Abstract
Background:
The diagnosis of myocardial infarction (MI) after non-cardiac surgery has traditionally relied on using relatively insensitive contemporary cardiac troponin (cTn) assays. We hypothesized that using a recently introduced novel high-sensitivity cTnT (hscTnT) assay would increase the detection rate of perioperative MI.
Methods:
In this ancillary study of the Vitamins in Nitrous Oxide trial, readjudicated incidence rates of myocardial injury (new isolated cTn elevation) and MI were compared when diagnosed by contemporary cTnI versus hscTnT. We probed various relative (e.g., >50%) or absolute (e.g., + 5 ng/L) hscTnT change metrics. Inclusion criteria for this ancillary study were the presence of a baseline and at least one postoperative hscTnT value.
Results:
Among 605 patients, 70 patients (12%) had ECG changes consistent with myocardial ischemia; 82 patients (14%) had myocardial injury diagnosed by contemporary cTnI, 31 (5.1%) of which had an adjudicated MI. After readjudication, 67 patients (11%) were diagnosed with MI when using hscTnT, a 2-fold increase. Incidence rates of postoperative myocardial injury ranged from 12% (n=73) to 65% (n=393) depending on the hscTnT metric used. Incidence rates of MI using various hscTnT change metrics and the presence of ischemic ECG changes, but without event adjudication, ranged from 3.6% (n=22) to 12% (n=74), a >3-fold difference. New postoperative hscTnT elevation, either by absolute or relative hscTnT change metric was associated with an up to 5-fold increase in 6-month mortality.
Conclusions:
The use of hscTnT compared to contemporary cTnI increases the detection rate of perioperative MI by a factor of two. Using different absolute or relative hscTnT change metrics may lead to under- or over-diagnosis of perioperative MI.
Acute myocardial infarction (MI) is diagnosed according to the international consensus document “The Third Universal Definition of Myocardial Infarction”.1 To objectively diagnose acute MI, at minimum two of three elements need to be present: (1) clinical symptoms consistent with myocardial ischemia, such as chest pain; (2) ECG changes consistent with myocardial ischemia, such as ST-segment elevation or depression; (3) a new rise (or fall) pattern of a cardiac biomarker, preferably cardiac troponin (cTn). Because myocardial ischemia after non-cardiac surgery is often silent, the diagnosis of acute perioperative MI relies greatly on the detection of new cardiac biomarker elevation.2–4
Until recently, cTn assays were relatively insensitive from an analytical perspective and preoperative cTn values were mostly undetectable, thus making it impossible to measure actual cTn change values. However, the recent development and introduction of high-sensitivity cTn (hscTn) assays changed this: several studies have now shown that hscTn values can be measured prior to non-cardiac surgery. 5–7
We thus hypothesized that the increased sensitivity of novel hscTn assays would increase the detection of postoperative cTn elevation. It is however unknown, if this would also translate into an increased detection rate of acute postoperative MI.
To answer these questions, we performed a secondary analysis of data obtained in the VINO trial.8 In the current study, we used adjudicated event rates of myocardial injury and MI as objective standard, which were diagnosed by a contemporary non-high-sensitivity cTnI assay according to the Third Universal Definition of MI. We then compared these event rates to event rates that were obtained after re-adjudicating events using a novel high-sensitivity cTnT (hscTnT) assay.
A secondary aim of this investigation was to compare various absolute and relative hscTnT change metrics, i.e. comparing the difference between preoperative and peak postoperative hscTnT. 9,10 The principal reason for investigating hscTn change metrics is their successful application in rapid rule in/rule out MI-protocols in emergency department setting, where the introduction of hscTn has profoundly changed how acute MI is diagnosed in patients presenting with acute chest pain.11–15
Methods
Study Design and Population
Patients were originally enrolled in the Vitamins in Nitrous Oxide (VINO) Trial (Clinicaltrials.gov number NCT00655980).8 In brief, the VINO trial was a double-blind, randomized, placebo-controlled, single-center trial that evaluated if patients carrying the MTHFR C677T or A1298C gene variant had higher risk for perioperative myocardial injury and infarction after nitrous oxide anesthesia for major non-cardiac surgery, and whether this risk could be mitigated by B-vitamins. The original trial was negative for any effect on postoperative myocardial injury and infarction. The VINO trial enrolled 625 patients, with elevated cardiac risk, scheduled for major non-cardiac surgery. For this ancillary study, 605 patients with baseline high-sensitivity cardiac troponin T (hscTnT) and at least one postoperative hscTnT measurement were included in the analysis. This study was approved by the institutional review board at Washington University in St. Louis.
Measurements
Biomarker Assays
HscTnT measurements were collected at pre-defined time points: baseline (within 2 hours before surgery), end of surgery (within 30 minutes after arrival in the post-anesthesia care unit), postoperative days 1, 2, and 3, or until discharge. HscTnT was processed on the Roche Elecsys 2010 analyzer (limit of detection: 5.0 ng/L; 99th percentile: men: hscTnT ≥ 14.5ng/L; women: hscTnT ≥10ng/L; 10% coefficient of variation (CV) at 13 ng/L).16,17 All hscTnT cutoffs used sex-specific reference values for the 99th percentile. The preoperative value was the baseline value, and the postoperative hscTnT peak was defined as the highest postoperative hscTnT concentration on any follow-up day. Cardiac troponin I (cTnI) concentrations were also collected over the same time points and were measured on a contemporary non-high-sensitivity assay (Siemens Dimension RxL analyzer; limit of detection: 0.04 μg/L (=40 ng/L); 99th percentile: 0.07μg/L; 10% CV at 0.14 μg/L). The contemporary cTnI values were used for clinical care.
Electrocardiograms
12-lead electrocardiograms (ECGs) were collected at the same time points to correlate with troponin concentrations at baseline, end of surgery, postoperative days 1, 2, and 3, or until discharge. The ECGs were read and analyzed by two investigators blinded to biomarker results for signs of myocardial ischemia: Q-waves, ST-elevation ≥ 0.2 mV, ST-depression or T-wave inversion ≥ 0.1 mV in at least two contiguous leads. Patients with at least one positive ECG finding, at any time in the 72 hours after surgery, were considered positive for myocardial ischemia. Ambiguous cases were resolved by consensus opinion that included the principal investigator.
Outcomes
The primary outcome of this study was acute myocardial infarction within the first three postoperative days, diagnosed according to the Third Universal Definition of MI. The diagnosis required a new postoperative cTn elevation > 99th percentile plus simultaneous ischemic changes on a 12-lead ECG and/or clinical symptoms consistent with acute myocardial ischemia, such as chest pain.18 New postoperative cTn elevation was either determined by a contemporary cTnI assay or hscTnT. If baseline hscTnT was already elevated >99th percentile, a >50% hscTnT rise was used). All patients who developed new postoperative hscTnT elevation were readjudicated for missed cardiac events. MI was also diagnosed when cardiology consultants diagnosed acute MI, and/or by cardiac imaging or coronary angiography. Readjudication included a review of patient records, charts, clinical data to identify missed cardiac events.
Myocardial injury was diagnosed when an isolated new cTn elevation above the 99th% URL (either by cTnI or hscTnT) without evidence of myocardial ischemia on ECG or echo was present. Mortality was assessed at 6 months, 1 year and 3 years from date of surgery.
