Abstract
Objective
Drinking goals set at treatment-onset predict treatment outcome in patients with alcohol use disorders. Yet, the cognitive constructs of goal setting and goal attainment are understudied in young adult drinkers. This study sought to examine how the interplay of goal setting and goal attainment during treatment impacts treatment outcome in a sample of young adult heavy drinkers.
Method
Participants were 128 young adult heavy drinkers (Mage=21.5 years) who participated in a double-blind, placebo-controlled, 8-week efficacy trial of naltrexone plus brief counseling. Participants were not required to be interested in changing their drinking for inclusion. Drinking goals were assessed at baseline, mid-treatment, and end-of-treatment. Alcohol outcomes were peak drinking, typical drinking, and drinking frequency.
Results
Results from PROCESS serial, multiple mediator models showed that goal setting and goal attainment at mid-treatment collectively predicted peak drinking (b= 0.87, 95%CI: 0.40, 1.37) and drinking frequency (b = 0.66, 95%CI: 0.37, 1.06). Only mid-treatment goal setting mediated the relationship between baseline goal setting and reduction of drinking frequency (b=0.35, 95%CI: 0.10, 0.85). Participants who set more ambitious drinking goals at baseline were more likely to set subsequent, ambitious goals; more ambitious goals at mid-treatment were associated with better treatment outcomes.
Conclusion
Setting initial, ambitious goals led to further ambitious goals, which ultimately contributed to lower levels of drinking. Thus, cognitive processes during treatment may be an important target of intervention efforts. For example, the inclusion of goal-setting exercises during treatment could serve to improve intervention effects.
Keywords: drinking, goal setting, young adults, drinking goals, alcohol
Heavy episodic drinking (i.e., consuming 4 or more drinks on a single occasion for females; 5 or more drinks on an occasion for males) is common among young adults (Substance Abuse and Mental Health Services Administration, 2011) and is associated with significant negative consequences (Jackson, Sher, Gotham, & Wood, 2001; Slutske, 2005). One of the most common interventions for college and young adult drinking is a harm reduction-based, brief motivational intervention (Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Foxcroft, Coombes, Wood, Allen, & Santimano, 2014). Indeed, treatment recommendations from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and guidance issued by the Food and Drug Administration (FDA) support alcohol treatments that target reductions in overall alcohol consumption and/or total abstinence (Allen, 2003; FDA, 2015). Young adults have reported that drinking goals to reduce the quantity and frequency of drinking are more desired than total abstinence (Epler, Sher, Loomis, & O’Malley, 2009). Yet, most work examining the effects of drinking goals on treatment outcomes arises from studies on patients with alcohol dependence and examines categorical drinking goals (e.g., abstinence vs. non-abstinence). Even in these broad terms, drinking goals at the onset of treatment are predictive of treatment outcomes (Bujarski, O’Malley, Lunny & Ray, 2013; Dunn & Strain, 2013). Yet, little work has examined the role of goal setting on treatment outcomes in young adult heavy drinkers.
Cognitive processes, including goal setting, can impact drinking behavior. In a review of behavioral counseling interventions for alcohol use among adults, goal setting (any vs. none) was one of three treatment elements (the others being feedback and advice) that led to statistically significant improvements in treatment outcomes (Whitlock, Polen, Green, Orleans, & Klein, 2004). Another study found that the inclusion of any goal setting was associated with larger effect sizes in brief interventions in college students (Scott-Sheldon, Carey, Elliott, Garey, & Carey, 2014). Further, setting a goal to reduce drinking prior to the weekend has been linked to reductions in binge drinking episodes during the weekend among young adults (Suffoletto, Kristan, Monti, & Clark, 2014). These studies highlight the potential importance of including a goal setting exercise in alcohol interventions for this population. More nuanced studies suggest that the specific type of goal (e.g., abstinence vs. drinking reduction) can also impact treatment outcomes. A review (van Amsterdam & van den Brink, 2013) suggested that, while different types of goals may be differentially associated with drinking outcomes, generally both abstinence-oriented (Dunn & Strain, 2013; Meyer, Wapp, Strik, & Moggi, 2014) and reduced-risk (Bujarski et al., 2013) drinking goals can be effective in reducing alcohol use in problem and dependent drinkers.
Drinking goal assessments are most commonly conducted prior to, or at the start of, treatment (Anton et al., 2006; Berger, Brondino, Fisher, Gwyther, & Garbutt, 2016; Bujarski et al., 2013; Copello et al., 2002; DeMartini et al., 2014). Studies examining drinking goals and their prediction of treatment outcomes have shown that roughly half of participants change their drinking goals post-treatment, and that goals set at discharge are more strongly associated with long-term outcomes than goals set at admission (Elal-Lawrence, Slade, & Dewey, 1986, 1987; Meyer et al., 2014). Therefore, one-time assessments of goals at pre-treatment may not adequately capture relations between goal setting and behavior change. Drinking goals may be dynamic as participants may not have a clearly defined goals when entering treatment and may modify or refine their goals during treatment (Ambrogne, 2002; van Amsterdam & van den Brink, 2013). Thus, goals set at different times (e.g., pre-, during, or post-treatment) may be differentially associated with treatment outcomes.
Goal setting theory (Locke & Latham, 1994; Locke & Latham, 2002) suggests that setting difficult or ambitious goals leads to better performance than setting easier, non-challenging goals. Two dimensions, in particular, can influence performance: specificity and difficulty (Locke & Latham, 2006; Webb, Sniehotta, & Michie, 2010). While theory regarding goal setting has focused mainly on educational or job performance (Lee, Locke, & Latham, 1989), setting specific goals, rather than vague, non-quantitative goals, has been identified as a strategy for changing health-related behaviors (Strecher et al., 1995). Various factors, including goal attainment and its impact on subsequent goal setting or treatment outcomes, may contribute to changes in goals over the course of treatment.
While some research suggests that an abstinence goal may be associated with better treatment outcomes than a non-abstinence goal (Adamson, Heather, Morton, Raistrick, & Team, 2010), not all individuals entering alcohol treatment have abstinence as a goal. As noted, this is particularly the case for young adults. Tailoring treatment approaches to individual goals for drinking may promote better outcomes than abstinence-only approaches (Bujarski et al., 2013). Most research on drinking goals in treatment has examined general goals such as “controlled” or “reduced” drinking (Aubin & Daeppen, 2013; Bujarski et al., 2013; Mann, Bladström, Torup, Gual, & van den Brink, 2013; Pachman, Foy, & Van Erd, 1978), with few studies focusing on the specific, participant-selected number of alcoholic beverages consumed as the drinking goal (Al-Otaiba, Worden, McCrady, & Epstein, 2008; Adamson, 2001). To our knowledge, no studies have examined specific, participant-selected drinking goals in young adults, the segment of the population most at risk for alcohol misuse and problems (Center for Behavioral Health Statistics and Quality, 2015) and most likely to prefer non-abstinence goals (Epler et al., 2009).
