLOBOCAN 2018. It is estimated that there will be 18 million new cases of cancer and 9.6 million cancer deaths in 2018. Lung cancer and breast cancer are the most frequent cancers in men and women, respectively, and the two leading causes of cancer death. Due to the high incidence and mortality rate of cancer, the global health care burden is also increasing rapidly.
Surgical treatment, chemotherapy, and radiotherapy are the primary treatment methods for cancer.4 If cancer patients are diagnosed early and receive timely surgical treatment, the probability of surviving for 5 years after surgery is greatly improved. However, when cancers are diagnosed late, the vast majority of patients are already in the terminal stages, and thus may have lost the opportunity of surgical treatment. In addition, due to adverse reactions caused by radiotherapy, such as fatigue, gastrointestinal reactions, skin damage, bone-marrow suppression, and cardiotoxicity,5 chemotherapy is still the main method of cancer treatment.
Nevertheless, due to lack of specificity and poor targeting, chemotherapy drugs not only kill tumor cells but also act on normal tissue, causing a reduction in immunity, significant side effects, and low drug efficacy. In addition, cancer patients can develop resistance to a single chemotherapy drug in clinical practice, resulting in a decrease in the subsequent curative effect. Multidrug resistance (MDR) was once considered the leading cause of chemotherapy failure, and may also promote tumor metastasis and recurrence.6 Based on recent statistics from the American Cancer Society, >90% of cancer patients die from different levels of MDR.
Therefore, the treatment of cancer should be changed from an initial single medication to combination therapy. The combination of two or more active antitumor ingredients plays a crucial role in complementarity and synergy, and has become the preferred scheme in cancer treatment. Notably, the combination of traditional Chinese medicines (TCMs) with chemotherapeutic drugs and the combination of various TCMs, which involves multiple targets and multiple signaling pathways, have improved efficacy compared with drugs with a single molecular target and become a new strategy for tumor therapy in recent years.7 Due to a great deal of investment and rapid development, nanotechnology is already used in various fields of biomedical science.8 Novel nanoformulation-based drug-delivery systems, such as liposomes, nanoparticles (NPs), vesicles, mesoporous silica NPs (MSNs), and micelles, provide promise in overcoming current limitations, including poor targeting, insufficient absorption, poor pharmacokinetics and bioavailability, and limited biodistribution.9–11
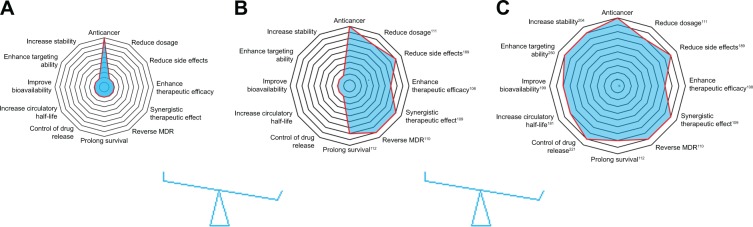
In this review, the anticancer activity of TCM compounds is introduced. The combined use of TCMs for antitumor therapy is analyzed and summarized. These combination therapies using a single nanocarrier system, namely code-livery, are analyzed to determine their potential in prolonging drug duration in vivo, targeting drug delivery, and reducing toxicity (Figure 1). Matters requiring attention and future perspectives in this field are also reviewed, in order to accelerate the clinical application of combination antitumor therapy using targeted nanotechnology.
Figure 1.
Advantages of targeted nanotechnology-based TCM-combination therapy.
Notes: (A) Antitumor effects of TCM; (B) antitumor effects of TCM-combination therapy; (C) antitumor effects of targeted nanotechnology-based TCM-combination therapy.
Abbreviations: TCM, traditional Chinese medicine; MDR, multidrug resistance.
Antitumor effects of TCMs
Herbs, animals, and minerals are used widely as health foods and medicines to remedy various diseases in Asia, and have been collected and recorded as effective and traditional therapies in the TCM literature. For example, artemisinin was isolated by Youyou Tu at the China Academy of Traditional Chinese Medicine in Beijing, and is now an effective medicine in the treatment of malaria. As a result, Tu won the Nobel Prize in Physiology or Medicine in 2015. In most developing countries, 80% of the population continue to use traditional medicines for primary health care.12 From 2016 to 2017, the total amount of TCM herbal medicines and other related products exported to the Belt and Road Initiative countries reached US$295 million. In addition, the WHO also recognized traditional medicine in its influential global medical compendium.13
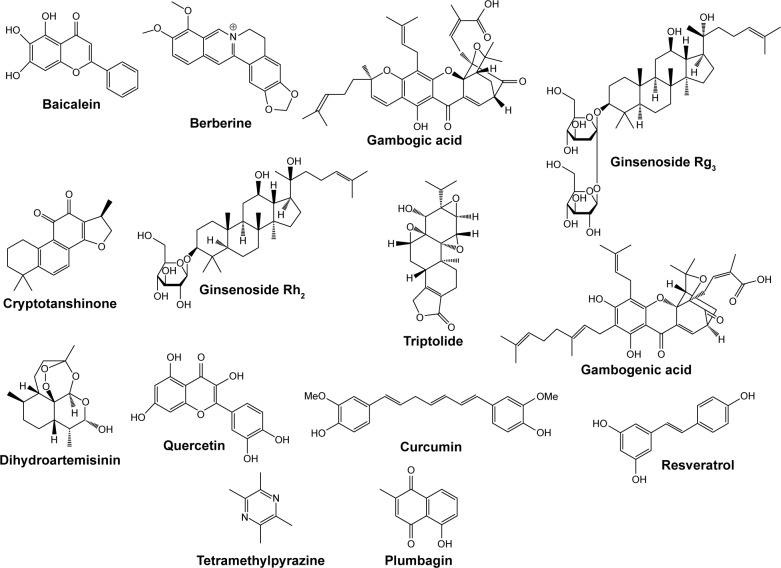
Worldwide, including in Western countries, TCM has been increasingly used in the past few decades, and is well known for its vital role in cancer prevention and treatment. A number of studies have confirmed that the active ingredients in TCM (curcumin [Cur], gambogic acid, and baicalein [BA], among others) are able to effectively induce apoptosis, interfere with tumor progression, inhibit tumor development, inhibit angiogenesis, cause cell-cycle arrest, and block metastasis. A summary of the antitumor effects of drugs isolated from TCMs is shown in Table 1. Structures of TCM compounds are shown in Figure 2.
Table 1.
Antitumor effects of traditional Chinese medicine
| Monomer composition | Source (Chinese name) | Anticancer category | Anticancer property |
|---|---|---|---|
| Curcumin (C21H20O6) | Curcuma longa (jiang huang) | Breast cancer, neurological cancers, lymphoma, lung cancer, melanoma, sarcoma, leukemia, gastrointestinal cancers, ovarian cancer, genitourinary cancers14 | It can inhibit the initiation step of cancer and malignant- cell proliferation during the promotion and progression of carcinogenesis.15 |
| Arsenic trioxide (As2O3) | Arsenic (pi shuang) | Acute promyelocytic leukemia,16 renal cancer, prostate cancer, hepatocellular carcinoma,17–19 lung cancer20,21 | As2O3 can induce the accumulation of cellular ROS, causing DNA damage and leading to cell-cycle arrest and apoptosis in various solid tumors.17–19 |
| Resveratrol (C14H12O3) | Polygonum cuspidatum (hu zhang) | Osteosarcoma cells,22 23 breast cancer, colon cancer,24 cervical cancer, blood cancer, kidney cancer, liver cancer, bladder cancer, thyroid cancer, esophageal cancer, prostate cancer, brain cancer, gastric cancer, bone cancer, ovarian cancer25 | It can induce apoptosis and inhibit proliferation by modulating the PI3K–Akt–mTOR and MAPK pathways.22,26,27 |
| Ginsenoside Rg3 (C42H72O13) | Panax ginseng (ren shen) | Breast cancer cells,28 colorectal tumor,29 ovarian cancer30 | Ginsenoside Rg3 can inhibit tumor development by inhibiting tumor angiogenesis, regulating apoptosis of tumor cells, controlling the proliferation, invasion, and metastasis of tumor cells, and inhibiting multidrug resistance.28–30 |
| Baicalein (C15H10O5) | Scutellaria baicalensis (huang qin) | HCT116 human colon cancer,31 pancreatic cancer stem cells,32 bladder cancer,33 breast cancer,34 gastric cancer,35 hepatocellular carcinoma36 | It can inhibit a variety of cyclins or cyclin-dependent kinases, regulate the cell cycle,37 scavenge oxidative radicals, weaken MAPK, Akt, or mTOR activities,38 inducing apoptosis39 and inhibiting the invasion and metastasis of tumors.40 |
| Gambogic acid (C38H44O8) | Garcinia hanburyi (teng huang) | Gastric cancer,41 prostate cancer,42 lung cancer,43 pancreatic cancer,44 hepatocarcinoma45 | Gambogic acid can induce apoptosis,46 enhance the accumulation of ROS,47 and inhibit telomerase activity.41,43 |
| Gambogenic acid (C38H46O9) | Garcinia hanburyi (teng huang) | Human nasopharyngeal carcinoma CNE1 cells,48 U251 glioblastoma cells,49 breast cancer,50 lung cancer51 | Gambogenic acid is associated with inhibition of proliferation of A549 cells by apoptosis induction and cell-cycle arrest,48,52,53 and can mediate apoptosis in human nasopharyngeal carcinoma CNE1 cells.49 |
| Quercetin (C15H10O7) | Hypericum ascyron (hong han lian) | Melanoma,54 HL60 cells57 prostate cancer,55 breast cancer,56 human leukemia | Quercetin can induce cancer-cell apoptosis by modulating signaling pathways and blocking cell-cycle progression,58 as well as actively suppress cancer proliferation and cancer metastasis.59 |
| Triptolide (C20H24O6) | Tripterygium wilfordii (lei gong teng) | Medulloblastoma,60 lung cancer cells,61 blood cancer cells, colon cancer cells, breast cancer cells, brain cancer cells, ovary cancer cells, kidney cancer cells, prostate cancer cells62,63 | Triptolide can inhibit cell proliferation and arrest the cell cycle,64 increase LC3α expression levels,65 and inhibit the PI3K–Akt–mTOR pathway. While ERK1/2 is activated, autophagy of cell death is induced.66,67 |
| Berberine (C20H18NO4) | Coptis chinensis (huang lian) | Human malignant pleural mesothelioma NCIH2452 cells,68 human colon cancer cells,69 hepatocellular carcinoma,70 breast cancer cells,71,72 human HSC3 oral cancer cells,73 human epidermoid carcinoma A431 cells74 | It can inhibit cancer-cell proliferation, induce cell-cycle arrest at the G1/G0 phase, induce apoptosis in cancer cells,69 cause cell-growth inhibition, and suppress cell migration and invasion.71–74 |
| Cryptotanshinone (C19H20O3) | Salvia miltiorrhiza (dan shen) | Prostate cancer,75 breast carcinoma,76 lung cancer77 | It inactivates STAT3 activity,75 arrests the cell cycle in the G1/G0 phase, and inhibits expression of cyclin D1.76 |
| Tetramethylpyrazine (C8H12N2) | Ligusticum striatum (chuan xiong) | Lung cancer,78 osteosarcoma79 | It can reduce activities of COX2 and MMP2/TIMP2,78 upregulate cytosolic NFκB p65 expression, and downregulate protein expression of nuclear NFκB p65, BCL2, and cyclin D1.79 |
| Dihydroartemisinin (C15H24O5) | Artemisia annua (huang hua hao) | Pancreatic cancer,80 osteosarcoma,81 liver cancer,82 leukemia83,84 | It can activate caspase 3, caspase 8, and caspase 9, upregulate the expression of Fas, cyclin D1, and Bax, downregulate the expression of CDC25B, Bcl2, and cyclin B1, and inhibit NFκB activity.85 |
| Ginsenoside Rh2 (C36H62O8) | Panax ginseng (ren shen) | Breast cancer,86 ovarian cancer,87 prostate cancer,88 leukemia,89 colorectal cancer,90 hepatocellular carcinoma91 | Some signaling pathways, such as TNFα,92 EGFR,93 JAK–STAT3,94 and PI3K–Akt95 have been implicated in the regulatory process of Rh2 in cancer cells. |
| Plumbagin (C11H8O3) | Plumbago zeylanica (bai hua dan) | Prostate cancer,96 breast cancer cells,97 melanoma cells98 | It can induce apoptosis and autophagy, destroy the cell cycle, inhibit invasion and metastasis, and prevent angiogenesis, with anticancer potential in different cancer cells in vitro and in vivo.99 |
Figure 2.
Chemical structures of the active components in traditional Chinese medicine.
Antitumor effects of TCM-combination therapy
Initially, cancer therapy consisted of a single drug, which could involve a single target. However, malignant disease is caused by many complicated factors, and treatment with a single drug is not adequate. Patients are usually susceptible to drug resistance after sequential cycles of therapy with these chemotherapy drugs,100 and a single medication frequently causes serious side effects. For instance, although cisplatin is clinically effective, it lacks selectivity for tumor tissue, resulting in serious side effects, such as kidney-function damage,101 neurotoxicity,102 ototoxicity,103 and the emergence of MDR, resulting in the failure of chemotherapy.104 In addition, long-term or high-dose cisplatin treatment can also cause severe anemia.105 Therefore, the clinical application of single drugs, such as cisplatin, has been greatly restricted.
Cancer therapy urgently requires a new therapeutic approach to overcome these shortcomings. Combination-drug therapy is a new mode of treatment, and has gradually gained the attention of researchers.106 Combination therapy involves the simultaneous or sequential use of two or more medicines for therapeutic purposes, and gradually plays a meaningful role in a complementary way, has synergistic action, and alleviates adverse reactions. It can not only produce a better therapeutic effect by regulating multiple signaling pathways in abnormal cells and act on multiple targets simultaneously but also reduce the occurrence of MDR and reduce both the dosage and side effects. The combination of two or more active antitumor ingredients is now a vital treatment method for tumors, and has received US Food and Drug Administration (FDA) approval.107
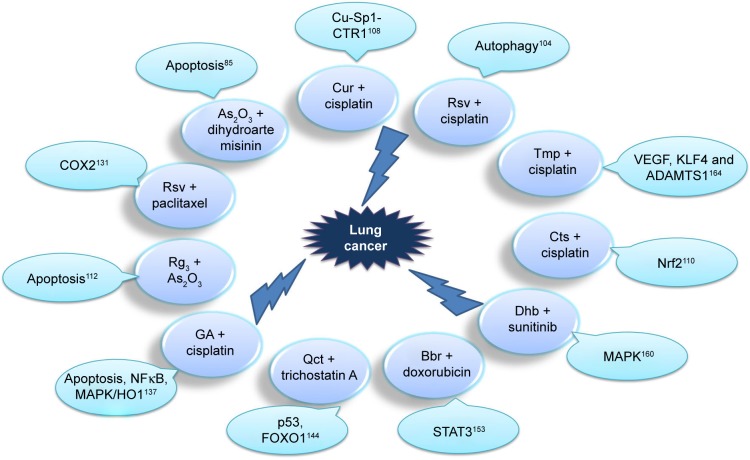
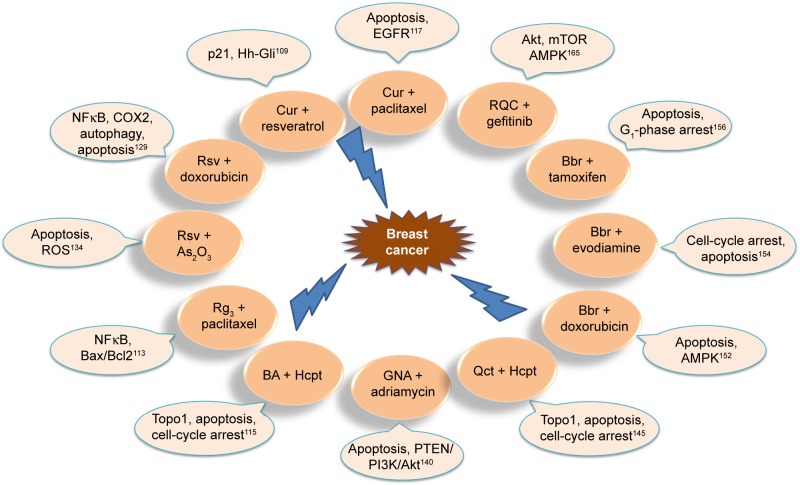
Based on classic TCM theory, the combination of antitumor TCMs exhibits promising potential in cancer treatment such as: 1) enhancing the therapeutic efficacy of chemotherapeutic drugs – due to the combined effects of Cur and cisplatin determined in vitro and in vivo, experimental results demonstrate that Cur can enhance the antitumor effect of cisplatin in A549 cells in vitro, the combination markedly inhibiting tumor growth and promoting apoptosis in the A549-xenograft mouse model;108 2) achieving synergistic therapeutic effects – resveratrol and Cur synergistically cause apoptosis in breast cancer cells by p2 (Waf/Cip1)-mediated inhibition of the Hedgehog–Gli cascade;109 3) reversing drug resistance – the combination of cryptotanshinone and cisplatin leads to cell death and apoptosis, and cryptotanshinone reverses cisplatin resistance in human lung carcinoma A549 cells by downregulating the Nrf2 pathway;110 4) reducing the dose of drugs – combination therapy with triptolide and cisplatin completely suppresses tumor growth, suggesting that lower concentrations of cisplatin and triptolide may produce a synergistic anticancer effect;111 and 5) prolonging survival – As2O3 combined with ginsenoside Rg3 can significantly inhibit the proliferation of NCIH1299 cells and prolong survival of tumor-bearing nude mice, with a significant effect on lung cancer treatment.112 In addition, TCM-combination therapy results in good prognosis, has fewer adverse reactions, has long-lasting curative effects, regulates the expression of intracellular marker proteins, and reduces the side effects of drugs.112–115 Further superior effects are shown in Table 2. The anti–lung cancer and anti–breast cancer mechanisms of TCM-combination therapy are shown in Figures 3 and 4. TCM-combination therapy achieves the effects that single chemotherapeutic drugs fail to achieve, and has become the main direction in clinical and experimental research on antitumor therapy.116
Table 2.