Statistical Methods
Adjudicated incidence rates of perioperative MI and myocardial injury were compared between events diagnosed using the contemporary cTnI assay and hscTnT.19 These incidence rates were then compared to unadjudicated incidence rates obtained using 11 absolute and relative hscTnT change metrics to determine if and by how much incidence rates would differ if only made with biomarker and ECG data (but without clinical adjudication), as most postoperative events of myocardial ischemia are silent.
The following absolute and relative hscTnT change metrics were used: (1) postoperative hscTnT >99th percentile; (2) postoperative hscTnT >99th percentile if baseline <99th percentile; (3) postoperative hscTnT increase >50% from baseline; (4) postoperative hscTnT increase >50% from baseline and one postoperative value >99th percentile; (5) postoperative hscTnT increase >100% from baseline; (6) postoperative hscTnT increase >100% from baseline and one postoperative value >99th percentile; (7) postoperative hscTnT increase by >100% if baseline <99th percentile, or increased by >50% if baseline hscTnT >99th percentile; (8) postoperative hscTnT increase > 5 ng/L from baseline; (9) postoperative hscTnT increase > 5 ng/L from baseline and one postoperative value >99th percentile; (10) postoperative hscTnT increase > 10 ng/L from baseline; (11) postoperative increase > 10 ng/L from baseline hscTnT and one postoperative value >99th percentile.
Survival analysis was performed for each hscTnT metric at six months, one year, and three years. For all hscTnT metrics and the contemporary cTnI definition for diagnosis of MI, we used Kaplan-Meier curves and log-rank tests to compare patients who had a MI and patients who did not have a MI. A Cox proportional hazards model was used to calculate the hazard ratios for each definition of myocardial injury and infarction by cTnI and hscTnT change metrics. The Cox proportional hazards models were then adjusted for potential confounders of age, sex, race, history of chronic kidney disease, and coronary artery disease (CAD). History of CAD or its equivalent (history of PCI or CABG) were combined into one dichotomous variable to reduce collinearity in the regression analyses. All Cox models were tested using Schoenfeld residuals to assure proportional hazard assumptions were not violated. Statistical methods were performed using Stata Version 14.0 (2015). All tests were two-sided; results were not adjusted for multiple comparisons and a p-value <0.05 was considered statistically significant.
Results
Demographics
The final study population included 605 patients with both baseline and at least one postoperative hscTnT value. Surgical procedures included predominantly vascular and orthopedic surgery.8 Table 1 shows a summary of patient characteristics for the study population based on the clinical diagnosis of acute MI using the contemporary non-high-sensitivity cTnI assay. At baseline, 290/605 (48%) study participants had elevated hscTnT above the sex-specific 99th percentile.
Table 1:
Characteristics of the Study Population and Patients with Acute MI diagnosed by Contemporary cTnI
| Demographics | No Myocardial Infarction (n=574) | Myocardial Infarction (n=31) | Total (n=605) |
|---|---|---|---|
| Mean Age (yrs) ±SD | 65 ±11 | 69 ±9 | 65 ±11 |
| Female sex - no. (%) | 218 (38%) | 10 (32%) | 228 (38%) |
| Race- no.(%) | |||
| White | 460 (80%) | 27 (87%) | 487 (81%) |
| Black | 112 (20%) | 4 (13%) | 116 (19%) |
| Other | 2 (0.34%) | 0 (0%) | 2 (0.32%) |
| Smoking - no. (%) | 428 (75%) | 23 (74%) | 451 (75%) |
| Diabetes - no. (%) | 201 (35%) | 13 (43%) | 214 (36%) |
| Hypertension - no. (%) | 461 (80%) | 26 (84%) | 487 (81%) |
| Hypercholesterolemia - no. (%) | 374 (65%) | 14 (48%) | 388 (64%) |
| Heart Failure - no. (%) | 63 (11%) | 6 (19%) | 69 (11%) |
| Chronic Kidney Disease - no. (%) | 59 (10%) | 7 (23%) | 66 (11%) |
| Coronary Artery Disease - no. (%) | 315 (55%) | 25 (81%) | 340 (56%) |
| History of CABG - no. (%) | 92 (16%) | 11 (35%) | 103 (17%) |
| History of PCI - no. (%) | 185 (33%) | 16 (53%) | 201 (34%) |
| History of Myocardial Infarction - no. (%) | 151 (26%) | 13 (42%) | 164 (27%) |
Diagnostic Criteria for MI by High Sensitivity Cardiac Troponin T
In the parent trial, and used as comparator group, 82/605 (14%) patients had myocardial injury diagnosed with a contemporary non-high-sensitivity cTnI assay within the first 3 days after surgery, 31 (5.1%) of whom had an adjudicated MI. 70 patients (12%) had ECG changes consistent with myocardial ischemia.
After readjudication of all patients who developed a new hscTnT elevation above the 99th percentile or a >50% increase compared to baseline if the baseline was already >99th percentile (using the high-sensitivity cardiac troponin T assay), 67 patients (11%) were diagnosed with MI, a >2-fold increase in call rate (Table 2). Among the 67 patients, one patient had a ST-elevation MI (1.5%), 57 patients a NSTEMI (85%), and 9 had unspecific ECG changes (13%); 20 patients (30%) had clinical symptoms consistent with myocardial ischemia and 47 had no symptoms (70%); 8 patients (12%) were referred to coronary angiography and 4 (6%) received a PCI and stent.
Table 2.
Incidence Rates of Myocardial Injury and Infarction based on Different Absolute and Relative hscTnT Change Metrics
| Cardiac Troponin Change Metrics | Myocardial Injury | MI |
|---|---|---|
|
Contemporary cTnI comparison group (new cTnI elevation >99th percentile; adjudicated MIs) |
82 (13.6%, 95% CI: 11.1; 16.5) | 31 (5.1%; 95% CI: 3.6; 7.2) |
|
Re-adjudicated cardiac events using hscTnT (new hscTnT elevation >99th percentile, or >50% increase from baseline) |
134 (22.2%, 95% CI: 19.0; 25.6) | 67 (11.1%; 95% CI: 8.8; 13.8) |
| Unadjudicated cardiac event rates based on hscTnT and ECG changes | ||
| Post-op hscTnT >99th%tile | 390 (64.4%; 95% CI: 60.6; 68.2) | 74 (12.2%; 95% CI: 9.9; 15.1) |
| Post-op hscTnT >99th%tile if baseline <99th %tile | 107 (17.7%; 95% CI: 14.9; 20.9) | 22 (3.6%; 95% CI:2.4; 5.5) |
| Post-op hscTnT increase >50% from baseline | 173 (28.6%; 95% CI: 25.1; 32.3) | 52 (8.6%; 95% CI: 6.6; 11.1) |
| Post-op hscTnT increase >50% from baseline and one Post-op value >99th %tile | 138 (22.8%; 95% CI: 19.6; 26.3) | 51 (8.4%; 95% CI: 6.5; 10.9) |
| Post-op hscTnT increase >100% from baseline | 86 (14.2%; 95% CI: 11.7; 17.2) | 40 (6.6%; 95% CI: 4.9; 8.9) |
| Post-op hscTnT increase >100% from baseline and one Post-op value >99th%tile | 73 (12.1%; 95% CI: 9.7; 14.9) | 39 (6.4%; 95% CI: 4.7; 8.7) |
| Post-op hscTnT increase by >100% if baseline <99th%, or increased by >50% if baseline hscTnT >99th% | 151 (25.0%; 95% CI: 21.7; 28.6) | 52 (8.6%; 95% CI: 6.6; 11.1) |
| Post-op increase > 5 ng/L from baseline hscTnT | 206 (34.1%; 95% CI: 30.4; 37.9) | 35 (5.9%; 95% CI: 4.2; 8.0) |
| Post-op increase > 5 ng/L from baseline hscTnT and one Post-op value >99th%tile | 193 (31.9%; 95% CI: 28.3; 35.7) | 35 (5.9%; 95% CI: 4.2; 8.0) |
| Post-op increase > 10 ng/L from baseline hscTnT | 103 (17.0%; 95% CI: 14.2; 20.2) | 31 (5.1%; 95% CI: 3.6; 7.2) |
| Post-op increase > 10 ng/L from baseline hscTnT and one Post-op value >99th%tile | 103 (17.0%; 95% CI: 14.2; 20.2) | 31 (5.1%; 95% CI: 3.6; 7.2) |
Based on the absolute or relative hscTnT change metric used, which compared the change between baseline and peak hscTnT, the incidence rate of myocardial injury (isolated hscTnT elevation without evidence of myocardial ischemia) ranged from 12% (n=73) to 65% (n=393), a >5-fold difference (Table 2). Nearly all hscTnT change metrics captured more myocardial injury events than with the contemporary non-high-sensitivity cTnI assay.
