Abstract
Objective:
One of the most prevalent and distressing symptoms following breast cancer treatment is menopausal symptoms. Asian American breast cancer survivors have lower quality of life and often receive inadequate management of menopausal symptoms compared to other racial/ethnic groups. Technology-based programs could be a solution to fill the gap in care. The purpose of this study was to test the efficacy of a technology-based information and coaching/support program on menopausal symptoms of Asian American breast cancer survivors.
Methods:
This study adopted a randomized pretest/posttest group design among 91 Asian American breast cancer survivors (42 in an intervention group who used the program and the American Cancer Society [ACS] website and 49 in a control group who used only the ACS website). The intervention was a theory-driven and culturally tailored intervention program that aimed to provide information and coaching/support using computers and mobile devices. Multiple instruments were used to measure background characteristics and menopausal symptoms at pre-test, post 1-month, and post 3-months. An intent-to-treat linear mixed-model growth curve analysis was used to analyze the data.
Results:
The intervention group showed a significant decrease in the distress scores of menopausal symptoms over time: physical (β = −0.07, p = 0.08), psychological (β = −0.13, p = 0.05), psychosomatic (β = −0.17, p = 0.06), and total symptoms (β = −0.19, p = 0.01). Theory-based variables including attitudes, social influences and self-efficacy partially mediated the impact of the intervention on the distress scores of menopausal symptoms (p < 0.10).
Conclusions:
The program was effective in alleviating menopausal symptoms of Asian American breast cancer survivors.
Keywords: technology-based intervention, menopause, symptoms, Asian American, breast cancer, survivors
Introduction
Due to advances in early detection and treatment, breast cancer survivors represent nearly 70% of the 5.6 million female cancer survivors in the U.S.1–3 These women usually have combinations of surgery, radiation, chemotherapy, or endocrine therapy, all of which could result in clinically significant symptoms including menopausal symptoms. Indeed, about 60% to 100% of breast cancer survivors reportedly experience at least one menopausal symptom.4
Chemotherapy could result in temporary or permanent ovarian failure and subsequent premature menopause in pre-menopausal women, and endocrine therapy could worsen existing menopausal symptoms.5 Also, menopausal symptoms could result from quitting hormone therapy (HT) during the breast cancer treatment process5; those taking HT at the time of diagnosis are usually advised to cease HT.2,6–9 Furthermore, about 52% of breast cancer patients taking tamoxifen complained of night sweats, and 78% of them experienced hot flashes.2,6–9 These symptoms reportedly decrease the women’s quality of life and daily functioning, and increase their fatigue, depression, anxiety, and sleep disruption.2,6–9 The symptoms could be acute or chronic and could increase distress, subsequently compromising the women’s quality of life.10
Asian American breast cancer survivors have been frequently reported to have lower quality of life compared to other racial/ethnic groups.11–14 A major reason for their lower quality of life was postulated as inadequate management of symptoms including menopausal symptoms.11,12,15,16 Furthermore, the relationship between poor quality of life and fewer sources of information and coaching/support for symptom management was stronger for Asian Americans than for Whites.11,12,15,16 In Tu et al.’s study,17 Chinese Americans lacked information and coaching/support despite high family support. Ashing-Giwa et al.18 pointed out that family support delayed care seeking and caused self-deprecation in Asian Americans. These demonstrate a definite need for information and coaching/support in this specific population.
Technology-based programs could be a solution to fill the gap in care. Mainly because of easy access (e.g., no transportation required, 24-hour access, etc.) without time or cost constraints on both sides (patients and health care providers), technology-based programs are effective in providing information and coaching/support compared to conventional programs.19–22 Researchers have also indicated their effectiveness in approaching isolated/marginalized people with stigmatized conditions and underserved populations such as racial/ethnic minority groups.23–24 Furthermore, socially marginalized groups reportedly indicate greater interests in e-health than those not marginalized, and the marginalized groups value technology-based programs.25–30
In this study, a technology-based information and coaching/support program was tested for its efficacy on menopausal symptoms of Asian American breast cancer survivors. The program was developed based on the findings from previous studies31–43 that focused on racial/ethnic differences in cancer pain and symptom experience. Subsequently, the program was culturally tailored to Asian American midlife women by incorporating their unique cultural attitudes toward breast cancer and menopausal symptom management. The program was theoretically based on the Bandura’s Theory of Behavioral Change44 while focusing on changing the women’s attitudes, self-efficacy, and barriers (see the below for more information on the program). The hypotheses that were tested included:
Hypothesis 1. Those who use the program and the American Cancer Society (ACS) website show significantly greater improvements than those who use only the ACS website in self-reported menopausal symptoms (total distress scores and frequencies) from a pre-test (Time 0) to two follow-up time points (post 1 month [Time 1] and post 3 months [Time 2]).
Hypothesis 2. Theory-based variables (attitudes, social influences, perceived barriers, and self-efficacy) mediate the effects of the intervention on self-reported menopausal symptoms (total distress scores and frequencies) from Time 0 to Time 2.
Methods
A randomized repeated measures pretest/posttest control group design was adopted in this study. This was a part of an ongoing intervention study to examine the efficacy of a theory-driven, culturally tailored technology-based program on enhancing survivorship of Asian American breast cancer survivors. The parent study was approved by the Institutional Review Board of the institution where the authors were associated with. The CONSORT guidelines were used to guide the research process and reporting.45 The data for the study have been collected from January 2017 to May 2018.
Samples and Settings
The participants have been recruited through online and offline support/social groups for Asian Americans (e.g., churches, organizations, forums, healthcare centers, professional groups, etc.). Study announcements were made by sending messages to gatekeepers (e.g., website owners, pastors, etc.) and by posting study flyers in various groups (e.g., social media groups, community support groups, etc.).
The inclusion criteria were those who (a) identified themselves as Chinese, Korean, or Japanese; (b) were aged 21 years and older; (c) were diagnosed with breast cancer in the past 5 years; (d) could read and write English, Mandarin Chinese, Korean, or Japanese; and (e) could access the Internet. A total of 91 Asian American breast cancer survivors completed the pre-test questionnaire. In the control group, the retention rate was 85.7% at post 1-month (n = 36) and 76.2% at post 3-months (n = 32). In the intervention group, the retention rate was 79.6% at post 1-month (n = 39) and 69.4% at post 3-months (n = 34; Figure 1). Despite the dropouts, no one officially withdrew from the study.
Figure 1.