Antitumor effects of TCM-combination therapy
| Monomer composition | Combination therapy | Cellular, animal levels | Advantages of combination therapies | Reference |
|---|---|---|---|---|
| Curcumin (Cur) | Cur + cisplatin | Human non-small-cell lung cancer (NSCLC) A549, A549-xenograft mouse model | Cur can strengthen the antitumor effect of cisplatin in A549 cells in vitro. Cur combined with cisplatin can inhibit tumor growth and promote apoptosis in xenograft mouse model. | 108 |
| Cur + paclitaxel | Breast cancer cell line MCF7, MCF7-xenograft mouse model | Cur combined with paclitaxel can inhibit the growth of MCF7 cells synergistically, induce significant apoptosis in MCF7 cell lines, and exert increased antitumor efficacy in mouse models. | 117 | |
| Cur + Rsv | Breast epithelial MCF10A-Tr, tumor xenograft in mice | Cur and Rsv causes apoptosis synergistically in breast cancer cells by p2 Waf/Cip1-mediated inhibition of Hedgehog–Gli cascade. | 109 | |
| Colon cancer HCT116 (wild type) cells, xenografts in SCID mice | The combination of Cur and Rsv has stronger inhibitory effects on the growth of p53-positive (wild type) and p53-negative (HCT116) colon cancer cells in vitro and in vivo than either agent alone. | 119 | ||
| Cur + Rsv–diallyl disulfide | Malignant rhabdoid (SJRH4, RD/18) and osteosarcoma (SAOS2) cell lines | Cur induces apoptosis in rhabdomyosarcoma and osteosarcoma cells, which is potentiated when Cur is combined with Rsv or diallyl disulfide. | 120 | |
| Cur + As2O3/lonidamine | U937 and HL60 human acute myeloid leukemia cells, K562 chronic myelogenous leukemia cells | Cur plus As2O3 or lonidamine stimulates events typical of the mitochondrial executioner pathway. Cotreatment with Cur may be an effective way to improve the efficacy of As2O3 and lonidamine as antineoplastic agents for myeloid leukemia cells. | 121 | |
| Cur + vesicular stomatitis virus | PC3 prostate cancer cells, mouse model of prostate cancer | Cur makes prostate cancer cells sensitive to the oncolytic effects of vesicular stomatitis virus through modulating antiviral responses and components of the intrinsic apoptotic pathway. | 122 | |
| Cur + Qct | Human gastric cancer MGC803 cells | The combination of Cur and Qct has a significant inhibitory effect on cell proliferation and a stronger effect on gastric cancer MGC803 cells than individual therapy. | 123 | |
| Arsenic trioxide (ATO) | ATO + artesunate | Human K562 cell lines | Artesunate combined with ATO can significantly promote apoptosis of K562 cells induced by artesunate. | 124 |
| ATO + dihydroartemisinin | A549 cells | Dihydroartemisinin effectively sensitizes A549 cells to ATO, increasing the effectiveness of ATO-induced cell death, and can cooperate with ATO to exert synergistic effects in promoting apoptosis in A549 lung cancer cells. | 85 | |
| ATO + cisplatin– doxorubicin (Dox) | HepG2 cell lines, hepatic cancer stem cells | This study was critical in realizing the potential for synergy between ATO and chemotherapeutic protocols, such as cisplatin and Dox. | 125 | |
| Human hepatoma BEL7402 cells, mouse hepatoma HepA | Low-dose cisplatin or Dox and ATO in combination can increase the antihepatocarcinoma effect. | 126 | ||
| ATO + Dox | SGC7901/S human GC cell line, Dox-resistant SGC7901/ADM cell line | ATO can reverse MDR to Dox in human GC cells. This may be relevant to decreased Pgp expression. | 127 | |
| ATO + matrine | Myeloma cell lines RPMI 8226 and U266 | Matrine shows an antimyeloma effect by inducing apoptosis, and ATO combined with matrine enhances apoptosis induced by matrine, having synergistic effects. | 128 | |
| Resveratrol (Rsv) | Rsv + cisplatin | A549 cells | Rsv combined with cisplatin synergistically induced apoptosis by modulating autophagic cell death in A549 cells. | 104 |
| Rsv + Dox | MCF7 and MDA-MB231 cell lines, Ehrlich ascitic carcinoma–bearing mice | Rsv combined with Dox can inhibit tumor volume and prolong the life of Ehrlich ascitic carcinoma cell–bearing mice. | 129 | |
| Rsv + paclitaxel | HepG2 human liver cancer cells | Rsv can enhance the anticancer effect of paclitaxel on HepG2 cells and be used as a sensitizer of paclitaxel. | 130 | |
| NSCLC cell line A549 | Rsv enhances the anticancer effects of paclitaxel in A549 cells, and thus Rsv might be used as an excellent sensitizer for paclitaxel. | 131 | ||
| Rsv + temozolomide | Human glioblastoma U87 MG and GBM8401 cell lines, GBM-SKH (GBM) cell line, orthotopic xenograft model | Rsv can enhance temozolomide-mediated antitumor effects in glioblastoma multiforme in vitro and in vivo by ROS-dependent AMPK–TSC–mTOR signaling pathway. | 132 | |
| Rsv + Qct | Human hepatoblastoma HepG2 cells | Rsv plays different roles in autophagy according to cellular energy state, and can represent a promising strategy to sensitize cancer cells to Qct therapy. | 133 | |
| Rsv + As2O3 | HeLa, MCF7, and NB4 cells, HeLa-cell mouse model | Rsv can significantly raise the antitumor effect induced by As2O3 in vitro, and As2O3 combined with Rsv can significantly inhibit tumor growth and angiogenesis in nude mice. | 134 | |
| Ginsenoside Rg3 | Rg3 + As2O3 | NCIH1299 lung cancer cells, nude mice bearing hepatoma | As2O3 combined with Rg3 can dramatically inhibit proliferation of NCIH1299 cells and prolong the survival of nude mice bearing tumors, having a significant effect on lung cancer therapy. | 112 |
| Rg3 + paclitaxel | Triple-negative breast cancer lines MDA-MB231, sMDA-MB453, BT549, mouse MDA-MB231-xenograft model | Rg3 promotes cytotoxicity and apoptotic effects of paclitaxel on triple-negative breast cancer through inhibition of NFκB activity and regulating Bax/Bcl2 expression. | 113 | |
| Rg3 + paclitaxel/cisplatin | Mouse tumor-xenograft models | The combined use of Rg3 can remarkably raise the inhibitory effects of chemotherapy on tumor growth, and expression levels of Ki67 in the chemotherapy + Rg3 group were significantly lower than in the other groups (Rg3 alone, paclitaxel alone, and cisplatin alone). | 114 | |
| Rg3 + docetaxel | Colon cancer (HCT116 and SW620) cells | Compared to treatment with Rg3 or docetaxel alone, combination therapy can inhibit the growth of cancer cells and induce apoptosis of cancer cells more effectively, accompanied by significant inhibition of NFκB activity. | 135 | |
| Baicalein (BA) | BA + taxol | Human ovarian cancer A2780 cells, SKOV3 cells, and OVCAR cells | BA combined with taxol at low concentrations can play a synergistic antitumor role via the Akt–β-catenin signaling pathway and mitochondria-mediated cell apoptosis in ovarian cancer cells. | 136 |
| BA + 10-hydroxycamptothecin (Hcpt) | BGC823, MCF7, and SMMC7721 cells, mice xenografted with BGC823 tumors | In BGC823, MCF7, and SMMC7721 cells, BA significantly enhances the anticancer activity of Hcpt at an atoxic dose. Hcpt with BA is a novel and effective combination therapy, which synergistically target Topo I and upregulate p53 to induce cell-cycle arrest and cell apoptosis. | 115 | |
| Gambogic acid (GA) | GA + cisplatin | Human NSCLC A549, NCIH460, and NCIH1299 cell lines | GA synergizes the growth-inhibitory activity of CDDP and enhances the apoptosis-induced effect of CDDP on NSCLC cells, meanwhile sensitizing lung cancer cells to CDDP in vitro and in vivo. | 137 |
| GA + gemcitabine | PANC1 and BxPC3 cells, mouse xenograft model of human pancreatic cancer | GA inhibits the activation of ERK–E2F1–RRM2 signaling pathway to sensitize pancreatic cancer cells to gemcitabine in vitro and in vivo. | 138 | |
| GA + sunitinib | Renal carcinoma cell lines 786O and CAKI1, mouse xenograft models | Therapy of 786O and CAKI1 cells with GA or sunitinib can reduce the proliferation of tumor cells, especially when combined with the two medicines. The combination of GA and sunitinib has greater antitumor efficacy than either drug alone. | 139 | |
| Gambogenic acid (GNA) | GNA + adriamycin (Adr) | MCF7 cell lines, MCF7/ADR cell lines | GNA can increase the chemosensitivity of breast cancer cells to Adr. This modulatory role is mediated by suppression of the PTEN–PI3K–Akt pathway, leading to apoptosis in MCF7/ADR cells. | 140 |
| GNA + bortezomib (Btz) | Myeloma MM1S cells, tumor-xenograft models | Btz and GNA have strong synergistic effect in combination therapy, inducing apoptosis of MM.1S cells. The combination of Btz and GNA is superior to single drug on MM.1S-xenograft models. | 141 | |
| Quercetin (Qct) | Qct + tamoxifen | Prostate-tumor xenografts in mice | Tamoxifen combined with Qct can effectively delay the occurrence of tumors, inhibit the final volume of tumors, and reduce the weight of the end-point tumor (P<0.05). | 142 |
| Qct + metformin | PC3 and LNCaP cells, prostate cancer xenografts in nude mice | Combined application of metformin and Qct has a significantly stronger effect on apoptosis of prostate cancer cells than monotherapy, and combination therapy can inhibit the VEGF–Akt–PI3K signaling pathway to play a synergistic antitumor effect. | 143 | |
| Qct + trichostatin A | Mouse xenograft model of A549 cells | Qct enhances the antitumor effect of trichostatin A and prevents trichostatin A-induced muscle wasting. | 144 | |
| Qct + Hcpt | MCF7, BGC823, and HepG2 cells, MCF7 xenograft in nude mice | The combination of Qct and Hcpt can inhibit Topo I in MCF7 cells, which synergistically induces cell-cycle arrest and apoptosis by triggering DNA damage. | 145 | |
| Qct + irinotecan–SN38 | The AGS human gastric adenocarcinoma cell line, AGS xenograft mouse model | Qct combined with irinotecan has a superior regulatory effect on angiogenesis and EMT-related factors. Qct may enhance the efficacy of irinotecan–SN38 in the human AGS cell line. | 146 | |
| Triptolide (TL) | TL + sorafenib | Huh7 and PLC/PRF/5 cells, Huh7 tumor-xenograft mouse model | Sorafenib combined with TL is superior to single-drug therapy in increasing cell death and apoptosis in vitro. | 147 |
| TL + cisplatin | Human gastric adenocarcinoma SCM1 cells, xenografts in SCID mice | TL can raise the cytotoxicity of cisplatin to SCM1 cells, and the combined therapy can significantly inhibit the growth of tumors. | 111 | |
| Urothelial cancer cells, PC3 prostate cancer cell line, mouse xenograft model | Cancer-specific enhancement of cisplatin-induced cytotoxicity with TL by the interaction of inactivated GSK3β with p53. | 148 | ||
| TL + oxaliplatin | Colon cancer cell line SW480, nude mouse model | Combination therapy with TL and oxaliplatin exerts synergistic antitumor effects at low concentrations in colon cancer cells, with less cytotoxicity, which exhibits high potency for clinical applications. | 149 | |
| TL + fluorouracil | Colon carcinoma HT29 cells, tumor xenografts in nude mice | The combined effects of TL and fluorouracil on the growth of colon carcinoma are better than that of single drug, whether in vitro or in vivo. TL combined with fluorouracil has synergistic effects at lower concentrations and promotes apoptosis, but the side effects of chemotherapy are not increased. | 150 | |
| TL + gemcitabine | Pancreatic cancer BxPC3 and PANC1 cell lines | TL can increase gemcitabine-induced cell-growth inhibition and apoptosis synergistically. When TL is combined with gemcitabine, the potential for therapy of pancreatic cancer increases markedly. | 151 | |
| Berberine (Bbr) | Bbr + Dox | Human breast cancer MCF7/MDR cells, tumor xenografts in the BALB/c nu/nu mice | Bbr can increase the sensitivity of drug-resistant breast cancer to Dox chemotherapy and can directly induce apoptosis in vitro and in vivo by dose-orchestrated AMPK signaling. | 152 |
| NSCLC NCIH460, NCIH1975 cells | Bbr inhibits Dox-mediated STAT3 activation and enhances the cytotoxic effect in lung cancer cells of Dox treatment. | 153 | ||
| Bbr + evodiamine | Human breast cancer MCF7 cells, mice with MCF7 human breast cancer xenografts | Bbr combined with evodiamine plays a synergistic role in inhibiting the proliferation of MCF7 cells through inducing cell-cycle arrest and apoptosis. | 154 | |
| Bbr + galangin | ECA9706 cells, nude mice with xenograft tumors | Galangin combined with Bbr synergistically exerts cell-growth inhibition, apoptosis, and cell-cycle arrest in esophageal carcinoma cells and also exhibits outstanding synergistic anticancer role in vivo. | 155 | |
| Bbr + tamoxifen | MCF7 and MCF7/TAM cells | Bbr combined with tamoxifen is more effective than tamoxifen alone in inducing cell-growth inhibition, inducing G1-phase arrest and activating cell apoptosis. | 156 | |
| Bbr + sorafenib | SMMC7721 and HepG2 cells | The combination of Bbr and sorafenib exhibits a synergistic inhibitory effect on the proliferation of SMMC7721 and HepG2 cells. | 157 | |
| Allicin (AN) | AN + IL2 | BXPC3 cell line, pancreatic cancer xenograft in mice | The combination of AN and IL2 can inhibit the growth of tumors and prolong survival, possibly by activation of CD4+ T, CD8+ T, and NK cells. | 158 |
| AN + fluorouracil | SK-Hep1 and BEL7402 cell lines, hepatocellular carcinoma-xenograft models in nude mice | By ROS-mediated mitochondrial pathway, AN can increase the sensitivity of hepatocellular carcinoma cells to fluorouracil-induced-apoptosis. Combination of AN and fluorouracil can be used as a novel chemotherapeutic regimen for hepatocellular carcinoma. | 159 | |
| Dihydroberberine (Dhb) | Dhb + sunitinib | Human NSCLC NCIH460, NCIH460 cell-xenografted nude mice | Sunitinib shows synergistic effects on proliferation, colony formation, and growth of transplantable tumors of NCIH460 cells, suggesting that Dhb can increase the sensitivity of lung cancer to sunitinib. | 160 |
| Oxymatrine (Omt) | Omt + oxaliplatin | Colon cancer lines (HT29 and SW480), SW480 xenograft mouse model | A combined index value <1 for Omt and oxaliplatin has a synergistic effect. Compared with oxaliplatin or Omt alone, combination therapy has more effective inhibition on tumor weight and volume of SW480-xenotransplant mice. | 161 |
| Omt + NM3 | Human gastric cancer cell lines SGC7901, MKN45, MKN74, human gastric cancer xenografted in mice | Omt combined with NM3 can synergistically inhibit the growth of human gastric cancer cell line SGC7901 in vitro and the growth of xenograft human gastric cancer cell line SGC7901 in vivo. | 162 | |
| Tetraarsenic oxide (TAO) | TAO + cisplatin | Human cervical carcinoma cell line HPV16, CaSki cells, mice bearing CaSki-cell tumors | TAO can induce apoptosis. Combined with cisplatin, it can significantly increase the number of apoptotic cells, exerting a synergistic role. | 163 |
| Cryptotanshinone (Cts) | Cts + cisplatin | A549 cells, A549/DDP cells | Compared with cisplatin monotherapy, the combination of Cts and cisplatin induces cell death and apoptosis by increasing the sensitivity of A549/DDP cells to cisplatin. Cts can reverse the resistance of human lung cancer A549 cells to cisplatin by downregulating the Nrf2 pathway. | 110 |
| Tetramethylpyrazine (Tmp) | Tmp + cisplatin (CDDP) | Lewis lung cancer mice | The inhibitory effect of Tmp combined with DDP on tumor growth is enhanced compared to Tmp- or CDDP-alone treatment. Tmp with CDDP had additional or synergistic effects to inhibit tumor growth effectively. | 164 |
| Catechin (RQC) | RQC + gefitinib | Human metastatic breast cancer cell line MDA-MB231, hairless SCID female mice | Combination of RQC and gefitinib can significantly reduce the viability of gefitinib- resistant breast cancer cells. Compared with RQC or gefitinib alone, it can significantly inhibit the growth and metastasis of breast tumors in nude mice. | 165 |
| Dihydroartemisinin (Dha) | Dha + gemcitabine | BxPC3 and PANC1 cell lines, BALB/c nude mice | Dha significantly enhances the inhibition and apoptosis of gemcitabine on BxPC3 and PANC1 cell lines in vitro. Combination therapy can significantly enhance the antitumor effect of gemcitabine. | 80 |
| Epigallocatechin- 3-gallate (EGCG) | EGCG + Dox | Human prostate-cell lines, mouse tumor modeling with PC3ML cells | EGCG can be effectively used to improve the efficacy of Adr through improving its ability to eradicate highly aggressive, metastatic, or primary tumors. | 166 |
| Human HCC cell line BEL7404/Dox, xenograft mouse model | EGCG can enhance Dox-induced cytotoxicity and increase the sensitivity of drug-resistant hepatocellular carcinoma cells to Dox at an atoxic dose. | 167 | ||
| Ginsenoside Rh2 | Rh2 + paclitaxel–mitoxantrone | LNCaP prostate-tumor cells, human LNCaP-tumor xenograft | Rh2 combined with paclitaxel shows stronger inhibition and synergistic effect on growth in a cultured LNCaP cell line. | 88 |
Abbreviations: SCID, severe combined immunodeficiency; MDR, multidrug resistance; CDDP, cis-diamminedichloroplatinum; EMT, epithelial–mesenchymal transition.
Figure 3.
Anti–lung cancer mechanism of TCM-combination therapy.
Abbreviations: Cur, curcumin; Rsv, resveratrol; Tmp, tetramethylpyrazine; Cts, cryptotanshinone; Qct, quercetin; Bbr, berberine; Dhb, dihydroberberine; GA, gambogic acid.
Figure 4.
Anti–breast cancer mechanism of TCM-combination therapy.
Abbreviations: Cur, curcumin; Rsv, resveratrol; Bbr, berberine; Hcpt, hydroxycamptothecin; Qct, quercetin; GNA, gambogenic acid; BA, baicalein.
Nevertheless, there are three possible interactions in drug combinations: antagonistic, additive, and synergistic effects. Therefore, if we do not understand interactions among drugs, blindly combining drugs will not only fail to achieve the desired response but also lead to reduced efficacy and increased toxicity, and even produce drug-borne diseases. For instance, the combination of paclitaxel (Ptx) and BA shows antagonism in breast cancer MCF7 cells,117 and Liu et al118 suggested that the combination of gambogic acid and bortezomib should be avoided in patients. In addition, attention should be paid to the proportion and sequence of the two drugs in combination.