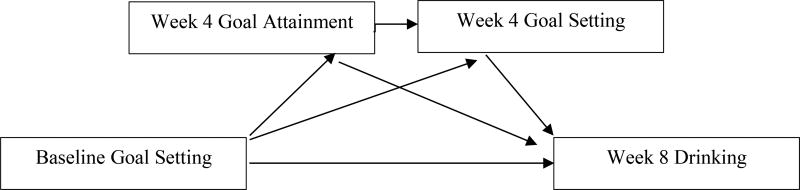
The current study was designed to examine relations among alcohol consumption, goal setting (i.e., specific participant-generated goals regarding drink quantity), and attainment of drinking goals in a sample of young adult heavy drinkers who participated in an 8-week, double-blind, placebo-controlled trial of naltrexone (for full study details see O’Malley et al., 2015). We sought to build an overall, multiple mediation model to examine the dynamic effects of alcohol goal setting and goal attainment on end-of-treatment drinking. We hypothesized that setting a more ambitious drinking goal (i.e., a goal for greater drinking reduction) at baseline would be associated with more goal attainment at mid-treatment; that more goal attainment would be associated with more ambitious drinking goals set at mid-treatment; that better goal attainment and more ambitious goals at mid-treatment would predict less drinking at the end of treatment; and that goal attainment and goal setting at mid-treatment would collectively mediate relations between baseline drinking goal and end-of-treatment drinking (see Figure 1 for model schematic).
Figure 1.
Overall schematic of the serial multiple mediation model of the overall relations among goal attainment, goal setting, and alcohol treatment outcome in a sample of young adult heavy drinkers
Method
Participants and Procedure
Participants were 140 young adult heavy drinkers who were recruited to participate in an 8-week, randomized, placebo-controlled trial of the efficacy and safety of naltrexone (O'Malley et al., 2015). Participants met eligibility criteria if they were: 1) 18–25 years of age; 2) reported at least four heavy drinking days (≥5 drinks in a day for men, ≥4 drinks in a day for women) in the previous four weeks; and 3) exhibited no significant cognitive impairments. Participants were excluded from the study if they had significant psychiatric illness, risk for alcohol withdrawal, medical contraindications, dependence on a drug other than nicotine, or had recently used psychotropic medications other than serotonin reuptake inhibitors or non-benzodiazepine medications for performance anxiety. Participants were not required to be treatment-seeking nor were they required to have any particular level of motivation to change their drinking. Study advertisements used varying language to recruit potential participants including, “Thinking about cutting down… but don’t want to stop?” Thus, while neither a specific level of motivation to change nor an interest in abstinence was required, some ads were framed in terms of an interest in drinking reduction. Participants could receive up to $415 for their participation (see O'Malley et al., 2015). The Human Investigation Committee of REDACTED approved the study protocol. Of the 140 individuals randomized to receive either placebo or naltrexone, 128 (n=61 allocated to naltrexone and n=67 to placebo) began treatment and were included in the main outcome analyses (O’Malley et al., 2015). The 12 participants who were removed were randomized non-starters, did not attend the first session, and did not receive any treatment. As a result, they were considered not evaluable. Power analysis details for the main trial can be found in the original manuscript (see O’Malley et al., 2015).
At baseline, participants met with a therapist with a master’s or doctoral degree in psychology for a brief, personalized, motivational alcohol reduction intervention. The manual for Brief Alcohol Screening and Intervention for College Students (BASICS: Dimeff, Baer, Kivlahan, & Marlatt, 1999; O’Malley, Corbin, Palmer, Leeman, & Romano, 2006) provided the content of the behavioral session, including a discussion of drinking goals. Participants then met with a nurse practitioner who reviewed the use of naltrexone for drinking reduction (O’Malley et al., 2006). Progress toward goals was monitored in subsequent appointments at weeks 4 and 8, during which time drinking goals were re-evaluated. A total of 110 (86%) participants completed all assessments reported in the current study (naltrexone: N=51; placebo: N=59). A full description of participant characteristics and study procedures and the design and overview of the main trial are provided in the primary outcome manuscript (O'Malley et al., 2015).
Measures
Demographics
Participants reported demographic information including sex, age, race, and ethnicity.
Alcohol use
Daily alcohol use was assessed using the Timeline Follow-Back interview (TLFB; Sobell & Sobell, 2000) at baseline for the preceding 30 days and at each subsequent visit (i.e., weeks 4 and 8) to assess alcohol consumption since the previous appointment. A standard drink was defined as a 12-oz beer, 5-oz glass of wine, or a 1.5-oz shot of hard liquor either straight or in a mixed drink, all equivalent to approximately 0.6-oz or 14g of pure alcohol. Peak drinking was the number of drinks consumed on the heaviest day of drinking. Typical drinking was the number of drinks consumed on a typical drinking occasion. Drinking frequency was the number of drinking days per week. Baseline values of each construct were used as model covariates.
Goal setting
Participants were given feedback about their drinking over the prior two weeks using a worksheet that summarized the frequency of drinking days per week, total number of drinks per drinking day, and the peak number of drinks consumed in a day. Based on this information, the nurse practitioner asked participants to set goals for the next two weeks regarding drinking frequency, typical number of drinks on a drinking occasion, and peak drinking (e.g., number of drinks “on your heaviest drinking day”). Drinking goals were set by participants at three assessment points: baseline, week 4, and week 8; participants could adjust their drinking goal at each assessment. Peak drinking goal was the targeted actual number of drinks that the participant stated he/she would consume on his/her heaviest drinking day. Higher drinking goals, therefore, are less ambitious goals; lower goals are more ambitious. Typical drinking goal was the targeted actual number of drinks that the participant stated he/she would consume on a typical drinking day. Frequency drinking goal was the specific number of drinking days the participant stated he/she would drink in the next two weeks.
