Abstract
Objective:
To examine the perceived value, benefits, drawbacks, and ideas for technology development and implementation of surface electromyography (sEMG) recordings in neurologic rehabilitation practice from clinical stakeholder perspectives.
Design:
A qualitative, phenomenological study was conducted. In-depth, semi-structured interviews and focus groups were completed. Sessions included questions about clinician perspectives and demonstrations of four sEMG systems to garner perceptions of specific system features.
Setting:
The study was conducted at four hospital systems in a large metropolitan area.
Participants:
22 adult and pediatric physical therapists, occupational therapists, and physiatrists from inpatient, outpatient, and research settings took part in the study.
Interventions:
Not Applicable
Main Outcome Measures:
Interviews and focus groups were audio-recorded, transcribed verbatim, then coded for analysis into themes.
Results:
Four major themes emerged. (1) Low-tech clinical practice and future directions for rehabilitation; (2) Barriers to sEMG uptake and potential solutions; (3) Benefits of sEMG for targeted populations; and 4) Essential features of sEMG systems.
Conclusion:
Surface EMG systems were not routinely utilized for assessment or intervention following neurologic injury. Despite recognition of potential clinical benefits of sEMG use, clinicians identified limited time and resources as key barriers to implementation. Perspectives on design and sEMG system features indicated the need for streamlined, intuitive, and clinically impactful applications. Further research is needed to determine feasibility and clinical relevance of sEMG in rehabilitation intervention.
Keywords: Surface Electromyography, Neurorehabilitation, Clinician Perspectives, Clinical Translation, Technology, Qualitative Research
Neurologic conditions are a ubiquitous healthcare issue across the world. In the US, nearly 800,000 individuals have a stroke each year, and globally, other neurologic conditions such as Parkinson disease, traumatic brain injury, brain tumors, and dementia impact 5000 individuals per 100,000 person-years1,2. Associated healthcare costs in the US of the most commonly identified neurologic conditions were recently reported at nearly $800 billion annually, with spending projected to increase as the population ages3. Factors such as socioeconomic status, co-morbid medical conditions, geographical location, lack of clinical trials, and an increasingly resource-limited healthcare climate have also been identified as challenges in neurologic rehabilitation practice4. Because of these challenges, ongoing research focused on improving long-term recovery and harnessing the potential of new technology in rehabilitation to support the health and participation of individuals affected by neurologic conditions is essential5.
Surface electromyography (sEMG) is one technology that has been suggested as a tool to enhance understanding and treatment of neurologic conditions5–11. Established in the 1940’s for muscle physiology research, sEMG was used throughout subsequent decades as a less-invasive alternative to needle EMG, applied to evaluate neuromuscular patterns across a wide range of applications from surgical decision-making to sports enhancement6,7,9,12–14. There is a growing body of evidence describing the use and utility of sEMG specifically with individuals with neurologic conditions, as well as a general sentiment in the literature that sEMG may be underutilized in clinical practice6,10,15. Existing research has demonstrated the utility of sEMG to aid in prognosticating long-term recovery, understanding muscle activity profiles and interlimb coordination, quantifying dynamic motor control parameters in gait, providing biofeedback, and tracking response to conservative rehabilitation or surgical intervention in adults and children with neurologic conditions 8,11,16–27.
Collectively, this evidence suggests that sEMG may be an important tool for understanding the underlying mechanisms of recovery and enhancing motor outcomes. However, translational use of sEMG in the clinic and community is limited6,10,28. Minimal research has considered the perspectives of clinicians or patients in implementing such tools and methods in clinical practice, and whether or not this type of wearable technology is justified 29,30. A gap in translational knowledge exists in understanding whether incorporating sEMG data might be useful for improved specificity, standardized rehabilitation intervention, or improved patient outcomes when compared to standard clinical care following neurologic injury. Further, it is important to understand if and how implementation of more traditionally lab-based technology may have a place in the clinic, as a benefit for both rehabilitation professionals as well as clinical populations. To begin addressing this gap, the purpose of this study was to qualitatively examine clinician-stakeholder perspectives of the current landscape of technology use in clinical rehabilitation environments, with a focus on the perceived value, benefits, and drawbacks of sEMG systems to support the evaluation and care of individuals with neurologic conditions.
Methods
A qualitative, phenomenological study was conducted using in-depth, semi-structured interviews and focus groups, which included demonstrations of four sEMG systems to garner perceptions of specific system features. This study was approved by the authors’ institutional review board. All participants gave written consent to take part in the study; pseudonyms are used for privacy and confidentiality. A researcher and physical therapist (HAF) with qualitative research expertise and no previous relationship to the participants led all research activities, and one assistant facilitated audio recordings and handwritten notes of each session. Using convenience sampling, clinicians were recruited from pediatric and adult rehabilitation settings within the Seattle metropolitan region. Inclusion criteria were: 1) age >18 years; 2) licensed healthcare provider; 3) currently working with adults or children with neurologic conditions; 4) proficiency communicating in English.
Using a phenomenological approach intended to both describe and interpret clinician perspectives, interviews and focus groups were conducted to obtain primary source thoughts, interpretations, and experiences individually or within a group of similar peers31–34. Semi-structured interview questions were developed into an interview guide, reviewed by the authors, edited until consensus of question content and order was reached, and piloted with one volunteer to ensure clarity (Figure 1). Three single interviews and five focus groups with two to eight participants were conducted at clinic sites over a span of six months.
Figure 1.
Sample Questions from Semi-Structured Interview Guide
This figure shows a sampling of the semi-structured interview questions that were prepared and delivered as a part of the interviews and focus groups for the study.
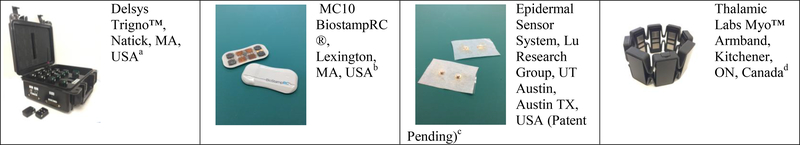
During each interview or focus group, a brief demonstration of four research lab-owned sEMG systems was performed. This included three commercially available and one lab-designed prototype, selected to demonstrate the range of systems and sensors: (1) Delsys Trigno™, Natick, MA, USA (a); (2) MC10 BiostampRC ®, Lexington, MA, USA (b); (3) Epidermal Sensor System, Lu Research Group, UT Austin, TX, USA. Patent Pending (c); and (4) Thalamic Labs Myo™ Armband, Kitchener, ON, Canada (d) (Figure 2). Participants were briefed on system cost, functions, interface, battery life/bandwith, skin preparation and placement, and raw signal images (Table 1). Feedback from the participants about the features of each system was solicited as a part of the interview or focus group responses.