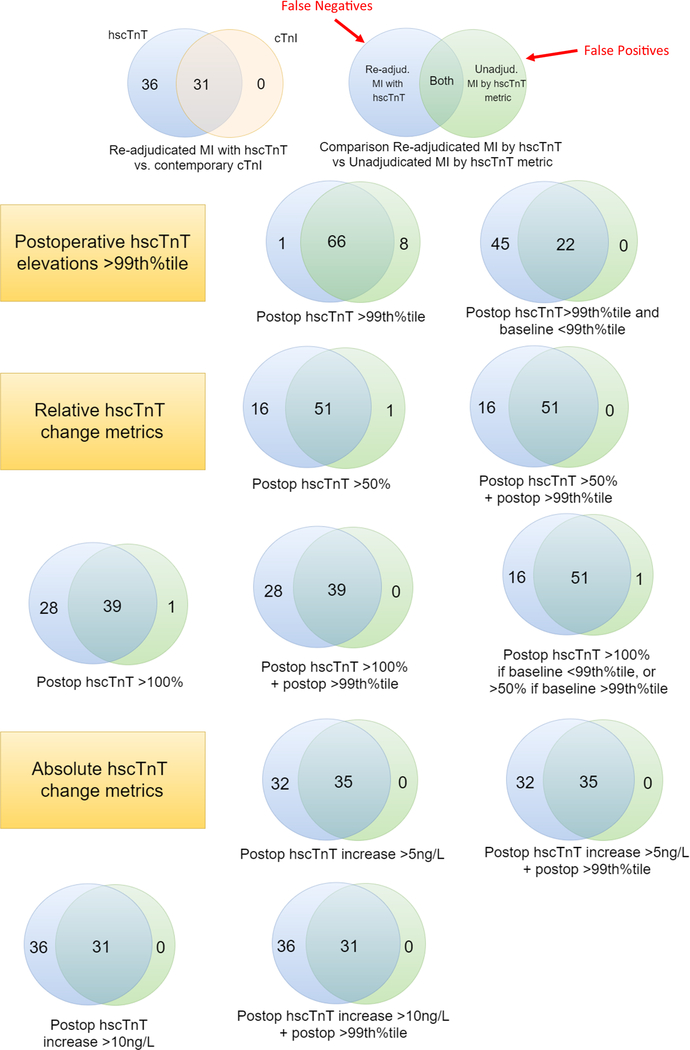
Incidence rates of perioperative MI ranged from 3.6% (n=22) to 12% (n=74) by absolute and relative hscTnT change metric, when diagnosed in combination with ischemic ECG changes, but without event adjudication, a >3-fold difference. Figure 1 shows Venn diagrams comparing re-adjudicated MI call rates by hscTnT to the call rates obtained by using absolute and relative hscTnT change metric.
Figure 1. Comparison of MI Call Rates between cTnI and hscTnT.
Venn diagrams depicting individual comparisons of MI call rates between adjudicated hscTnT MIs (blue), cTnI (bisque), and one of 11 unadjudicated hscTnT absolute or relative change metric (green). Overlapping areas indicate MI cases that were correctly called by both methods; to the right are cases that were falsely classified as MI (false positives) by unadjudicated hscTnT metric; to the left are events that were missed by the unadjudicated hscTnT metric (false negatives), indicated by the red arrows.
Short-Term and Long-Term Mortality
Among the 605 study patients, there were 21 (3.5%) deaths at 6 months, 42 (7.0%) deaths at 1 year, and 96 (16%) deaths at 3 years. Table 3 compares hazard ratios for each cTnI and hscTnT change metric and Figure 2 shows Kaplan-Meier survival curves for MIs adjudicated by either contemporary cTnI assays versus hscTnT. Patients with new postoperative hscTnT elevation above the 99th percentile, either by absolute or relative hscTnT change metric, experienced up to 5-fold increase in 6-month mortality. This finding was consistent with the 3.4-fold increased risk of short-term mortality seen in MI diagnosed by the contemporary TnI (p= 0.047, 95% CI: 1.0, 12). The association of preoperative and postoperative hscTnT elevation with increased rate of mortality decreased over the 1-year and 3-year follow-up periods (Table 3).