Goal attainment
Percent goal attainment was calculated at week 4. Percent goal attainment was calculated for each drinking construct: peak drinking, typical drinking, and drinking frequency. For example, week 4 goal attainment was calculated with the following conceptual formula: (actual peak drinking reduction at week 4)/(goal peak drinking reduction at week 4)*100. Mathematically, percent goal attainment was calculated with the following formula: ((baseline peak drinking – week 4 peak drinking)/(baseline peak drinking – week 4 peak drinking goal))*100. This calculation of percent goal attainment ensured that findings would not be driven by a heavier drinker’s ability to reduce his/her drinking by a larger absolute number of drinks.
Contemplation Ladder
Participants were asked to complete a 1-item measure to assess their motivation to change drinking behavior at baseline. Participants were asked to choose “the number that indicates your current thoughts about reducing your alcohol use.” The item was scored from 1 (“no thought of reducing my alcohol use”) to 10 (“taking action to change my alcohol use”). The sample’s mean on the contemplation ladder was 5.20 (SD=2.16) and the range was 1–10. Score on the contemplation ladder was used as a model covariate.
Statistical Analyses
Three serial, multiple mediator models were built via PROCESS (Hayes, 2013) to examine relations among goal setting, goal attainment, and treatment outcome (see Figure 1). One model was built for each of the three alcohol constructs. The goal of the models was to examine both the direct and indirect effects of baseline goal setting on end-of-treatment drinking, while modeling a simultaneous process in which baseline goal setting impacts goal attainment at week 4, which subsequently impacts goal setting at week 4, which impacts end-of-treatment drinking at week 8. The serial, multiple mediation models tested the following hypothesis: baseline goal setting → goal attainment (week 4) → goal setting (week 4) → end-of-treatment alcohol outcome (week 8). In this model, variables that are presumed to be causally prior are modeled as affecting all variables later in the causal sequence. Three specific indirect effects and one direct effect were estimated. All indirect effects were estimated as the product of regression weights linking X to Y through at least one mediator (M). Bootstrapped 95% confidence intervals (5000 iterations; bias-corrected) were calculated for indirect effects. Bias-corrected confidence intervals have been shown to perform best in terms of both power and Type I error rate (cf. Williams & MacKinnon, 2008) and allow a test of the specific and total indirect effects of the models, while also yielding a point estimate of the indirect effect and the SE of the mediation effect (Preacher & Hayes, 2008). To control for the potential impact of motivation, baseline alcohol consumption, and treatment condition on these paths, the model included baseline contemplation ladder (i.e., motivation to change drinking) score, medication condition, and the baseline drinking value for each construct (i.e., baseline peak drinking was a covariate for the peak drinking goal model) as covariates.
Additional exploratory analyses were also conducted after all PROCESS models were complete. These exploratory analyses sought to assess whether there were any baseline participant characteristics that were associated with changes in drinking goals during treatment. Correlations and one-way ANOVAs were used to conduct these post-hoc analyses.
Results
Sample Description
A complete description of participants enrolled in the trial, including a CONSORT diagram, has been published (DeMartini et al., 2016; O'Malley et al., 2015). Briefly, the sample was, on average, 21.45 years old (SD=2.15), 77% white, and 69% male; 71% were current students and 79% met criteria for current alcohol abuse or dependence. At baseline, they reported drinking heavily on 33.8% (SD=15.2) of days and had an average of 11.02 drinks (SD=4.39) on their heaviest drinking (peak) day in the prior 2 weeks. Participants set an average peak drinking goal of 7.95 (SD=4.39) drinks per peak occasion (see Table 1). Individuals with missing data (n=13 at week 4; n=18 at week 8) and those with no missing data did not differ significantly at baseline on peak drinking (p=0.43) or frequency of heavy drinking (p=0.35).
Table 1.
Means and standard deviations of drinking goals, percent drinking goal attainment, and actual drinking consumption and frequency at baseline, week 4, and week 8.
| Baseline | Week 4 | Week 8 | |
|---|---|---|---|
| Peak Drinking | 11.02 (4.39) | 8.52 (4.85) | 6.82 (4.50) |
| Peak Goal Set | 7.95 (3.14) | 6.97 (2.72) | 6.32 (2.51) |
| % Peak Goal Attainment | -- | 0.59 (1.38) | 0.76 (1.30) |
| Typical Drinking | 6.36 (2.68) | 5.12 (2.87) | 4.45 (2.81) |
| Typical Goal Set | 4.91 (2.04) | 4.42 (1.83) | 4.01 (1.54) |
| % Typical Goal Attainment | -- | 0.61 (1.06) | 0.73 (0.96) |
| Drinking Frequency | 7.34 (2.71) | 5.50 (2.73) | 4.75 (3.00) |
| Frequency Goal Set | 5.59 (2.03) | 5.05 (1.89) | 4.56 (1.84) |
| % Frequency Goal Attainment | -- | 0.72 (1.02) | 1.04 (1.15) |
Note. Drinking frequency reflects the number of drinking days per week.
Serial Multiple Mediator Models
Three PROCESS serial, multiple mediator models were used to examine the direct effect of baseline goal setting on 3 different week 8 treatment outcomes: (1) peak drinking, (2) typical drinks per drinking day, and (3) drinking frequency. The models assessed the effect of baseline goals on treatment outcomes through mid-treatment goal attainment and goal setting at week 4 (see Figure 1).
In each model, a subset of participants reported that they did not want to change their drinking. For these participants, the denominator of the goal attainment formula was 0, and therefore the formula was undefined and incalculable. Twenty participants (6 females and 14 males) reported that they did not want to make any changes to their peak drinking. Twenty participants (6 females, 14 males) reported that they did not want to make any changes to their typical drinking. Sixteen participants (4 females, 12 males) reported that they did not want to change their drinking frequency. Because it was not possible to calculate goal attainment accurately for these participants, they were removed from the analyzable sample for their respective treatment outcome (e.g., participants who reported a goal of no change on peak drinking were removed from the specific peak drinking analysis). To examine differences between participants who reported a goal of no change and those who reported change goals, we compared the groups on baseline measures including age, gender, motivation for change (contemplation ladder), alcohol-related consequences, direct and indirect protective behavioral strategies, drinking motives, and additional measures of pre-trial alcohol consumption. We did this for each of the three treatment outcomes (e.g., participants who reported no change goal for peak drinking, participants who reported no change goal for drinking frequency). Participants who reported no peak drinking change goal were younger (M=20.30 (SD=1.99) vs M=21.62 (SD=2.14) (t(126)= −2.17, p<0.05)) and reported lower motivation to change (M=4.20 (SD=1.91) vs M=5.38(SD=2.17) (t(126)= −2.28, p<0.05)) than those who had a peak drinking change goal. Participants who reported no typical drinking change goal reported a lower percent of heavy drinking days (M=26.17 (SD=12.62) vs M=35.26(SD=15.23) (t(126)= −2.51, p<0.05)) than those who had a goal for typical drinking. For drinking frequency, there were significant group differences for percent days abstinent in the 30 days before intake (t(126)= 2.53, p<0.05), total drinks consumed in the 30 days before intake (t(126)= −2.07, p<0.05), and percent heavy drinking days in the 30 days before intake (t(126)= −2.17, p<0.05). Participants who reported no drinking frequency change goal had higher percent days abstinent (M=57.29 (SD=16.52) vs M=45.00(SD=18.43)), fewer total drinks (M=80.25 (SD=34.31) vs M=108.48(SD=52.98)), and a lower percentage of heavy drinking days (M=26.25 (SD=10.17) vs M=34.92(SD=15.49).