Applications of targeted nanotechnology in TCM-combination therapy
During the early 20th century, Paul Ehrlich proposed the concept of targeted drugs, which consisted of three components: the drug, targeting moiety, and drug carrier. The main aim was to deliver the drug to the specific target organ under the specific guiding mechanism.168 Targeted preparations are characterized by increasing the intensity of pharmacological action in target tissue, controlling drug release, and decreasing systemic adverse reactions. Targeted drug-delivery systems have become one of the important high-profile topics in modern pharmacy. Nanotargeted drug-delivery systems have remarkable advantages in improving the bioavailability of drugs, enhancing the targeting ability of drugs, improving the distribution and pharmacokinetic properties of antitumor drugs in vivo and in vitro, increasing the stability of drugs, solubilizing poorly soluble drugs, protecting drugs from degradation in vivo, intelligently regulating the release of components, enhancing efficacy, and reducing toxicity.169–172 Moreover, metastasis of neoplastic cells is the major cause of death in cancer patients,173,174 and nanosize drug-delivery systems also provide an encouraging strategy for lymphatic metastases.175 In 2004, the National Cancer Institute (NCI) launched the NCI Cancer Nanotechnology Alliance, which aims to use nanotechnology to combat cancer.176
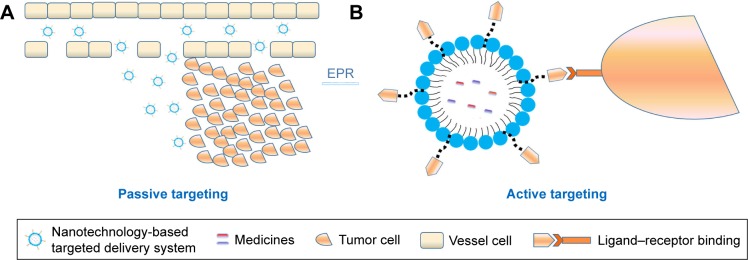
In recent years, many types of nanopreparations of TCMs, which involve the combination of nanotargeted drug-delivery systems and the advantages of TCM components in the treatment of tumors, have been reported.177–179 Simultaneously, nanotargeted drug-delivery systems are also promising multidrug carriers and allow the development of drug combinations by systematically controlling drug release and delivering drug to solid tumors.180 Codelivery of multiple antitumor agents in a single well-designed nanocarrier has significant advantages over monotherapy.181,182 Generally, drug targeting can be classified into three categories: passive targeted preparations, active targeted preparations, and other physicochemical targeted drug-delivery systems.
Passive targeted drug-delivery systems
In a passive targeted drug-delivery system, lipids, adipoids, proteins, and biodegradable high-molecular-weight polymers are mainly used as carriers, and the drug is encapsulated or embedded into various colloidal systems, forming stable structures, such as polymeric NPs (PNPs), micelles, nanovesicles, and liposomes, to increase drug concentration in tumor cells, decrease drug distribution in blood and other organs, and prevent toxicity and adverse reactions. This spontaneous accumulation, or “passive” targeting, is particularly effective against tumors, due to leaky angiogenic vessels and poor lymphatic drainage of the tumor, which is currently referred to as the enhanced permeability and retention (EPR) effect. That is to say, the high permeability of tumor blood vessels allows nanosystems to enter the interstitial spaces of the tumor, while impaired lymphatic filtration allows these nanosystems to remain there. This phenomenon does not exist in normal tissue. Currently, EPR-mediated drug delivery is considered effective in delivering drugs into tumors, especially nanocarriers (Figure 5). The size of the particles is also closely related to their distribution.183 The different sizes of these nanosystems decide the in vivo distribution behavior. Nanopreparations of <100 nm can be slowly accumulated in bone marrow; nanocarriers of 100–200 nm are apt to become enriched in the solid-tumor site; nanosystems of 0.2–3 μm are taken by macrophagocytes in the liver and spleen and particles of >7 μm are often intercepted by pulmonary capillary beds and enter the pulmonary tissues or alveoli.184
Figure 5.
Passive (A) and active (B) targeting of tumors.
Abbreviation: EPR, enhanced permeability and retention.
Liposomes
Liposomes are microvesicles with one or more aqueous cavities formed by the encapsulation of one or two amphiphilic molecular double-layer membranes, and the drug is encapsulated or embedded into the liposomes to form the liposome drug. Due to the similarity between the structure and the biological membrane, the encapsulation of water-soluble and fat-soluble drugs can reduce the drug dose, lower drug toxicity, delay release, lower in vivo elimination speed, change in vivo distribution of the drug, and achieve targeted release. Due to these advantages, liposome drugs have attracted considerable attention, and many studies have been carried out on them.185
Plumbagin is a quinonoid isolated from the roots of Plumbago zeylanica (bai hua dan in Chinese).186 It has high antip-roliferative activity against a variety of tumor cell lines,187,188 and its anticancer properties have also been demonstrated in vivo.186 Celecoxib and plumbagin are two antitumor drugs that synergistically kill melanoma cells instead of normal cells. The combined use of these two agents in traditional approaches was not possible, due to their poor bioavailability and toxicity concerns. In order to circumvent these challenges, Raghavendra et al182 developed a nanoliposome containing celecoxib and plumbagin, named CelePlum 777, which has good stability and can release these two drugs at optimal proportion to achieve the maximum synergistic killing effect. Compared to nanoliposomes containing individual drugs, CelePlum 777 can enhance the inhibition of melanoma-cell proliferation in vitro and reduce the growth of melanoma tumors, with negligible systemic toxicity in nude mice. The goal of loading different individual drugs into a nanoliposome that releases the drugs at synergizing ratios was realized.
Previous studies have shown that Cur can reduce side effects caused by cisplatin (cis-diamminedichloroplatinum [CDDP]), including ototoxicity,189 nephrotoxicity,190 and neurotoxicity.191 In addition, Cur can also overcome resistance to CDDP and improve the sensitivity of hepatocellular carcinoma cells to CDDP.192 However, due to poor water-solubility and the different pharmacokinetics of CDDP and Cur,193 the cocktail of both drugs controlling the drug proportions and dose regimen at target cancer cells would be challenging. Based on a previous approach and advantages of the liposome, Cheng et al194 developed a liposomal delivery system using a reverse-microemulsion and film-dispersion method, which coencapsulated CDDP and Cur and transplanted them into hepatocellular carcinoma cells. The anti-tumor activity of CDDP-Cur liposomes against HepG2 cells was higher than that of free drug or encapsulated-monodrug therapy, and retention was prolonged (t½=2.38 hours). Therefore, coloaded liposomes can be used as an effective treatment for tumors, with great clinical application potential.
Polymeric nanoparticles
NPs are solid colloid particles 10–100 nm in size formed by drug dissolution, encapsulation, or adsorption on macromolecular materials. NPs within the particle-size range of 10–100 nm can hide the physicochemical characteristics of the drug, and the in vivo process of the drugs depends on the physicochemical characteristics of the carriers.195 NPs are characterized by a relatively simple preparation process, a significant solubilization effect on active components, significantly improved drug targeting to tumors, and proneness to surface modification. They can improve drug stability, reduce digestive tract stimulation, achieve sustained release or controlled release,196 effectively overcome multiple physiological barriers encountered in vivo, and achieve accurate, safe, efficient, and targeted therapeutic effects. Coating the surface of NPs with polyethylene glycol (PEG), or “PEGylation”, is a commonly used approach to improve the efficiency of drug delivery to target cells and tissue. PEGylation is capable of achieving prolonged blood circulation of nanocarriers, and can improve colloidal stability by providing steric surface hindrance. In addition, it has the ability to improve particle dispersion and decrease hemolysis.197,198 Polylactic-co-glycolic acid (PLGA), a biodegradable polymer, is atoxic to final degradation products and has been approved by the FDA.181,199 The antitumor effects of codelivered PNPs in TCM combinations are shown in Table 3.
Table 3.
Polymeric nanoparticles (NPs) for codelivery of antitumor agents
| Codelivery ingredients | Delivery-system materials | Method | Advantages | Reference |
|---|---|---|---|---|
| Epigallocatechin gallate (EGCG) + paclitaxel (Ptx) | Polylactic-co-glycolic acid (PLGA)–casein polymer– protein hybrid NPs | Emulsion precipitation | The core–shell nanoconstruct sequentially released EGCG followed by Ptx, which was sustained for 7 and 12 days, respectively. Compared with the bare drugs, dual-loaded NPs significantly increased plasma concentration, residence time, and circulatory half-life of nanoencapsulated Ptx and EGCG. | 181 |
| Camptothecin (CA) + ABT737 | PEGylated polymeric NPs | Nanoencapsulation | Dual-loaded NPs exerted synergistic cytotoxic effects against HCT116 cells, RKO cells, and HT29 cells at a range of NP concentrations. | 200 |
| Gambogic acid (GA) + docetaxel (Dtx) | PLGA NPs | Nanoprecipitation | GA and Dtx were released synchronously in blood from the NPs in vivo. Compared with the saline control group, free Dtx solution and free Dtx-GA solution, the cocarrier NP-preparation group had the strongest inhibitory effect on the MCF7/ADR human breast-tumor xenograft. | 201 |
| Quercetin (Qct) + tamoxifen (Tmx) | PLGA NPs | Emulsion–diffusion solvent evaporation | NPs coencapsulated with Tmx and Qct had higher cellular uptake, cytotoxicity, and tumor suppression in female rats compared to free Tmx citrate, free Qct, and their combination. | 202 |
| Piperlongumine (PL) + Ptx | PLGA and -α-tocopheryl D PEG succinate NPs | Organic solvent evaporation | Compared with free Ptx, the double-loaded NPs had a sustained drug-release rate, showing increased cytotoxicity and cellular uptake in vitro. Ptx/PL-PT NPs suppressed tumor growth more efficiently with less toxicity than Ptx solution. | 203 |
| Qct + etoposide (Etp) | PLGA NPs | Single-emulsification (oil in water) solvent evaporation | With sustained release shown by NP pharmacokinetic parameters, bioavailability increased gradually. Cytotoxicity assays showed that the IC50 values of Etp-loaded NPs and Etp + Qct double-loaded NPs were nine- and elevenfold lower than free Etp. | 199 |
| Piperine + rapamycin | PLGA NPs | Nanoprecipitation | Dual-loaded NPs exhibited sustained release, with potential for long-term therapeutic action with less dosing frequency, and would result in a reduction of dosing and improved bioavailability compared to single-drug administration. | 204 |
| Vincristine (VI) + verapamil (VE) | PLGA NPs | Oil-in-water emulsion- solvent evaporation | The toxicity of coencapsulated NPs was lower than that of the free VI–VE combination. Compared with normal saline, free VI, free VI–VE combination, and single-drug NP combination, the coencapsulated NP group had the best tumor growth–inhibition effect in the MCF7/ADR human breast-tumor xenograft. | 205 |
Abbreviation: PEG, polyethylene glycol.
Lipid–polymer hybrid nanoparticles
As indicated, it has been demonstrated by the increasing numbers of research reports that biodegradable PNPs and liposomes have become the two main types of active TCM nanocarriers. Lipid–polymer hybrid NPs (LPNs) are nuclear-shell NPs formed by polymer core–lipid/lipid–PEG shells206,207 that have the advantages of biodegradable PNPs and bionic liposomes.
Li et al208 prepared LPNs and PNPs loaded with cisplatin and Cur. Results indicated that LPNs had higher anticancer efficacy than PNPs and free drugs. Cytotoxicity was highest in vitro and antitumor effect best in vivo. Therefore, LPNs can be used as a targeted and synergistic nanodrug codelivery system for tumor chemotherapy. In a similar study, Zhu et al209 developed vincristine–quercetin (Qct) dual-loaded LPNs. The experimental results proved that the LPNs loaded with both drugs exhibited better antitumor efficacy in vitro and in vivo.
Ruttala et al210 developed nanocarriers loaded with Ptx and Cur using a method different from the previously mentioned studies. Ptx-loaded albumin NPs were prepared and encapsulated in PEGylated hybrid liposomes containing Cur by a thin-film hydration method. This combination guaranteed the release of Ptx and Cur in a sustained and sequential manner. Compared with a cocktail combination, the dual-drug-loaded nanocarrier had a better cytotoxic effect at a lower dose. Therefore, such coloading drug-delivery systems can be used as a promising treatment method to improve clinical efficacy in various malignant tumors. NPs containing genistein and Ptx have also showed similar experimental results.211
Nanostructured lipid carriers
Nanostructured lipid carriers (NLCs) are novel lipid NPs and mixtures of solid and liquid lipids, which have the advantages of excellent drug-loading capacity and sustained-release properties. Jiang et al212 prepared etoposide (Etp)- and Cur-loaded NLCs by the solvent-injection technique. Etp-Cur NLCs had the highest cytotoxicity in vitro and higher accumulation in tumor tissues in vivo compared with other preparations, including Etp NLCs, Etp + Cur solution, Etp solution, and NLCs. In addition, Etp-Cur NLCs displayed low cytotoxicity in normal tissue in vivo, suggesting that NLCs could serve as a promising therapeutic strategy in the treatment of tumors.
Mesoporous silica nanoparticles
MSNs have attracted much attention due to their potential biomedical applications. MSNs possess many attractive features for application in the delivery of TCMs, such as the size of tuning particles/pores, large surface, large pore volume, high loading capacity, mass producibility, biocompatibility, and chemical inertia.213,214 TCMs can be dissolved in surfactant micelles, simultaneously hydrolyzed, and concentrated with silica to form NPs.
Jia et al215 prepared NPs using the self-assembly in situ drug-loading approach, in order to deliver the anticancer drug Ptx and the MDR-reversal agent tetrandrine (Tet) to increase the intracellular concentration of Ptx, enhance its antitumor effect, and minimize the exposure of normal cells to Ptx and Tet. The study demonstrated that Tet significantly increased the accumulation of NPs in cells. Furthermore, Ptx-Tet–cetyltrimethylammonium bromide MSNs suppressed tumor-cell growth more efficiently than the delivery of Ptx (Ptx–cetyltrimethylammonium bromide MSNs) or free Ptx alone. The prepared NPs released the drugs easily in the acidic environment of tumors, and thus, side effects and toxicity in normal tissue and organs were reduced. This nano-carrier may have important potential in clinical applications to avoid MDR by codelivering multiple TCMs. Solid self-nanoemulsifying drug-delivery systems containing tamoxifen and Qct have also shown similar experimental results.216
PEGylated lipid bilayer–supported mesoporous silica nanoparticles
The anticancer drug axitinib (Axt) is a small-molecule tyrosine kinase–receptor inhibitor of VEGFR1, -2, and -3.217,218 Another anticancer drug, celastrol (Cst), can induce the suppression of angiogenesis219 and enhance the antitumor activity of standard chemotherapeutic drugs.220 Choi et al221 loaded Cst into an MSN carrier and subsequently coated it with a lipid bilayer containing Axt, denoted by “ACML”, to increase the synergistic efficacy of the two agents. The difference in drug loading resulted in a sequential-release pattern where Axt was released first to exert its anticancer effect, and then Cst was released to further induce a synergistic effect. The experimental results showed that the synergistic apoptotic effect of ACML against cancer cells was stronger than the Axt-Cst cocktail. Moreover, ACML had a greater tumor-inhibitory effect than either drug administered alone in a tumor-xenograft mouse model. It has been proved that PEGylated lipid bilayer–supported MSNs have the potential to be used as an effective therapeutic strategy for malignant tumors.
Micellar systems
Self-assembled polymeric micelles have been studied widely, due to their excellent role in cancer treatment. Polymeric micelles have a core–shell structure, where hydrophobic drugs are soluble and remain stable in the hydrophobic core of the micelles, and the hydrophilic shell can prolong internal circulation and improve spatial stability by reducing opsonization during blood circulation. Furthermore, polymeric micelles can selectively and effectively accumulate in tumor tissues due to the EPR effect, thus enhancing the therapeutic effects of the loaded chemotherapeutic drugs. As such, codelivery micellar systems have attracted considerable attention.222,223
Doxorubicin (Dox) has extensive antitumor activity against various solid tumors, including lung cancers, melanoma, neurological cancers, sarcoma, leukemia, lymphoma, gastrointestinal cancers, genitourinary cancers, breast cancers, and ovarian cancers.14 Due to the rapid elimination of drugs in vivo, the cocktail combination of free Dox and Cur often fails to provide enough antitumor efficacy or low systemic toxicity. Furthermore, the combination of Dox and Cur has not been realized clinically. In recent years, a few studies have proposed that codelivering Dox and Cur may result in less toxicity, good drug-release profiles, and improved drug distribution in tumor tissue.224–226 Zhang et al223 prepared dual-loaded micelles with coencapsulated Dox and Cur. The experimental results showed that Dox delivered by this method prolonged systemic circulation and increased its accumulation in the tumor, resulting in a lower level of the toxic metabolite doxorubicinol in heart tissue than free Dox alone or the cocktail combination. In addition, Gu et al225 assembled micelles loaded with Dox and Cur. The micelles prolonged the circulation of Dox or Cur when compared with the individual administration of either, and exhibited strong inhibition of tumor growth and reduced Dox side effects.
Ptx has a broad spectrum of activity against various tumors. It has been used clinically for more than two decades. However, it is poorly soluble and has considerable limitations in clinical applications. In addition, Ptx extravasation of cancer cells caused by Pgp activity is also a main factor limiting its clinical efficacy.227,228 Abouzeid et al229 prepared micelles loaded with Ptx and Cur using the thin-film hydration method. Cur–Ptx-loaded micelles released the entrapped drugs with a slow pattern, and resulted in a threefold inhibition of tumors in vitro. The combination of Cur and Ptx was shown to reverse MDR in a resistant human ovarian adenocarcinoma model. Therefore, these combinations of micelles have significant advantages in vitro and in vivo over individual drug treatment, especially in drug-resistant tumors.
Microemulsions
A microemulsion is a transparent or semitransparent oil– water system with low viscosity, isotropism, and thermodynamic stability, and is spontaneously formed by an oil phase, water phase, emulsifier, and coemulsifier. As an ideal drug carrier, it has the advantages of solubilizing components with different solubility properties, good dispersibility, excellent absorbability, and increased bioavailability.230
BA is one of the most commonly used traditional chemotherapeutic drugs for the treatment of various cancers, including HCT116 human colon cancer,31 pancreatic cancer stem cells,32 and bladder cancer.33 It is known that BA has the ability to inhibit the function of Pgp.231 Meng et al230 developed nanoemulsions (NEs) coencapsulating Ptx and BA using rotary evaporation. The research showed that compared with other Ptx preparations, Ptx-BA NEs had a better antitumor effect on MCF7/Tax cells. Studies on cellular uptake have shown that Ptx-BA NEs accumulate effectively in cancer cells. More importantly, Ptx-BA NEs have a higher antitumor effect than other Ptx formulations used in antitumor in vivo studies. The combined delivery of Ptx and BA by NEs may provide a potential combination-treatment strategy to overcome MDR.
Nanovesicles
Nanovesicles are microvesicles with a quasiliposome duallayer structure formed by the self-assembly of synthesized or naturally modified amphiphilic polymers and cholesterol in hydrophilic media. In contrast to other micromolecular vesicles, the polymer vesicle is characterized by good molecular designability, high intensity of the vesicle, excellent stability, and strong permeability.232,233 As a TCM carrier, it can improve histocompatibility and cell permeability and encapsulate hydrophilic drugs or lipophilic drugs.