Table 3:
Hazard Ratios of Myocardial Injury and Infarction
| Six Month Mortality Hazard Ratio (21 deaths) |
One Year Mortality Hazard Ratio (42 deaths) |
Three Year Mortality Hazard Ratio (92 deaths) |
Incidence of Death (3yrs) |
||||
|---|---|---|---|---|---|---|---|
| Myocardial Injury and Infarction Change Metrics | Unadjusted [95% CI] n=605 | Adjusted [95% CI] n=596 | Unadjusted [95% CI] n = 605 | Adjusted [95% CI] n= 596 | Unadjusted [95% CI] n= 605 | Adjusted [95% CI], n=596 | Deaths per MI metric no. (%) |
| MI by contemporary cTnI (n=31) | 3.4 [1.0, 12] | 3.4 [1.0, 12] | 1.5 [0.5, 5.0] | 1.5 [0.4, 5.0] | 1.4 [0.6, 3.2] | 1.3 [0.6, 3.1] | 6 (18.8%) |
| Myocardial Injury by cTnI (n=82) | 1.6 [0.5, 4.8] | 1.3 [0.4, 4.0] | 1.1 [0.5, 2.6] | 0.9 [0.4, 2.2] | 1.3 [0.7, 2.2] | 1.1 [0.6, 2.0] | 9 (11.0%) |
| Myocardial Injury by hscTnT (n= 324) | 2.0 [0.8, 5.2] | 1.3 [0.5, 3.7] | 2.1 [1.1, 4.1] | 1.6 [0.8, 3.2] | 1.9 [1.2, 3.0] | 1.7 [1.1, 2.7] | 61 (18.8%) |
| Re-adjudicated MI using hscTnT1 (n=67) | 3.6 [1.4, 9.3] | 3.2 [1.2, 8.6] | 1.4 [0.6, 3.4] | 1.2 [0.5, 3.0] | 1.1 [0.6, 2.1] | 1.0 [0.5, 1.9] | 11 (16.4%) |
| Relative hscTnT change metrics for MI | |||||||
| Increased >50% from baseline (n= 52) | 4.8 [1.8, 12] | 4.3 [1.6, 11] | 1.9 [0.8, 4.6] | 1.7 [0.7, 4.2] | 1.2 [0.6, 2.4] | 1.1 [0.5, 2.1] | 9 (17.3%) |
| Increased >50% from baseline and one post-op value >99th %tile (n=51) | 4.9 [1.8, 13] | 4.3 [1.6, 12] | 2.0 [0.8, 4.7] | 1.7 [0.7, 4.2] | 1.1 [0.5, 2.3] | 0.9 [0.4, 2.0] | 8 (15.7%) |
| Increased >100% from baseline (n=40) | 5.0 [1.8, 14] | 4.8 [1.7, 13] | 2.1 [0.8, 5.4] | 2.0 [0.8, 5.2] | 1.4 [0.7, 3.0] | 1.4 [0.7, 2.9] | 8 (20.0%) |
| Increased >100% from baseline and one post-op value >99th%tile (n=39) | 5.1 [1.8, 14] | 4.8 [1.7, 14] | 2.2 [0.6, 5.5] | 2.0 [0.8, 5.3] | 1.3 [0.6, 2.8] | 1.2 [0.5, 2.6] | 7 (18.0%) |
| Increased >100% if baseline <99th%, or >50% if baseline hscTnT >99th% (n=52) | 4.7 [1.8, 12] | 4.3 [1.6, 11] | 1.9 [0.8, 4.6] | 1.7 [0.7, 4.2] | 1.2 [0.6, 2.4] | 1.1 [0.5, 2.1] | 9 (17.3%) |
| Absolute hscTnT change metrics MI | |||||||
| Post-op hscTnT >99th%tile (n=74) | 4.0 [1.6, 10] | 3.7 [1.4, 9.6] | 1.6 [0.7, 3.5] | 1.3 [0.6, 3.1] | 1.1 [0.6, 2.1] | 1.0 [0.5, 1.8] | 12 (16.2%) |
| Post-op hscTnT >99th%tile if baseline <99th %tile (n=22) | 4.9 [1.4, 17] | 5.0 [1.4, 17] | 2.3 [0.7, 7.3] | 2.3 [0.7, 7.3] | 0.9 [0.3, 3.0] | 1.0 [0.3, 3.0] | 3 (13.6%) |
| Increased by >10 ng/L (n=31) | 3.5 [1.0, 12] | 3.5[1.0, 12] | 1.5 [0.5, 5.0] | 1.6 [0.5, 5.3] | 1.1 [0.5, 2.8] | 1.1 [0.4, 2.8] | 5 (16.1%) |
| Increased by >10 ng/L and one post-op value >99th%tile (n=31) | 3.5 [1.0, 12] | 3.5 [1.0, 12] | 1.5 [0.5, 5.0] | 1.6 [0.5, 5.3] | 1.1 [0.5, 2.8] | 1.1 [0.5, 2.8] | 5 (16.1%) |
1-Adjudicated MI events after detailed review of patient records. Bold p<0.05.
Figure 2A-C. Unadjusted Kaplan-Meier Survival Curves for MI diagnosed by three representative hscTnT metrics.
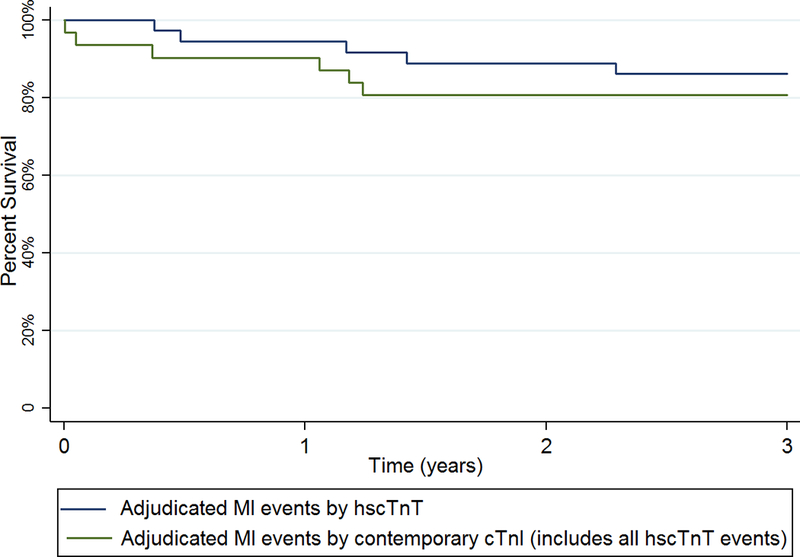
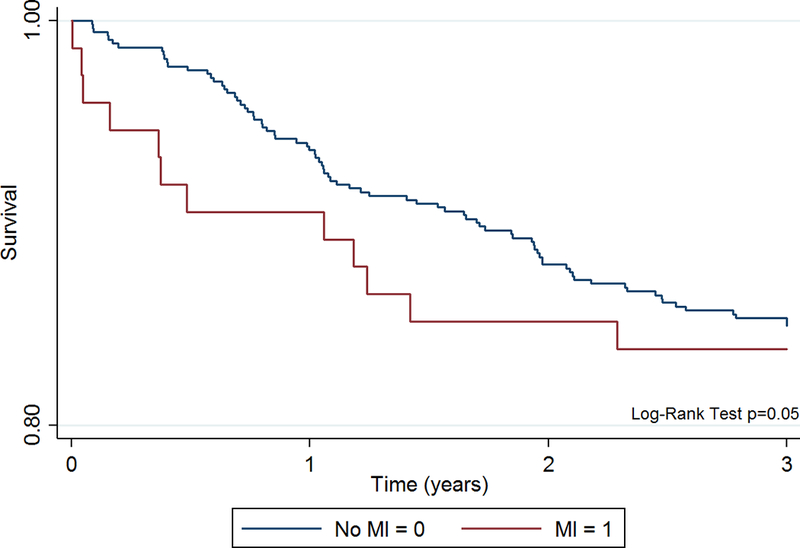
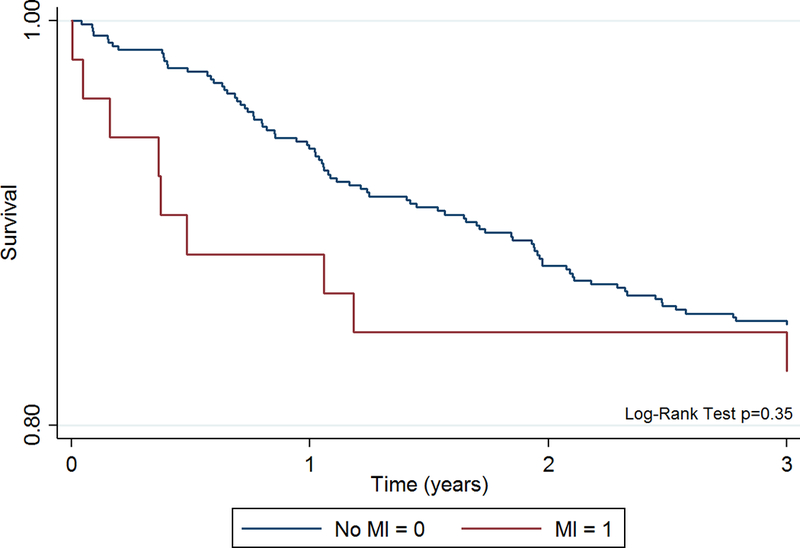
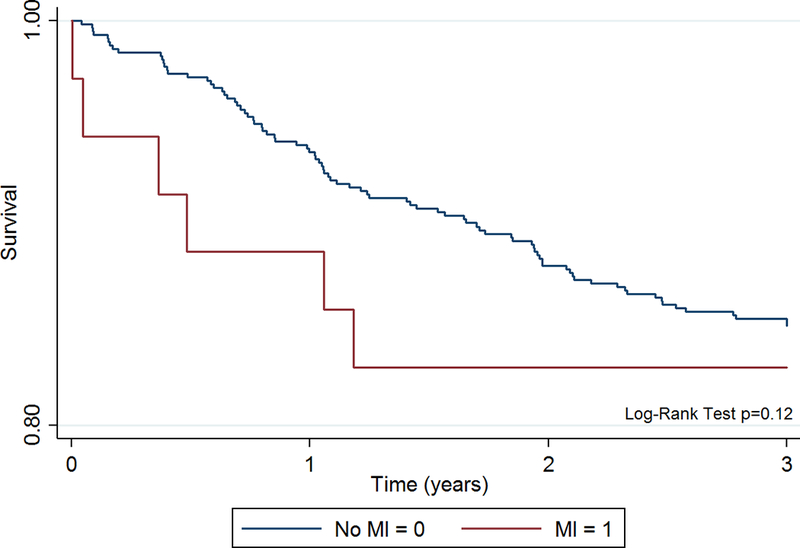
All MIs needed evidence if ischemic ECG changes plus either one postoperative hscTnT value >99th% (Fig. 2A), a >50% hscTnT increase (Fig. 2B), or a >5ng/L hscTnT increase (Fig. 2C).
Discussion
High-sensitivity cardiac troponin assays have profoundly changed how acute MI is diagnosed.11,20–22 When clinicians rely on contemporary non-high-sensitivity cTn assays, the only available standard in the United States until very recently, the recommendation is to obtain a cTn value at the time of presentation and a second one 6–9 hours later due to the relative insensitivity of the assay. hscTn – in contrast – can detect a rising or falling cTn pattern in less than 2 hours with a high degree of sensitivity and specificity to rule-in/-out acute MI. Over the last five years, significant progress has been made in the clarification of rule-in/rule-out protocols for acute MI in patients presenting with clinical symptoms consistent with acute coronary syndrome in the emergency department using hscTn assays.11,21–29 However, scant if any data are currently available for perioperative patients using the hscTn assays. Thus, the goal of this study was to fill the knowledge gap and to determine if the introduction of hscTnT versus contemporary non-high-sensitivity cTn assays would change the incidence rates of detected perioperative myocardial injury and infarction.