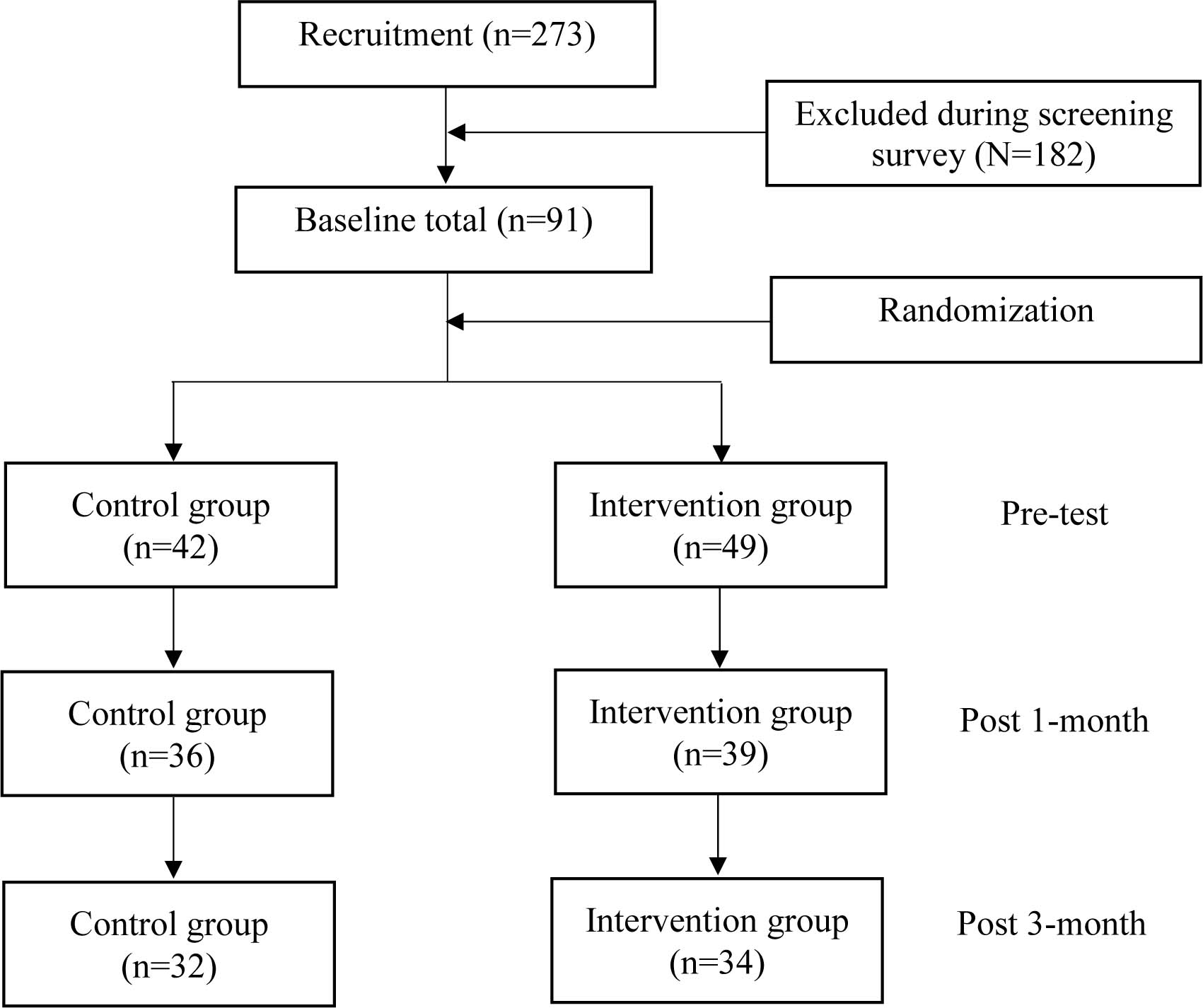
The participant flow diagram.
The sample size was calculated using the G*Power 3.1.9.2 software.46 With an assumed effect size of 0.8047(the difference in the menopausal symptom scores), at least 21 participants per group were necessary to achieve 80% of power at an alpha level of 0.10. Thus, the current number of participants (n = 91) was adequate to detect actual differences between the control and intervention groups over time.
TICAA
The TICAA is a theory-driven and culturally tailored intervention program that aims to provide information and coaching/support for Asian American breast cancer survivors. Again, the program is theoretically based on the Bandura’s Theory of Behavioral Change.44 According to the theory, changing individuals’ attitudes, self-efficacy, perceived barriers, and social influences results in changes in health behaviors, subsequently influencing health outcomes. The TICAA is composed of culture-specific educational modules (provided in English, simplified and traditional Chinese, Korean, and Japanese), culture-specific online resources, and group and individual coaching by culturally matched nurse interventionists (e.g., Chinese RN interventionists for Chinese participants). The information and coaching/support provided by the TICAA are expected to change the women’s attitudes related to breast cancer and symptom management, self-efficacy, perceived barriers, and social influences. In general, coaching/support48–50 and information51–54 reportedly change health behaviors through changing attitudes, self-efficacy, perceived barriers, and social influences. More detailed information on the TICAA is available elsewhere (to be added).
Instruments
Questions on background characteristics.
Background characteristics were measured using questions on age (in years), sub-ethnicity (Chinese, Korean, or Japanese), marital status (married/partnered or nonmarried/unpartnered), yearly family income (totally insufficient, somewhat insufficient, sufficient, or more than sufficient), perceived health status (1 = “not healthy at all” to 6 = “very healthy”), breast cancer type (invasive or non-invasive), breast cancer stage (stage 1 to 4 or unsure), symptom management (yes or no), and the use of medicine (yes or no). Initially, the participants’ marital status was grouped into 5 categories, but it was later collapsed into two categories because less than 8% of the participants belonged to the ‘single/never had partner/widowed’ category.
Questions on Attitudes and Social Influences.
The sub-scales on attitudes and social influences from the Questions on Attitudes, Subjective Norm, Perceived Behavioral Control, and Behavioral Intention (QASPB)55 were used to measure the participants’ attitudes and social influences related to survivorship management. The sub-scale on attitudes included six items, and each item was assessed on a 6-point Likert scale (−3 = “dull” to 3 = “interesting”). The sub-scale on social influences consisted of three items, and each item was assessed on a 7-point Likert scale (1= “disagree” to 7 = “agree”). The attitudes and social influences scores were calculated by averaging the items in each sub-scale. In this study, Cronbach’s alpha of the attitudes sub-scale was 0.96 and that of the social influence sub-scale was 0.85.
Questions on perceived barriers.
To measure the participants’ perceived barriers, the modified Barriers to Health Activities Scale56 was used. The scale was comprised of sixteen items that asked the participants to rate the frequencies of interferences in managing issues/concerns related to breast cancer due to specific problems listed in individual items. Each item was assessed on a 4-point Likert scale (1 = “never” to 4 = “always”), and the average of all items was calculated as the perceived barrier scores. The scale had a high internal consistency (Cronbach’s alpha = 0.91).
The Cancer Behavior Inventory (CBI-B).