Alemi et al234 loaded both Cur and Ptx into cationic PEGylated niosomal formulations using thin-film hydration method to enhance efficacy in MCF7 human breast adenocarcinoma cells. The combination of Ptx and Cur, particularly in the nanoniosome formulations, improved the effectiveness of cancer therapy. The novel cationic PEGylated niosome delivery of combined Ptx and Cur is an effective strategy in the treatment of breast cancer.
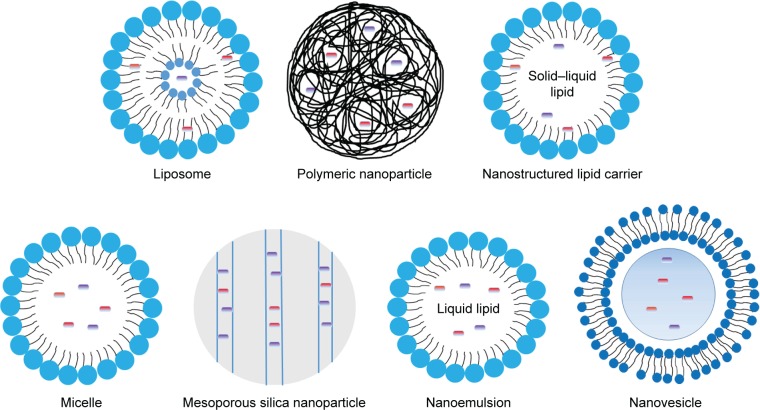
Schematic illustrations of these nanosystems for drugs are shown in Figure 6. In addition, graphene oxide,235 carbon nanotubes,236,237 nanorods,238 nanosponges,239 solid lipid NPs,240 nanometal–organic frameworks,241 metallosupra-molecular nanogels,242 and microspheres243 all provide new opportunities for the antitumor effects of TCM-combination therapy.
Figure 6.
Schematic illustrations of several nanosystems for drugs.
Despite the EPR effect, most nanosystems fail to find their way toward tumor sites.244 Under most circumstances, 90% or more of the administered nanosystems end up in the liver or spleen, increasing adverse systemic reactions and causing low therapeutic efficacy.245,246
Active targeted drug-delivery systems
An active targeting preparation is a drug-delivery system which can utilize the modified drug carrier as a “missile” and deliver the drug selectively to the target area to allow the drug to accumulate and exert its efficacy. The mechanism of active targeting is that after surface modification with the specific targeted antibody or ligand via covalent or noncovalent binding, the nanodelivery system can avoid recognition and phagocytosis by macrophages and change natural in vivo distribution, so as to deliver the drug to the targeted tumor site and exert its active tumor-targeting effects.247 For instance, due to the difference between tumor cells and normal cells in terms of receptor expression or other biological characteristics, the tumor-targeted drug-delivery system has been developed to ensure that the drug acts only on tumor cells248 and induces the off-target effect in normal tissue, which has become a high-profile topic in studies on drug-delivery systems.
Transferrin (Tf)-modified nanocarriers
The Tf receptor is commonly present in normal cells and tumor cells. However, expression of the Tf receptor is approximately four to five times that on the surface of tumor cells than on normal cells.249 Transferrin can bind with the Tf receptor and be internalized into the cells under mediation by the receptors to reach the targeted site.
Cui et al250 designed Tf-decorated NPs (Tf-PEG Cur–Dox NPs) to codeliver Cur and Dox for breast cancer therapy. Results showed that the combination of Tf-PEG-Cur and Dox NPs exerted higher cytotoxicity in MCF7 cells compared with Tf-PEG-Cur NPs alone. Higher accumulation of Tf-PEG Cur–Dox NPs was observed in tumors compared to the Cur-Dox injection. Therefore, Tf-PEG Cur–Dox NPs displayed higher efficiency in vitro and in vivo, and resulted in efficient tumor-targeted drug delivery, reduced cytotoxicity, and a stronger antitumor effect.
Folic acid–modified nanocarriers
Similarly to distribution of the Tf receptor on surfaces of tumor-cell membrane, folic acid receptors on tumor cells are overexpressed compared with normal cells, and their activity is also significantly higher than that on normal cells. In addition, folic acid is characterized by low immunogenicity, high modifiability, and high storability. Utilization of the difference in folic acid–receptor expression between tumor sites and normal tissue can achieve targeted delivery of a folic acid–modified drug to cancer cells.251,252
Prodrugs of Ptx and baicalein containing dual-targeted ligands of folate and hyaluronic acid have been synthesized. NPs loaded with these prodrugs (Ptx–baicalein) have also been prepared and the synergistic antitumor effect evaluated in vitro and in vivo. The results showed that the Ptx–baicalein NP drug-delivery system delivered Ptx–baicalein prodrugs to drug-resistant human lung cancer cells, and the delivery was proven to be effective. In addition, Ptx–baicalein NPs exerted an enhanced synergistic anticancer effect, which also overcame MDR to Ptx.253
Low-density lipoprotein–modified nanocarriers
The low-density lipoprotein (LDL) receptor is widely present on the surface of various cells and tissue types, but is overexpressed in tumor cells. LDL is an endogenous NP with good biocompatibility, good biodegradability, and low immunogenicity, and can avoid being recognized and cleared by the in vivo endogenous reticuloendothelial system.254,255 Therefore, LDL is an ideal potential ligand for tumor targeting.
A novel nanocarrier containing Ptx-loaded micelles and siRNA-loaded LDL has been developed. Results showed that the delivery system delivered siRNA and Ptx directly to cancer cells, enhancing the intracellular release of drugs and genes, increasing intracellular drug concentration, decreasing drug efflux, prolonging circulation, and reversing MDR.256,257
Cell-penetrating/tumor-targeting peptide–modified nanocarriers
Nanocarriers using cell-penetrating and/or tumor-targeting peptides for functionalization are a promising strategy, and have attracted the attention of researchers. In our previous report, we reviewed the classification of polypeptide- and polypeptide-modified nanocarriers in detail.258 In this report, recent research progress is summarized in the following paragraphs.
Epigallocatechin-3-gallate (EGCG), a major polyphenol in green tea, has been widely studied as a potential anticancer drug. Narayanan et al259 prepared targeted drug-loaded core–shell NPs using anti-EGFR and anti-HER2 antibodies, and entrapped a combination of Ptx and EGCG at different doses in the core and shell, respectively, using emulsion precipitation. Cellular uptake in MDA-MB231 cells was higher for targeted NPs than untargeted NPs at 24 hours. The sequential release of EGCG followed by Ptx from this core–shell nanocarrier sensitized Ptx-resistant MDA-MB231 cells to Ptx, induced their apoptosis, and inhibited NFκB activation. In addition, EGFR-peptide (GE11)-targeted, pH-sensitive docetaxel Dtx–Cur NPs260 and arginylglycylaspartic acid–modified lipid-coated PLGA NPs targeting delivery of both sorafenib and Qct261 achieved significant inhibition of tumor growth in vitro and in vivo.
In addition, galactosamine can recognize and bind to the asialoglycoprotein receptor on the surface of hepatocellular carcinoma cells, and a galactosamine-mediated drug-delivery carrier was significant for targeted liver cancer therapy.262,263 Glycyrrhizin, glycyrrhetinic acid, and mannose can serve as the guiding group in liver-targeted drug-delivery systems, with good potential.264–270 As natural endogenous ligands, bile acids have good biocompatibility and are ideal routes for targeting hepatocellular cancer.271 In addition, sialic acid,272 human Nanog,273 and hyaluronic acid274 are excellent targets in cancer therapy. Vapreotide is a somatostatin analogue and can be also used as a ligand for targeted drug delivery based on its high affinity to somatostatin receptors, which are overexpressed in many tumor cells.275 Several studies have shown that double-modified nanocarriers have also attracted considerable attention in anticancer drug research.276,277 Dual or multiple targeting also provides a new approach for antitumor therapy.
Physicochemical targeted drug-delivery systems
Physicochemical targeting refers to the binding of magnetic, pH-sensitive, temperature-sensitive, or electromagnetic wave–responsive materials onto the surface of drug-delivery systems (such as NPs and liposomes) to make them respond to various stimuli in vitro and in vivo (such as pH, temperature, applied magnetic fields, ultrasonic waves, infrared rays, and electromagnetic radiation) to ensure that the drug acts directly on the target area, increases drug concentration at the lesion site, and reduces adverse reactions. Most studies have used magnetic NPs, temperature-sensitive NPs, and pH-sensitive NPs.
NPs that are pH-sensitive have been designed to promote uptake in tumor cells278 and accelerate drug release at tumor sites, as the extracellular pH (6.5–7.2) of the tumor is different to that of normal tissue.216 Zhang et al278 developed a codelivery system for Dox and Cur using pH-sensitive NPs. Enhanced release in the acidic environment of cancer cells and enhanced cellular internalization of the cargoes delivered from Dox–Cur NPs were observed in SMMC7721 cells and human umbilical vein endothelial cells compared to the free drugs. Therefore, pH-sensitive NPs can provide a promising strategy for the effective inhibition of cancer in a synergistic manner. Danafar et al279 achieved codelivery of Cur and sulforaphane (SF) with PEGylated gold-coated Fe3O4 magnetic NPs as an effective and promising antitumor agent. Results showed that SF–Cur coloaded Fe3O4@Au NPs caused a decrease in cell viability and induced apoptosis by increasing the Bax:Bcl2 ratio. Moreover, photosensitizer NPs,280 thermosensitive NPs,281 and redox-sensitive NPs282 also provide new opportunities for nanosystems with anti-tumor TCM combinations.
Conclusion
The significant challenge posed by cancers, as well as adverse reactions and drug resistance induced by long-term treatment of a single drug, compels us to change our focus from a single target to the regulation of networks in vivo. Many complex factors cause cancer; therefore, it is rational that treatment should involve multiple components, genes, systems, and target pathways. The combination of drugs has resulted in a new approach to cancer treatment. Rational combinations of drugs not only result in synergy but also reduce the occurrence of drug resistance and adverse reactions, which has resulted in combination therapy, thus becoming a significant antitumor treatment in the clinic and in research. As such, this significant research direction may allow medical researchers to identify a chemotherapeutic combination regimen with high efficacy and low toxicity.
The combination of TCMs for clinical therapy has increased. TCM combinations can exert improved synergistic antitumor effects by adjusting the multiple signaling pathways of tumor cells. Compared with single-drug therapy, combinations of TCMs can reduce the toxicity and side effects of chemotherapy drugs and increase the antitumor effect of drugs. Simultaneously, TCM combinations and chemical drugs can improve immunofunction, relieve clinical symptoms, improve patient survival and quality of life, and improve the efficacy of chemotherapy drugs.
It should be noted that there are usually three approaches in targeted nanotechnology-based TCM-combination-therapy: nanodrugs combined with conventional preparations, coloading of two or more anticancer drugs in a single nanocarrier system (recorded as codelivery), and combined administration of different nanosystems. The loading of two drugs into a single well-designed nanocarrier synchronizes the pharmacokinetic and biological distribution of different drugs to achieve a synergistic effect, which has distinct advantages. This method has been summarized in detail. An increasing number of studies have shown that dual nanosystems have distinct advantages in antitumor treatment and can provide drugs for different targets or sites of action, as they are administered flexibly using different dose/time schedules. Consequently, the remaining two methods urgently require further investigation. In addition, with further comparative analyses of these three research methods, the most suitable form of drug use for cancers can be identified to provide basic considerations in terms of design principles and management progress.
Acknowledgments
This study was financially supported by the National Natural Science Foundation of China (81673605).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, et al. GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;2018(68):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Ferlay J, Colombet MI. Global and regional estimates of the incidence and mortality for 38 cancers: GLOBOCAN 2018. Lyon: International Agency for Research on Cancer/World Health Organization; 2018. [Google Scholar]
- 4.Li FM, Wang XQ. Identifying anticancer peptides by using improved hybrid compositions. Sci Rep. 2016;6:33910. doi: 10.1038/srep33910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng PP, Li J, Kros JM. Breakthroughs in modern cancer therapy and elusive cardiotoxicity: critical research-practice gaps, challenges, and insights. Med Res Rev. 2018;38(1):325–376. doi: 10.1002/med.21463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Q, Yang Z, Nie Y, Shi Y, Fan D. Multi-drug resistance in cancer chemotherapeutics: mechanisms and lab approaches. Cancer Lett. 2014;347(2):159–166. doi: 10.1016/j.canlet.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Li S, Zhang B, Jiang D, Wei Y, Zhang N. Herb network construction and co-module analysis for uncovering the combination rule of traditional Chinese herbal formulae. BMC Bioinformatics. 2010;11(S11):S6. doi: 10.1186/1471-2105-11-S11-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heath JR. Nanotechnologies for biomedical Science and translational medicine. Proc Natl Acad Sci U S A. 2015;112(47):14436–14443. doi: 10.1073/pnas.1515202112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ho BN, Pfeffer CM, Singh AT. Update on Nanotechnology-based drug delivery systems in cancer treatment. Anticancer Res. 2017;37(11):5975–5981. doi: 10.21873/anticanres.12044. [DOI] [PubMed] [Google Scholar]
- 10.Wang K, Kievit FM, Zhang M. Nanoparticles for cancer gene therapy: recent advances, challenges, and strategies. Pharmacol Res. 2016;114:56–66. doi: 10.1016/j.phrs.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Yang Y, Yu C. Advances in silica based nanoparticles for targeted cancer therapy. Nanomedicine. 2016;12(2):317–332. doi: 10.1016/j.nano.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 12.Grover JK, Yadav SP. Pharmacological actions and potential uses of Momordica charantia: a review. J Ethnopharmacol. 2004;93(1):123–132. doi: 10.1016/j.jep.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 13.Cyranoski D. Why Chinese medicine is heading for clinics around the world. Nature. 2018;561(7724):448–450. doi: 10.1038/d41586-018-06782-7. [DOI] [PubMed] [Google Scholar]
- 14.Anand P, Sundaram C, Jhurani S, Kunnumakkara AB, Aggarwal BB. Curcumin and cancer: an “old-age” disease with an “age-old” solution. Cancer Lett. 2008;267(1):133–164. doi: 10.1016/j.canlet.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 15.Duvoix A, Blasius R, Delhalle S, et al. Chemopreventive and therapeutic effects of curcumin. Cancer Lett. 2005;223(2):181–190. doi: 10.1016/j.canlet.2004.09.041. [DOI] [PubMed] [Google Scholar]
- 16.Zhang TD, Chen GQ, Wang ZG, Wang ZY, Chen SJ, Chen Z. Arsenic trioxide, a therapeutic agent for APL. Oncogene. 2001;20(49):7146–7153. doi: 10.1038/sj.onc.1204762. [DOI] [PubMed] [Google Scholar]
- 17.Dogra S, Bandi S, Viswanathan P, Gupta S. Arsenic trioxide amplifies cisplatin toxicity in human tubular cells transformed by HPV-16 E6/E7 for further therapeutic directions in renal cell carcinoma. Cancer Lett. 2015;356(2 Pt B):953–961. doi: 10.1016/j.canlet.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ji H, Li Y, Jiang F, et al. Inhibition of transforming growth factor beta/ SMAD signal by MiR-155 is involved in arsenic trioxide-induced anti-angiogenesis in prostate cancer. Cancer Sci. 2014;105(12):1541–1549. doi: 10.1111/cas.12548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang X, Jiang F, Mu J, et al. Arsenic trioxide attenuates the invasion potential of human liver cancer cells through the demethylation-activated microRNA-491. Toxicol Lett. 2014;227(2):75–83. doi: 10.1016/j.toxlet.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 20.Jiang X, Chen C, Zhao W, Zhang Z. Sodium arsenite and arsenic tri-oxide differently affect the oxidative stress, genotoxicity and apoptosis in A549 cells: an implication for the paradoxical mechanism. Environ Toxicol Pharmacol. 2013;36(3):891–902. doi: 10.1016/j.etap.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Walker AM, Stevens JJ, Ndebele K, Tchounwou PB. Evaluation of arsenic trioxide potential for lung cancer treatment: assessment of apoptotic mechanisms and oxidative damage. J Cancer Sci Ther. 2016;08(01):1–9. doi: 10.4172/1948-5956.1000379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alkhalaf M, Jaffal S. Potent antiproliferative effects of resveratrol on human osteosarcoma SJSA1 cells: novel cellular mechanisms involving the ERKs/p53 cascade. Free Radic Biol Med. 2006;41(2):318–325. doi: 10.1016/j.freeradbiomed.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 23.Zhu W, Qin W, Zhang K, et al. Trans-resveratrol alters mammary promoter hypermethylation in women at increased risk for breast cancer. Nutr Cancer. 2012;64(3):393–400. doi: 10.1080/01635581.2012.654926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel KR, Brown VA, Jones DJ, et al. Clinical pharmacology of resveratrol and its metabolites in colorectal cancer patients. Cancer Res. 2010;70(19):7392–7399. doi: 10.1158/0008-5472.CAN-10-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rauf A, Imran M, Butt MS, Nadeem M, Peters DG, Mubarak MS. Resveratrol as an anti-cancer agent: a review. Crit Rev Food Sci Nutr. 2018;58(9):1428–1447. doi: 10.1080/10408398.2016.1263597. [DOI] [PubMed] [Google Scholar]