In the United States, the current standard cTn assays do not have the analytic sensitivity of hscTn assays and were used in the parent VINO trial to diagnose myocardial injury and infarction. In this ancillary study, these incidence rates (14%, and 5%, respectively) were used as main comparator. We then re-adjudicated all patients with a new postoperative hscTnT elevation >99th percentile, or – if they were already elevated > 99th percentile at baseline – a >50% postoperative hscTnT rise for missed cardiac events. After re-adjudication, the “call rate” increased from 14% to 22% for myocardial injury and from 5% to 11% for myocardial infarction, about a 2-fold increase.
In order to determine, how incidence rates of myocardial injury and infarction would differ when only using hscTnT change metric and ECG evidence of myocardial ischemia, but without adjudication, we then compared a total of 11 absolute and relative hscTnT change metrics. These absolute and relative hscTnT change metrics had been proposed in the literature as diagnostic cutoffs for acute MI in patients with acute chest pain presenting to the emergency department. Some hscTnT metrics were too stringent and resulted in lower call rate compared to the contemporary cTnI assay (e.g., postoperative hscTnT >99th percentile if baseline <99th percentile), and some were overly broad, such as simply relying on a postoperative hscTnT elevation >99th percentile without comparison to the preoperative baseline value. Most hscTnT change metrics, however, resulted in a markedly higher call rate of postoperative myocardial injury and infarction. However, the call rate may even be higher if clinicians use different approaches.13
Short-term mortality (6-month) risk was increased 3- to 5-fold when patients experienced a postoperative hscTnT increase and this effect was rather consistent regardless of the hscTnT change metric used. Of note, as we have shown previously preoperatively elevated hscTnT above the 99th percentile, an indicator of elevated cardiovascular risk, was independently associated with both short-term as well as long-term mortality.5 The multicenter VISION study showed conclusively that isolated postoperative cTn elevations are associated with an increased risk for 30-day morbidity and mortality, yet VISION did not collect preoperative blood samples and was thus unable to definitively determine if these cTn elevations were new or in a rising/falling pattern.9,29 Our study now provides definitive evidence that both myocardial injury as well as myocardial infarction detected and quantified by comparing baseline and peak postoperative hscTnT samples markedly influence postoperative cardiovascular outcomes.
The definitive value of the 99th percentile for the hscTnT assay is currently under discussion: we used the published sex-specific values of 10 ng/L for women and 14.5 ng/L for men.16 However, others recommend higher values, 13 ng/L for women and 20 ng/L for men. Because this is an area of active investigation, reference values may change in the future and thus influence the validity of our results. Furthermore, comparisons to hscTnI assays have not been published and would be very informative, as many hospitals use hscTnI and not hscTnT.
At present, the mechanism underlying postoperative cardiac troponin release after non-cardiac surgery is unclear, and there may be some pathophysiological differences between early and late increases. In some patients, the mechanism is likely due to supply-demand mismatch and ischemic imbalance in the setting of obstructive coronary artery disease resulting in myocardial ischemia. In other patients, however, it may involve mechanism that resemble more stress-induced cardiomyopathy or simple shear stress of cardiomyocytes without coronary flow limitation. In other patients, postoperative cTn may be due to secondary causes such as pulmonary embolism or sepsis. We believe in our patient population, the majority of events were due to acute myocardial injury or non-ST-elevation MI (type II MI), as the exact nature and nomenclature is currently under discussion.30
Evidence from this study suggest that (1) it is helpful to obtain a preoperative hscTnT value to determine if a postoperatively elevated hscTnT value is new, and to be able to quantify the extent of myocardial injury, and (2) that the use of hscTn assays will be markedly more sensitive in the diagnosis of postoperative myocardial injury and infarction. At present, it is unclear which particular hscTn absolute or relative change metric will be used in the future, but it appears that a >50% increase with at least one value >99th percentile may be a good starting point.