Self-efficacy was measured with six items that were adopted from the CBI-B. The CBI-B assessed if the participants accepted cancer and maintained positive attitudes and confidence in seeking and understanding medical information and seeking social support.57 Each item used a 9-point Likert scale (1 = “not at all confident” to 9 = “total confident”). The average of all items was calculated as the efficacy score. In this study, the scale showed a high internal consistency (Cronbach’s alpha=0.90).
The Memorial Symptom Assessment Scale-Short Form (MSAS-SF).
Items on menopausal symptoms were extracted from the MSAS-SF. The MSAS-SF is a well-validated tool for assessing the distress and frequency of symptoms in cancer patients during the past seven days.58 The distress subscale measures the distress associated with 28 prevalent physical and psychological symptoms (particularly where symptom frequency is not important, such as hair loss), whereas the frequency subscale measures four prevalent psychologic symptoms. For the current study, only the items related to menopausal symptoms were selected from the MSAS-SF.
The items on menopausal symptoms were divided into three categories based on the Midlife Women’s Symptom Index (MSI)59: physical, psychological, and psychosomatic symptoms. The symptom distress subscale included 15 physical symptoms, two psychological symptoms, and two psychosomatic symptoms. Physical symptoms included “nausea,” “vomiting,” “shortness of breath,” “night sweats,” “feeling bloated,” “problems with urination,” “diarrhea,” “weight loss,” “itching,” “changes in skin,” “constipation,” “swelling of arms or legs,” “numbness/tingling in hands/feet,” “lack of appetite,” and “pain.” Psychological symptoms included “difficulty concentrating” and “problems with sexual interest or activity.” Psychosomatic symptoms include “difficulty sleeping” and “dizziness.” The symptom distress was scored on a 5-point Likert scale (0.8 = “not at all” to 4.0 = “very much”). The total distress scores were calculated as the average of the three symptom sub-scores (physical, psychological and psychosomatic symptoms); each sub-score was the average of the items in each symptom category. In this study, Cronbach’s alpha of the symptom distress subscale was 0.84.
The symptom frequency was assessed only for four psychological symptoms (“feeling sad,” “worrying,” “feeling irritable,” and “feeling nervous”). The symptom frequency was rated on a 4-point Likert scale (1 = “rarely” to 4 = “almost constantly”). The total frequency score was calculated as the average of the item ratings. In this study, Cronbach’s alpha of the symptom frequency subscale was 0.86.
Data Collection Procedures
The participants could select one of the five language versions of the project website (English, Mandarin Chinese [traditional and simplified], Korean, and Japanese). When potential participants visited the project website and clicked the ‘I agree to participate’ button (after reviewing the electronic informed consent form in their selected languages), they were screened against the inclusion criteria. Only those who met the inclusion criteria were linked to the pre-test questionnaire. At the completion of the pre-test questionnaire, the participants were enrolled into the project website by research staff. During the enrollment process, the participants were automatically randomized into two groups (control vs. intervention groups) using an automated random number generator on the project website. They were allowed to change their IDs and passwords once they logged in the project website. Then, an electronic instruction sheet was given to the participants (e.g., information on when they need to re-visit, when to complete the next questionnaires, how to use the program, etc.).
Both groups were provided with a link to the American Cancer Society (ACS) websites on breast cancer survivorship including menopausal symptom management and asked to use the website whenever they wanted. For three months, the intervention group was required to use both the TICCA program and the ACS websites while the control group was required to use only the ACS website. The intervention group was provided with weekly group or individual coaching sessions by culturally-matched nurse interventionists. They were also encouraged to utilize culture-specific online resources that were available on the project website. At the end of the first and the third months, the participants were asked to fill out the second and third questionnaires. Both groups were also asked to maintain their usual information searches through their usual resources. Biweekly reminders and thank you emails were sent to the participants.
Data Analysis
All analyses were performed using the SAS, version 9.4. (SAS Institute, Cary, NC). Statistical significances were determined at an alpha level of 0.10 due to the relatively small sample size. To retain the maximum number of cases, mean substitutions were used for continuous variables when there were less than 20% missing data while missing data were kept for the categorical variables. All the continuous and categorical variables had less than 20% missing fields in the intervention and control groups (no significant differences in missing information). All outcome variables were examined for normality, and the data with non-normal distributions were log-transformed before the analyses. The data were analyzed using an intention-to-treat approach.
First, the data were analyzed using descriptive statistics (e.g., frequencies, percentages, means, or standard deviations) to describe the participants’ background characteristics. Also, these characteristics were compared between the control and intervention groups using chi-square tests, Fisher’s exact tests, and two-sample independent t-tests. No significant differences were found in the characteristics between the Intervention and control groups.
To test the intervention effects, a linear mixed-model growth cure analysis was adopted with both fixed and random effects in the model, using the SAS PROC MIXED.60 A separate mixed model was built for each outcome, and the analysis included the effects of time (pre-test, post-1-month, and post-3-months), treatment groups (control and intervention), and time x treatment group interactions. In addition, a random intercept and a random slope (only with a significant time fixed effect) were modeled to account for individual variations in the changes in the menopausal symptom scores over time. Further, theory-based variables (attitudes, social influences, perceived barriers, and self-efficacy) were included as additional predictors in each linear mixed-model in order to examine their potential mediating effects. The analysis used the maximum likelihood estimation, the unstructured covariance structure, and the Kenward-Roger degree of freedom method. The degree of freedom method is ideal for this study because it could be used in models with unbalanced designs, could handle complex covariance structures, and could adjust for the bias due to a small sample size.61 With nested models, the Akaike information criterion (AIC) was compared to select the best fitting model.
Results
Characteristics of the Participants
Table 1 presents the participants’ background characteristics; the control and intervention groups did not significantly differ in their background characteristics. The average age was 51.3 years (SD=11.31). About 57%, 23%, and 20% of the participants were Chinese, Korean, and Japanese, respectively. Approximately two-thirds of the participants were married or partnered. The participants were almost equally divided into the insufficient and sufficient income groups. The participants tended to perceive their health as “fair” (the total mean score = 3.46 on a 6-point scale [1~6], SD = 1.07). Over two-thirds of the participants had an invasive form of breast cancer (Stage I or II). About 64% were managing their symptoms, and a majority of them (80.9%) were taking medications. In particular, almost all the participants were taking estrogen antagonists such as tamoxifen, letrozole, or anastrozole for treatment of their hormonally-responsive breast cancer.
Table 1.