Figure 2.
Sample Commercial and Lab-Based sEMG Sensors
This figure shows the four commercial and lab-based sEMG sensor systems that were used in a brief demonstration for the participants to garner their feedback on the features and functions of a variety of sEMG systems. These four systems are routinely used in the authors’ research labs.
Table 1.
Surface EMG feature comparison chart
| DELSYS Trigno™ a | MC10 Biostamp® b | EES Lu Research Group, UTAustin c | Thalamic Labs Myo™ Armband d | |
|---|---|---|---|---|
| Cost* | Wireless Lab > $20,000 Includes adhesives, software program, 16 sensors, AD cable, charger/USB cord. | Eval kit < $2000 Includes Tablet/software, charger, 3 sensors. Additional sensors & skin adhesive stickers <$1000 | Each sensor < $0.50 PCB Board TBD, targeted cost < $50.00 (materials cost only) No current software. | Myo gesture control armband < $300 Includes USB charging cord, extra sizing links, access to software. |
| Features | EMG, Accelerometer (both can be used together). Wireless. Functions within 20m of base station. | ECG, EMG, Accelerometer, Gyroscope. (2 functions can be concurrent) Water resistant 2m. Wireless. | Gold filament/snap electrode connections embedded in medical tape. Wireless. | EMG, accelerometer, gyroscope, and magnetometer. Detects hand gestures which are used to direct task. Wireless. |
| Interface | Wireless sensors send data to receiver on base station, connected via cable to PC. | Wireless sensors send data to tablet via blue tooth, data then uploaded to cloud via Wifi. | Individual PCB board snaps on directly to sensor. SD card built in to version 1, version 2 will use Bluetooth to upload data. | Wireless Bluetooth sends data to device- Mac, PC, or tablet (iOS and android). |
| Battery Life/Bandwith | Full charge operation time = 8 hrs | Rechargeable Li Ion Battery, Clinical Applications = 3 hrs | PCB has onboard battery with 24 hrs of recording capacity. | Rechargeable Li Ion battery Full charge operation time = 12 hrs |
| Skin Prep and placement | Shave skin area, then abrade with alcohol prep pad. After dry, use electrode spray, and place adhesive on sensor and then affix to skin. After use, remove adhesive and discard, use alcohol prep pad to clean sensor. | Soap and water to placement area, rub skin to increase bloodflow. Apply adhesive sticker to sensor, apply conductive gel to sensor, affix to desired body location. After use, wash sensor with soap and water. | Shave skin area, then abrade with alcohol prep pad. After dry, use electrode spray, and place adhesive on sensor and then affix to skin. After use, remove adhesive and discard. Tape electrodes will be tested for repeat use, but may be reusable up to three times. | None. |
| Multiple Electrodes & Individual Muscle Test | Multiple sensors can be used simultaneously. Individual muscles may be tested. | Multiple sensors can be used simultaneously. Individual muscles may be tested. | Multiple sensors can be used simultaneously. Individual muscles may be tested. | 8 sensors built in. Forearm only. Individual muscles may not be tested. |
Cost information is approximate and may require formal quoting process directly from sensor companies.
Interviews and focus groups were audio-recorded, de-identified, transcribed verbatim, and coded for analysis using constant comparison until data saturation was achieved and major themes emerged35. Data analysis was inductive, grounded in the participants’ experiences and perceptions, and responsive to the research questions33,35. A rich, ‘thick’ description of participant experiences, supported directly by verbatim quotations, allows credibility determination of the data to be reader-driven36. Following open and focused coding by the first author (HAF), content analysis was independently conducted by two additional authors (HAF and DH)37. A final review was conducted by four authors (HAF, SWM, VEK, and KMS) continuing to explore alternate coding interpretations and using consensus to ultimately agree on the final themes. Several participants also engaged in member checking, reviewing portions of their data to ensure accuracy and avoid misinterpretation33,35.
Results
Twenty-two participants across Seattle completed the study (Table 2). Professional experience ranged from 1.5 to 37 years (mean=14.5 (14.1)). Four major themes emerged, with greater than 90% agreement in thematic outcomes by the authors (Table 3).
Table 2.
Participant Demographics
| Demographic | Frequency |
|---|---|
| Gender | |
| Female | 86.3% (n = 19) |
| Male | 13.7% (n = 3) |
| Occupation | |
| Occupational Therapist | 59.0% (n=13) |
| Physical Therapist | 31.8% (n=7) |
| hysiatrist | 9.0% (n=2) |
| Racial/Ethnic Background | |
| Caucasian | 81.8% (n=18) |
| Asian | 9.0% (n=2) |
| Hispanic | 9.0% (n=2) |
| Practice Setting | |
| Adult | 69.2% (n=15) |
| Pediatric | 31.8% (n=7) |
| Inpatient (pediatric or adult) | 50.0% (n=11) |
| Outpatient (pediatric or adult) | 36.3% (n=8) |
| Research or Administration (pediatric or adult) | 13.7% (n=3) |
Table 3.