Peak Drinking
A PROCESS serial, multiple mediator model was used to examine the direct effect of baseline goal setting on week 8 peak drinking and the indirect effects of baseline goal setting on week 8 peak drinking through goal attainment and goal setting at week 4 (see Table 2). Baseline contemplation ladder and baseline peak drinking were model covariates. Per best practice recommendations for the assessment and comparison of indirect effects in a multiple mediator model (Preacher & Hayes, 2008), testing model results involved two parts. First, we examined whether the set of mediators together transmitted the effect of baseline goal setting to the week 8 treatment outcome of peak drinking (Preacher & Hayes, 2008). For peak drinking, the total indirect effect of the mediator set was significant (b= 0.87, Bootstrapped SE=0.25, 95%CI: 0.40, 1.37). Therefore, goal attainment and goal setting at week 4 collectively mediated the effect of baseline goal setting on peak drinking at week 8. The total effects (i.e., sum of all indirect paths plus direct path from baseline to outcome) of the model were also significant (b= 0.66, Bootstrapped SE=0.20, p<0.01, 95%CI: 0.25, 1.06). To assess the directionality of the set of mediators, the directions of the a paths (i.e., the beta weights of the paths from baseline goal setting to each mediator) and b paths (i.e., the beta weights from the mediators to the outcome) were examined. The directions of the a paths were different for each construct: (1) negative for attainment (b = −0.05, SE = 0.07) and (2) positive for goal setting (b = 0.74, SE = 0.07). More ambitious baseline goals (i.e., low number of drinks set as the goal) were associated with higher levels of attainment and with more ambitious goals at week 4. The directions of effects were the same for the b paths: (1) negative for attainment to peak drinking (b = −0.55, SE = 0.29) and (2) positive for goal setting to peak drinking (b = 1.13, SE = 0.27). The relationship between week 4 goal attainment and week 4 goal setting was also negative (b = −0.18, SE = 0.10). Taken together, these results suggest that a more ambitious baseline peak drinking goal leads to higher goal attainment and another ambitious goal at week 4; greater attainment at week 4 leads to lower peak drinking at week 8 while less ambitious goals at week 4 are associated with higher levels of peak drinking at week 8.
Table 2.
Mediation of the effect of baseline goal setting on end-of-treatment peak drinking through mid-treatment goal setting and goal attainment
| Bootstrapping | |||
|---|---|---|---|
|
|
|||
| BC 95% CI | |||
|
|
|||
| b (SE) | Lower | Upper | |
| Goal Attainment | 0.03 (0.04) | −0.45 | 0.13 |
| Goal Setting | 0.84 (0.24) | 0.39 | 1.32 |
| Attainment and Goal Setting | 0.01 (0.02) | −0.01 | 0.08 |
| Total Indirect Effect | 0.87 (0.25) | 0.40 | 1.37 |
Note. BC = bias-corrected.
Next, we examined the specific indirect effect pathways. Importantly, in a multiple mediator model, the specific effect of a mediator is conditional on the presence of the other mediator (Preacher & Hayes, 2008). The three specific paths are: (a) the indirect path from baseline goal setting through week 4 goal attainment to week 8 drinking; (b) the indirect path from baseline goal setting through week 4 goal setting to week 8 drinking; (c) the indirect path from baseline goal setting through week 4 goal attainment and week 4 goal setting to week 8 drinking. The indirect path through week 4 goal attainment to week 8 drinking was not significant (b=0.03, 95%CI: −0.05–0.13.). In contrast, the indirect effect of baseline goal setting through week 4 goal setting to week 8 drinking was significant (b=0.84, 95%CI: 0.39–1.32). The indirect effect of baseline drinking through week 4 goal attainment and week 4 goal setting to week 8 drinking was not significant (b=0.01, 95%CI: −0.01–0.08). Contrasts comparing the specific indirect effects showed that the indirect effect through goal setting was significantly larger than the path through goal attainment (b=−0.81, Bootstrapped 95%CI: −1.30– −0.39) and the path through both mediators (b=−0.83, Bootstrapped 95%CI: −1.31– −0.37).
Typical Drinking
As with the peak drinking model, model effects were examined by first assessing whether the set of mediators transmitted the effect of baseline goal setting to week 8 typical drinking (Preacher & Hayes, 2008). The total indirect effect of the mediator set was not significant (b = 0.28, Bootstrapped 95%CI: −0.08–0.78). Therefore, the combination of mid-treatment goal setting and goal attainment did not mediate the relationship between baseline goal setting and typical drinking at week 8.
Next, we examined the specific indirect effect pathways. The same three paths detailed in the peak drinking model were examined for typical drinking. The results replicated the peak drinking model. The indirect effect of baseline goal setting through week 4 goal setting to week 8 drinking was significant (b=0.35, Bootstrapped 95%CI: 0.10–0.85). The indirect paths through week 4 goal attainment (b=−0.06, Bootstrapped 95%CI: −0.31–0.13), and week 4 goal attainment and goal setting (b=−0.004, Bootstrapped 95%CI: −0.04–0.005), were not significant. Therefore, goal setting at mid-treatment operated as the sole mediator of the relationship between baseline goal setting and typical drinking outcome. To understand the directionality, the coefficients of the a and b paths were examined. More ambitious goals (i.e., low total number of drinks) at baseline were associated with a subsequent ambitious goal at week 4 (b = 0.61, SE = 0.07), and more ambitious goals at week 4 were associated with lower levels of typical drinking at week 8 (b = 0.57, SE = 0.24). Taken together, these results indicate that setting an ambitious goal at baseline leads to subsequent ambitious goals, and that these goals ultimately lead to a better treatment outcome.