This study had several limitations. The patient population as well as surgical procedures were high-risk. Thus, the results of this study may not be applicable to an unselected adult patient population. As one of the most recent guidelines states, recommendations pertain only to patients (1) 45 years of age and older or (2) patients 18–44 years of age with known significant cardiovascular disease who undergo surgeries that require at least an overnight stay in the hospital after surgery. 31
In conclusion, this study showed that the use of a novel hscTnT assay – regardless of change metric – will likely lead to an increased incidence rate of diagnosed perioperative MI. Both absolute and relative hscTnT rising patterns have prognostic implications for short term mortality after non-cardiac surgery.
Acknowledgments
Funding/Support:
The parent VINO trial was funded by a grant from the National Institute for General Medical Sciences (K23 GM087534) and a grant to Washington University Institute of Clinical and Translational Sciences (UL1RR024992), the Foundation for Anesthesia Education and Research (FAER), and the Division of Clinical and Translational Research, Department of Anesthesiology, Washington University. Roche Diagnostics (Indianapolis, IN) provided the hscTnT assays and covered the costs of running these assays. PN is currently funded by NIH/NHLBI (R01HL126892).
Footnotes
Disclosures:
Brown, Samaha, Rao, Helwani, Duma, Brown, Gage, Miller: No conflicts of interest.
Nagele: Research Support: Roche Diagnostics US; Abbott Diagnostics.
Scott: Research Support - Siemens Healthcare Diagnostic; Abbott Diagnostics, Instrumentation Laboratories; Consulting - Instrumentation Laboratories; Becton-Dickinson, Alere; Speaker fees: Abbott
Jaffe: Consultation: Beckman, Ortho, Abbott, Alere, Critical Diagnostics, Roche, Radiometer, Amgen and theHeart.org
Apple: Industry Grant/Research Support through Minneapolis Medical Research Foundation, no salary, that involve cardiac troponin: Abbott Diagnostics, Siemens, Ortho-Clinical Diagnostics, Roche Diagnostics, Radiometer; Paid Consultant: Instrumentation Laboratories, Alere, T2 Biosystems
Contributor Information
Jamie C. Brown, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine in St. Louis
Eslam Samaha, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine in St. Louis
Srikar Rao, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine in St. Louis
Mohammad A. Helwani, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine in St. Louis
Andreas Duma, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine in St. Louis
Frank Brown, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine in St. Louis
Brian F. Gage, Department of Internal Medicine, Washington University School of Medicine in St. Louis
J. Philip Miller, Department of Internal Medicine, Division of Biostatistics, Washington University School of Medicine in St. Louis
Allan S. Jaffe, Cardiovascular Division, Department of Internal Medicine and Division of Core Clinical Laboratory Services, Department of Laboratory Medicine and Pathology, Rochester, Minnesota, Mayo Clinic and Medical School
Fred S. Apple, Department of Laboratory Medicine & Pathology, Minneapolis, Minnesota, Hennepin County Medical Center and University of Minnesota School of Medicine
Mitchell G. Scott, Department of Pathology & Immunology, Washington University School of Medicine in St. Louis
Peter Nagele, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine in St. Louis
References
- 1.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Katus HA, Lindahl B, Morrow DA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Infarction JTFftUDoM. Third universal definition of myocardial infarction. Circulation 2012;126:2020–35. [DOI] [PubMed] [Google Scholar]
- 2.Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, Davila-Roman VG, Gerhard-Herman MD, Holly TA, Kane GC, Marine JE, Nelson MT, Spencer CC, Thompson A, Ting HH, Uretsky BF, Wijeysundera DN, American College of C, American Heart A. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 2014;64:e77–137. [DOI] [PubMed] [Google Scholar]
- 3.Biccard BM, Rodseth RN. The pathophysiology of peri-operative myocardial infarction. Anaesthesia 2010;65:733–41. [DOI] [PubMed] [Google Scholar]
- 4.Landesberg G, Beattie WS, Mosseri M, Jaffe AS, Alpert JS. Perioperative myocardial infarction. Circulation 2009;119:2936–44. [DOI] [PubMed] [Google Scholar]
- 5.Nagele P, Brown F, Gage BF, Gibson DW, Miller JP, Jaffe AS, Apple FS, Scott MG. High-sensitivity cardiac troponin T in prediction and diagnosis of myocardial infarction and long-term mortality after noncardiac surgery. Am Heart J 2013;166:325–32 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weber M, Luchner A, Seeberger M, Mueller C, Liebetrau C, Schlitt A, Apostolovic S, Jankovic R, Bankovic D, Jovic M, Mitrovic V, Nef H, Mollmann H, Hamm CW. Incremental value of high-sensitive troponin T in addition to the revised cardiac index for peri-operative risk stratification in non-cardiac surgery. Eur Heart J 2013;34:853–62. [DOI] [PubMed] [Google Scholar]
- 7.Kavsak PA, Walsh M, Srinathan S, Thorlacius L, Buse GL, Botto F, Pettit S, McQueen MJ, Hill SA, Thomas S, Mrkobrada M, Alonso-Coello P, Berwanger O, Biccard BM, Cembrowski G, Chan MT, Chow CK, de Miguel A, Garcia M, Graham MM, Jacka MJ, Kueh JH, Li SC, Lit LC, Martinez-Bru C, Naidoo P, Nagele P, Pearse RM, Rodseth RN, Sessler DI, Sigamani A, Szczeklik W, Tiboni M, Villar JC, Wang CY, Xavier D, Devereaux PJ. High sensitivity troponin T concentrations in patients undergoing noncardiac surgery: a prospective cohort study. Clin Biochem 2011;44:1021–4. [DOI] [PubMed] [Google Scholar]