Coding Framework
| Quote | Open Coding | Focused Coding | Theme |
|---|---|---|---|
| “At the impairment level it’s usually like manual muscle testing, range of motion. As OT’s I think we look at functional achievements, you know, like they were able to reach a can on this shelf one day, but the next day they were able to reach the high shelf, things like that” | MMT, ROM, Functional Assessment, Tools of the Trade Reaching Height, Low Tech Equipment | Tools of the Trade, Low-tech Assessments | Low-Tech Clinical Practice |
| “And not to go back to the time management thing, but another one that we all struggle with is not just patient care and documentation and that stuff, but, um, any additional projects, you know, like working on any sort of presentations or research or CPR certification (laughs) - it’s hard to fit that in, so time is really a struggle” | Time Management, Patient Care Responsibilities, Documentation, Additional Projects, Research, CPR Training | Professional Duties, Limited Resources (Time) | Barriers to sEMG Uptake |
| “I do agree that right before [apatient’s] arm becomes functional, ‘I swear you’re gaining strength, you just have to trust me, I know you can’t use it yet, but…’ So I think it would be great [for them] to see the actual progress” | Return to Function, Trust between therapist and patient, seeing progress, gaining strength | Trust, Seeing Actual Change | Potential Clinical Benefits of sEMG |
| “I think [the tipping point] is evidence based enough to support the cost. Like, if you said you could buy this one for $200, but, eh, we don’t really know if it’s effective, or you could by the $2000 and research shows that would make a difference” | Buy-In from clinicians, evidencebased, cost of technology, clinical effectiveness | Evidence-Based Technology, Cost and Clinical Effectiveness | Essential Features of sEMG Technology |
Low-tech Clinical Practice
Most clinicians used little to no technology in general when evaluating or treating muscle function in adults and children with neurologic conditions. For assessment of muscle activity, most clinicians (n= 19) relied primarily on clinical observation of functional skills and kinematics, and used palpation, manual muscle testing and standardized outcome measures, noting their assessment choices were often based on time constraints and reimbursement considerations (Table 4, Quotes 1–3). Two thirds (n=14) of the clinicians reported using low-tech tools like analog dynamometers, theraband, supported task grading, and body-weight resistance for strength intervention. A minority of clinicians (n=5) reported using high-tech equipment for treatment, including functional electrical-stimulation bikes or portable handheld units; one therapist worked as a clinical trainer for a robotic exoskeleton company. Those clinicians with sEMG experience (n=3) noted that outside a research environment, their use of technology in clinical practice was limited (Quote 4). Clinicians acknowledged a desire to use more technology juxtaposed with implementation challenges like cost and comparative outcomes effectiveness (Quote 5). Some participants noted that one key to technology implementation is to train students to advocate for its use during educational and clinical experiences (Quote 6).
Table 4:
Themes, Descriptions, and Representative Quotes
| Theme | Description | Sub-theme/topic | Representative quotes |
|---|---|---|---|
| Low tech clinical practice | Comprises clinician perspectives on their primary tools for assessment of muscle activity, preferred interventions for muscle strengthening, use and knowledge of technology in practice, and future directions for clinical practice. | Clinical observation; muscle assessment tools; functional assessment | 1: “At the impairment level it’s usually like manual muscle testing, range of motion. As OT’s I think we look at functional achievements, you know, like they were able to reach a can on this shelf one day, but the next day they were able to reach the high shelf, things like that” (Laura, OT, Hospital A). |
| 2: “I use manual muscle test, that’s basically it. I feel like for me, especially when it comes to what is going to most broadly show, um, the greatest amount of improvement, and that insurance companies are going to look at and say, ‘ok, this treatment is justified’, in my mind, it should be something very functional.” (Jack, PT, Hospital D and private company). | |||
| 3: “Just manual muscle testing. And even at times, I get to a point where because of our 45- minute sessions run out so quickly, and when I’m doing functional tests or outcomes measures, I don’t really check strength at the end, because all I really care about is that they’re able to do stairs, that they are able to walk, they’re able to do things functionally” (Leah, PT, Hospital C). | |||
| Use of EMG restricted to research environments | 4: “I still do clinical practice, and I don’t think I’ve used anything to measure specific muscle activity other than manual muscle testing. Maybe grip strength testing, that’s the only thing I can think of. I just used EMG during our research” (Anna, OT, Hospital D). | ||
| Mixed desire to use more technology in practice | 5: “It seems like there are a lot of opportunities for technologies being leveraged, the logistics of how we are going to pay for that is another argument. But then, you know, I guess I’d be interested in knowing to what degree is the outcome different. If you get there faster but it’s still the same outcome, does it justify the cost?” (Jeff, PT, Hospital C). | ||
| Future impact and implementation of rehab technology | 6: “You should be using technological means to make some of these measurements to improve the sensitivity of what you’re measuring and document change across time with the therapy…But I don’t think the students, when they go out there to do their clinical internships and beyond, see those things being used very much and therefore they let it all go, rather than trying to change the profession. So, it’s something that I challenge our students to be- the change agents that take some of this technology and actually apply it in their clinical practice” (Julia, PT, Hospital D and academic researcher). | ||
| Barriers to EMG uptake | Comprises clinician perspectives on various barriers to implementation of sEMG technology in various clinical settings. | Personal: Lack of time and training | 7: “The hardest…not the hardest, but one of the hardest, [is] getting the most out of the 45- minute sessions we have with the patients” (Henley, OT, Hospital A). |
| 8: “It’s hard to fit [it all] in, so time is really a struggle” (Jasmine, OT, Hospital A). | |||
| Clinical experience and technology ‘savvy’ | 9: “I think one of the challenges I have as a new therapist is if I want to try a different modality or try a different treatment method, there’s not a lot of room for practice, and I find that if I don’t use it regularly or don’t have the chance to really practice with it until I’ve mastered it, I’m very unlikely to be able to grab- in my one hour treatment session, to run and grab the equipment, set it up, initiate it, explain it to the family, like, it just feels impossible, so I avoid using it” (Jessica, OT, Hospital B). | ||
| 10: “Anything technology is hard for me. I’m old, and it’s just, it just, it scares me and I, you know, I’m less likely to do stuff like [EMG] than... unless I had somebody with me. Because I just, we don’t have time to mess around with stuff, and I don’t have my own personal person to help me, you know” (Lauren, OT, Hospital B). | |||