Drinking Frequency
Model effects were examined using the same approach discussed for peak and typical drinking (Preacher & Hayes, 2008). For drinking frequency, the total indirect effect of the set of mediators was significant (b = 0.66, Bootstrapped SE=0.17, 95%CI: 0.37, 1.06). Therefore, taken as a set, goal attainment and goal setting at week 4 significantly mediated the effect of baseline goal setting on drinking frequency at week 8. Regarding the directions of the mediators, the directions of the a paths (i.e., the beta weights of the paths from baseline goal setting to each mediator) were: (1) positive for attainment (b=0.06, SE = 0.09) and (2) positive for goal setting (b=0.56, SE = 0.08). The direction of the path between week 4 goal attainment and week 4 goal setting was negative (b = −0.16, SE = 0.09). The directions of the b paths (i.e., the beta weights from the mediators to the outcome) were: (1) positive for attainment (b=0.02, SE = 0.23) and (2) positive for goal setting (b=1.19, SE = 0.26). Taken together, these results indicate that a more ambitious baseline drinking frequency goal (i.e., lower total drinking days) was associated with lower goal attainment and another ambitious goal at week 4; greater attainment at week 4 led to a more ambitious drinking goal at week 4; and more ambitious drinking goals at week 4 led to less drinking at week 8.
Next, we examined the specific indirect effects. The results replicated those of the peak drinking and typical drinking models. The indirect effect of baseline goal setting through week 4 goal setting was significant (b=0.67, Bootstrapped 95%CI: 0.39–1.07). Indirect paths through week 4 goal attainment (b=0.002, Bootstrapped 95%CI: −0.04–0.05), and week 4 goal attainment and goal setting (b=−0.01, Bootstrapped 95%CI: −0.05–0.005), were not significant. Contrasts comparing the specific indirect effects showed that the indirect effect through goal setting was significantly larger than the paths through goal attainment (b=−0.67, Bootstrapped 95%CI: −1.06– −0.38) and through both mediators (b=−0.68, Bootstrapped 95%CI: −1.09– −0.39).
Associations with Changes in Drinking Goal Setting
Given the clear importance of the goal setting construct in the models detailed above, we sought to understand whether participants’ baseline characteristics were associated with their level of goal change between baseline and week 4 and between baseline and week 8 (see Table 1). Two types of change scores were created for goal setting: 1) week 4 goal change and 2) week 8 goal change. To create week 4 goal change for the three drinking outcomes, we subtracted week 4 goal from baseline goal for each outcome. To create week 8 goal change for all three outcomes, we subtracted week 8 goal from baseline goal. Therefore, drinking goals for each outcome had two change scores.
Week 4
Correlations and one-way ANOVAs assessed relationships between baseline participant characteristics and the week 4 drinking goal change variables. Changes in peak drinking goal were associated with weight (r=0.21, p<0.05) and lifetime 24-hour maximum alcohol consumption (r=0.24, p<0.01). Higher weight and higher lifetime maximum were associated with a less ambitious goal change. Changes in typical drinking goal were associated with age (r=−0.25, p<0.01). Older age was associated with more ambitious goal changes. Changes in drinking frequency goals were not associated with any baseline construct. Notably, none of the change scores were associated with gender (peak: F(1,110)=0.20, p=0.65; typical: F(1,110)=0.77, p=0.38; frequency: F(1,110)=0.02, p=0.89) or any baseline drinking variables (all ps > 0.05).
Week 8
Correlations and one-way ANOVAs assessed relationships between baseline participant characteristics and the week 8 drinking goal change variables. Changes in peak drinking goal were associated with weight (r=0.22, p<0.05) and lifetime 24-hour maximum alcohol consumption (r=0.30, p<0.01). Again, higher weight and higher lifetime maximum consumption were associated with a less ambitious goal change. Changes in typical drinking goal were associated with age (r=−0.29, p<0.01); older participants had more ambitious goal changes. Changes in drinking frequency goals were not associated with any baseline construct. Only changes in typical drinking goal setting were associated with baseline drinking. Changes in typical drinking goals were associated with baseline peak drinking (r=0.33, p<0.001) and typical drinking (r=0.42, p<0.001) but not with drinking frequency (r=−0.11, p=0.24). Higher levels of consumption, demonstrated by higher peak and typical drinking, were associated with less ambitious goal changes.
Discussion
The present study examined effects of goal setting and goal attainment on multiple alcohol treatment outcomes in a sample of young adult heavy drinkers randomized to receive 8 weeks of treatment with naltrexone or placebo. Consistent with our hypotheses, mid-treatment goal setting and goal attainment collectively accounted for relations between baseline goal setting and week 8 peak drinking and drinking frequency. Although the combination of mid-treatment goal setting and goal attainment did not significantly mediate the effect of baseline goal setting on week 8 typical drinking, goal setting at mid-treatment was a significant mediator on its own. Moreover, in all 3 models, the indirect path through mid-treatment goal setting was significant, highlighting the particular importance of this pathway. Again consistent with our hypotheses, across drinking outcomes, participants with more ambitious mid-treatment goals reported lower drinking levels at week 8. Therefore, dynamic cognitive processes during treatment were associated with treatment outcomes.
We hypothesized that ambitious goals at baseline would be associated with subsequent, ambitious drinking goals. Our findings were consistent with this hypothesis. As noted, the indirect pathway from baseline goal setting through week 4 goal setting to alcohol treatment outcome was significant across models. Participants who set ambitious goals at baseline then set subsequent ambitious drinking goals at week 4. Ambitious goals at week 4 were then associated with decreased drinking at week 8. These findings highlight the importance of assessing treatment goals during treatment, even in a sample of participants who are not necessarily seeking treatment for their alcohol consumption. These results suggest that ultimate treatment success may be predicated upon setting ambitious, realistic goals throughout treatment.
Indeed, key moderators of goal effects are goal importance, goal commitment, and feedback (Locke & Latham, 2002). Goal performance has been demonstrated to be the strongest when people are committed to their goals and making public commitments to goals enhances that commitment (Locke & Latham, 2002; Hollenbeck, Williams, & Klein, 1989). The BASICS intervention allows the creation of a space to discuss personal drinking goals and state them verbally to a counselor, and also in the case of the intervention for this study, to an advanced practice registered nurse. Thus, participants in this trial were asked to publically state their drinking goals and do so repeatedly. It is likely that this practice enhanced commitment to these goals and engendered participants’ own sense of the importance of their personal goals. Of particular importance, our study provided feedback on participants’ progress toward their goals. Typical, single-session interventions for young adults and college students are unable to provide this feedback. Following participants for longer than a single session created an opportunity for participants to assess their feedback and decide how to proceed. Given that participants who set ambitious goals at baseline were more likely to set additional ambitious goals, this feedback could have increased their motivation to continue to reduce their drinking.