- 26.Cai H, Scott E, Kholghi A, et al. Cancer chemoprevention: evidence of a nonlinear dose response for the protective effects of resveratrol in humans and mice. Sci Transl Med. 2015;7(298):298ra117. doi: 10.1126/scitranslmed.aaa7619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oi N, Yuan J, Malakhova M, et al. Resveratrol induces apoptosis by directly targeting Ras-GTPase-activating protein SH3 domain-binding protein 1. Oncogene. 2015;34(20):2660–2671. doi: 10.1038/onc.2014.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zou M, Wang J, Gao J, Han H, Fang Y. Phosphoproteomic analysis of the antitumor effects of ginsenoside Rg3 in human breast cancer cells. Oncol Lett. 2018;15(3):2889–2898. doi: 10.3892/ol.2017.7654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang X, Zou J, Cai H, et al. Ginsenoside Rg3 inhibits colorectal tumor growth via down-regulation of C/EBPβ/NF-κB signaling. Biomed Pharmacother. 2017;96:1240–1245. doi: 10.1016/j.biopha.2017.11.092. [DOI] [PubMed] [Google Scholar]
- 30.Liu T, Zhao L, Hou H, Ding L, Chen W, Li X. Ginsenoside 20(S)-Rg3 suppresses ovarian cancer migration via hypoxia-inducible factor 1 alpha and nuclear factor-kappa B signals. Tumour Biol. 2017;39(5):101042831769222. doi: 10.1177/1010428317692225. [DOI] [PubMed] [Google Scholar]
- 31.Su MQ, Zhou YR, Rao X, et al. Baicalein induces the apoptosis of HCT116 human colon cancer cells via the upregulation of DEPP/ Gadd45a and activation of MAPKs. Int J Oncol. 2018;53(2):750–760. doi: 10.3892/ijo.2018.4402. [DOI] [PubMed] [Google Scholar]
- 32.Song L, Chen X, Wang P, Gao S, Qu C, Liu L. Effects of baicalein on pancreatic cancer stem cells via modulation of sonic hedgehog pathway. Acta Biochim Biophys Sin. 2018;50(6):586–596. doi: 10.1093/abbs/gmy045. [DOI] [PubMed] [Google Scholar]
- 33.Chao JI, Su WC, Liu H-F. Baicalein induces cancer cell death and proliferation retardation by the inhibition of CDC2 kinase and survivin associated with opposite role of p38 mitogen-activated protein kinase and Akt. Mol Cancer Ther. 2007;6(11):3039–3048. doi: 10.1158/1535-7163.MCT-07-0281. [DOI] [PubMed] [Google Scholar]
- 34.Zhou Q, Wang S, Zhang H, et al. The combination of baicalin and baicalein enhances apoptosis via the ERK/p38 MAPK pathway in human breast cancer cells. Acta Pharmacol Sin. 2009;30(12):1648–1658. doi: 10.1038/aps.2009.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yan XI, Rui X, Zhang KAI. Baicalein inhibits the invasion of gastric cancer cells by suppressing the activity of the p38 signaling pathway. Oncol Rep. 2015;33(2):737–743. doi: 10.3892/or.2014.3669. [DOI] [PubMed] [Google Scholar]
- 36.Wang YF, Li T, Tang ZH, et al. Baicalein triggers autophagy and inhibits the protein kinase B/Mammalian target of rapamycin pathway in hepatocellular carcinoma HepG2 cells. Phytother Res. 2015;29(5):674–679. doi: 10.1002/ptr.5298. [DOI] [PubMed] [Google Scholar]
- 37.Wu JY, Tsai KW, Li YZ, et al. Anti-Bladder-Tumor effect of baicalein from Scutellaria baicalensis Georgi and its application in vivo. Evid Based Complement Alternat Med. 2013;2013:579751. doi: 10.1155/2013/579751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guo Z, Hu X, Xing Z, et al. Baicalein inhibits prostate cancer cell growth and metastasis via the caveolin-1/AKT/mTOR pathway. Mol Cell Biochem. 2015;406(1–2):111–119. doi: 10.1007/s11010-015-2429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peng Y, Guo C, Yang Y, et al. Baicalein induces apoptosis of human cervical cancer HeLa cells in vitro. Mol Med Rep. 2015;11(3):2129–2134. doi: 10.3892/mmr.2014.2885. [DOI] [PubMed] [Google Scholar]
- 40.Chandrashekar N, Selvamani A, Subramanian R, Pandi A, Thiruvengadam D. Baicalein inhibits pulmonary carcinogenesis-associated inflammation and interferes with COX-2, MMP-2 and MMP-9 expressions in-vivo. Toxicol Appl Pharmacol. 2012;261(1):10–21. doi: 10.1016/j.taap.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 41.Yu J, Guo QL, You QD, et al. Gambogic acid-induced G2/M phase cell-cycle arrest via disturbing CDK7-mediated phosphorylation of CDC2/p34 in human gastric carcinoma BGC-823 cells. Carcinogenesis. 2007;28(3):632–638. doi: 10.1093/carcin/bgl168. [DOI] [PubMed] [Google Scholar]
- 42.Wang X, Deng R, Lu Y, et al. Gambogic acid as a non-competitive inhibitor of ATP-binding cassette transporter B1 reverses the multidrug resistance of human epithelial cancers by promoting ATP-binding cassette transporter B1 protein degradation. Basic Clin Pharmacol Toxicol. 2013;112(1):25–33. doi: 10.1111/j.1742-7843.2012.00921.x. [DOI] [PubMed] [Google Scholar]
- 43.Wu ZQ, Guo QL, You QD, Zhao L, Gu H-Y. Gambogic acid inhibits proliferation of human lung carcinoma SPC-A1 cells in vivo and in vitro and represses telomerase activity and telomerase reverse transcriptase mRNA expression in the cells. Biol Pharm Bull. 2004;27(11):1769–1774. doi: 10.1248/bpb.27.1769. [DOI] [PubMed] [Google Scholar]
- 44.Wang C, Zhang H, Chen Y, Shi F, Chen B. Gambogic acid-loaded magnetic Fe(3)O(4) nanoparticles inhibit Panc-1 pancreatic cancer cell proliferation and migration by inactivating transcription factor ETS1. Int J Nanomedicine. 2012;7:781–787. doi: 10.2147/IJN.S28509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo QL, You QD, Wu ZQ, Yuan ST, Zhao L. General gambogic acids inhibited growth of human hepatoma SMMC-7721 cells in vitro and in nude mice. Acta Pharmacol Sin. 2004;25(6):769–774. [PubMed] [Google Scholar]
- 46.Zhu X, Zhang H, Lin Y, et al. Mechanisms of gambogic acid-induced apoptosis in non-small cell lung cancer cells in relation to transferrin receptors. J Chemother. 2009;21(6):666–672. doi: 10.1179/joc.2009.21.6.666. [DOI] [PubMed] [Google Scholar]
- 47.Nie F, Zhang X, Qi Q, et al. Reactive oxygen species accumulation contributes to gambogic acid-induced apoptosis in human hepatoma SMMC-7721 cells. Toxicology. 2009;260(1–3):60–67. doi: 10.1016/j.tox.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 48.Yan F, Wang M, Chen H, et al. Gambogenic acid mediated apoptosis through the mitochondrial oxidative stress and inactivation of Akt signaling pathway in human nasopharyngeal carcinoma CNE-1 cells. Eur J Pharmacol. 2011;652(1–3):23–32. doi: 10.1016/j.ejphar.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 49.Chen HB, Zhou LZ, Mei L, et al. Gambogenic acid-induced time- and dose-dependent growth inhibition and apoptosis involving Akt pathway inactivation in U251 glioblastoma cells. J Nat Med. 2012;66(1):62–69. doi: 10.1007/s11418-011-0553-7. [DOI] [PubMed] [Google Scholar]
- 50.Wang K, Tang Y, Sun M, et al. The mechanism of neogambogic acid-induced apoptosis in human MCF-7 cells. Acta Biochim Biophys Sin. 2011;43(9):698–702. doi: 10.1093/abbs/gmr063. [DOI] [PubMed] [Google Scholar]
- 51.Mei W, Dong C, Hui C, et al. Gambogenic acid kills lung cancer cells through aberrant autophagy. PLoS One. 2014;9(1):e83604. doi: 10.1371/journal.pone.0083604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li Q, Cheng H, Zhu G, et al. Gambogenic acid inhibits proliferation of A549 cells through apoptosis-inducing and cell cycle arresting. Biol Pharm Bull. 2010;33(3):415–420. doi: 10.1248/bpb.33.415. [DOI] [PubMed] [Google Scholar]
- 53.Cheng H, Su JJ, Peng JY, et al. Gambogenic acid inhibits proliferation of A549 cells through apoptosis inducing through up-regulation of the p38 MAPK cascade. J Asian Nat Prod Res. 2011;13(11):993–1002. doi: 10.1080/10286020.2011.605062. [DOI] [PubMed] [Google Scholar]
- 54.Zhang X, Xu Q, Saiki I. Quercetin inhibits the invasion and mobility of murine melanoma B16-BL6 cells through inducing apoptosis via decreasing Bcl-2 expression. Clin Exp Metastasis. 2000;18(5):415–421. doi: 10.1023/a:1010960615370. [DOI] [PubMed] [Google Scholar]
- 55.Tsai PH, Cheng CH, Lin C-Y, et al. Dietary flavonoids luteolin and quercetin suppressed cancer stem cell properties and metastatic potential of isolated prostate cancer cells. Anticancer Res. 2016;36(12):6367–6380. doi: 10.21873/anticanres.11234. [DOI] [PubMed] [Google Scholar]
- 56.Jia L, Huang S, Yin X, Zan Y, Guo Y, Han L. Quercetin suppresses the mobility of breast cancer by suppressing glycolysis through Akt-mTOR pathway mediated autophagy induction. Life Sci. 2018;208:123–130. doi: 10.1016/j.lfs.2018.07.027. [DOI] [PubMed] [Google Scholar]
- 57.Calgarotto AK, Maso V, Junior GC, et al. Antitumor activities of quercetin and green tea in xenografts of human leukemia HL60 cells. Sci Rep. 2018;8(1):3459. doi: 10.1038/s41598-018-21516-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Anand David AV, Arulmoli R, Parasuraman S. Overviews of biological importance of quercetin: a bioactive flavonoid. Pharmacogn Rev. 2016;10(20):84–89. doi: 10.4103/0973-7847.194044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lugli E, Ferraresi R, Roat E, et al. Quercetin inhibits lymphocyte activation and proliferation without inducing apoptosis in peripheral mononuclear cells. Leuk Res. 2009;33(1):140–150. doi: 10.1016/j.leukres.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 60.Zhang H, Li H, Liu Z, et al. Triptolide inhibits the proliferation and migration of medulloblastoma DAOY cells by upregulation of microRNA-138. J Cell Biochem. 2018;119(12):9866–9877. doi: 10.1002/jcb.27307. [DOI] [PubMed] [Google Scholar]
- 61.Mao X, Tong J, Wang Y, Zhu Z, Yin Y, Wang Y. Triptolide exhibits antitumor effects by reversing hypermethylation of WIF1 in lung cancer cells. Mol Med Rep. 2018;18(3):3041–3049. doi: 10.3892/mmr.2018.9263. [DOI] [PubMed] [Google Scholar]
- 62.Zhou ZL, Yang YX, Ding J, Li YC, Miao Z-H. Triptolide: structural modifications, structure-activity relationships, bioactivities, clinical development and mechanisms. Nat Prod Rep. 2012;29(4):457–475. doi: 10.1039/c2np00088a. [DOI] [PubMed] [Google Scholar]
- 63.Li SG, Shi QW, Yuan LY, et al. C-Myc-dependent repression of two oncogenic miRNA clusters contributes to triptolide-induced cell death in hepatocellular carcinoma cells. J Exp Clin Cancer Res. 2018;37:51. doi: 10.1186/s13046-018-0698-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang Y, Liu T, Li H. Enhancement of triptolide-loaded micelles on tumorigenicity inhibition of human ovarian cancer. J Biomater Sci Polym Ed. 2016;27(7):545–556. doi: 10.1080/09205063.2015.1131667. [DOI] [PubMed] [Google Scholar]
- 65.Hu G, Gong X, Wang L, et al. Triptolide promotes the clearance of α-synuclein by enhancing autophagy in neuronal cells. Mol Neurobiol. 2017;54(3):2361–2372. doi: 10.1007/s12035-016-9808-3. [DOI] [PubMed] [Google Scholar]
- 66.Kim SH, Kang JG, Kim CS, et al. Synergistic cytotoxicity of BIIB021 with triptolide through suppression of PI3K/AKT/mTOR and NF-κB signal pathways in thyroid carcinoma cells. Biomed Pharmacother. 2016;83:22–32. doi: 10.1016/j.biopha.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 67.Li W, Yang Y, Hu Z, Ling S, Fang M. Neuroprotective effects of DAHP and triptolide in focal cerebral ischemia via apoptosis inhibition and PI3K/Akt/mTOR pathway activation. Front Neuroanat. 2015;9:48. doi: 10.3389/fnana.2015.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yao Z, Wan Y, Li B, et al. Berberine induces mitochondrialmediated apoptosis and protective autophagy in human malignant pleural mesothelioma NCIH2452 cells. Oncol Rep. 2018;40(6):3603–3610. doi: 10.3892/or.2018.6757. [DOI] [PubMed] [Google Scholar]
- 69.Fukuda K, Hibiya Y, Mutoh M, Koshiji M, Akao S, Fujiwara H. Inhibition by berberine of cyclooxygenase-2 transcriptional activity in human colon cancer cells. J Ethnopharmacol. 1999;66(2):227–233. doi: 10.1016/s0378-8741(98)00162-7. [DOI] [PubMed] [Google Scholar]
- 70.Wang Z, Wang Y-S, Chang Z-M, et al. Berberine-loaded Janus nanocarriers for magnetic field-enhanced therapy against hepatocellular carcinoma. Chem Biol Drug Des. 2017;89(3):464–469. doi: 10.1111/cbdd.12866. [DOI] [PubMed] [Google Scholar]
- 71.Kuo HP, Chuang TC, Yeh MH, et al. Growth suppression of HER2-overexpressing breast cancer cells by berberine via modulation of the HER2/PI3K/AKT signaling pathway. J Agric Food Chem. 2011;59(15):8216–8224. doi: 10.1021/jf2012584. [DOI] [PubMed] [Google Scholar]
- 72.Kim S, Han J, Lee SK, et al. Berberine suppresses the TPA-induced MMP-1 and MMP-9 expressions through the inhibition of PKC-α in breast cancer cells. J Surg Res. 2012;176(1):e21–e29. doi: 10.1016/j.jss.2011.11.1041. [DOI] [PubMed] [Google Scholar]
- 73.Lin CC, Yang JS, Chen JT, et al. Berberine induces apoptosis in human HSC-3 oral cancer cells via simultaneous activation of the death receptor-mediated and mitochondrial pathway. Anticancer Res. 2007;27(5A):3371–3378. [PubMed] [Google Scholar]
- 74.Mantena SK, Sharma SD, Katiyar SK. Berberine inhibits growth, induces G1 arrest and apoptosis in human epidermoid carcinoma A431 cells by regulating Cdki-Cdk-cyclin cascade, disruption of mitochondrial membrane potential and cleavage of caspase 3 and PARP. Carcinogenesis. 2006;27(10):2018–2027. doi: 10.1093/carcin/bgl043. [DOI] [PubMed] [Google Scholar]
- 75.Shin DS, Kim HN, Shin KD, et al. Cryptotanshinone inhibits constitutive signal transducer and activator of transcription 3 function through blocking the dimerization in DU145 prostate cancer cells. Cancer Res. 2009;69(1):193–202. doi: 10.1158/0008-5472.CAN-08-2575. [DOI] [PubMed] [Google Scholar]
- 76.Chen W, Luo Y, Liu L, et al. Cryptotanshinone inhibits cancer cell proliferation by suppressing mammalian target of rapamycin-mediated cyclin D1 expression and RB phosphorylation. Cancer Prev Res. 2010;3(8):1015–1025. doi: 10.1158/1940-6207.CAPR-10-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen L, Wang HJ, Xie W, Yao Y, Zhang YS, Wang H. Cryptotanshinone inhibits lung tumorigenesis and induces apoptosis in cancer cells in vitro and in vivo. Mol Med Rep. 2014;9(6):2447–2452. doi: 10.3892/mmr.2014.2093. [DOI] [PubMed] [Google Scholar]
- 78.Xiao W, Zhu MX, Zhu MX, Pan XJ, Yang ZH, Zhou S-Y. Inhibition of cyclooxygenase-2 by tetramethylpyrazine and its effects on A549 cell invasion and metastasis. Int J Oncol. 2012;40(6):2029–2037. doi: 10.3892/ijo.2012.1375. [DOI] [PubMed] [Google Scholar]
- 79.Wang Y, Fu Q, Zhao W. Tetramethylpyrazine inhibits osteosarcoma cell proliferation via downregulation of NF-κB in vitro and in vivo. Mol Med Rep. 2013;8(4):984–988. doi: 10.3892/mmr.2013.1611. [DOI] [PubMed] [Google Scholar]
- 80.Wang SJ, Gao Y, Chen H, et al. Dihydroartemisinin inactivates NF-kappaB and potentiates the anti-tumor effect of gemcitabine on pancreatic cancer both in vitro and in vivo. Cancer Lett. 2010;293(1):99–108. doi: 10.1016/j.canlet.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 81.Ji Y, Zhang YC, Pei LB, Shi LL, Yan JL, Ma XH. Anti-tumor effects of dihydroartemisinin on human osteosarcoma. Mol Cell Biochem. 2011;351(1–2):99–108. doi: 10.1007/s11010-011-0716-6. [DOI] [PubMed] [Google Scholar]
- 82.Gao X, Luo Z, Xiang T, Wang K, Li J, Wang P. Dihydroartemisinin induces endoplasmic reticulum stress-mediated apoptosis in HepG2 human hepatoma cells. Tumori. 2011;97(6):771–780. doi: 10.1177/030089161109700615. [DOI] [PubMed] [Google Scholar]
- 83.Lai H, Singh NP. Selective cancer cell cytotoxicity from exposure to dihydroartemisinin and holotransferrin. Cancer Lett. 1995;91(1):41–46. doi: 10.1016/0304-3835(94)03716-v. [DOI] [PubMed] [Google Scholar]
- 84.Lai H, Sasaki T, Singh NP, Messay A. Effects of artemisinin-tagged holotransferrin on cancer cells. Life Sci. 2005;76(11):1267–1279. doi: 10.1016/j.lfs.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 85.Chen H, Gu S, Dai H, Li X, Zhang Z. Dihydroartemisinin sensitizes human lung adenocarcinoma A549 cells to arsenic trioxide via apoptosis. Biol Trace Elem Res. 2017;179(2):203–212. doi: 10.1007/s12011-017-0975-5. [DOI] [PubMed] [Google Scholar]
- 86.Oh M, Choi YH, Choi S, et al. Anti-proliferating effects of ginsenoside Rh2 on MCF-7 human breast cancer cells. Int J Oncol. 1999;14(5):869–875. doi: 10.3892/ijo.14.5.869. [DOI] [PubMed] [Google Scholar]