| Availability of appropriate patient supports | 11: “Just by virtue of our demographic here, a lot of our patients simply don’t have a lot of resources…they don’t have consistently a lot of great family support, and so, discharge planning and getting equipment for them- you know, there is great technology available but a lot of times they can’t afford it, and then also, um, their [dispo] is often to rural places that they won’t necessarily have follow up, so that’s another challenge that we face with a lot of patients here” (Jasmine, OT, Hospital A). |
||
| Equipment: Current Technology design/function | 12: “It was difficult to even just get the electrodes to stay on for a 10-minute test, let alone an hour worth of intervention. It’s like, if I have to scrub the skin really, really hard, and then let it dry, and then wrap it with pre-wrap to keep it from falling off, it was too much” (Rob, PT, Hospital D). | ||
| 13: “That system right there looks like a Cold-War era black box…I don’t know how patients might react to that” (Richard, PT, Hospital C). | |||
| 14: “[The sensors] are chunky, it’s going to fall off unless you wrap an ace wrap around it or something” (Samantha, Physiatrist, Hospital C). | |||
| Institutional: Logistics; Layout; Willingness to invest in Technology | 15: “I have seen a lot of changes…the frustration with the changes are less and less number of visits to achieve desired results. And in the olden days- neuro patients change more slowly, we know that- and so they also tended to be allotted more time for their changes. And there were just more resources- dollar resources- for them so they could be seen for a longer period…[Another frustration] is fitting the diagnosis into the insurance driven market, essentially, and then the other frustration is just knowing that there are pieces of equipment available, and due to funding we just, you know, can’t get it” (Holly, OT, Hospital C). | ||
| Policy: Funding; Healthcare reform | 16: “[Technology] is not being something that really likely [is] reimbursed. I think there’s some, there are wonderful innovations but with the money being what it is, you know…Medicare is not of the mind to be spending any more money on anything, and as soon as you bring up new technology, they’ll say, ‘Show me the evidence,’ and then they’ll dispute the evidence. They’ll say it’s not good, it’s not robust enough so we’ll consider it experimental and we won’t pay for it” (Richard, PT, Hospital C). | ||
| 17: “And that is sort of the, like, kickoff for, like, consumer-based insurance or private insurances, that they’ll follow Medicare” (Jeff, PT, Hospital C). | |||
| Potential solutions to implementation barriers | 18: “We’ve discussed even doing trainings or practice with each other periodically to keep our skills up on the FES bike. And to find time to meet, I mean, we haven’t tried very hard, but I know that to find time for us two to meet and do that would be really challenging with our schedules. Cause that is one of those activities that I don’t just go, ‘Oh, let’s just run them up to the gym and put them on the FES bike’. I feel like, ‘Oh, I need to go there first, I need to remember the settings’, and you know, so…” (Charlotte, OT, Hospital B). | ||
| 19: “But I do think that the next generation, the generation we’re training now to become physical therapists, they’re so in tune with technology, and they’ve all got, you know, a fitbit, and apps on their phones and stuff. I think they’re primed to pick this stuff up and use it. The old guys out there, they’re never going to use it, so (laughter) let them go to retirement, you know. But this, I mean, we have an opportunity I think, because [the students] have grown up using this stuff” (Julia, PT, Hospital D). | |||
| Potentia Benefits of sEMG | Comprises clinician perspectives of how EMG technology may be a beneficial tool in their professional settings as well as a tool that they might recommend to individuals with neurologic injury as a part of their community reintegration. | Standardization of assessment; specific quantitative evidence | 20: “So, if [sEMG] was able to give me information that would drive the therapeutic exercise, or their orthotic [prescription], or the treadmill training, or their- we have body weight suspension capabilities within our clinic- knowing that we need to use that or not use that… so sort of like putting in the context of clinically-meaningful difference” (Jamie, PT, Hospital B). |
| 21: “I think it would be useful, I was thinking when you have kids, because they’re not reliable, necessarily, and they’re not necessarily motivated, right? So you could do a manual muscle test and I could and Julia could and probably get three different results, depending on the mood of the kid, how hard they were performing, and all our subjectivity. So I think that [sEMG] would actually be useful for a person, kids especially, if you’re just not sure what’s going on and you want to measure at that level. So you know exactly what’s going on with the muscles” (Anna, OT, Hospital D). | |||
| Non-invasive tool to demonstrate early progress | 22: “I think [EMG] would be really great for our super weak patients that have like the 1, 2- muscle strength and they’re having trouble distinguishing, maybe they’re working in a flexor synergy and you’re trying to tease out some muscles. I think it would be good feedback for them at that level. It’s hard because they don’t see themselves make these drastic movements, maybe they are only moving an inch, but this is something you could show them, ‘Look! Your muscles are firing!’” (Laura, Hospital A). | ||
| 23: “I do agree that right before [a patient’s] arm becomes functional, ‘I swear you’re gaining strength, you just have to trust me, I know you can’t use it yet, but…’ So I think it would be great [for them] to see the actual progress” (Joyce, OT, Hospital A). | |||
| Ability to monitor progress outside of therapy | 24: “I think that there’s a lot of benefit to something that we can use in the clinic and show them, so we can track through. For my populations, being able to see how they perform in a home setting would be really valuable- so if it’s something that we can train up with families, or show them some results to watch themselves, there’d be a lot of benefit to that” (Charlotte, OT, Hospital B). | ||
| Benefits vs. privacy concerns | 25: “Technology that could be applied in the home would be great. I always like to know what they’re doing when I’m not looking. If they have it on at home, and I can get to that information, or even information that they don’t have it on, I can go, ‘Hey, by the way, could you put it on?’ That kind of stuff. Versus them having it for a week and not knowing whether I’m getting any usable data or not. If I can go on every night and ping in and say, ‘Oh, ok, they wore it for six hours today, this is awesome.’ It’s sort of a big brother thing, which there are some challenges with that, obviously, but that would be very helpful” (Jamie, PT, Hospital B). | ||
| Patient enjoyment; interest in technology | 26: “I do think that all the participants, at least in the beginning, thought the technology was cool. ‘This is cool! This is better than that old therapy where you make me do all this stuff, this is cool!’” (Julia, PT, Hospital D). | ||
| 27: “I think [they enjoyed it] especially once they got the hang of it. I think in the beginning, especially the adults post-stroke, got frustrated, because they would get stuck and they couldn’t figure it out…and eventually they’d just stumble upon the right thing, and it was, obviously, that’s the point, right? Then it rewards and they just continued to do it” (Anna, OT, Hospital D). | |||
| 28: “I think the [bracelet EMG system] just looks cool I mean, I wear a fitbit, it’s kind of the next step up from that, it’s super functional, it looks like you can just pop it on and go” (Jasmine, OT, Hospital A). | |||