We hypothesized that the set of cognitive constructs (i.e., goal setting and goal attainment) would mediate the relationship between baseline goals and treatment outcomes. We found partial support for this hypothesis: in two of the three multiple mediation models, the set of mediators significantly mediated the relationship between baseline goals and treatment outcome. Therefore, while only the specific path through goal setting was statistically significant, the constructs together facilitated the mediation. It is important to note that the relationship between goal attainment and goal setting was negative in both the peak drinking and drinking frequency models (i.e., the models with significant total indirect effects). Higher levels of goal attainment were associated with more ambitious mid-treatment goals; across models, more ambitious goals at mid-treatment were associated with better treatment outcomes. Consistent with our hypotheses, the results of the peak drinking model found that higher levels of goal attainment at mid-treatment were associated with more ambitious week 4 goals and with lower levels of drinking at week 8. In contrast, the direction of the relationship of goal attainment with drinking frequency was positive; higher levels of goal attainment had a positive relationship with drinking frequency. In this case, however, the beta weight for the relationship between attainment and outcome was very close to zero. In summary, while goal setting and goal attainment collectively mediated the relationship between baseline goals and drinking frequency, goal setting was clearly the stronger mediator.
We were also able to compare differences between participants who specified a change goal versus participants who did not. Participants who did not select a change goal tended to be younger and reported less drinking than those who set a change goal. It is noteworthy that, while participants who did not set a change goal drank less than others, they still met criteria for inclusion in a trial of heavy drinking young adults and reported at least 4 heavy drinking episodes in the 4 weeks prior to baseline. It could be, then, that these participants have overestimated the prevalence of heavy drinking among other young adults and/or perceive that heavy drinking is acceptable in their peer groups. It is known that perceived prevalence (i.e., descriptive norms) of drinking is associated with one’s own personal drinking. College students who overestimate the prevalence of drinking report higher drinking levels (see Lewis & Neighbors, 2004; Thombs, Ray-Tomasek, Osborn, & Olds, 2005). Moreover, college students who perceive increased approval of heavy drinking by their own friends report higher levels of alcohol consumption (Neighbors, O’Connor, Lewis, Chawla, Lee, & Fossos, 2008). College students who incorporate more heavy drinkers into their social networks also increase their drinking over time (DeMartini, Prince, & Carey, 2013). Students who perceive their networks to be accepting of heavy drinking could be uninterested in making changes to their own drinking.
This project is the first, to our knowledge, to specifically examine the effects of dynamic, mid-treatment cognitive processes on goal setting and achievement in young adult heavy drinkers. Studies on drinking goals usually examine only positive drinking goals in patients diagnosed with alcohol dependence (see DeMartini et al., 2014), and studies on college students and specifically, college students mandated to treatment, typically only assess changes in actual drinking across all participants irrespective of baseline desire to change (see Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Carey, Scott-Sheldon, Garey, Elliott, & Carey, 2016). Our results suggest that goal setting and goal attainment are important to consider in and of themselves. The effects of these cognitive processes on treatment outcomes may reflect more universal cognitive processes that exist during treatment, regardless of a participant’s initial interest in making a behavioral change.
There are several clinical implications of these findings. First, careful consideration of goals at treatment onset is warranted, particularly because the initial goal may influence subsequent goals and, ultimately, treatment outcome. Second, the attainment of goals should be monitored and encouraged over time, as goal attainment has been shown to be associated with better drinking outcomes following treatment (Adamson et al., 2010). Third, monitoring of on-going goal setting and goal attainment during treatment may be a clinically important methodology to understand patient progress and help achieve better treatment outcomes. Providing participants with the support and skills needed to achieve early ambitious goals appears to lead to additional, ambitious goals to reduce drinking, which ultimately were associated with lower drinking levels at the end of treatment.
These findings should be considered in light of the study’s limitations. Although eligibility criteria did not include motivation to reduce drinking, motivation and confidence, and changes therein, may have influenced goal setting and subsequent performance. While the present work controlled for baseline motivation, subsequent studies might examine how changes in motivation and alcohol refusal self-efficacy influence goal setting, goal attainment and subsequent treatment outcome. In particular, multiple assessments of motivation and goal setting and attainment would allow for a more fine-grained analysis or multi-group analysis of these interactive processes. Similarly, the use of a multi-item motivation to change scale might provide more specific information regarding how goals change differentially for participants in different stages of the change process. Further, the assessments of peak drinking were self-reports, and could have been influenced by bias, problems with recollection, and demand characteristics. Further, the majority of the sample was white and male, which limits generalizability. Thus, replication of this work is needed in more diverse samples. Additionally, the present study included the construct of goal attainment, which has yet to be examined extensively or included in standard treatment. Thus, an investigation of the utility of this construct in a treatment setting is warranted. As goal setting theory posits that the attainment of goals is influenced in part by the presence of conflicting goals (Locke & Latham, 1994), further work is needed to learn more about conflicting goals that young adults may hold in regard to alcohol consumption. It is possible that, in this group, peer influences and strong expectancies for positive outcomes of drinking interfere with goal setting or with progress towards alcohol reduction.
In conclusion, the results of current study suggest that cognitive processes during treatment play a significant role in predicting treatment outcome. Multiple assessments of goal attainment and goal setting during treatment for all participants may be an important and novel method to track clinical progress and to facilitate better overall treatment outcomes for young adult heavy drinkers.
Table 3.
Mediation of the effect of baseline goal setting on end-of-treatment typical drinking through mid-treatment goal setting and goal attainment
| Bootstrapping | |||
|---|---|---|---|
|
|
|||
| BC 95% CI | |||
|
|
|||
| b (SE) | Lower | Upper | |
| Goal Attainment | −0.06 (0.11) | −0.31 | 0.13 |
| Goal Setting | 0.35 (0.17) | 0.10 | 0.85 |
| Attainment and Goal Setting | −0.00 (0.01) | −0.04 | 0.00 |
| Total Indirect Effect | 0.28 (0.21) | −0.08 | 0.78 |
Note. BC = bias-corrected.
Table 4.