- 87.Nakata H, Kikuchi Y, Tode T, et al. Inhibitory effects of ginsenoside Rh2 on tumor growth in nude mice bearing human ovarian cancer cells. Jpn J Cancer Res. 1998;89(7):733–740. doi: 10.1111/j.1349-7006.1998.tb03278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xie X, Eberding A, Madera C, et al. Rh2 synergistically enhances paclitaxel or mitoxantrone in prostate cancer models. J Urol. 2006;175(5):1926–1931. doi: 10.1016/S0022-5347(05)00891-8. [DOI] [PubMed] [Google Scholar]
- 89.Xia T, Wang YN, Zhou CX, et al. Ginsenoside Rh2 and Rg3 inhibit cell proliferation and induce apoptosis by increasing mitochondrial reactive oxygen species in human leukemia Jurkat cells. Mol Med Rep. 2017;15(6):3591–3598. doi: 10.3892/mmr.2017.6459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yang J, Yuan D, Xing T, et al. Ginsenoside Rh2 inhibiting HCT116 colon cancer cell proliferation through blocking PDZ-binding kinase/T-LAK cell-originated protein kinase. J Ginseng Res. 2016;40(4):400–408. doi: 10.1016/j.jgr.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yang Z, Zhao T, Liu H, Zhang L. Ginsenoside Rh2 inhibits hepatocellular carcinoma through β-catenin and autophagy. Sci Rep. 2016;6(1):19383. doi: 10.1038/srep19383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Huang J, Peng K, Wang L, et al. Ginsenoside Rh2 inhibits proliferation and induces apoptosis in human leukemia cells via TNF-α signaling pathway. Acta Biochim Biophys Sin. 2016;48(8):750–755. doi: 10.1093/abbs/gmw049. [DOI] [PubMed] [Google Scholar]
- 93.Li S, Gao Y, Ma W, et al. EGFR signaling-dependent inhibition of glioblastoma growth by ginsenoside Rh2. Tumor Biol. 2014;35(6):5593–5598. doi: 10.1007/s13277-014-1739-x. [DOI] [PubMed] [Google Scholar]
- 94.Han S, Jeong AJ, Yang H, et al. Ginsenoside 20(S)-Rh2 exerts anticancer activity through targeting IL-6-induced JAK2/STAT3 pathway in human colorectal cancer cells. J Ethnopharmacol. 2016;194:83–90. doi: 10.1016/j.jep.2016.08.039. [DOI] [PubMed] [Google Scholar]
- 95.Guan N, Huo X, Zhang Z, Zhang S, Luo J, Guo W. Ginsenoside Rh2 inhibits metastasis of glioblastoma multiforme through Akt-regulated MMP13. Tumor Biol. 2015;36(9):6789–6795. doi: 10.1007/s13277-015-3387-1. [DOI] [PubMed] [Google Scholar]
- 96.Abedinpour P, Baron VT, Chrastina A, et al. Plumbagin improves the efficacy of androgen deprivation therapy in prostate cancer: a pre-clinical study. Prostate. 2017;77(16):1550–1562. doi: 10.1002/pros.23428. [DOI] [PubMed] [Google Scholar]
- 97.Kawiak A, Domachowska A. Plumbagin suppresses the invasion of HER2-overexpressing breast cancer cells through inhibition of IKKα-Mediated NF-κB activation. PLoS One. 2016;11(10):e0164064. doi: 10.1371/journal.pone.0164064. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 98.Oh TI, Yun JM, Park EJ, et al. Plumbagin suppresses α-MSH-Induced melanogenesis in B16F10 mouse melanoma cells by inhibiting tyrosinase activity. Int J Mol Sci. 2017;18(2):320. doi: 10.3390/ijms18020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liu Y, Cai Y, He C, Chen M, Li H. Anticancer properties and pharmaceutical applications of plumbagin: a review. Am J Chin Med. 2017;45(3):423–441. doi: 10.1142/S0192415X17500264. [DOI] [PubMed] [Google Scholar]
- 100.Pan ST, Li ZL, He ZX, Qiu JX, Zhou S-F. Molecular mechanisms for tumour resistance to chemotherapy. Clin Exp Pharmacol Physiol. 2016;43(8):723–737. doi: 10.1111/1440-1681.12581. [DOI] [PubMed] [Google Scholar]
- 101.Crona DJ, Faso A, Nishijima TF, Mcgraw KA, Galsky MD, Milowsky MI. A systematic review of strategies to prevent cisplatin-induced nephrotoxicity. Oncologist. 2017;22(5):609–619. doi: 10.1634/theoncologist.2016-0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhu J, Carozzi VA, Reed N, et al. Ethoxyquin provides neuroprotection against cisplatin-induced neurotoxicity. Sci Rep. 2016;6(1):28861. doi: 10.1038/srep28861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Karasawa T, Steyger PS. An integrated view of cisplatin-induced nephrotoxicity and ototoxicity. Toxicol Lett. 2015;237(3):219–227. doi: 10.1016/j.toxlet.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hu S, Li X, Xu R, et al. The synergistic effect of resveratrol in combination with cisplatin on apoptosis via modulating autophagy in A549 cells. Acta Biochim Biophys Sin. 2016;48(6):528–535. doi: 10.1093/abbs/gmw026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gao LP, Li Z, Guo ZY, Zhao Y-M. The effects of vitamin C on DDP-induced anemia in rats. Toxicol Mech Methods. 2013;23(6):383–388. doi: 10.3109/15376516.2013.769656. [DOI] [PubMed] [Google Scholar]
- 106.Lu DY, Chen EH, Wu HY, et al. Anticancer drug combinations, how far we can go through? Anticancer Agents Med Chem. 2017;17(1):21–28. [PubMed] [Google Scholar]
- 107.Webster RM. Combination therapies in oncology. Nat Rev Drug Discov. 2016;15(2):81–82. doi: 10.1038/nrd.2016.3. [DOI] [PubMed] [Google Scholar]
- 108.Zhang W, Shi H, Chen C, et al. Curcumin enhances cisplatin sensitivity of human NSCLC cell lines through influencing Cu-Sp1-CTR1 regulatory loop. Phytomedicine. 2018;48:51–61. doi: 10.1016/j.phymed.2018.04.058. [DOI] [PubMed] [Google Scholar]
- 109.Mohapatra P, Satapathy SR, Siddharth S, Das D, Nayak A, Kundu CN. Resveratrol and curcumin synergistically induces apoptosis in cigarette smoke condensate transformed breast epithelial cells through a p21(Waf1/Cip1) mediated inhibition of Hh-Gli signaling. Int J Biochem Cell Biol. 2015;66:75–84. doi: 10.1016/j.biocel.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 110.Xia C, Bai X, Hou X, et al. Cryptotanshinone reverses cisplatin resistance of human lung carcinoma A549 cells through down-regulating Nrf2 pathway. Cell Physiol Biochem. 2015;37(2):816–824. doi: 10.1159/000430398. [DOI] [PubMed] [Google Scholar]
- 111.Li CJ, Chu CY, Huang LH, et al. Synergistic anticancer activity of triptolide combined with cisplatin enhances apoptosis in gastric cancer in vitro and in vivo. Cancer Lett. 2012;319(2):203–213. doi: 10.1016/j.canlet.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 112.Che JB, Liu ZH, Ma HB, et al. Influence of As2O3 combined with ginsenosides Rg3 on inhibition of lung cancer NCI-H1299 cells and on subsistence of nude mice bearing hepatoma. Asian Pac J Trop Med. 2014;7(10):772–775. doi: 10.1016/S1995-7645(14)60134-6. [DOI] [PubMed] [Google Scholar]
- 113.Yuan Z, Jiang H, Zhu X, Liu X, Li J. Ginsenoside Rg3 promotes cytotoxicity of paclitaxel through inhibiting NF-κB signaling and regulating Bax/Bcl-2 expression on triple-negative breast cancer. Biomed Pharmacother. 2017;89:227–232. doi: 10.1016/j.biopha.2017.02.038. [DOI] [PubMed] [Google Scholar]
- 114.Chang L, Huo B, Lv Y, Wang Y, Liu W. Ginsenoside Rg3 enhances the inhibitory effects of chemotherapy on esophageal squamous cell carcinoma in mice. Mol Clin Oncol. 2014;2(6):1043–1046. doi: 10.3892/mco.2014.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tang Q, Ji F, Sun W, et al. Combination of baicalein and 10-hydroxy camptothecin exerts remarkable synergetic anti-cancer effects. Phytomedicine. 2016;23(14):1778–1786. doi: 10.1016/j.phymed.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 116.Zhen YS. Anticancer Drug research and development. Beijing, China: Chemical Industry Press; 2004. [Google Scholar]
- 117.Zhan Y, Chen Y, Liu R, Zhang H, Zhang Y. Potentiation of paclitaxel activity by curcumin in human breast cancer cell by modulating apoptosis and inhibiting EGFR signaling. Arch Pharm Res. 2014;37(8):1086–1095. doi: 10.1007/s12272-013-0311-3. [DOI] [PubMed] [Google Scholar]
- 118.Liu N, Huang H, Xu L, et al. The combination of proteasome inhibitors bortezomib and gambogic acid triggers synergistic cytotoxicity in vitro but not in vivo. Toxicol Lett. 2014;224(3):333–340. doi: 10.1016/j.toxlet.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 119.Majumdar AP, Banerjee S, Nautiyal J, et al. Curcumin synergizes with resveratrol to inhibit colon cancer. Nutr Cancer. 2009;61(4):544–553. doi: 10.1080/01635580902752262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Masuelli L, Marzocchella L, Focaccetti C, et al. Resveratrol and diallyl disulfide enhance curcumin-induced sarcoma cell apoptosis. Front Biosci. 2012;17(1):498–508. doi: 10.2741/3940. [DOI] [PubMed] [Google Scholar]
- 121.Sánchez Y, Simón GP, Calviño E, de Blas E, Aller P. Curcumin stimulates reactive oxygen species production and potentiates apoptosis induction by the antitumor drugs arsenic trioxide and lonidamine in human myeloid leukemia cell lines. J Pharmacol Exp Ther. 2010;335(1):114–123. doi: 10.1124/jpet.110.168344. [DOI] [PubMed] [Google Scholar]
- 122.Fehl DJ, Ahmed M. Curcumin promotes the oncoltyic capacity of vesicular stomatitis virus for the treatment of prostate cancers. Virus Res. 2017;228:14–23. doi: 10.1016/j.virusres.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 123.Zhang JY, Lin MT, Zhou MJ, et al. Combinational treatment of cur-cumin and quercetin against gastric cancer MGC-803 cells in vitro. Molecules. 2015;20(6):11524–11534. doi: 10.3390/molecules200611524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li Y, Feng L, Li Y, Jiang W, Shan N, Wang X. Artesunate possesses anti-leukemia properties that can be enhanced by arsenic trioxide. Leuk Lymphoma. 2014;55(6):1366–1372. doi: 10.3109/10428194.2013.829573. [DOI] [PubMed] [Google Scholar]
- 125.Tomuleasa C, Soritau O, Fischer-Fodor E, et al. Arsenic trioxide plus cisplatin/interferon α-2b/doxorubicin/capecitabine combination chemotherapy for unresectable hepatocellular carcinoma. Hematol Oncol Stem Cell Ther. 2011;4(2):60–66. doi: 10.5144/1658-3876.2011.60. [DOI] [PubMed] [Google Scholar]
- 126.Wang W, Qin SK, Chen BA, Chen HY. Experimental study on antitumor effect of arsenic trioxide in combination with cisplatin or doxorubicin on hepatocellular carcinoma. World J Gastroenterol. 2001;7(5):702–705. doi: 10.3748/wjg.v7.i5.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zhao YY, Yu L, Liu BL, He XJ, Zhang B-Y. Downregulation of P-gp, Ras and p-ERK1/2 contributes to the arsenic trioxide-induced reduction in drug resistance towards doxorubicin in gastric cancer cell lines. Mol Med Rep. 2015;12(5):7335–7343. doi: 10.3892/mmr.2015.4367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yu Q, Chen B, Zhang X, Qian W, Ye B, Zhou Y. Arsenic trioxide-enhanced, matrine-induced apoptosis in multiple myeloma cell lines. Planta Med. 2013;79(09):775–781. doi: 10.1055/s-0032-1328554. [DOI] [PubMed] [Google Scholar]
- 129.Rai G, Mishra S, Suman S, Shukla Y. Resveratrol improves the anticancer effects of doxorubicin in vitro and in vivo models: a mechanistic insight. Phytomedicine. 2016;23(3):233–242. doi: 10.1016/j.phymed.2015.12.020. [DOI] [PubMed] [Google Scholar]
- 130.Jiang Q, Yang M, Qu Z, Zhou J, Zhang Q. Resveratrol enhances anticancer effects of paclitaxel in HepG2 human liver cancer cells. BMC Complement Altern Med. 2017;17(1):477. doi: 10.1186/s12906-017-1956-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kong F, Zhang R, Zhao X, Zheng G, Wang Z, Wang P. Resveratrol raises in vitro anticancer effects of paclitaxel in NSCLC cell line A549 through COX-2 expression. Korean J Physiol Pharmacol. 2017;21(5):465–474. doi: 10.4196/kjpp.2017.21.5.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yuan Y, Xue X, Guo RB, Sun XL, Hu G. Resveratrol enhances the antitumor effects of temozolomide in glioblastoma via ROS-dependent AMPK-TSC-mTOR signaling pathway. CNS Neurosci Ther. 2012;18(7):536–546. doi: 10.1111/j.1755-5949.2012.00319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tomas-Hernández S, Blanco J, Rojas C, et al. Resveratrol potently counteracts quercetin starvation-induced autophagy and sensitizes HepG2 cancer cells to apoptosis. Mol Nutr Food Res. 2018;62(5):1700610. doi: 10.1002/mnfr.201700610. [DOI] [PubMed] [Google Scholar]
- 134.Zhao XY, Yang S, Chen YR, Li PC, Dou MM, Zhang J. Resveratrol and arsenic trioxide act synergistically to kill tumor cells in vitro and in vivo. PLoS One. 2014;9(6):e98925. doi: 10.1371/journal.pone.0098925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kim SM, Lee SY, Yuk DY, et al. Inhibition of NF-kappaB by ginsenoside Rg3 enhances the susceptibility of colon cancer cells to docetaxel. Arch Pharm Res. 2009;32(5):755–765. doi: 10.1007/s12272-009-1515-4. [DOI] [PubMed] [Google Scholar]
- 136.Pan Q, Xue M, Xiao S-S, Wan Y-J, Xu D-B. A combination therapy with baicalein and taxol promotes mitochondria-mediated cell apoptosis: involving in Akt/β-Catenin signaling pathway. DNA Cell Biol. 2016;35(11):646–656. doi: 10.1089/dna.2016.3312. [DOI] [PubMed] [Google Scholar]
- 137.Wang LH, Li Y, Yang SN, et al. Gambogic acid synergistically potentiates cisplatin-induced apoptosis in non-small-cell lung cancer through suppressing NF-κB and MAPK/HO-1 signalling. Br J Cancer. 2014;110(2):341–352. doi: 10.1038/bjc.2013.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Xia G, Wang H, Song Z, Meng Q, Huang X, Huang X. Gambogic acid sensitizes gemcitabine efficacy in pancreatic cancer by reducing the expression of ribonucleotide reductase subunit-M2 (RRM2) J Exp Clin Cancer Res. 2017;36(1):107. doi: 10.1186/s13046-017-0579-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Jiang XL, Zhang Y, Luo CL, Wu XH. Targeting renal cell carcinoma with gambogic acid in combination with sunitinib in vitro and in vivo. Asian Pac J Cancer Prev. 2012;13(12):6463–6468. doi: 10.7314/apjcp.2012.13.12.6463. [DOI] [PubMed] [Google Scholar]
- 140.He Y, Ding J, Lin Y, et al. Gambogenic acid alters chemosensitivity of breast cancer cells to adriamycin. BMC Complement Altern Med. 2015;15(1):181. doi: 10.1186/s12906-015-0710-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Chen R, Zhang H, Liu P, Wu X, Chen B. Gambogenic acid synergistically potentiates bortezomib-induced apoptosis in multiple myeloma. J Cancer. 2017;8(5):839–851. doi: 10.7150/jca.17657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ma ZS, Huynh TH, Ng CP, Do PT, Nguyen TH, Huynh H. Reduction of CWR22 prostate tumor xenograft growth by combined tamoxifen-quercetin treatment is associated with inhibition of angiogenesis and cellular proliferation. Int J Oncol. 2004;24(5):1297–1304. [PubMed] [Google Scholar]
- 143.Sun S, Gong F, Liu P, Miao Q. Metformin combined with quercetin synergistically repressed prostate cancer cells via inhibition of VEGF/ PI3K/Akt signaling pathway. Gene. 2018;664:50–57. doi: 10.1016/j.gene.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 144.Chan ST, Chuang CH, Lin YC, Liao JW, Lii CK, Yeh S-L. Quercetin enhances the antitumor effect of trichostatin A and suppresses muscle wasting in tumor-bearing mice. Food Funct. 2018;9(2):871–879. doi: 10.1039/c7fo01444a. [DOI] [PubMed] [Google Scholar]
- 145.Tang Q, Ji F, Wang J, Guo L, Li Y, Bao Y. Quercetin exerts synergetic anti-cancer activity with 10-hydroxy camptothecin. Eur J Pharm Sci. 2017;109:223–232. doi: 10.1016/j.ejps.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 146.Lei CS, Hou YC, Pai MH, Lin MT, Yeh S-L. Effects of quercetin combined with anticancer drugs on metastasis-associated factors of gastric cancer cells: in vitro and in vivo studies. J Nutr Biochem. 2018;51:105–113. doi: 10.1016/j.jnutbio.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 147.Alsaied OA, Sangwan V, Banerjee S, et al. Sorafenib and triptolide as combination therapy for hepatocellular carcinoma. Surgery. 2014;156(2):270–279. doi: 10.1016/j.surg.2014.04.055. [DOI] [PubMed] [Google Scholar]
- 148.Matsui Y, Watanabe J, Ikegawa M, Kamoto T, Ogawa O, Nishiyama H. Cancer-specific enhancement of cisplatin-induced cytotoxicity with triptolide through an interaction of inactivated glycogen synthase kinase-3beta with p53. Oncogene. 2008;27(33):4603–4614. doi: 10.1038/onc.2008.89. [DOI] [PubMed] [Google Scholar]
- 149.Liu Y, Xiao E, Yuan L, Li G. Triptolide Synergistically Enhances Antitumor Activity of Oxaliplatin in Colon Carcinoma In Vitro and In Vivo. DNA Cell Biol. 2014;33(7):418–425. doi: 10.1089/dna.2014.2356. [DOI] [PubMed] [Google Scholar]
- 150.Tang XY, Zhu YQ, Tao WH, Wei B, Lin XL. Synergistic effect of triptolide combined with 5-fluorouracil on colon carcinoma. Postgrad Med J. 2007;83(979):338–343. doi: 10.1136/pgmj.2006.055426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Qiao Z, He M, He MU, et al. Synergistic antitumor activity of gemcitabine combined with triptolide in pancreatic cancer cells. Oncol Lett. 2016;11(5):3527–3533. doi: 10.3892/ol.2016.4379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Pan Y, Zhang F, Zhao Y, et al. Berberine enhances chemosensitivity and induces apoptosis through Dose-orchestrated AMPK signaling in breast cancer. J Cancer. 2017;8(9):1679–1689. doi: 10.7150/jca.19106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhu T, Li LL, Xiao GF, et al. Berberine increases doxorubicin sensitivity by suppressing STAT3 in lung cancer. Am J Chin Med. 2015;43(7):1487–1502. doi: 10.1142/S0192415X15500846. [DOI] [PubMed] [Google Scholar]