| Potential for more specific information in nebulous clinical situations | 29: “If I can’t get them to do a certain movement, I’m like, ‘Well, is there any activity in that muscle?’ That would be helpful to get that information in terms of assessing, ‘Oh, yeah, there’s a little bit here’, and then a couple of sessions later, ‘Hey, there’s a lot more activity’. I guess I can see myself tracking it that way, but, just based on the cost and setup time and all of that, I just want to make sure it’s something that’s super functional, worth the 45 minutes I have in the session” (Leah, PT, Hospital C). | ||
| 30: “I think [EMG] could add well to practice by giving you something that had a more objective and sensitive measurement system to document change. Small changes, maybe that you don’t see, to improve the sensitivity of what you’re measuring and document change across time with the therapy.” (Julia, PT, Hospital D). | |||
| 31. “I would also say, beyond just the sensitivity of the measure, but also improving the reliability of the measure, both inter- and intrarater reliability pieces…since there is so much subjective nature in a lot of what we do with assessments, trying to parse that into more objective measures and ability to improve the reliability of those measures.” (Rob, PT, Hospital D) | |||
| Essential features of sEMG systems | Comprises clinician perspectives on desirable or undesirable features of the currently available sEMG systems that were demonstrated during the research visits, as well as hypothetical ‘wish list’ features that clinicians deemed critical if they were |
Simplicity | 32: “Anything we can do to minimize the prep time, any steps we can do to make it easier to use, people will use it more readily” (Jack, PT, Hospital D and Private Company). |
| 33: “I would say we’d have to have something that’s less than five minutes. If I can go sticker, sticker, sticker, turn it on and go, then it would happen” (Jamie, PT, Hospital B). | |||
| Minimal skin preparation; multiple sizes, especially for pediatric populations | 34: “In a clinical situation if I brought out something that to me, kind of looks like a little rubber toy- a little piece of, uh, flexible rubber, and I wash their skin and I slap it on, that would be tolerated by most school-age kids, and/or kids with developmental disabilities better than if I had to abrade the skin, alcohol, rub… Any of that would be received- that’s not that far from what you do before you get a blood draw, and all of these kids, whether you’re typically developed or not, the minute- they may not- you can keep telling them that there’s no needle coming, there’s no pokes, but I can guarantee you the minute you start abrading a kid’s skin and wiping them down with alcohol, you’ve set them up to not be performing in their normal performance. And I think it would be hard for parents- to get parents to do that” (Jamie, PT, Hospital B). | ||
| Waterproof | 35: “They can stay for multiple days even through showers and swimming and bathing and everything else. If I had that technology, it would’ve been much easier and I think it would’ve been very, very much better in a lot of ways for both families and myself” (Rob, PT, Hospital D). | ||
| Low cost, disposable | 36: “It seems like the first two [Delsys and Biostamp] you could probably use during therapies but therapies only. I wouldn’t feel comfortable leaving them. Sometimes I’ve built up utensils and I am like, ‘Please don’t lose this’ and it’s gone within two hours. The [Myo] or the [ESS] could be left with the patient. I think it’s less likely the [Myo] would be thrown away, just cause it looks important, you know?” (Laura, OT, Hospital A). | ||
| Evidence-Based | 37: “When it comes to PT’s especially, if you’re able to – maybe these devices haven’t been used in specific studies that you can relate it to, but maybe other similar studies have been conducted- I think having those as a way to reference the direction it’s going, the application, and how it’s been beneficial in the past, that way they can kind of understand why they are using this kind of intervention” (Jack, PT, Hospital D and Private Company). | ||
| 38: “I think [the tipping point] is evidence-based enough to support the cost. Like, if you said you could buy this one for $200, but, eh, we don’t really know if it’s effective, or you could by the $2000 and research shows that would make a difference” (Joyce, OT, Hospital A). | |||
| Intuitive user interface; compatible with phone or tablet | 39: “Because of the things like iPads and iPhones, you can do all kinds of incredible things easily that we never had before the capability of doing that. You’d have to go to your supervisor and ask them for money and buy some big monster video camera and now, you can bring up your cell phone and, you know, take a video and do something with it, cause of the apps and [capabilities]” (Julia, PT, Hospital D). |
Barriers to EMG Uptake
Clinicians identified a wide range of perceived barriers that limited uptake of sEMG and other high-tech tools into the clinical environment at personal, institutional, and national policy levels. At the personal level, all the clinicians (n=22) noted the lack of time and training available to implement new clinical practices (Quotes 7–8). Most clinicians (n= 18) reported they received very little training specific to sEMG systems during professional curricula, and of those that did, none felt confident using sEMG in their current practice. Clinicians acknowledged their experience levels as a potential barrier- newer graduates pointed to a need for practice, while seasoned clinicians pointed to a lack of ‘tech savvy’ in learning new systems (Quotes 9–10). Even if technology is available to use in the clinic, participants indicated that a lack of appropriate supports to ensure successful application of technology make justification challenging (Quote 11).
At an equipment level, aesthetics, set-up time, functional carry over, and functionality in multiple environments were commonly noted sEMG limitations (Quotes 12–14). On an institutional level, perceived barriers included facility layout, ‘convincing’ department administration to invest in technology under ever-tightening budgets in resource-limited environments, and providing evidence to support return-on-investment, including costs and maintenance of equipment and staff training (Quote 15). From a policy perspective, clinicians with administrative roles spoke to larger challenges with rehabilitation funding given overarching government healthcare policies and resulting impacts on clinical practice and resources (Quotes 16–17).
Clinicians identified potential solutions to these barriers, such as forging new partnerships with community-based health and fitness initiatives where technology is more mainstream, access to practice time with ‘clinic technology champions’ (Quote 18), and empowering students to bring their technological savvy into the clinic to facilitate uptake into practice (Quote 19).
Potential Benefits of sEMG
All clinicians verbalized potential or actual benefits of EMG. Most clinicians (n=20) spoke to the potential of sEMG in prognosticating recovery, providing specific quantitative evidence for or against treatment decisions, and providing secondary information (Quote 20). Pediatric clinicians (n=7) spoke about the standardization that sEMG technology could provide for children (Quote 21). Several clinicians (n=8) felt that sEMG could be an encouraging and noninvasive tool to show early progress, especially at a time when discouragement could be high (Quotes 22–23). About a third (n= 8) of clinicians brought up the benefit of tracking patients’ progress outside of therapy, either during hospital downtime or at home in their community, although some clinicians brought up tensions in doing so regarding patient privacy (Quotes 2425).