- 8.Nagele P, Brown F, Francis A, Scott MG, Gage BF, Miller JP, Team VS. Influence of nitrous oxide anesthesia, B-vitamins, and MTHFR gene polymorphisms on perioperative cardiac events: the vitamins in nitrous oxide (VINO) randomized trial. Anesthesiology 2013;119:19–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Botto F, Alonso-Coello P, Chan MT, Villar JC, Xavier D, Srinathan S, Guyatt G, Cruz P, Graham M, Wang CY, Berwanger O, Pearse RM, Biccard BM, Abraham V, Malaga G, Hillis GS, Rodseth RN, Cook D, Polanczyk CA, Szczeklik W, Sessler DI, Sheth T, Ackland GL, Leuwer M, Garg AX, Lemanach Y, Pettit S, Heels-Ansdell D, Luratibuse G, Walsh M, Sapsford R, Schunemann HJ, Kurz A, Thomas S, Mrkobrada M, Thabane L, Gerstein H, Paniagua P, Nagele P, Raina P, Yusuf S, Devereaux PJ, Devereaux PJ, Sessler DI, Walsh M, Guyatt G, McQueen MJ, Bhandari M, Cook D, Bosch J, Buckley N, Yusuf S, Chow CK, Hillis GS, Halliwell R, Li S, Lee VW, Mooney J, Polanczyk CA, Furtado MV, Berwanger O, Suzumura E, Santucci E, Leite K, Santo JA, Jardim CA, Cavalcanti AB, Guimaraes HP, Jacka MJ, Graham M, McAlister F, McMurtry S, Townsend D, Pannu N, Bagshaw S, Bessissow A, Bhandari M, Duceppe E, Eikelboom J, Ganame J, Hankinson J, Hill S, Jolly S, Lamy A, Ling E, Magloire P, Pare G, Reddy D, Szalay D, Tittley J, Weitz J, Whitlock R, Darvish-Kazim S, Debeer J, Kavsak P, Kearon C, Mizera R, O’Donnell M, McQueen M, Pinthus J, Ribas S, Simunovic M, Tandon V, Vanhelder T, Winemaker M, Gerstein H, McDonald S, O’Bryne P, Patel A, Paul J, Punthakee Z, Raymer K, Salehian O, Spencer F, Walter S, Worster A, Adili A, Clase C, Cook D, Crowther M, Douketis J, Gangji A, Jackson P, Lim W, Lovrics P, Mazzadi S, Orovan W, Rudkowski J, Soth M, Tiboni M, Acedillo R, Garg A, Hildebrand A, Lam N, Macneil D, Mrkobrada M, Roshanov PS, Srinathan SK, Ramsey C, John PS, Thorlacius L, Siddiqui FS, Grocott HP, McKay A, Lee TW, Amadeo R, Funk D, McDonald H, Zacharias J, Villar JC, Cortes OL, Chaparro MS, Vasquez S, Castaneda A, Ferreira S, Coriat P, Monneret D, Goarin JP, Esteve CI, Royer C, Daas G, Chan MT, Choi GY, Gin T, Lit LC, Xavier D, Sigamani A, Faruqui A, Dhanpal R, Almeida S, Cherian J, Furruqh S, Abraham V, Afzal L, George P, Mala S, Schunemann H, Muti P, Vizza E, Wang CY, Ong GS, Mansor M, Tan AS, Shariffuddin II, Vasanthan V, Hashim NH, Undok AW, Ki U, Lai HY, Ahmad WA, Razack AH, Malaga G, Valderrama-Victoria V, Loza-Herrera JD, De Los Angeles Lazo M, Rotta-Rotta A, Szczeklik W, Sokolowska B, Musial J, Gorka J, Iwaszczuk P, Kozka M, Chwala M, Raczek M, Mrowiecki T, Kaczmarek B, Biccard B, Cassimjee H, Gopalan D, Kisten T, Mugabi A, Naidoo P, Naidoo R, Rodseth R, Skinner D, Torborg A, Paniagua P, Urrutia G, Maestre ML, Santalo M, Gonzalez R, Font A, Martinez C, Pelaez X, De Antonio M, Villamor JM, Garcia JA, Ferre MJ, Popova E, Alonso-Coello P, Garutti I, Cruz P, Fernandez C, Palencia M, Diaz S, Del Castillo T, Varela A, de Miguel A, Munoz M, Pineiro P, Cusati G, Del Barrio M, Membrillo MJ, Orozco D, Reyes F, Sapsford RJ, Barth J, Scott J, Hall A, Howell S, Lobley M, Woods J, Howard S, Fletcher J, Dewhirst N, Williams C, Rushton A, Welters I, Leuwer M, Pearse R, Ackland G, Khan A, Niebrzegowska E, Benton S, Wragg A, Archbold A, Smith A, McAlees E, Ramballi C, Macdonald N, Januszewska M, Stephens R, Reyes A, Paredes LG, Sultan P, Cain D, Whittle J, Del Arroyo AG, Sessler DI, Kurz A, Sun Z, Finnegan PS, Egan C, Honar H, Shahinyan A, Panjasawatwong K, Fu AY, Wang S, Reineks E, Nagele P, Blood J, Kalin M, Gibson D, Wildes T, Vascular events In noncardiac Surgery patIents cOhort evaluatioN Writing Group oboTVeInSpceI, Appendix 1. The Vascular events In noncardiac Surgery patIents cOhort evaluatio NSIWG, Appendix 2. The Vascular events In noncardiac Surgery patIents cOhort evaluatio NOC, Vascular events In noncardiac Surgery patIents cOhort evaluatio NVSI. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 2014;120:564–78. [DOI] [PubMed] [Google Scholar]
- 10.Biccard BM, Devereaux PJ, Rodseth RN. Cardiac biomarkers in the prediction of risk in the non-cardiac surgery setting. Anaesthesia 2014;69:484–93. [DOI] [PubMed] [Google Scholar]
- 11.Sandoval Y, Smith SW, Apple FS. Present and Future of Cardiac Troponin in Clinical Practice: A Paradigm Shift to High-Sensitivity Assays. Am J Med 2016;129:354–65. [DOI] [PubMed] [Google Scholar]
- 12.Lipinski MJ, Baker NC, Escarcega RO, Torguson R, Chen F, Aldous SJ, Christ M, Collinson PO, Goodacre SW, Mair J, Inoue K, Lotze U, Sebbane M, Cristol JP, Freund Y, Chenevier-Gobeaux C, Meune C, Eggers KM, Pracon R, Schreiber DH, Wu AH, Ordonez-Llanos J, Jaffe AS, Twerenbold R, Mueller C, Waksman R. Comparison of conventional and high-sensitivity troponin in patients with chest pain: a collaborative meta-analysis. Am Heart J 2015;169:6–16 e6. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Mair J, Giannitsis E, Mueller C, Lindahl B, Blankenberg S, Huber K, Plebani M, Biasucci LM, Tubaro M, Collinson P, Venge P, Hasin Y, Galvani M, Koenig W, Hamm C, Alpert JS, Katus H, Jaffe AS, Study Group on Biomarkers in Cardiology of ESC Working Group on Acute Cardiac Care. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J 2012;33:2252–7. [DOI] [PubMed] [Google Scholar]
- 14.Shah AS, Anand A, Sandoval Y, Lee KK, Smith SW, Adamson PD, Chapman AR, Langdon T, Sandeman D, Vaswani A, Strachan FE, Ferry A, Stirzaker AG, Reid A, Gray AJ, Collinson PO, McAllister DA, Apple FS, Newby DE, Mills NL, High Si. High-sensitivity cardiac troponin I at presentation in patients with suspected acute coronary syndrome: a cohort study. Lancet 2015;386:2481–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reichlin T, Cullen L, Parsonage WA, Greenslade J, Twerenbold R, Moehring B, Wildi K, Mueller S, Zellweger C, Mosimann T, Rubini Gimenez M, Rentsch K, Osswald S, Muller C. Two-hour algorithm for triage toward rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Am J Med 2015;128:369–79 e4. [DOI] [PubMed] [Google Scholar]
- 16.Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA. Analytical validation of a high-sensitivity cardiac troponin T assay. Clin Chem 2010;56:254–61. [DOI] [PubMed] [Google Scholar]
- 17.Giannitsis E, Becker M, Kurz K, Hess G, Zdunek D, Katus HA. High-sensitivity cardiac troponin T for early prediction of evolving non-ST-segment elevation myocardial infarction in patients with suspected acute coronary syndrome and negative troponin results on admission. Clin Chem 2010;56:642–50. [DOI] [PubMed] [Google Scholar]