- 154.Du J, Sun Y, Lu YY, et al. Berberine and evodiamine act synergistically against human breast cancer MCF-7 cells by inducing cell cycle arrest and apoptosis. Anticancer Res. 2017;37(11):6141–6151. doi: 10.21873/anticanres.12063. [DOI] [PubMed] [Google Scholar]
- 155.Ren K, Zhang W, Wu G, et al. Synergistic anti-cancer effects of galangin and berberine through apoptosis induction and proliferation inhibition in oesophageal carcinoma cells. Biomed Pharmacother. 2016;84:1748–1759. doi: 10.1016/j.biopha.2016.10.111. [DOI] [PubMed] [Google Scholar]
- 156.Wen C, Wu L, Fu L, Zhang X, Zhou H. Berberine enhances the anti-tumor activity of tamoxifen in drugsensitive MCF7 and drugresistant MCF7/TAM cells. Mol Med Rep. 2016;14(3):2250–2256. doi: 10.3892/mmr.2016.5490. [DOI] [PubMed] [Google Scholar]
- 157.Huang Y, Wang K, Gu C, et al. Berberine, a natural plant alkaloid, synergistically sensitizes human liver cancer cells to sorafenib. Oncol Rep. 2018;40(3):1525–1532. doi: 10.3892/or.2018.6552. [DOI] [PubMed] [Google Scholar]
- 158.Wang CJ, Wang C, Han J, et al. Effect of combined treatment with recombinant interleukin-2 and allicin on pancreatic cancer. Mol Biol Rep. 2013;40(12):6579–6585. doi: 10.1007/s11033-013-2766-1. [DOI] [PubMed] [Google Scholar]
- 159.Zou X, Liang J, Sun J, et al. Allicin sensitizes hepatocellular cancer cells to anti-tumor activity of 5-fluorouracil through ROS-mediated mitochondrial pathway. J Pharmacol Sci. 2016;131(4):233–240. doi: 10.1016/j.jphs.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 160.Dai B, Ma Y, Wang W, et al. Dihydroberberine exhibits synergistic effects with sunitinib on NSCLC NCI-H460 cells by repressing MAP kinase pathways and inflammatory mediators. J Cell Mol Med. 2017;21(10):2573–2585. doi: 10.1111/jcmm.13178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Liu Y, Bi T, Wang Z, et al. Oxymatrine synergistically enhances antitumor activity of oxaliplatin in colon carcinoma through PI3K/ Akt/mTOR pathway. Apoptosis. 2016;21(12):1398–1407. doi: 10.1007/s10495-016-1297-3. [DOI] [PubMed] [Google Scholar]
- 162.Song MQ, Zhu JS, Chen JL, et al. Synergistic effect of oxymatrine and angiogenesis inhibitor NM-3 on modulating apoptosis in human gastric cancer cells. World J Gastroenterol. 2007;13(12):1788–1793. doi: 10.3748/wjg.v13.i12.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Byun JM, Jeong DH, Lee DS, et al. Tetraarsenic oxide and cisplatin induce apoptotic synergism in cervical cancer. Oncol Rep. 2013;29(4):1540–1546. doi: 10.3892/or.2013.2243. [DOI] [PubMed] [Google Scholar]
- 164.Tang JH, Zhang HM, Zhang ZH, Zhang X-L. Effect of tetramethylpyrazine combined with cisplatin on VEGF, KLF4 and ADAMTS1 in Lewis lung cancer mice. Asian Pac J Trop Med. 2017;10(8):813–818. doi: 10.1016/j.apjtm.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 165.Castillo-Pichardo L, Dharmawardhane SF. Grape polyphenols inhibit Akt/mammalian target of rapamycin signaling and potentiate the effects of gefitinib in breast cancer. Nutr Cancer. 2012;64(7):1058–1069. doi: 10.1080/01635581.2012.716898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Stearns ME, Amatangelo MD, Varma D, Sell C, Goodyear SM. Combination therapy with epigallocatechin-3-gallate and doxorubicin in human prostate tumor modeling studies: inhibition of metastatic tumor growth in severe combined immunodeficiency mice. Am J Pathol. 2010;177(6):3169–3179. doi: 10.2353/ajpath.2010.100330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Liang G, Tang A, Lin X, et al. Green tea catechins augment the antitumor activity of doxorubicin in an in vivo mouse model for chemoresistant liver cancer. Int J Oncol. 2010;37(1):111–123. [PubMed] [Google Scholar]
- 168.Brodsky FM. Monoclonal antibodies as magic bullets. Pharm Res. 1988;05(1):1–9. doi: 10.1023/a:1015860525341. [DOI] [PubMed] [Google Scholar]
- 169.Ye BL, Ruan XJ, Zheng ZH, Cai HJ. Chitosan-coated doxorubicin nanoparticles drug delivery system inhibits cell growth of liver cancer via p53/PRC1 pathway. Biochem Biophys Res Commun. 2018;495(1):414–420. doi: 10.1016/j.bbrc.2017.10.156. [DOI] [PubMed] [Google Scholar]
- 170.Gao GH, Li Y, Lee DS. Environmental pH-sensitive polymeric micelles for cancer diagnosis and targeted therapy. J Control Release. 2013;169(3):180–184. doi: 10.1016/j.jconrel.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 171.Zhang X, Achazi K, Steinhilber D, Kratz F, Dernedde J, Haag R. A facile approach for dual-responsive prodrug nanogels based on den-dritic polyglycerols with minimal leaching. J Control Release. 2014;174:209–216. doi: 10.1016/j.jconrel.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 172.Zhang H, Wang K, Zhang P, He W, Song A, Luan Y. Redox-sensitive micelles assembled from amphiphilic mPEG-PCL-SS-DTX conjugates for the delivery of docetaxel. Colloids Surf B Biointerfaces. 2016;142:89–97. doi: 10.1016/j.colsurfb.2016.02.045. [DOI] [PubMed] [Google Scholar]
- 173.Sun YW, Xu J, Zhou J, Liu W-J. Targeted drugs for systemic therapy of lung cancer with brain metastases. Oncotarget. 2018;9(4):5459–5472. doi: 10.18632/oncotarget.23616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wick MR. Metastases of malignant neoplasms: Historical, biological, & clinical considerations. Semin Diagn Pathol. 2018;35(2):112–122. doi: 10.1053/j.semdp.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 175.Obinu A, Gavini E, Rassu G, Maestri M, Bonferoni MC, Giunchedi P. Lymph node metastases: importance of detection and treatment strategies. Expert Opin Drug Deliv. 2018;15(5):459–467. doi: 10.1080/17425247.2018.1446937. [DOI] [PubMed] [Google Scholar]
- 176.Hull LC, Farrell D, Grodzinski P. Highlights of recent developments and trends in cancer nanotechnology research – View from NCI Alliance for nanotechnology in cancer. Biotechnol Adv. 2014;32(4):666–678. doi: 10.1016/j.biotechadv.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 177.Yallapu MM, Khan S, Maher DM, et al. Anti-cancer activity of cur-cumin loaded nanoparticles in prostate cancer. Biomaterials. 2014;35(30):8635–8648. doi: 10.1016/j.biomaterials.2014.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Zhang Z, Qian H, Yang M, et al. Gambogic acid-loaded biomimetic nanoparticles in colorectal cancer treatment. Int J Nanomedicine. 2017;12:1593–1605. doi: 10.2147/IJN.S127256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zhang YQ, Shen Y, Liao MM, et al. Galactosylated chitosan triptolide nanoparticles for overcoming hepatocellular carcinoma: enhanced therapeutic efficacy, low toxicity, and validated network regulatory mechanisms. Nanomedicine. 2019;15(1):86–97. doi: 10.1016/j.nano.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 180.Jabr-Milane LS, van Vlerken LE, Yadav S, Amiji MM. Multifunctional nanocarriers to overcome tumor drug resistance. Cancer Treat Rev. 2008;34(7):592–602. doi: 10.1016/j.ctrv.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Narayanan S, Pavithran M, Viswanath A, et al. Sequentially releasing dual-drug-loaded PLGA-casein core/shell nanomedicine: design, synthesis, biocompatibility and pharmacokinetics. Acta Biomater. 2014;10(5):2112–2124. doi: 10.1016/j.actbio.2013.12.041. [DOI] [PubMed] [Google Scholar]
- 182.Gowda R, Kardos G, Sharma A, Singh S, Robertson GP. Nanoparticle-based celecoxib and plumbagin for the synergistic treatment of melanoma. Mol Cancer Ther. 2017;16(3):440–452. doi: 10.1158/1535-7163.MCT-16-0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Torchilin V. Tumor delivery of macromolecular drugs based on the EPR effect. Adv Drug Deliv Rev. 2011;63(3):131–135. doi: 10.1016/j.addr.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 184.Gaumet M, Vargas A, Gurny R, Delie F. Nanoparticles for drug delivery: the need for precision in reporting particle size parameters. Eur J Pharm Biopharm. 2008;69(1):1–9. doi: 10.1016/j.ejpb.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 185.Yu C, Zhou Q, Xiao F, et al. Enhancing doxorubicin delivery toward tumor by hydroxyethyl Starch-g-Polylactide partner nanocarriers. ACS Appl Mater Interfaces. 2017;9(12):10481–10493. doi: 10.1021/acsami.7b00048. [DOI] [PubMed] [Google Scholar]
- 186.Hafeez BB, Zhong W, Fischer JW, et al. Plumbagin, a medicinal plant (Plumbago zeylanica)-derived 1,4-naphthoquinone, inhibits growth and metastasis of human prostate cancer PC-3M-luciferase cells in an orthotopic xenograft mouse model. Mol Oncol. 2013;7(3):428–439. doi: 10.1016/j.molonc.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Li YC, He SM, He ZX, et al. Plumbagin induces apoptotic and autophagic cell death through inhibition of the PI3K/Akt/mTOR pathway in human non-small cell lung cancer cells. Cancer Lett. 2014;344(2):239–259. doi: 10.1016/j.canlet.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 188.Lee JH, Yeon JH, Kim H, et al. The natural anticancer agent plumbagin induces potent cytotoxicity in MCF-7 human breast cancer cells by inhibiting a PI-5 kinase for ROS generation. PLoS One. 2012;7(9):e45023. doi: 10.1371/journal.pone.0045023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Youm I, West MB, Li W, Du X, Ewert DL, Kopke RD. siRNA-loaded biodegradable nanocarriers for therapeutic MAPK1 silencing against cisplatin-induced ototoxicity. Int J Pharm. 2017;528(1–2):611–623. doi: 10.1016/j.ijpharm.2017.06.035. [DOI] [PubMed] [Google Scholar]
- 190.Kuhad A, Pilkhwal S, Sharma S, Tirkey N, Chopra K. Effect of curcumin on inflammation and oxidative stress in cisplatin-induced experimental nephrotoxicity. J Agric Food Chem. 2007;55(25):10150–10155. doi: 10.1021/jf0723965. [DOI] [PubMed] [Google Scholar]
- 191.Al Moundhri MS, Al-Salam S, Al Mahrouqee A, Beegam S, Ali BH. The effect of curcumin on oxaliplatin and cisplatin neurotoxicity in rats: Some behavioral, biochemical, and histopathological studies. J Med Toxicol. 2013;9(1):25–33. doi: 10.1007/s13181-012-0239-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Zhang J, Liu J, Xu X, Li L. Curcumin suppresses cisplatin resistance development partly via modulating extracellular vesicle-mediated transfer of MEG3 and miR-214 in ovarian cancer. Cancer Chemother Pharmacol. 2017;79(3):479–487. doi: 10.1007/s00280-017-3238-4. [DOI] [PubMed] [Google Scholar]
- 193.Hu Q, Sun W, Wang C, Gu Z. Recent advances of cocktail chemotherapy by combination drug delivery systems. Adv Drug Deliv Rev. 2016;98:19–34. doi: 10.1016/j.addr.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Cheng Y, Zhao P, Wu S, et al. Cisplatin and curcumin co-loaded nano-liposomes for the treatment of hepatocellular carcinoma. Int J Pharm. 2018;545(1–2):261–273. doi: 10.1016/j.ijpharm.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 195.Zhang YD. Nanobiotechnology. Science Press; Beijing, China: 2005. [Google Scholar]
- 196.Moghimi SM, Hunter AC, Murray JC. Longcirculating and target specific nanoparticles: theory to practice. Pharmacol Rev. 2001;53:283–318. [PubMed] [Google Scholar]
- 197.Pasut G, Veronese FM. State of the art in pegylation: the great versatility achieved after forty years of research. J Control Release. 2012;161(2):461–472. doi: 10.1016/j.jconrel.2011.10.037. [DOI] [PubMed] [Google Scholar]
- 198.Suk JS, Xu Q, Kim N, Hanes J, Ensign LM. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev. 2016;99:28–51. doi: 10.1016/j.addr.2015.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Fatma S, Talegaonkar S, Iqbal Z, et al. Novel flavonoid-based biodegradable nanoparticles for effective oral delivery of etoposide by P-glycoprotein modulation: an in vitro, ex vivo and in vivo investigations. Drug Deliv. 2016;23(2):500–511. doi: 10.3109/10717544.2014.923956. [DOI] [PubMed] [Google Scholar]
- 200.Schmid D, Jarvis GE, Fay F, et al. Nanoencapsulation of ABT-737 and camptothecin enhances their clinical potential through synergistic antitumor effects and reduction of systemic toxicity. Cell Death Dis. 2014;5(10):e1454. doi: 10.1038/cddis.2014.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Xu Y, Wang C, Ding Y, et al. Nanoparticles with optimal ratiometric co-delivery of docetaxel with gambogic acid for treatment of multidrug-resistant breast cancer. J Biomed Nanotechnol. 2016;12(9):1774–1781. doi: 10.1166/jbn.2016.2282. [DOI] [PubMed] [Google Scholar]
- 202.Jain AK, Thanki K, Jain S. Co-encapsulation of tamoxifen and quercetin in polymeric nanoparticles: implications on oral bioavailability, antitumor efficacy, and drug-induced toxicity. Mol Pharm. 2013;10(9):3459–3474. doi: 10.1021/mp400311j. [DOI] [PubMed] [Google Scholar]
- 203.Liu Q, Zhao D, Zhu X, et al. Coloaded nanoparticles of paclitaxel and Piperlongumine for enhancing synergistic antitumor activities and reducing toxicity. J Pharm Sci. 2017;106(10):3066–3075. doi: 10.1016/j.xphs.2017.05.027. [DOI] [PubMed] [Google Scholar]
- 204.Katiyar SS, Muntimadugu E, Rafeeqi TA, Domb AJ, Khan W. Co-delivery of rapamycin- and piperine-loaded polymeric nanoparticles for breast cancer treatment. Drug Deliv. 2016;23:2608–2616. doi: 10.3109/10717544.2015.1039667. [DOI] [PubMed] [Google Scholar]
- 205.Chen Y, Zheng XL, Fang DL, et al. Dual agent loaded PLGA nanoparticles enhanced antitumor activity in a multidrug-resistant breast tumor eenograft model. Int J Mol Sci. 2014;15(2):2761–2772. doi: 10.3390/ijms15022761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Hadinoto K, Sundaresan A, Cheow WS. Lipid-polymer hybrid nanoparticles as a new generation therapeutic delivery platform: a review. Eur J Pharm Biopharm. 2013;85(3 Pt A):427–443. doi: 10.1016/j.ejpb.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 207.Mandal B, Bhattacharjee H, Mittal N, et al. Core–shell-type lipid– polymer hybrid nanoparticles as a drug delivery platform. Nanomedicine. 2013;9(4):474–491. doi: 10.1016/j.nano.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 208.Li C, Ge X, Wang L. Construction and comparison of different nanocarriers for co-delivery of cisplatin and curcumin: a synergistic combination nanotherapy for cervical cancer. Biomed Pharmacother. 2017;86:628–636. doi: 10.1016/j.biopha.2016.12.042. [DOI] [PubMed] [Google Scholar]
- 209.Zhu B, Yu L, Yue Q. Co-delivery of vincristine and quercetin by nanocarriers for lymphoma combination chemotherapy. Biomed Pharmacother. 2017;91:287–294. doi: 10.1016/j.biopha.2017.02.112. [DOI] [PubMed] [Google Scholar]
- 210.Ruttala HB, Ko YT. Liposomal co-delivery of curcumin and albumin/ paclitaxel nanoparticle for enhanced synergistic antitumor efficacy. Colloids Surf B Biointerfaces. 2015;128:419–426. doi: 10.1016/j.colsurfb.2015.02.040. [DOI] [PubMed] [Google Scholar]
- 211.Mendes LP, Gaeti MP, de Ávila PH, et al. Multicompartimental nanoparticles for co-encapsulation and multimodal drug delivery to tumor cells and neovasculature. Pharm Res. 2014;31(5):1106–1119. doi: 10.1007/s11095-013-1234-x. [DOI] [PubMed] [Google Scholar]
- 212.Jiang H, Geng D, Liu H, Li Z, Cao J. Co-delivery of etoposide and curcumin by lipid nanoparticulate drug delivery system for the treatment of gastric tumors. Drug Deliv. 2016;23(9):3665–3673. doi: 10.1080/10717544.2016.1217954. [DOI] [PubMed] [Google Scholar]
- 213.Tang F, Li L, Chen D. Mesoporous silica nanoparticles: synthesis, bio-compatibility and drug delivery. Adv Mater. 2012;24(12):1504–1534. doi: 10.1002/adma.201104763. [DOI] [PubMed] [Google Scholar]
- 214.Zhang XG, Miao J, Dai YQ, Du YZ, Yuan H, Hu F-Q. Reversal activity of nanostructured lipid carriers loading cytotoxic drug in multi-drug resistant cancer cells. Int J Pharm. 2008;361(1–2):239–244. doi: 10.1016/j.ijpharm.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 215.Jia L, Li Z, Shen J, et al. Multifunctional mesoporous silica nanoparticles mediated co-delivery of paclitaxel and tetrandrine for overcoming multidrug resistance. Int J Pharm. 2015;489(1–2):318–330. doi: 10.1016/j.ijpharm.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 216.Jain AK, Thanki K, Jain S. Solidified self-nanoemulsifying formulation for oral delivery of combinatorial therapeutic regimen: Part II in vivo pharmacokinetics, antitumor efficacy and hepatotoxicity. Pharm Res. 2014;31(4):946–958. doi: 10.1007/s11095-013-1214-1. [DOI] [PubMed] [Google Scholar]
- 217.Pemovska T, Johnson E, Kontro M, et al. Axitinib effectively inhibits BCR-ABL1(T315I) with a distinct binding conformation. Nature. 2015;519(7541):102–105. doi: 10.1038/nature14119. [DOI] [PubMed] [Google Scholar]
- 218.Escudier B, Gore M. Axitinib for the management of metastatic renal cell carcinoma. Drugs R D. 2011;11(2):113–126. doi: 10.2165/11591240-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Pang X, Yi Z, Zhang J, et al. Celastrol suppresses angiogenesis-mediated tumor growth through inhibition of Akt/mammalian target of rapamycin pathway. Cancer Res. 2010;70(5):1951–1959. doi: 10.1158/0008-5472.CAN-09-3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Sethi G, Ahn KS, Pandey MK, Aggarwal BB. A novel triterpene, potentiates TNF-induced apoptosis and suppresses invasion of tumor cells by inhibiting NF-kappaB-regulated gene products and TAK1-mediated NF-kappaB activation. Blood. 2007;109:2727–2735. doi: 10.1182/blood-2006-10-050807. [DOI] [PubMed] [Google Scholar]