Clinicians experienced with sEMG noted patients’ enjoyment during biofeedback training (Quotes 26–27). Following demonstrations, clinicians without sEMG experience also anticipated some systems and features as potentially interesting to patients (Quote 28) or having the potential to provide further objective clinical information in nebulous treatment situations (Quotes 29–31). About half the clinicians (n=12) spontaneously identified patient populations who might benefit from sEMG technology use in clinical and/or home use applications, including individuals with stroke, cerebral palsy, Amyotrophic Lateral Sclerosis or Multiple Sclerosis, pediatric cancers, spinal cord injury, amputation, or conversion disorders. While most clinicians saw applicability in both assessment and intervention, biofeedback was the most frequently mentioned clinical application.
Essential Features of sEMG Systems
Clinicians outlined features they found desirable or undesirable in the currently available sEMG systems, and a hypothetical ‘wish list’ features deemed critical for translation. Simplicity was a top priority for all clinicians (n=22), in terms of clinical use and clinician training (Quotes 32–33). Most clinicians (n=18) preferred a soap and water approach for skin preparation, especially in pediatric populations (Quote 34). Waterproof features and advances in lower-profile sensors were noted by all the experienced sEMG users (n=3) and most of the inexperienced users (n = 17) as essential technology developments (Quote 35). Cost concerns, fear of loss, and lack of disposability were reported as undesirable features by nearly all of clinicians (n=20) (Quote 36).
All pediatric practitioners (n=7) asked about multiple sensor sizes and adjustability, and all PT participants (n=7) asked if the Myo™ d armband could be worn on the lower extremity. Clinicians also reported a greater likelihood of sEMG technology use if a more robust evidence base and direct linkages to normative values or meaningful clinical outcomes existed for their patient populations (Quotes 37–38). Clinicians spoke about an intuitive user interface, preferring a tablet or mobile phone application that provided meaningful real-time or post-intervention information. Although no single sEMG system had every desired feature, advancements in technology and the ability to use everyday tools as tracking platforms were features mentioned that enhanced the promise of sEMG as a relevant clinical rehabilitation tool (Quote 39).
Discussion
Literature suggests that sEMG is a valuable, non-invasive research tool to assess neuromuscular conditions following injury and throughout the recovery process, however, there has not been translation of this work into routine neurorehabilitation practice38. Thus, it is essential to understand the perspectives, barriers, demands, and key features required by clinicians, as one group of primary stakeholders, to understand if translation into rehabilitation settings is feasible or beneficial for enhancing clinical outcomes.
The four themes that emerged from this study are an instructive step in addressing this gap. For example, results within low tech clinical practice reflect a similar lack of uptake of sEMG applications from bench to bedside previously noted by other authors 6,10,38. Professional development literature notes the fluid use of low-tech clinical tools as a hallmark of rehabilitation practice expertise39. However, the participants’ desire to use technology to elevate specificity and standardization in neurorehabilitation has not been widely addressed. Thus, while not surprising that the participants in this study reported minimal technology use despite following accepted clinical standards, these data represent an important next step in investigating the potential roles and benefits of incorporating technologies like sEMG to advance outcomes in rehabilitation.
Barriers to sEMG uptake highlighted similar challenges in implementing change in clinical practice that have been previously identified at individual, organizational, institutional, and policy levels40–43. While rehabilitation clinicians value formal continuing education, opportunities to pursue it have been called inadequate due to economic, temporal, and administrative resource limitations43. Even when opportunities for knowledge or skill development occur, such as during professional rehabilitation education, participants noted a ‘use it or lose it’ mentality, expressing discomfort incorporating unfamiliar modalities44. Ultimately, participants’ desire for more rigorous and clear evidence highlighting the benefits of sEMG within clinical and community environments reflects the ongoing professional mandate for improving evidence-based rehabilitation over the past two decades40,45. The potential solutions offered by participants to guide future research and clinical translation of sEMG such as ‘technology champions’ that could serve as a designated expert or referral source or a bottom-up approach of training rehabilitation students to incorporate their ‘tech-savvy’ into professional practice, are consistent with previously suggested approaches in the literature to enhance the presence and use of technology in clinical environments45–47.
Despite barriers, participants were eager to learn about, interact with, and assess the Potential clinical benefits of sEMG, noting that sEMG would not necessarily replace but enhance their current clinical methods and measures and potentially increase interest and motivation from their patients. These findings support previous literature on the role of sEMG in biofeedback applications to facilitate motivation in rehabilitation22,24,48. Participants stressed that results of sEMG use must provide a distinct, clinically relevant, and functional benefit, especially given the direction of rehabilitation practice away from impairment-level foci toward more holistic activity and participation level changes. This perspective is somewhat supported by previous sEMG literature, but also provides new insight into how to better translate sEMG findings into clinically relevant applications4,6,8.
Clinicians identified essential features of sEMG systems that would increase their likelihood of using sEMG systems in neurologic rehabilitation. Simplicity of the system and data interpretation, ease of set up, and ultimate clinical relevance were key cornerstones to support future translation. No single currently available commercial or lab-designed sEMG system met all the criteria discussed by the participants, but desirable aggregate features were noted. Aligning with recent literature that noted the importance of flexible sensor design and capability across environments and improved precision over existing technologies, participants proposed a mobile phone application, which could blend the precision of rehabilitation technology with the aesthetic of wearable lay technologies like fitness trackers49. Very few qualitative studies have examined perceptions of wearable sensor acceptability, but issues of comfort, aesthetic, and willingness to wear the sensor in public were key findings mirrored in this study29,50,51.
Limitations and Future Directions
Qualitative methods are not designed to be generalized to larger populations. Given the regional focus, the trends and perspectives captured in these data may not represent perceptions or practice patterns across the wider rehabilitation field. Attempts were made to mitigate this by including a variety of participants from diverse professional settings, however larger studies are needed. Since sEMG is primarily a research tool, limited clinical exposure was anticipated, thus the research team included a standardized demonstration of sEMG features prior to asking for participant perceptions, however, future studies should recruit experienced clinicians also. Finally, to fit into clinical schedules, the demonstrations included a basic ‘show and tell’, signal printouts, and a feature comparison chart. While clinicians could physically and visually inspect each system, they could not appraise the real-time set up or implementation processes, which could have affected responses. Future research should include immersion in clinical practice settings to observe clinical behaviors, real-time setup and system demonstration, as well as a readiness to change survey, to determine the likelihood of sEMG technology incorporation in various rehabilitation settings49.