Characteristics of the control and intervention groups at the pre-test.
| Characteristics | Range | Control (N=42) |
Intervention (N=49) |
Total (N=91) |
p |
|---|---|---|---|---|---|
| Age (y) (Mean±SD) | 21–79 | 51.91±10.01 | 50.63±12.75 | 51.32±11.31 | .59 |
| Subethnicity, N (%) | .22 | ||||
| Chinese | 28 (66.67) | 24 (48.98) | 52 (57.14) | ||
| Korean | 7 (16.67) | 14 (28.57) | 21 (23.08) | ||
| Japanese | 7 (16.67) | 11 (22.45) | 18 (19.78) | ||
| Marital status, N (%) | .23 | ||||
| Married or partnered | 32 (76.19) | 31 (64.58) | 63 (70.00) | ||
| Nonmarried or unpartnered | 10 (23.81) | 17 (35.42) | 27 (30.00) | ||
| Yearly family income, N (%) | .11 | ||||
| Totally insufficient | 4 (9.76) | 12 (25.00) | 16 (17.98) | ||
| Somewhat insufficient | 2 (41.46) | 13 (27.08) | 30 (33.71) | ||
| Sufficient | 13 (31.71) | 19 (39.58) | 32 (35.96) | ||
| More than sufficient | 7 (17.07) | 4 (8.33) | 11 (12.36) | ||
| Perceived health status (Mean±SD) | 1.0–5.8 | 3.57±0.96 | 3.34±1.16 | 3.46±1.07 | .30 |
| Breast cancer: types, N (%) | .56 | ||||
| Invasive | 27 (75.00) | 37 (80.43) | 64 (78.05) | ||
| Non-invasive (in situ) | 9 (25.00) | 9 (19.57) | 18 (21.95) | ||
| Breast cancer: stages, N (%) | .99a | ||||
| Stage1 | 13 (32.50) | 17 (35.42) | 30 (34.09) | ||
| Stage2 | 17 (42.50) | 20 (41.67) | 37 (42.05) | ||
| Stage3 | 4 (10.00) | 5 (10.42) | 9 (10.23) | ||
| Stage4 | 2 (5.00) | 3 (6.25) | 5 (5.68) | ||
| Unsure | 4 (10.00) | 3 (6.25) | 7 (7.95) | ||
| Symptom management, N (%) | .65 | ||||
| Yes | 22 (61.11) | 31 (65.96) | 53 (63.86) | ||
| No | 14 (38.89) | 16 (34.04) | 30 (36.14) | ||
| The use of medication, N (%) | .32 | ||||
| Yes | 35(85.37) | 37 (77.08) | 72 (80.90) | ||
| No | 6 (14.63) | 11 (22.92) | 17 (19.10) |
SD = standard deviation
Fisher’s exact test
Table 2 compares the outcome and theory-based variables by group at pre-test. There were no statistically significant group differences in the distress scores of physical, psychosomatic, and psychological symptoms as well as in the frequencies of psychological symptoms. In addition, no statistically significant differences were found between the groups in the women’s attitudes, social influences, perceived barriers, and self-efficacy.
Table 2.
Outcome and theory-based variables by group at the pre-test.
| Outcome variables (Mean±SD) |
Range | Control (N=42) |
Intervention (N=49) |
Total (N=91) |
p |
|---|---|---|---|---|---|
| Symptom Distress | |||||
| Physical symptomsa | 0.8–2.4 | 1.40±0.38 | 1.42±0.50 | 1.41±0.45 | .82 |
| Psycho logical symptomsb | 0.8–2.9 | 1.67±0.50 | 1.72±0.70 | 1.70±0.61 | .66 |
| Psychosomatic symptomsc | 0.8–3.5 | 1.67±0.63 | 1.89±0.84 | 1.75±0.75 | .35 |
| Total | 0.8–2.6 | 1.58±0.39 | 1.65±0.58 | 1.62±0.50 | .66 |
| Symptom Frequency | |||||
| Psychological symptomsd
(log transformed) |
0.9–3.6 | 1.93±0.67 | 1.84±0.73 | 1.89±0.70 | .57 |
| Theory-based variables | |||||
| Attitudes | 1.2–5.9 | 3.49 (2.03) | 4.06 (1.89) | 3.80 (1.96) | .17 |
| Social influences | 1.1–6.8 | 5.72 (1.45) | 5.61 (1.28) | 5.67 (1.36) | .71 |
| Perceived barriers | 1.0–3.9 | 3.12 (0.55) | 2.98 (0.61) | 3.05 (0.59) | .27 |
| Self-efficacy | 1.1–8.8 | 5.96 (1.56) | 6.16 (1.77) | 6.06 (1.67) | .55 |
SD = standard deviation/ All categories of symptoms were measured using the MSAS-SF.
Physical symptoms included ‘nausea,’ ‘vomiting,’ ‘shortness of breath,’ ‘sweats,’ ‘feeling bloated,’ ‘problems with urination,’ ‘diarrhea,’ ‘weight loss,’ ‘itching,’ ‘changes in skin,’ ‘constipation,’ ‘swelling of arms or legs,’ ‘numbness/tingling in hands/feet,’ ‘lack of appetite,’ and ‘pain.’
Psychological symptoms included ‘difficulty concentrating’ and ‘problems with sexual interest or activity.’
Psychosomatic symptoms included ‘difficulty sleeping’ and ‘dizziness.’
Psychological symptoms included ‘feeling sad,’ ‘worrying,’ ‘feeling irritable,’ and ‘feeling nervous.’
The Effects on Menopausal Symptoms (Hypothesis 1)
Table 3 shows the fixed effects of time, study arms, and time x study arm interactions after controlling for the random intercept/slope. The intervention group showed a significant decrease in the distress scores of menopausal symptoms over time: physical (β = −0.07, p = 0.08), psychological (β = −0.13, p = 0.05), psychosomatic (β = −0.17, p = 0.06), and total symptoms (β = −0.19, p = 0.01). The distress scores of menopausal symptoms (in each domain and in total) were not significantly different between the groups at pre-test when individual variations were taken into account. The time effect was not statistically significant since the directions of the time-related changes in the distress scores of menopausal symptoms were opposite between the groups. In addition, the frequencies of psychological symptoms significantly decreased over time for both groups (β = −0.11, p = 0.01) although the time x study arm interaction was not statistically significant.
Table 3.
Menopausal symptoms at pre-test, post-1-month, and post-3-months by group.
| Control (N=42) |
Intervention (N=49) |
p | |||||
|---|---|---|---|---|---|---|---|
| Outcome variables | Mean+ | SD | Mean | SD | Group | Time | Group*Time |
| Symptom Distress | |||||||
| Physical symptomsa | |||||||
| Pre-test | 1.40 | 0.32 | 1.42 | 0.37 | .76 | .21 | .08* |
| Post 1 month | 1.41 | 0.29 | 1.36 | 0.34 | |||
| Post 3 months | 1.42 | 0.27 | 1.31 | 0.32 | |||
| Psychological symptomsb | |||||||
| Pre-test | 1.64 | 0.37 | 1.76 | 0.47 | .39 | .28 | .05** |
| Post 1 month | 1.67 | 0.33 | 1.65 | 0.43 | |||
| Post 3 months | 1.71 | 0.29 | 1.55 | 0.38 | |||
| Psychosomatic symptomsc | |||||||
| Pre-test | 1.67 | 0.47 | 1.82 | 0.66 | .34 | .13 | .06* |
| Post 1 month | 1.69 | 0.42 | 1.67 | 0.56 | |||
| Post 3 months | 1.70 | 0.42 | 1.52 | 0.49 | |||
| Total | |||||||
| Pre-test | 1.57 | 0.33 | 1.66 | 0.45 | .36 | .098* | .01** |
| Post 1 month | 1.59 | 0.31 | 1.57 | 0.41 | |||
| Post 3 months | 1.61 | 0.30 | 1.47 | 0.37 | |||
| Symptom Frequency | |||||||
| Psychological symptomsd (log transformed) |
|||||||
| Pre-test | 1.94 | 0.54 | 1.82 | 0.54 | .40 | .008*** | .89 |
| Post 1 month | 1.84 | 0.42 | 1.71 | 0.45 | |||
| Post 3 months | 1.73 | 0.37 | 1.59 | 0.43 | |||
SD = standard deviation/ All categories of symptoms were measured using the MSAS-SF.