Mediation of the effect of baseline goal setting on end-of-treatment drinking frequency through mid-treatment goal setting and goal attainment
| Bootstrapping | |||
|---|---|---|---|
|
|
|||
| BC 95% CI | |||
|
|
|||
| b (SE) | Lower | Upper | |
| Goal Attainment | 0.00 (0.02) | −0.04 | 0.05 |
| Goal Setting | 0.67 (0.17) | 0.39 | 1.07 |
| Attainment and Goal Setting | −0.01 (0.01) | −0.05 | 0.00 |
| Total Indirect Effect | 0.66 (0.17) | 0.37 | 1.06 |
Note. BC = bias-corrected.
Public Health Significance.
Young adult heavy drinkers who set more ambitious goals to reduce their drinking were more likely to set subsequent, ambitious drinking goals and were more likely to have reduced drinking at the end of 8 weeks of alcohol treatment. Goal attainment and goal setting during alcohol treatment are important predictors of ultimate alcohol treatment outcomes. Inclusion of multiple drinking goal assessments and evaluation of young adults’ ability to meet those goals may be important for understanding treatment outcomes among heavy drinking young adults.
Acknowledgments
Dr. Kranzler has been a consultant, advisory board member, and a CME speaker for Alkermes and an advisory board member for Alkermes. He is a member of the American Society of Clinical Psychopharmacology’s Alcohol Clinical Trials Initiative (ACTIVE), which in the last three years was supported by AbbVie, Alkermes, Amygdala Neurosciences, Arbor, Ethypharm, Indivior, Lilly, Lundbeck, Otsuka, and Pfizer.
Dr. O’Malley reports the following activities for the past 12 months: Member of the American Society of Clinical Psychopharmacology workgroup, the Alcohol Clinical Trials Initiative, supported with funding from Amygdala, Arbor Pharmaceuticals, Ethypharma, Lundbeck, Otsuka, and Indivior; donated study medications, Pfizer Pharmaceuticals, Astra Zeneca, Novartis; Consultant/Advisory Board Member, Alkermes, Indivior, Opiant, Mitsubishi Tanabe.
This article received grant funding from the NIAAA, grant numbers P50 AA012870 and R01 AA016621-01.
References
- Adamson SJ, Simon SD. Drinking goal selection and treatment outcome in out-patients with mild—moderate alcohol dependence. Drug and Alcohol Review. 2001;20(4):351–359. [Google Scholar]
- Adamson SJ, Heather N, Morton V, Raistrick D. Initial preference for drinking goal in the treatment of alcohol problems: II. Treatment outcomes. Vol. 45. United Kingdom: Oxford University Press; 2010. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. Alcoholism: Developing Drugs for Treatment Guidance for Industry. Silver Spring, MD: Center for Drug Evaluation and Research (CDER); 2015. [Google Scholar]
- Al-Otaiba Z, Worden BL, McCrady BS, Epstein EE. Accounting for self-selected drinking goals in the assessment of treatment outcome. Psychology of Addictive Behaviors. 2008;22(3):439. doi: 10.1037/0893-164X.22.3.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JP. Measuring outcome in interventions for alcohol dependence and problem drinking: executive summary of a conference sponsored by the national institute on alcohol abuse and alcoholism. Alcoholism: Clinical and experimental research. 2003;27(10):1657–1660. doi: 10.1097/01.ALC.0000091223.72517.13. [DOI] [PubMed] [Google Scholar]
- Ambrogne JA. Reduced-risk drinking as a treatment goal: what clinicians need to know. Journal of substance abuse treatment. 2002;22(1):45–53. doi: 10.1016/s0740-5472(01)00210-0. [DOI] [PubMed] [Google Scholar]
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Aubin HJ, Daeppen JB. Emerging pharmacotherapies for alcohol dependence: a systematic review focusing on reduction in consumption. Drug and Alcohol Dependence. 2013;133(1):15–29. doi: 10.1016/j.drugalcdep.2013.04.025. [DOI] [PubMed] [Google Scholar]
- Berger L, Brondino M, Fisher M, Gwyther R, Garbutt JC. Alcohol Use Disorder Treatment: The Association of Pretreatment Use and the Role of Drinking Goal. The Journal of the American Board of Family Medicine. 2016;29(1):37–49. doi: 10.3122/jabfm.2016.01.150143. [DOI] [PubMed] [Google Scholar]
- Bujarski S, O'Malley SS, Lunny K, Ray LA. The effects of drinking goal on treatment outcome for alcoholism. Journal of Consulting and Clinical Psychology. 2013;81(1):13. doi: 10.1037/a0030886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32(11):2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Garey L, Elliott JC, Carey MP. Alcohol interventions for mandated college students: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2016;84(7):619. doi: 10.1037/a0040275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. 2015 Retrieved from http://www.samhsa.gov/data/
- Copello A, Orfor J, Hodgson R, Tober G, Barrett C UKATT Research Team. Social behaviour and network therapy basic principles and early experiences. Addictive Behaviors. 2002;27(3):345–366. doi: 10.1016/s0306-4603(01)00176-9. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Devine EG, DiClemente CC, Martin DJ, Ray LA, O'Malley SS. Predictors of pretreatment commitment to abstinence: results from the COMBINE study. Journal of Studies on Alcohol and Drugs. 2014;75(3):438–446. doi: 10.15288/jsad.2014.75.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMartini KS, Gueorguieva R, Leeman RF, Corbin WR, Fucito LM, Kranzler HR, O'Malley SS. Longitudinal findings from a randomized clinical trial of naltrexone for young adult heavy drinkers. Journal of Consulting and Clinical Psychology. 2016;84(2):185–190. doi: 10.1037/ccp0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMartini KS, Prince MA, Carey KB. Identification of trajectories of social network composition change and the relationship to alcohol consumption and norms. Drug and Alcohol Dependence. 2013;132(1–2):309–315. doi: 10.1016/j.drugalcdep.2013.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. New York: The Guilford Press; 1999. [Google Scholar]
- Dunn KE, Strain EC. Pretreatment alcohol drinking goals are associated with treatment outcomes. Alcoholism: Clinical and Experimental Research. 2013;37(10):1745–1752. doi: 10.1111/acer.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elal-Lawrence G, Slade PD, Dewey ME. Predictors of outcome type in treated problem drinkers. Journal of Studies on Alcohol. 1986;47(1):41–47. doi: 10.15288/jsa.1986.47.41. [DOI] [PubMed] [Google Scholar]