This line of inquiry will next extend to individuals with neurologic conditions and their caregivers to gain end-user perspectives on sEMG technology, evaluate its potential to support community re-integration goals, and determine how clinician and end-user perspectives may align. Ultimately, the goal of future inquiry should inform technology development and testing of wearable sEMG systems and seek ways to harness technology to improve functional outcomes of individuals with neurological conditions.
Conclusion
Surface EMG systems are not routinely utilized by clinicians in inpatient or outpatient settings for assessment or treatment of muscle activity following neurologic injury. Despite recognition of potential clinical benefits of sEMG use, clinicians identified the need for a streamlined, intuitive, and clinically impactful application that is not yet wholly achieved by current systems. Wearable sensor technology has become mainstream for tracking fitness and activity, but current technology is not well-linked to rehabilitation-specific needs and outcomes. Surface EMG systems have the potential to inform clinical practice, but to achieve uptake by clinicians and patients, sensors and interfaces must be accurate, intuitive, unobtrusive, and generate feedback that is meaningful and accessible to all stakeholders. This research provides foundational insights on the feasibility and clinical relevance of current muscle tracking and training technology from the perspective of rehabilitation professionals who aim to improve recovery and community participation after neurologic injury.
Acknowledgments
The authors would like to thank the participants and their professional organizations/facilities for their willingness to share their perspectives, and Jacque Li for her assistance with data transcription. This project was funded by the National Institutes of Health, National Institute of Biomedical Imaging and Bioengineering, R01EB021935.
Dr. Kelly reports grants from National Institutes of Health during the conduct of the study and personal fees from Sage Bionetworks, outside the submitted work. The other authors have no conflicts of interest to disclose.
List of Abbreviations:
- EMG
Electromyography
- sEMG
Surface Electromyography
- US
United States
Footnotes
The data contained in this manuscript were presented to physical therapists during a Neurology Section poster presentation at the American Physical Therapy Association Combined Sections Meeting in New Orleans, LA on February 24, 2018.
Suppliers
The following products were purchased from manufacturers for use in this and other studies, with the exception of the Epidermal Sensor Systemc units, which have been built and provided by our university research partner.
a. Delsys Trigno™, Natick, MA, USA. https://www.delsys.com/products/wireless-emg/
b. MC10 BiostampRC ®, Lexington, MA, USA. https://www.mc10inc.com/ourproducts/biostamprc
c. Epidermal Sensor System, Lu Research Group, UT Austin, Austin TX, USA. Patent Pending. http://lu.ae.utexas.edu/
d. Thalamic Labs Myo™ Armband, Kitchener, ON, Canada. https://www.myo.com/
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.The American Stroke Association. Impact of Stroke. 2017; http://www.strokeassociation.org/STROKEORG/AboutStroke/Impact-of-Stroke-Strokestatistics_UCM_310728_Article.jsp#.WgyKt2iPLD4 Accessed 11/15/17, 2017.
- 2.Pringsheim T, Fiest K, Jette N. The international incidence and prevalence of neurologic conditions How common are they? Neurology. 2014;83(18):1661–1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gooch CL, Pracht E, Borenstein AR. The burden of neurological disease in the United States: a summary report and call to action. Annals of neurology. 2017;81(4):479–484. [DOI] [PubMed] [Google Scholar]
- 4.Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery. Stroke. 2016;47(6):e98–e169. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Neurological disorders: public health challenges. World Health Organization; 2006. [Google Scholar]
- 6.Cram JR. The history of surface electromyography. Applied psychophysiology and biofeedback. 2003;28(2):81–91. [DOI] [PubMed] [Google Scholar]
- 7.Scheving LE, Pauly JE. An electromyographic study of some muscles acting on the upper extremity of man. The Anatomical Record. 1959;135(4):239–245. [DOI] [PubMed] [Google Scholar]
- 8.Twitchell TE. The restoration of motor function following hemiplegia in man. Brain. 1951;74(4):443–480. [DOI] [PubMed] [Google Scholar]
- 9.Wolf S, Basmajian J. Assessment of paraspinal electromyographic activity in normal subjects and in chronic back pain patients using a muscle biofeedback device. International series on biomechanics VIB. 1978:319–324. [Google Scholar]
- 10.Hogrel J-Y. Clinical applications of surface electromyography in neuromuscular disorders. Neurophysiologie Clinique/Clinical Neurophysiology. 2005;35(2):59–71. [DOI] [PubMed] [Google Scholar]
- 11.Dewald JP, Pope PS, Given JD, Buchanan TS, Rymer WZ. Abnormal muscle coactivation patterns during isometric torque generation at the elbow and shoulder in hemiparetic subjects. Brain. 1995;118(2):495–510. [DOI] [PubMed] [Google Scholar]
- 12.Inman VT, Abbott LC. Observations on the function of the shoulder joint. JBJS. 1944;26(1):1–30. [DOI] [PubMed] [Google Scholar]
- 13.Wolf SL, Binder-Macleod SA. Electromyographic biofeedback applications to the hemiplegic patient: changes in upper extremity neuromuscular and functional status. Physical Therapy. 1983;63(9):1393–1403. [DOI] [PubMed] [Google Scholar]
- 14.Konrad P The abc of emg. A practical introduction to kinesiological electromyography. 2005;1:30–35. [Google Scholar]
- 15.Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders E-Book: Clinical-Electrophysiologic Correlations (Expert Consult-Online). Elsevier Health Sciences; 2012. [Google Scholar]
- 16.Hawe RL, Dewald JP. Development of a method to quantify inter-limb coupling in individuals with hemiparetic stroke. Paper presented at: Engineering in Medicine and Biology Society (EMBC), 2015 37th Annual International Conference of the IEEE2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller LC, Dewald JP. Involuntary paretic wrist/finger flexion forces and EMG increase with shoulder abduction load in individuals with chronic stroke. Clinical Neurophysiology. 2012;123(6):1216–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Butler EE, Steele KM, Torburn L, Gamble JG, Rose J. Clinical motion analyses over eight consecutive years in a child with crouch gait: a case report. Journal of medical case reports. 2016;10(1):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steele KM, Rozumalski A, Schwartz MH. Muscle synergies and complexity of neuromuscular control during gait in cerebral palsy. Developmental Medicine & Child Neurology. 2015;57(12):1176–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Damiano DL, Arnold AS, Steele KM, Delp SL. Can strength training predictably improve gait kinematics? A pilot study on the effects of hip and knee extensor strengthening on lower-extremity alignment in cerebral palsy. Physical therapy. 2010;90(2):269–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz MH, Rozumalski A, Steele KM. Muscle synergy complexity is related to selective motor control in cerebral palsy. Gait & Posture. 2014;39:S40. [Google Scholar]