Predicted means for individual outcomes by group and time.
Physical symptoms included ‘nausea,’ ‘vomiting,’ ‘shortness of breath,’ ‘sweats,’ ‘feeling bloated,’ ‘problems with urination,’ ‘diarrhea,’ ‘weight loss,’ ‘itching,’ ‘changes in skin,’ ‘constipation,’ ‘swelling of arms or legs,’ ‘numbness/tingling in hands/feet,’ ‘lack of appetite,’ and ‘pain.’
Psychological symptoms included ‘difficulty concentrating’ and ‘problems with sexual interest or activity.’
Psychosomatic symptoms included ‘difficulty sleeping’ and ‘dizziness.’
Psychological symptoms included ‘feeling sad,’ ‘worrying,’ ‘feeling irritable,’ and ‘feeling nervous.’
p < .10
p < .05
p < .01
The Mediation of the Theory-Based Variables (Hypothesis 2)
Table 4 shows the changes in the time x study arm interaction coefficients for the distress scores and frequencies before and after adjusting for each of the theory-based variables. Notably, a percent difference in the magnitudes of the regression coefficients was calculated between the unadjusted and adjusted models in order to determine the extent of mediation of each theory-based variable. The values were calculated by 100*(β0−β1)/β0, where (β0) is the coefficient in an initial baseline model and (β1) is the coefficient in a model, adjusted for each theory-based variable.
Table 4.
Regression coefficients of menopausal symptom distress scores and frequencies (unadjusted and adjusted for theory-based variables).
| Group x Time interaction | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome variables | Model 1e | Model 2f | % difference in magnitude of β (Model 1 vs 2) |
Model 3g | % difference in magnitude of β (Model 1 vs 3) |
Model 4h | % difference in magnitude of β (Model 1 vs 4) |
Model 5i | % difference in magnitude of β (Model 1 vs 5) |
||||||
| Symptom distress | |||||||||||||||
| Physicala | −0.069* | −0.061 | −11.60 | −0.058* | −15.94 | −0.069* | 0.00 | −0.068* | −1.45 | ||||||
| Psychologicalb | −0.133** | −0.120* | −9.77 | −0.122** | −8.27 | −0.133** | 0.00 | −0.130** | −2.26 | ||||||
| Psychosomaticc | −0.167* | −0.157* | −6.00 | −0.154* | −7.78 | −0.166* | −0.06 | −0.160* | −4.19 | ||||||
| Total | −0.118** | −0.061** | −48.30 | −0.108** | −8.47 | −0.119** | 0.08 | −0.111** | −5.93 | ||||||
| Symptom frequency | |||||||||||||||
| Psychologicald
(log transformed) |
−0.011 | −0.008 | −27.27 | −0.007 | −36.36 | −0.011 | 0.00 | −0.010 | −9.09 | ||||||
Note. The group x time interactions were estimated for the intervention group, relative to the control group as a reference/ / All categories of symptoms were measured using the MSAS-SF.
Physical symptoms included ‘nausea,’ ‘vomiting,’ ‘shortness of breath,’ ‘sweats,’ ‘feeling bloated,’ ‘problems with urination,’ ‘diarrhea,’ ‘weight loss,’ ‘itching,’ ‘changes in skin,’ ‘constipation,’ ‘swelling of arms or legs,’ ‘numbness/tingling in hands/feet,’ ‘lack of appetite,’ and ‘pain.’
Psychological symptoms included ‘difficulty concentrating’ and ‘problems with sexual interest or activity.’
Psychosomatic symptoms included ‘difficulty sleeping’ and ‘dizziness.’
Psychological symptoms included ‘feeling sad,’ ‘worrying,’ ‘feeling irritable,’ and ‘feeling nervous.’
Model 1 = group + time + group x time + random intercept/slope
Model 2 = Model 1 + attitudes
Model 3 = Model 1 + social influences
Model 4 = Model 1 + perceived barriers
Model 5 = Model 1 + self-efficacy
p <.10
p <.05
Model 1 included the fixed effects (time, study arm, and time x study arm) and random intercept or slope. Models 2 to 5 were controlled for the women’s attitudes, social influences, perceived barriers, and self-efficacy, respectively. After adjusting for the attitudes in Model 2, there were decreases (ranged from 6.00% to 48.30%) in the time x study arm interaction coefficients across the outcome variables (the symptom distress scores and frequencies). The attitudes in Model 2 fully mediated the intervention effect on the distress scores of physical symptoms (β = −0.07 [p<0.10] to −0.06 [not significant]) while the attitudes partially mediated its effect on the distress scores of psychological (β = −0.13 to −0.12, p < 0.10), psychosomatic (β = −0.17 to −0.16, p < 0.10]), and total symptoms (β = −0.12 to −0.06, p < .05]). The inclusion of social influences in Model 3 also decreased the interaction coefficients from 7.80% to 36.40% across the outcome variables. The social influences in Model 3 partially mediated the intervention effect on the distress scores of all types of symptoms (β = −0.07 ~ −0.06, p < 0.10 for physical symptoms; β = −0.13 ~ −0.12, p < 0.05 for psychological symptoms; β = −0.17 ~ −0.15, p < 0.10 for psychosomatic symptoms; and β = −0.12 ~ −0.11, p < 0.05 for total symptoms). Yet, the perceived barriers in Model 4 barely mediated the intervention effect on the distress scores of all types of symptoms according to the percent differences in the magnitudes of coefficients that were almost zero (range: 0.00–0.08). Finally, the self-efficacy in Model 5 partially mediated the intervention effect on the distress scores of all symptoms (β = −0.069 ~ −0.068, p < 0.10 for physical symptoms; β = −0.133 ~ −0.130, p < 0.05 for psychological symptoms; and β = −0.167 ~ −0.160, p < 0.10 for psychosomatic symptoms; and β = −0.118 ~ −0.111, p < 0.05 for total symptoms). After adjusting for the self-efficacy in Model 5, there were decreases (ranged from 1.5% to 9.1%) in the interaction coefficients across the outcome variables. Based on the percent differences in the magnitudes of coefficients between the unadjusted and adjusted models, the extent of mediation was the strongest for the women’s attitudes and social influences, followed by self-efficacy and perceived barriers. Yet, no theory-based variables mediated the intervention effects on the symptom frequencies.