- Elal-Lawrence G, Slade PD, Dewey ME. Treatment and follow-up variables discriminating abstainers, controlled drinkers and relapsers. Journal of Studies on Alcohol. 1987;48(1):39–46. doi: 10.15288/jsa.1987.48.39. [DOI] [PubMed] [Google Scholar]
- Epler AJ, Sher KJ, Loomis TB, O'Malley SS. College student receptiveness to various alcohol treatment options. Journal of American College Health. 2009;58(1):26–32. doi: 10.3200/JACH.58.1.26-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- Hollenbeck JR, Williams CR, Klein HJ. An empirical examination of the antecedents of commitment to difficult goals. Journal of Applied Psychology. 1989;74(1):18. [Google Scholar]
- Jackson KM, Sher KJ, Gotham HJ, Wood PK. Transitioning into and out of large-effect drinking in young adulthood. Journal of Abnormal Psychology. 2001;110(3):378–391. doi: 10.1037//0021-843x.110.3.378. [DOI] [PubMed] [Google Scholar]
- Lee TW, Locke EA, Latham GP. Goal setting theory and job performance 1989 [Google Scholar]
- Lewis MA, Neighbors C. Gender-specific misperceptions of college student drinking norms. Psychology of Addictive Behaviors. 2004;18:334–339. doi: 10.1037/0893-164X.18.4.334. [DOI] [PubMed] [Google Scholar]
- Locke E, Latham G. Goal-setting theory. Organizational Behavior 1: Essential Theories of Motivation and Leadership. 1994:159–183. [Google Scholar]
- Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. American psychologist. 2002;57(9):705. doi: 10.1037//0003-066x.57.9.705. [DOI] [PubMed] [Google Scholar]
- Locke EA, Latham GP. New directions in goal-setting theory. Current directions in psychological science. 2006;15(5):265–268. [Google Scholar]
- Mann K, Bladström A, Torup L, Gual A, van den Brink W. Extending the treatment options in alcohol dependence: a randomized controlled study of as-needed nalmefene. Biological Psychiatry. 2013;73(8):706–713. doi: 10.1016/j.biopsych.2012.10.020. [DOI] [PubMed] [Google Scholar]
- Meyer A, Wapp M, Strik W, Moggi F. Association between drinking goal and alcohol use one year after residential treatment: a multicenter study. Journal of addictive diseases. 2014;33(3):234–242. doi: 10.1080/10550887.2014.950025. [DOI] [PubMed] [Google Scholar]
- Neighbors C, O'Connor RM, Lewis MA, Chawla N, Lee CM, Fossos N. The relative impact of injuctive norms on college student drinking: the role of reference group. Psychology of Addictive Behaviors. 2008;22(4):576–581. doi: 10.1037/a0013043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley SS, Corbin WR, Leeman RF, DeMartini KS, Fucito LM, Ikomi J, Romano DM, Wu R, Toll BA, Sher KJ, Gueorguieva R. Reduction of alcohol drinking in young adults by naltrexone: a double-blind, placebo-controlled, randomized clinical trial of efficacy and safety. Journal of Clinical Psychiatry. 2015;76(2):e207–213. doi: 10.4088/JCP.13m08934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley S, Corbin W, Palmer R, Leeman R, Romano D. Manual for Combining Naltrexone with BASICS for the Treatment of Heavy Alcohol Use in Adults. New Haven, CT: Yale University School of Medicine; 2006. [Google Scholar]
- Pachman JS, Foy DW, Van Erd M. Goal choice of alcoholics: a comparison of those who choose total abstinence vs. those who choose responsible, controlled drinking. Journal of Clinical Psychology. 1978;34(3):781–783. doi: 10.1002/1097-4679(197807)34:3<781::aid-jclp2270340343>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Plant RW, O'Malley S. Initial motivations for alcohol treatment: Relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors. 1995;20(3):279–297. doi: 10.1016/0306-4603(94)00072-7. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Carey KB, Elliott JC, Garey L, Carey MP. Efficacy of alcohol interventions for first-year college students: a meta-analytic review of randomized controlled trials. Journal of consulting and clinical psychology. 2014;82(2):177. doi: 10.1037/a0035192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS. Alcohol use disorders among US college students and their non-college-attending peers. Archives of General Psychiatry. 2005;62(3):321–327. doi: 10.1001/archpsyc.62.3.321. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol Timeline Followback (TLFB) In: A. P. Association, editor. Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000. pp. 477–479. [Google Scholar]
- Strecher VJ, Seijts GH, Kok GJ, Latham GP, Glasgow R, DeVellis B, Meertens RM, Bulger DW. Goal setting as a strategy for health behavior change. Health Education & Behavior. 1995;22(2):190–200. doi: 10.1177/109019819502200207. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2010 National Survey on Drug Use and Health: Summary for National Findings. Rockville, MD: Substace Abuse and Mental Health Services Administration; 2011. (NSDUH Series H-41, HHS Publication No. SMA 11-4658) [Google Scholar]
- Suffoletto B, Kristan J, Monti P, Clark D. Pre-weekend goals to limit drinking predicts fewer weekend binge episodes among young adults with problem drinking. Alcoholism: Clinical & Experimental Research. 2014;38:128A. [Google Scholar]
- Thombs DL, Ray-Tomasek J, Osborn CJ, Olds RS. The role of sex-specific normative beliefs in undergraduate alcohol use. Americal Journal of Health Behavior. 2005;29:342–351. doi: 10.5993/ajhb.29.4.6. [DOI] [PubMed] [Google Scholar]
- van Amsterdam J, van den Brink W. Reduced-risk drinking as a viable treatment goal in problematic alcohol use and alcohol dependence. Journal of Psychopharmacology. 2013;27(11):987–997. doi: 10.1177/0269881113495320. [DOI] [PubMed] [Google Scholar]
- Webb TL, Sniehotta FF, Michie S. Using theories of behaviour change to inform interventions for addictive behaviours. Addiction. 2010;105(11):1879–1892. doi: 10.1111/j.1360-0443.2010.03028.x. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the US Preventive Services Task Force. Annals of Internal Medicine. 2004;140(7):557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Williams J, MacKinnon DP. Resampling and distribution of the product methods for testing indirect effects in complex models. Structural Equation Modeling. 2008;15:23–51. doi: 10.1080/10705510701758166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood RE, Mento AJ, Locke EA. Task complexity as a moderator of goal effects: A meta-analysis. Journal of Applied Psychology. 1987;72(3):416. [Google Scholar]