- 221.Choi JY, Ramasamy T, Kim SY, et al. PEGylated lipid bilayer-supported mesoporous silica nanoparticle composite for synergistic co-delivery of axitinib and celastrol in multi-targeted cancer therapy. Acta Biomater. 2016;39:94–105. doi: 10.1016/j.actbio.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 222.Ramasamy T, Ruttala HB, Chitrapriya N, et al. Engineering of cell microenvironment-responsive polypeptide nanovehicle co-encapsulating a synergistic combination of small molecules for effective chemotherapy in solid tumors. Acta Biomater. 2017;48:131–143. doi: 10.1016/j.actbio.2016.10.034. [DOI] [PubMed] [Google Scholar]
- 223.Zhang D, Xu Q, Wang N, et al. A complex micellar system co-delivering curcumin with doxorubicin against cardiotoxicity and tumor growth. Int J Nanomedicine. 2018;13:4549–4561. doi: 10.2147/IJN.S170067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Ma W, Guo Q, Li Y, Wang X, Wang J, Tu P. Co-assembly of doxorubicin and curcumin targeted micelles for synergistic delivery and improving anti-tumor efficacy. Eur J Pharm Biopharm. 2017;112:209–223. doi: 10.1016/j.ejpb.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 225.Gu Y, Li J, Li Y, et al. Nanomicelles loaded with doxorubicin and curcumin for alleviating multidrug resistance in lung cancer. Int J Nanomedicine. 2016;11:5757–5770. doi: 10.2147/IJN.S118568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Wang J, Ma W, Tu P. Synergistically improved anti-tumor efficacy by co-delivery doxorubicin and curcumin polymeric micelles. Macromol Biosci. 2015;15(9):1252–1261. doi: 10.1002/mabi.201500043. [DOI] [PubMed] [Google Scholar]
- 227.Shapira A, Livney YD, Broxterman HJ, Assaraf YG. Nanomedicine for targeted cancer therapy: towards the overcoming of drug resistance. Drug Resist Updat. 2011;14(3):150–163. doi: 10.1016/j.drup.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 228.Sreekanth CN, Bava SV, Sreekumar E, Anto RJ. Molecular evidences for the chemosensitizing efficacy of liposomal curcumin in paclitaxel chemotherapy in mouse models of cervical cancer. Oncogene. 2011;30(28):3139–3152. doi: 10.1038/onc.2011.23. [DOI] [PubMed] [Google Scholar]
- 229.Abouzeid AH, Patel NR, Torchilin VP. Polyethylene glycol-phosphatidylethanolamine (PEG-PE)/vitamin E micelles for co-delivery of paclitaxel and curcumin to overcome multi-drug resistance in ovarian cancer. Int J Pharm. 2014;464(1–2):178–184. doi: 10.1016/j.ijpharm.2014.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Meng L, Xia X, Yang Y, et al. Co-encapsulation of paclitaxel and baicalein in nanoemulsions to overcome multidrug resistance via oxidative stress augmentation and P-glycoprotein inhibition. Int J Pharm. 2016;513(1–2):8–16. doi: 10.1016/j.ijpharm.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 231.Ishii K, Tanaka S, Kagami K, et al. Effects of naturally occurring polymethyoxyflavonoids on cell growth, P-glycoprotein function, cell cycle, and apoptosis of daunorubicin-resistant T lymphoblastoid leukemia cells. Cancer Invest. 2010;28(3):220–229. doi: 10.3109/07357900902744486. [DOI] [PubMed] [Google Scholar]
- 232.Letchford K, Burt H. A review of the formation and classification of amphiphilic block copolymer nanoparticulate structures: micelles, nanospheres, nanocapsules and polymersomes. Eur J Pharm Biopharm. 2007;65(3):259–269. doi: 10.1016/j.ejpb.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 233.Singh R, Lillard JW. Nanoparticle-based targeted drug delivery. Exp Mol Pathol. 2009;86(3):215–223. doi: 10.1016/j.yexmp.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Alemi A, Zavar Reza J, Haghiralsadat F, et al. Paclitaxel and curcumin coadministration in novel cationic PEGylated niosomal formulations exhibit enhanced synergistic antitumor efficacy. J Nanobiotechnol. 2018;16(1):28. doi: 10.1186/s12951-018-0351-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Han C, Zhang C, Ma T, et al. Hypericin-functionalized graphene oxide for enhanced mitochondria-targeting and synergistic anticancer effect. Acta Biomater. 2018;77:268–281. doi: 10.1016/j.actbio.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 236.Pereira S, Lee J, Rubio N, et al. Cationic Liposome- multi-walled carbon nanotubes hybrids for dual siPLK1 and doxorubicin delivery in vitro. Pharm Res. 2015;32(10):3293–3308. doi: 10.1007/s11095-015-1707-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Martincic M, Tobias G. Filled carbon nanotubes in biomedical imaging and drug delivery. Expert Opin Drug Deliv. 2015;12(4):563–581. doi: 10.1517/17425247.2015.971751. [DOI] [PubMed] [Google Scholar]
- 238.Zhu F, Tan G, Jiang Y, Yu Z, Ren F. Rational design of multi-stimuli-responsive gold nanorod–curcumin conjugates for chemo-photothermal synergistic cancer therapy. Biomater Sci. 2018;6(11):2905–2917. doi: 10.1039/c8bm00691a. [DOI] [PubMed] [Google Scholar]
- 239.Lockhart JN, Stevens DM, Beezer DB, Kravitz A, Harth E. Dual drug delivery of tamoxifen and quercetin: regulated metabolism for anticancer treatment with nanosponges. J Control Release. 2015;220(Pt B):751–757. doi: 10.1016/j.jconrel.2015.08.052. [DOI] [PubMed] [Google Scholar]
- 240.Liu B, Han L, Liu J, Han S, Chen Z, Jiang L. Co-delivery of paclitaxel and TOS-cisplatin via TAT-targeted solid lipid nanoparticles with synergistic antitumor activity against cervical cancer. Int J Nanomedicine. 2017;12:955–968. doi: 10.2147/IJN.S115136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.He C, Lu K, Liu D, Lin W. Nanoscale Metal–Organic frameworks for the co-delivery of cisplatin and pooled siRNAs to enhance therapeutic efficacy in drug-resistant ovarian cancer cells. J Am Chem Soc. 2014;136(14):5181–5184. doi: 10.1021/ja4098862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Yao X, Chen L, Chen X, et al. pH-responsive metallo-supramolecular nanogel for synergistic chemo-photodynamic therapy. Acta Biomater. 2015;25:162–171. doi: 10.1016/j.actbio.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 243.Gaspar VM, Moreira AF, Costa EC, et al. Gas-generating TPGS-PLGA microspheres loaded with nanoparticles (NIMPS) for co-delivery of minicircle DNA and anti-tumoral drugs. Colloids Surf B Biointerfaces. 2015;134:287–294. doi: 10.1016/j.colsurfb.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 244.Wilhelm S, Tavares AJ, Dai Q, et al. Analysis of nanoparticle delivery to tumours. Nat Rev Mat. 2016;1(5) [Google Scholar]
- 245.Albanese A, Tang PS, Chan WCW. The effect of nanoparticle size, shape, and surface chemistry on biological systems. Annu Rev Biomed Eng. 2012;14(1):1–16. doi: 10.1146/annurev-bioeng-071811-150124. [DOI] [PubMed] [Google Scholar]
- 246.Zhang XQ, Xu X, Bertrand N, Pridgen E, Swami A, Farokhzad OC. Interactions of nanomaterials and biological systems: implications to personalized nanomedicine. Adv Drug Deliv Rev. 2012;64(13):1363–1384. doi: 10.1016/j.addr.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Bertrand N, Wu J, Xu X, Kamaly N, Farokhzad OC. Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Adv Drug Deliv Rev. 2014;66:2–25. doi: 10.1016/j.addr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Gabizon A, Horowitz AT, Goren D, Tzemach D, Shmeeda H, Zalipsky S. In vivo fate of folate-targeted polyethylene-glycol liposomes in tumor-bearing mice. Clin Cancer Res. 2003;9:6551–6559. [PubMed] [Google Scholar]
- 249.Calzolari A, Oliviero I, Deaglio S, et al. Transferrin receptor 2 is frequently expressed in human cancer cell lines. Blood Cells Mol Dis. 2007;39(1):82–91. doi: 10.1016/j.bcmd.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 250.Cui T, Zhang S, Sun H. Co-delivery of doxorubicin and pH-sensitive curcumin prodrug by transferrin-targeted nanoparticles for breast cancer treatment. Oncol Rep. 2017;37(2):1253–1260. doi: 10.3892/or.2017.5345. [DOI] [PubMed] [Google Scholar]
- 251.Low PS, Antony AC. Folate receptor-targeted drugs for cancer and inflammatory diseases. Adv Drug Deliv Rev. 2004;56(8):1055–1058. doi: 10.1016/j.addr.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 252.Wang Y, Wang Y, Xiang J, Yao K. Target-specific cellular uptake of taxol-loaded heparin-PEG-folate nanoparticles. Biomacromolecules. 2010;11(12):3531–3538. doi: 10.1021/bm101013s. [DOI] [PubMed] [Google Scholar]
- 253.Wang W, Xi M, Duan X, Wang Y, Kong F. Delivery of baicalein and paclitaxel using self-assembled nanoparticles: synergistic antitumor effect in vitro and in vivo. Int J Nanomedicine. 2015;10:3737–3750. doi: 10.2147/IJN.S80297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Firestone RA. Low-density lipoprotein as a vehicle for targeting antitumor compounds to cancer cells. Bioconjug Chem. 1994;5(2):105–113. doi: 10.1021/bc00026a002. [DOI] [PubMed] [Google Scholar]
- 255.Sudhof T, Goldstein J, Brown M, Russell D. The LDL receptor gene: a mosaic of exons shared with different proteins. Science. 1985;228(4701):815–822. doi: 10.1126/science.2988123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Zhu WJ, Yang SD, Qu CX, et al. Low-density lipoprotein-coupled micelles with reduction and pH dual sensitivity for intelligent co-delivery of paclitaxel and siRNA to breast tumor. Int J Nanomedicine. 2017;12:3375–3393. doi: 10.2147/IJN.S126310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Yang SD, Zhu WJ, Zhu QL, et al. Binary-copolymer system base on low-density lipoprotein-coupled N-succinyl chitosan lipoic acid micelles for co-delivery MDR1 siRNA and paclitaxel, enhances anti-tumor effects via reducing drug. J Biomed Mater Res. 2017;105(5):1114–1125. doi: 10.1002/jbm.b.33636. [DOI] [PubMed] [Google Scholar]
- 258.Kebebe D, Liu Y, Wu Y, Vilakhamxay M, Liu Z, Li J. Tumor-targeting delivery of herb-based drugs with cell-penetrating/tumor-targeting peptide-modified nanocarriers. Int J Nanomedicine. 2018;13:1425–1442. doi: 10.2147/IJN.S156616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Narayanan S, Mony U, Vijaykumar DK, Koyakutty M, Paul-Prasanth B, Menon D. Sequential release of epigallocatechin gallate and paclitaxel from PLGA-casein core/shell nanoparticles sensitizes drug-resistant breast cancer cells. Nanomedicine. 2015;11(6):1399–1406. doi: 10.1016/j.nano.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 260.Yan J, Wang Y, Jia Y, et al. Co-delivery of docetaxel and curcumin pro-drug via dual-targeted nanoparticles with synergistic antitumor activity against prostate cancer. Biomed Pharmacother. 2017;88:374–383. doi: 10.1016/j.biopha.2016.12.138. [DOI] [PubMed] [Google Scholar]
- 261.Wang C, Su L, Wu C, Wu J, Zhu C, Yuan G. RGD peptide targeted lipid-coated nanoparticles for combinatorial delivery of sorafenib and quercetin against hepatocellular carcinoma. Drug Dev Ind Pharm. 2016;42(12):1938–1944. doi: 10.1080/03639045.2016.1185435. [DOI] [PubMed] [Google Scholar]
- 262.Zhao R, Li T, Zheng G, Jiang K, Fan L, Shao J. Simultaneous inhibition of growth and metastasis of hepatocellular carcinoma by co-delivery of ursolic acid and sorafenib using lactobionic acid modified and pH-sensitive chitosan-conjugated mesoporous silica nanocomplex. Biomaterials. 2017;143:1–16. doi: 10.1016/j.biomaterials.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 263.Shen Z, Wei W, Tanaka H, et al. A galactosamine-mediated drug delivery carrier for targeted liver cancer therapy. Pharmacol Res. 2011;64(4):410–419. doi: 10.1016/j.phrs.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 264.Yan T, Li D, Li J, et al. Effective co-delivery of doxorubicin and curcumin using a glycyrrhetinic acid-modified chitosan-cystamine-poly(ε-caprolactone) copolymer micelle for combination cancer chemotherapy. Colloids Surf Biointerfaces. 2016;145:526–538. doi: 10.1016/j.colsurfb.2016.05.070. [DOI] [PubMed] [Google Scholar]
- 265.Tsuji H, Osaka S, Kiwada H. Targeting of liposomes surface-modified with glycyrrhizin to the liver. I. Preparation and biological disoposition. Chem Pharm Bull. 1991;39(4):1004–1008. doi: 10.1248/cpb.39.1004. [DOI] [PubMed] [Google Scholar]
- 266.Ishida S, Sakiya Y, Ichikawa T, Taira Z. Uptake of glycyrrhizin by isolated rat hepatocytes. Biol Pharm Bull. 1993;16(3):293–297. doi: 10.1248/bpb.16.293. [DOI] [PubMed] [Google Scholar]
- 267.Negishi M, Irie A, Nagata N, Ichikawa A. Specific binding of glycyrrhetinic acid to the rat liver membrane. Biochim Biophys Acta. 1991;1066(1):77–82. doi: 10.1016/0005-2736(91)90253-5. [DOI] [PubMed] [Google Scholar]
- 268.Lin A, Liu Y, Huang Y, et al. Glycyrrhizin surface-modified chitosan nanoparticles for hepatocyte-targeted delivery. Int J Pharm. 2008;359(1–2):247–253. doi: 10.1016/j.ijpharm.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 269.Lee SJ, Zheng NY, Clavijo M, Nussenzweig MC. Normal host defense during systemic candidiasis in mannose receptor-deficient mice. Infect Immun. 2003;71(1):437–445. doi: 10.1128/IAI.71.1.437-445.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Hirata K, Maruyama T, Watanabe H, et al. Genetically engineered mannosylated-human serum albumin as a versatile carrier for liver-selective therapeutics. J Control Release. 2010;145(1):9–16. doi: 10.1016/j.jconrel.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 271.Zhang J, Yu C, Jiang G. Synthesis of cholic-acid-carrying polymer and in-vitro evaluation of hepatoma-targeting nanoparticles decorated with the polymer. J Biomater Sci Polym Ed. 2016;27(9):865–879. doi: 10.1080/09205063.2016.1168764. [DOI] [PubMed] [Google Scholar]
- 272.Elgohary MM, Helmy MW, Abdelfattah E-ZA, et al. Targeting sialic acid residues on lung cancer cells by inhalable boronic acid-decorated albumin nanocomposites for combined chemo/herbal therapy. J Control Release. 2018;285:230–243. doi: 10.1016/j.jconrel.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 273.Xia Y, Xu T, Wang C, et al. Novel functionalized nanoparticles for tumor-targeting co-delivery of doxorubicin and siRNA to enhance cancer therapy. Int J Nanomedicine. 2018;13:143–159. doi: 10.2147/IJN.S148960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Wan L, Jiao J, Cui Y, et al. Hyaluronic acid modified mesoporous carbon nanoparticles for targeted drug delivery to CD44-overexpressing cancer cells. Nanotechnology. 2016;27(13):135102. doi: 10.1088/0957-4484/27/13/135102. [DOI] [PubMed] [Google Scholar]
- 275.Feng Q, Yu MZ, Wang JC, et al. Synergistic inhibition of breast cancer by co-delivery of VEGF siRNA and paclitaxel via vapreotide-modified core–shell nanoparticles. Biomaterials. 2014;35(18):5028–5038. doi: 10.1016/j.biomaterials.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 276.Chen J, Li S, Shen Q. Folic acid and cell-penetrating peptide conjugated PLGA–PEG bifunctional nanoparticles for vincristine sulfate delivery. Eur J Pharm Sci. 2012;47(2):430–443. doi: 10.1016/j.ejps.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 277.Gao Z, You C, Wu H, Wang M, Zhang X, Sun B. FA and cRGD dual modified lipid-polymer nanoparticles encapsulating polyaniline and cisplatin for highly effective chemo-photothermal combination therapy. J Biomater Sci Polym Ed. 2018;29(4):397–411. doi: 10.1080/09205063.2017.1421348. [DOI] [PubMed] [Google Scholar]
- 278.Zhang J, Li J, Shi Z, et al. pH-sensitive polymeric nanoparticles for co-delivery of doxorubicin and curcumin to treat cancer via enhanced pro-apoptotic and anti-angiogenic activities. Acta Biomater. 2017;58:349–364. doi: 10.1016/j.actbio.2017.04.029. [DOI] [PubMed] [Google Scholar]
- 279.Danafar H, Sharafi A, Kheiri S, Kheiri Manjili H. Co-delivery of sulforaphane and curcumin with pegylated iron Oxide-Gold core shell nanoparticles for delivery to breast cancer cell line. Iran J Pharm Res. 2018;17(2):480–494. [PMC free article] [PubMed] [Google Scholar]
- 280.Chang JE, Cho HJ, Yi E, Kim DD, Jheon S. Hypocrellin B and paclitaxel-encapsulated hyaluronic acid-ceramide nanoparticles for targeted photodynamic therapy in lung cancer. J Photochem Photobiol B. 2016;158:113–121. doi: 10.1016/j.jphotobiol.2016.02.035. [DOI] [PubMed] [Google Scholar]
- 281.Yin Y, Hu Q, Xu C, et al. Co-delivery of doxorubicin and interferon-γ by thermosensitive nanoparticles for cancer immunochemotherapy. Mol Pharm. 2018;15(9):4161–4172. doi: 10.1021/acs.molpharmaceut.8b00564. [DOI] [PubMed] [Google Scholar]
- 282.Yin T, Wang L, Yin L, Zhou J, Huo M. Co-delivery of hydrophobic paclitaxel and hydrophilic AURKA specific siRNA by redox-sensitive micelles for effective treatment of breast cancer. Biomaterials. 2015;61:10–25. doi: 10.1016/j.biomaterials.2015.05.022. [DOI] [PubMed] [Google Scholar]