Discussion
The findings supported the beneficial effects of the TICAA on alleviating menopausal symptoms of Asian American breast cancer survivors by changing the women’s attitudes, self-efficacy, and social influences. This finding is consistent with those in the literature on technology-based programs; technology-based programs in general effectively provide information and coaching/support, change health behaviors, and improve health outcomes.19–22
Usually, 3 months are considered to be adequate to observe significant effects of a technology-based intervention on decreasing menopausal symptoms.62 In a systematic literature review, the average intervention period of technology-based interventions related to menopause was 52 days (range = 1–90 days).62 The findings of this study certainly agrees with the literature; the 3-month intervention period of the TICAA was adequate to decrease menopausal symptoms by changing the women’s attitudes, self-efficacy, and social influences.
The 3-month period of the intervention, yet, was not enough to change the women’s perceived barriers related to symptom management in this study. The literature supports that dividing a person’s assessment on the barriers to a specific behavior (perceived barriers) from the assessed difficulty of the behavior (self-efficacy) is infeasible.63 Thus, some researchers suggest merging the two concepts so that research participants could be asked for their confidence to deal with specific barriers (“barriers-based self-efficacy”).63 Since the two concepts were measured using different scales in this study, the different findings in the two concepts (significant changes in self-efficacy, but no significant changes in perceived barriers) may be due to differences in the instruments (e.g., validity, reliability, etc.).
Because researchers usually do not have the controllability of users’ behaviors in technology-based interventions using computers and mobile devices,64 the reliability of the data that are collected through the technology-based interventions totally depends on the users’ willingness and acceptance of the intervention.65 Subsequently, high dropout rates have been reported as a major weakness of the technology-based interventions.65 Indeed, research participants could not feel pressured to complete the intervention or questionnaires,66 could easily stop participating in the study by leaving the Website,67 and/or could feel uncomfortable about using technology.68 However, this study indicated relatively high retention rates (about or over 80% across the groups and time points), which is much higher than the retention rates that have been reported in the current literature.62 Maybe, this is due to the fact that the intervention was culturally tailored to this specific population by incorporating culture-specific components with several culture-specific features (e.g., the use of culturally matched interventionists, ethnic-specific educational sessions, etc.). Also, the high retention rates might reflect Asian Americans’ tendency in their research participation; they wanted to be a good research participant.69 The literature also supports the characteristics of Asian culture that emphasizes a balance and harmony in interactions.70
The findings, yet, need to be carefully interpreted due to the following limitations. First of all, this study tended to include a wide range of menopausal symptoms in order to reflect diverse menopausal symptoms of ethnically different populations, which could confound the findings. Furthermore, menopausal symptoms were measured using a non-menopause specific instrument and the items were pre-determined by the parent study, which might cause the underestimation or overestimation of the women’s actual menopausal symptoms. In addition, there could possibly exist selection biases because the participants had to have access to the Internet (using computers or mobile devices). Moreover, all the data were self-reported, which could be a source of bias as well. Because the study was a technology-based intervention study targeting a hidden underserved population in the communities, it was essential to ensure participants’ anonymity. Subsequently, it was virtually impossible to obtain the participants’ medical records to confirm their self-reported data (e.g., their diagnosis of breast cancer). Finally, there was no control of the sample selection process and the sample size because this was a part of the ongoing parent study.
Conclusions
The findings of this study strongly supported the efficacy of a 3-month technology-based intervention on alleviating menopausal symptoms among Asian American breast cancer survivors. Also, the findings supported that the TICAA could change the women’s attitudes, self-efficacy, and social influences, and subsequently decrease the women’s menopausal symptoms. Based on the findings, this paper concludes with the following implications for future research and practice. First, a 3-month intervention period would be sufficient for future technology-based interventions that aim to decrease menopausal symptoms of Asian American breast cancer survivors. Second, possible response biases (e.g., social desirability bias) need to be carefully monitored and controlled during the intervention process. Third, further studies with diverse groups of women are needed to confirm the findings reported in this paper. Also, objective measures confirming self-reported data need to be incorporated into future research and practice in order to avoid possible biases that may result from self-reported data. Finally, more studies are needed to determine the best ways to deliver an intervention to racial/ethnic minority breast cancer survivors.
Acknowledgments
Source of Funding: The study was funded by the National Cancer Institute (NIH/NCI; 1R01CA203719).
Financial disclosures: Dr. Mao is supported by a grant from the National Institutes of Health/National Cancer Institute Cancer Center (P30 CA008748).
Footnotes
conflicts of interest: The other authors have nothing to disclose.
References
- 1.American Cancer Society. Cancer Facts & Figures 2015 Special Section: Breast Carcinoma In Situ http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/. Accessed September 23, 2015.
- 2.American Cancer Society. Breast cancer facts & figures http://www.cancer.org/docroot/STT/STT_0.asp. Accessed March 17, 2012.
- 3.National Cancer Institute. SEER Stat Fact Sheets: Breast http://seer.cancer.gov/statfacts/html/breast.html. Accessed December 31, 2013.
- 4.Mazor M, Lee K, Dhruva A, et al. Menopausal-related symptoms in women one year after breast cancer surgery. J Pain Symptom Manage 2018;55(4):1138–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loibl S, Lintermans A, Dieudonné AS, Neven P. Management of menopausal symptoms in breast cancer patients. Maturitas 2011;68(2):148–154. doi: 10.1016/j.maturitas.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 6.American Cancer Society. Breast Cancer Signs and Symptoms http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-signs-symptoms. Accessed August 7, 2014.
- 7.American Cancer Society. Signs and Symptoms of Cancer. What are signs and symptoms? http://www.cancer.org/cancer/cancerbasics/signs-and-symptoms-of-cancer. Accessed August 7, 2014.