- 22.Barreca S, Wolf SL, Fasoli S, Bohannon R. Treatment interventions for the paretic upper limb of stroke survivors: a critical review. Neurorehabilitation and neural repair. 2003;17(4):220–226. [DOI] [PubMed] [Google Scholar]
- 23.Huang H, Wolf SL, He J. Recent developments in biofeedback for neuromotor rehabilitation. Journal of neuroengineering and rehabilitation. 2006;3(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolf S, Baker M, Kelly J. EMG biofeedback in stroke: a 1-year follow-up on the effect of patient characteristics. Archives of physical medicine and rehabilitation. 1980;61(8):351–355. [PubMed] [Google Scholar]
- 25.Wolf SL. Electromyographic biofeedback applications to stroke patients: a critical review. Physical therapy. 1983;63(9):1448–1459. [DOI] [PubMed] [Google Scholar]
- 26.Brown EVD, McCoy SW, Fechko AS, Price R, Gilbertson T, Moritz CT. Preliminary investigation of an electromyography-controlled video game as a home program for persons in the chronic phase of stroke recovery. Archives of physical medicine and rehabilitation. 2014;95(8):14611469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Betker A, Szturm T, Moussavi Z. Development of an interactive motivating tool for rehabilitation movements. Paper presented at: Engineering in Medicine and Biology Society, 2005. IEEE-EMBS 2005. 27th Annual International Conference of the2006. [DOI] [PubMed] [Google Scholar]
- 28.Damiano DL, Quinlivan JM, Owen BF, Payne P, Nelson KC, Abel MF. What does the Ashworth scale really measure and are instrumented measures more valid and precise? Developmental medicine and child neurology. 2002;44(2):112–118. [DOI] [PubMed] [Google Scholar]
- 29.Fisher JM, Hammerla NY, Rochester L, Andras P, Walker RW. Body-worn sensors in Parkinson’s disease: evaluating their acceptability to patients. Telemedicine and e-Health. 2016;22(1):63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pals RA, Hansen UM, Johansen CB, et al. Making sense of a new technology in clinical practice: a qualitative study of patient and physician perspectives. BMC health services research. 2015;15(1):402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kramer JM, Hammel J. “I Do Lots of Things”: Children with cerebral palsy’s competence for everyday activities. International Journal of Disability, Development and Education. 2011;58(2):121–136. [Google Scholar]
- 32.Thomas N, O’kane C. The ethics of participatory research with children. Children & society. 1998;12(5):336–348. [Google Scholar]
- 33.Ulin P, Robinson E, Tolley E. Qualitative methods in public health: a field guide for applied research..San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- 34.Davidsen AS. Phenomenological approaches in psychology and health sciences. Qualitative research in psychology. 2013;10(3):318–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Merriam SB, Tisdell EJ. Qualitative research: A guide to design and implementation. Hoboken, NJ: John Wiley & Sons; 2015. [Google Scholar]
- 36.Jensen GM, Gwyer J, Shepard KF, Hack LM. Expert practice in physical therapy. Physical therapy. 2000;80(1):28–43. [PubMed] [Google Scholar]
- 37.Fujiura GT. Perspectives on the Publication of Qualitative Research. Intellectual and developmental disabilities. 2015;53(5):323–328. [DOI] [PubMed] [Google Scholar]
- 38.Woodford HJ, Price CI. EMG biofeedback for the recovery of motor function after stroke. The Cochrane Library. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jensen G, Gwyer J, Hack L, Shepard K. Expertise in physical therapy practice. Elsevier Inc.; 2007. [Google Scholar]
- 40.Jette DU, Bacon K, Batty C, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Physical therapy. 2003;83(9):786–805. [PubMed] [Google Scholar]
- 41.Swinkels RA, van Peppen RP, Wittink H, Custers JW, Beurskens AJ. Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. BMC musculoskeletal disorders. 2011;12(1):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Physical therapy. 2016;89(2):125–135. [DOI] [PubMed] [Google Scholar]
- 43.Rappolt S, Tassone M. How rehabilitation therapists gather, evaluate, and implement new knowledge. Journal of Continuing Education in the Health Professions. 2002;22(3):170–180. [DOI] [PubMed] [Google Scholar]
- 44.Childs S, Blenkinsopp E, Hall A, Walton G. Effective e-learning for health professionals and students—barriers and their solutions. A systematic review of the literature—findings from the HeXL project. Health Information & Libraries Journal. 2005;22(s2):20–32. [DOI] [PubMed] [Google Scholar]
- 45.Jette AM. Overcoming Ignorance and Ineptitude in 21st Century Rehabilitation. Oxford University Press; 2017. [DOI] [PubMed] [Google Scholar]
- 46.Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. Jama. 2011;306(9):978–988. [DOI] [PubMed] [Google Scholar]
- 47.Walker MF, Fisher RJ, Korner-Bitensky N, McCluskey A, Carey LM. From what we know to what we do: translating stroke rehabilitation research into practice. International Journal of Stroke. 2013;8(1):11–17. [DOI] [PubMed] [Google Scholar]
- 48.Huang H, He J, Wolf SL. Recent developments in biofeedback for neuromotor rehabilitation. Journal of neuroengineering and rehabilitation. 2006;3(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Olugbade T, Berthouze N, Marquardt N, Williams A. Human Observer and Automatic Assessment of Movement Related Self-Efficacy in Chronic Pain: from Exercise to Functional Activity. IEEE Transactions on Affective Computing. 2018. [Google Scholar]
- 50.McNaney R, Vines J, Roggen D, et al. Exploring the acceptability of google glass as an everyday assistive device for people with parkinson’s. Paper presented at: Proceedings of the 32nd annual ACM conference on Human factors in computing systems2014. [Google Scholar]
- 51.Taylor-Piliae RE, Mohler MJ, Najafi B, Coull BM. Objective fall risk detection in stroke survivors using wearable sensor technology: a feasibility study. Topics in stroke rehabilitation. 2016;23(6):393–399. [DOI] [PubMed] [Google Scholar]