- 18.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Katus HA, Lindahl B, Morrow DA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasché P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Infarction JEAAWTFftUDoM. Third universal definition of myocardial infarction. Circulation 2012;126:2020–35. [DOI] [PubMed] [Google Scholar]
- 19.Jaffe AS, Moeckel M, Giannitsis E, Huber K, Mair J, Mueller C, Plebani M, Thygesen K, Lindahl B. In search for the Holy Grail: suggestions for studies to define delta changes to diagnose or exclude acute myocardial infarction: a position paper from the study group on biomarkers of the Acute Cardiovascular Care Association. Eur Heart J Acute Cardiovasc Care 2014;3:313–6. [DOI] [PubMed] [Google Scholar]
- 20.Nestelberger T, Wildi K, Boeddinghaus J, Twerenbold R, Reichlin T, Gimenez MR, Puelacher C, Jaeger C, Grimm K, Sabti Z, Hillinger P, Kozhuharov N, du Fay de Lavallaz J, Pinck F, Lopez B, Salgado E, Miro O, Bingisser R, Lohrmann J, Osswald S, Mueller C. Characterization of the observe zone of the ESC 2015 high-sensitivity cardiac troponin 0h/1h-algorithm for the early diagnosis of acute myocardial infarction. Int J Cardiol 2016;207:238–45. [DOI] [PubMed] [Google Scholar]
- 21.Jaeger C, Wildi K, Twerenbold R, Reichlin T, Rubini Gimenez M, Neuhaus JD, Grimm K, Boeddinghaus J, Hillinger P, Nestelberger T, Singeisen H, Gugala M, Pretre G, Puelacher C, Wagener M, Honegger U, Schumacher C, Moreno Weidmann Z, Kreutzinger P, Krivoshei L, Freese M, Stelzig C, Dietsche S, Ernst S, Rentsch K, Osswald S, Mueller C. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am Heart J 2016;171:92–102 e1–5. [DOI] [PubMed] [Google Scholar]
- 22.Boeddinghaus J, Reichlin T, Cullen L, Greenslade JH, Parsonage WA, Hammett C, Pickering JW, Hawkins T, Aldous S, Twerenbold R, Wildi K, Nestelberger T, Grimm K, Rubini-Gimenez M, Puelacher C, Kern V, Rentsch K, Than M, Mueller C. Two-Hour Algorithm for Triage toward Rule-Out and Rule-In of Acute Myocardial Infarction by Use of High-Sensitivity Cardiac Troponin I. Clin Chem 2016;62:494–504. [DOI] [PubMed] [Google Scholar]
- 23.Twerenbold R, Wildi K, Jaeger C, Gimenez MR, Reiter M, Reichlin T, Walukiewicz A, Gugala M, Krivoshei L, Marti N, Moreno Weidmann Z, Hillinger P, Puelacher C, Rentsch K, Honegger U, Schumacher C, Zurbriggen F, Freese M, Stelzig C, Campodarve I, Bassetti S, Osswald S, Mueller C. Optimal Cutoff Levels of More Sensitive Cardiac Troponin Assays for the Early Diagnosis of Myocardial Infarction in Patients With Renal Dysfunction. Circulation 2015;131:2041–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tanglay Y, Twerenbold R, Lee G, Wagener M, Honegger U, Puelacher C, Reichlin T, Mann S, Druey S, Hochgruber T, Zurcher S, Radosavac M, Kreutzinger P, Pretre G, Stallone F, Hillinger P, Jaeger C, Rubini Gimenez M, Freese M, Wild D, Rentsch K, Osswald S, Zellweger MJ, Mueller C. Incremental value of a single high-sensitivity cardiac troponin I measurement to rule out myocardial ischemia. Am J Med 2015;128:638–46. [DOI] [PubMed] [Google Scholar]
- 25.Sara JD, Holmes DR Jr., Jaffe AS Fundamental concepts of effective troponin use: important principles for internists. Am J Med 2015;128:111–9. [DOI] [PubMed] [Google Scholar]
- 26.Sanchis J, Abellan L, Garcia-Blas S, Mainar L, Mollar A, Valero E, Consuegra-Sanchez L, Roque M, Bertomeu-Gonzalez V, Chorro FJ, Nunez E, Nunez J. Usefulness of delta troponin for diagnosis and prognosis assessment of non-ST-segment elevation acute chest pain. Eur Heart J Acute Cardiovasc Care 2016;5:399–406. [DOI] [PubMed] [Google Scholar]
- 27.Rubini Gimenez M, Twerenbold R, Jaeger C, Schindler C, Puelacher C, Wildi K, Reichlin T, Haaf P, Merk S, Honegger U, Wagener M, Druey S, Schumacher C, Krivoshei L, Hillinger P, Herrmann T, Campodarve I, Rentsch K, Bassetti S, Osswald S, Mueller C. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am J Med 2015;128:861–70 e4. [DOI] [PubMed] [Google Scholar]
- 28.Reichlin T, Twerenbold R, Wildi K, Rubini Gimenez M, Bergsma N, Haaf P, Druey S, Puelacher C, Moehring B, Freese M, Stelzig C, Krivoshei L, Hillinger P, Jager C, Herrmann T, Kreutzinger P, Radosavac M, Weidmann ZM, Pershyna K, Honegger U, Wagener M, Vuillomenet T, Campodarve I, Bingisser R, Miro O, Rentsch K, Bassetti S, Osswald S, Mueller C. Prospective validation of a 1-hour algorithm to rule-out and rule-in acute myocardial infarction using a high-sensitivity cardiac troponin T assay. CMAJ 2015;187:E243–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neumann JT, Sorensen NA, Schwemer T, Ojeda F, Bourry R, Sciacca V, Schaefer S, Waldeyer C, Sinning C, Renne T, Than M, Parsonage W, Wildi K, Makarova N, Schnabel RB, Landmesser U, Mueller C, Cullen L, Greenslade J, Zeller T, Blankenberg S, Karakas M, Westermann D. Diagnosis of Myocardial Infarction Using a High-Sensitivity Troponin I 1-Hour Algorithm. JAMA Cardiol 2016;1:397–404. [DOI] [PubMed] [Google Scholar]
- 29.Vascular Events In Noncardiac Surgery Patients Cohort Evaluation Study I, Devereaux PJ, Chan MT, Alonso-Coello P, Walsh M, Berwanger O, Villar JC, Wang CY, Garutti RI, Jacka MJ, Sigamani A, Srinathan S, Biccard BM, Chow CK, Abraham V, Tiboni M, Pettit S, Szczeklik W, Lurati Buse G, Botto F, Guyatt G, Heels-Ansdell D, Sessler DI, Thorlund K, Garg AX, Mrkobrada M, Thomas S, Rodseth RN, Pearse RM, Thabane L, McQueen MJ, VanHelder T, Bhandari M, Bosch J, Kurz A, Polanczyk C, Malaga G, Nagele P, Le Manach Y, Leuwer M, Yusuf S. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA 2012;307:2295–304. [DOI] [PubMed] [Google Scholar]
- 30.Nagele P The Case for a Revised Definition of Myocardial Infarction-Resolving the Ambiguity of Type 2 Myocardial Infarction. JAMA Cardiol 2016;1:247–8. [DOI] [PubMed] [Google Scholar]
- 31.Duceppe E, Parlow J, MacDonald P, Lyons K, McMullen M, Srinathan S, Graham M, Tandon V, Styles K, Bessissow A, Sessler DI, Bryson G, Devereaux PJ. Canadian Cardiovascular Society Guidelines on Perioperative Cardiac Risk Assessment and Management for Patients Who Undergo Noncardiac Surgery. Can J Cardiol 2017;33:17–32. [DOI] [PubMed] [Google Scholar]