- 8.Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol 2014;32(16):1739–1747. doi: 10.1200/JCO.2013.52.4629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Satija A, Ahmed SM, Gupta R, et al. Breast cancer pain management - a review of current & novel therapies. Indian J Med Res 2014;139:216–225. [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenberg SM, Partridge AH. New insights into nonadherence with adjuvant endocrine therapy among young women with breast cancer. J Natl Cancer Inst 2015;107(10):djv245. doi: 10.1093/jnci/djv245. [DOI] [PubMed] [Google Scholar]
- 11.Yi JK, Swartz MD, Reyes-Gibby CC. English proficiency, symptoms, and quality of life in Vietnamese- and Chinese-American breast cancer survivors. J Pain Symptom Manage 2011;42(1):83–92. doi: 10.1016/j.jpainsymman.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 12.Lim J, Yi J. The effects of religiosity, spirituality, and social support on quality of life: a comparison between Korean American and Korean breast and gynecologic cancer survivors. Oncol Nurs Forum 2009;36(6):699–708. doi: 10.1188/09.ONF.699-708. [DOI] [PubMed] [Google Scholar]
- 13.Lim J, Zebrack B. Different pathways in social support and quality of life between Korean American and Korean breast and gynecological cancer survivors. Qual Life Res 2008;17(5):679–689. doi: 10.1007/s11136-008-9343-4. [DOI] [PubMed] [Google Scholar]
- 14.Lim JW, Ashing-Giwa KT. Is family functioning and communication associated with health-related quality of life for Chinese-and Korean-American breast cancer survivors? Qual Life Res 2013;22(6):1319–29. doi: 10.1007/s11136-012-0247-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Cancer Society. Cancer Facts & Figures http://www.cancer.org/research/cancerfactsfigures/cancerfactsfigures/cancer-facts-figures-2013. Accessed December 31, 2013.
- 16.Chlebowski RT, Chen Z, Anderson GL, et al. Ethnicity and breast cancer: factors influencing differences in incidence and outcome. J Natl Cancer Inst 2005;97(6):439–448. doi: 10.1093/jnci/dji064. [DOI] [PubMed] [Google Scholar]
- 17.Tu S-P, Chen H, Chen A, Lim J, May S, Drescher C. Clinical trials: understanding and perceptions of female Chinese-American cancer patients. Cancer 2005;104(12 Suppl):2999–3005. doi: 10.1002/cncr.21524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ashing-Giwa KT, Padilla G, Tejero J, et al. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psychooncology 2004;13(6):408–428. doi: 10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trudeau KJ, Ainscough JL, Trant M, Starker J, Cousineau TM. Identifying the educational needs of menopausal women: a feasibility study. Womens Health Issues 2011;21(2):145–152. doi: 10.1016/j.whi.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saver BG, Gustafson D, Taylor TR, et al. A tale of two studies: the importance of setting, subjects and context in two randomized, controlled trials of a web-based decision support for perimenopausal and postmenopausal health decisions. Patient Educ Couns 2007;66(2):211–222. doi: 10.1016/j.pec.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Col NF. Using Internet technologies to improve and simplify counseling about menopause: the WISDOM website. Maturitas 2007;57(1):95–99. doi: 10.1016/j.maturitas.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 22.Al-Zadjali M, Keller C, Larkey LK, Albertini L, Center for Healthy Outcomes in Aging. Evaluation of intervention research in weight reduction in post menopausal women. Geriatr Nurs 2010;31(6):419–434. doi: 10.1016/j.gerinurse.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Pekmezi DW, Williams DM, Dunsiger S, et al. Feasibility of using computer-tailored and internet-based interventions to promote physical activity in underserved populations. Telemed J E-Health 2010;16(4):498–503. doi: 10.1089/tmj.2009.0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoo J-S, Hwang A-R, Lee H-C, Kim C-J. Development and validation of a computerized exercise intervention program for patients with type 2 diabetes mellitus in Korea. Yonsei Med J 2003;44(5):892–904. [DOI] [PubMed] [Google Scholar]
- 25.Mead N, Varnam R, Rogers A, Roland M. What predicts patients’ interest in the Internet as a health resource in primary care in England? J Health Serv Res Policy 2003;8(1):33–39. doi: 10.1258/13558190360468209. [DOI] [PubMed] [Google Scholar]
- 26.Moore M, Bias RG, Prentice K, Fletcher R, Vaughn T. Web usability testing with a Hispanic medically underserved population. J Med Libr Assoc 2009;97(2):114–121. doi: 10.3163/1536-5050.97.2.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell M, Meier A, Carr C. Health behavior changes after colon cancer: a comparison of findings from face-to-face and on-line focus groups. Fam Comm Health 2001;24(3):88–103. [DOI] [PubMed] [Google Scholar]
- 28.Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Educ Res 2001;16(6):671–692. [DOI] [PubMed] [Google Scholar]
- 29.Wanner M, Martin-Diener E, Braun-Fahrländer C, Bauer G, Martin BW. Effectiveness of active-online, an individually tailored physical activity intervention, in a real-life setting: randomized controlled trial. J Med Internet Res 2009;11(3):e23. doi: 10.2196/jmir.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Massoudi BL, Olmsted MG, Zhang Y, Carpenter RA, Barlow CE, Huber R. A web-based intervention to support increased physical activity among at-risk adults. J Biomed Inform 2010;43(5 Suppl):S41–45. doi: 10.1016/j.jbi.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 31.Im E-O, Ho T-H, Brown A, Chee W. Acculturation and the cancer pain experience. J Transcult Nurs 2009;20(4):358–370. doi: 10.1177/1043659609334932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Im E-O, Lim H-J, Clark M, Chee W. African American cancer patients’ pain experience. Cancer Nurs 2008;31(1):38–46. doi: 10.1097/01.NCC.0000305685.59507.9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Im E-O, Lee SH, Liu Y, Lim H-J, Guevara E, Chee W. A national online forum on ethnic differences in cancer pain experience. Nurs Res 2009;58(2):86–94. doi: 10.1097/NNR.0b013e31818fcea4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Im E-O, Chee W, Lim H-J, Liu W-M. An online forum exploring needs for help of patients with cancer: gender and ethnic differences. Oncol Nurs Forum 2008;35(4):653–660. doi: 10.1188/08.ONF.653-660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Im E-O, Liu Y, Kim YH, Chee W. Asian American cancer patients’ pain experience. Cancer Nurs 2008;31(3):E17–23. doi: 10.1097/01.NCC.0000305730.95839.83. [DOI] [PubMed] [Google Scholar]
- 36.Im E-O, Chee W. Decision support computer program for cancer pain management. Comput Inform Nurs 2003;21(1):12–21. [DOI] [PubMed] [Google Scholar]
- 37.Im E-O, Chee W. Evaluation of the decision support computer program for cancer pain management. Oncol Nurs Forum 2006;33(5):977–982. doi: 10.1188/06.ONF.977-982. [DOI] [PubMed] [Google Scholar]
- 38.Im E-O, Chee W, Guevara E, et al. Gender and ethnic differences in cancer pain experience: a multiethnic survey in the United States. Nurs Res 2007;56(5):296–306. doi: 10.1097/01.NNR.0000289502.45284.b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Im E-O. Online support of patients and survivors of cancer. Semin Oncol Nurs 2011;27(3):229–236. doi: 10.1016/j.soncn.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 40.Im E-O, Chee W, Lim H-J, Liu Y, Guevara E, Kim KS. Patients’ attitudes toward internet cancer support groups. Oncol Nurs Forum 2007;34(3):705–712. doi: 10.1188/07.ONF.705-712. [DOI] [PubMed] [Google Scholar]
- 41.Im E-O, Chee W. The DSCP-CA: a decision support computer program--cancer pain management. Comput Inform Nurs 2011;29(5):289–296. doi: 10.1097/NCN.0b013e3181f9dd23. [DOI] [PubMed] [Google Scholar]
- 42.Im E-O, Lee B, Chee W. The questions on the use of internet cancer support groups: instrument development. Comput Inform Nurs 2011;29(6):344–351. doi: 10.1097/NCN.0b013e3181fc3c97. [DOI] [PubMed] [Google Scholar]
- 43.Im E-O, Lee B, Chee W. The use of internet cancer support groups by Asian Americans and White Americans living with cancer. J Transcult Nurs 2011;22(4):386–396. doi: 10.1177/1043659611414142. [DOI] [PubMed] [Google Scholar]
- 44.Bandura A Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 45.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, CONSORT Group. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 2008;148(4):295–309. [DOI] [PubMed] [Google Scholar]
- 46.Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 47.Cohen J Statistical power analysis. Curr Dir Psychol Sci 1992;1(3):98–101. doi: 10.1111/1467-8721.ep10768783. [DOI] [Google Scholar]
- 48.Price M, Butow P, Kirsten L. Support and training needs of cancer support group leaders: a review. Psychooncology 2006;15(8):651–663. doi: 10.1002/pon.1009. [DOI] [PubMed] [Google Scholar]
- 49.Gotay CC, Moinpour CM, Unger JM, et al. Impact of a peer-delivered telephone intervention for women experiencing a breast cancer recurrence. J Clin Oncol 2007;25(15):2093–2099. doi: 10.1200/JCO.2006.07.4674. [DOI] [PubMed] [Google Scholar]
- 50.Kissane DW, Love A, Hatton A, et al. Effect of cognitive-existential group therapy on survival in early-stage breast cancer. J Clin Oncol 2004;22(21):4255–4260. doi: 10.1200/JCO.2004.12.129. [DOI] [PubMed] [Google Scholar]
- 51.Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity. a systematic review. Am J Prev Med 2002;22(4 Suppl):73–107. [DOI] [PubMed] [Google Scholar]
- 52.Perry C, Klepp K, Dubovitz B, Golden D, Griffin S. Promoting healthy eating and physical activity patterns among adolescents: a pilot study of “Slice of Life”. Health Educ Q 1987;2:93–103. [Google Scholar]
- 53.Davis S, Lambert L, Gomez Y, Skipper B. Southwest cardiovascular curriculum project: study findings for American Indian elementary students. J Health Educ 1995;26:S72–S81. [Google Scholar]
- 54.Holcomb JD, Lira J, Kingery PM, Smith DW, Lane D, Goodway J. Evaluation of Jump Into Action: a program to reduce the risk of non-insulin dependent diabetes mellitus in school children on the Texas-Mexico border. J Sch Health 1998;68(7):282–288. [DOI] [PubMed] [Google Scholar]
- 55.Armitage CJ. Can the theory of planned behavior predict the maintenance of physical activity? Health Psychol 2005;24(3):235–245. doi: 10.1037/0278-6133.24.3.235. [DOI] [PubMed] [Google Scholar]
- 56.Stuifbergen AK, Becker HA. Predictors of health-promoting lifestyles in persons with disabilities. Res Nurs Health 1994;17(1):3–13. [DOI] [PubMed] [Google Scholar]
- 57.Merluzzi TV, Martinez Sanchez MA. Assessment of self-efficacy and coping with cancer: development and validation of the cancer behavior inventory. Health Psychol 1997;16(2):163–170. [DOI] [PubMed] [Google Scholar]
- 58.Chang VT, Hwang SS, Feuerman M, Kasimis BS, Thaler HT. The memorial symptom assessment scale short form (MSAS-SF). Cancer 2000;89(5):1162–1171. [DOI] [PubMed] [Google Scholar]
- 59.Im E-O. The Midlife Women’s Symptom Index (MSI). Health Care Women Int 2006;27(3):268–287. doi: 10.1080/07399330500506600. [DOI] [PubMed] [Google Scholar]
- 60.Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS System for Mixed Models 2nd ed. Cary, NC: SAS Institute; 2006. [Google Scholar]
- 61.Bell BA, Ene M, Smiley W, Schoeneberger JA. A multilevel model primer using SAS PROC MIXED https://pdfs.semanticscholar.org/8364/cdd13d05f5dc5a7eba4bded4abac15cecdf0.pdf. Accessed July 1, 2018.
- 62.Im E-O, Lee Y, Chee E, Chee W. Web-based interventions for menopause: a systematic integrated literature review. Maturitas 2017;95:24–30. doi: 10.1016/j.maturitas.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 63.Glasgow RE, Toobert DJ, Gillette CD. Psychosocial barriers to diabetes self-management and quality of life. Diabetes Spectr 2001;14(1):33–41. doi: 10.2337/diaspect.14.1.33. [DOI] [Google Scholar]
- 64.Sward KA, Richardson S, Kendrick J, Maloney C. Use of a Web-based game to teach pediatric content to medical students. Ambul Pediatr 2008;8(6):354–359. doi: 10.1016/j.ambp.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 65.Park M-J, Kim H-S. Evaluation of mobile phone and Internet intervention on waist circumference and blood pressure in post-menopausal women with abdominal obesity. Int J Med Inf 2012;81(6):388–394. doi: 10.1016/j.ijmedinf.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 66.Bosak KA, Yates B, Pozehl B. Effects of an Internet physical activity intervention in adults with metabolic syndrome. West J Nurs Res 2010;32(1):5–22. doi: 10.1177/0193945909333889. [DOI] [PubMed] [Google Scholar]
- 67.Song M, Choe M-A, Kim KS, et al. An evaluation of Web-based education as an alternative to group lectures for diabetes self-management. Nurs Health Sci 2009;11(3):277–284. doi: 10.1111/j.1442-2018.2009.00458.x. [DOI] [PubMed] [Google Scholar]
- 68.Koivunen M, Välimäki M, Patel A, et al. Effects of the implementation of the web-based patient support system on staff’s attitudes towards computers and IT use: a randomised controlled trial. Scand J Caring Sci 2010;24(3):592–599. doi: 10.1111/j.1471-6712.2009.00755.x. [DOI] [PubMed] [Google Scholar]
- 69.Bossen D, Veenhof C, Dekker J, de Bakker D. The usability and preliminary effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis. BMC Med Inform Decis Mak 2013;13:61. doi: 10.1186/1472-6947-13-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Spector RE. Cultural diversity in health and illness. J Transcult Nurs 2002;13(3):197–199. doi: 10.1177/10459602013003007. [DOI] [PubMed] [Google Scholar]


