Abstract
Objective:
To assess whether indicators of limited access to services explained changes in second-trimester abortion after implementation of a restrictive abortion law in Texas.
Methods:
We used cross-sectional vital statistics data on abortions performed in Texas before (November 1, 2011-October 31, 2012) and after (November 1, 2013-October 31, 2014) implementation of Texas’ abortion law. We conducted monthly mystery client calls for information about abortion facility closures and appointment wait times to calculate distance from women’s county of residence to the nearest open Texas facility, the number of open abortion facilities in women’s region of residence (facility network size), and days until the next consultation visit. We estimated mixed-effects logistic regression models to assess the association between obtaining abortion care after the law’s implementation and having a second-trimester abortion (≥12 weeks of gestation), following adjustment for distance, network size, and wait times.
Results:
Overall, 64,902 Texas-resident abortions occurred in the period before the law was introduced and 53,174 occurred after its implementation. After implementation, 14.5% of abortions were performed ≥12 weeks of gestation, compared with 10.5% before the law (p<.001; unadjusted odds ratio [OR] 1.45; 95% CI: 1.40–1.50). Adjusting for distance to the nearest facility and facility network size reduced the odds of having a second-trimester abortion after implementation (OR: 1.17; 95% CI: 1.10–1.25). Women living 50–99 miles from the nearest facility (versus <10 miles) had higher odds of second-trimester abortion (OR: 1.24; 95% CI: 1.11–1.39), as did women in regions with <1 facility per 250,000 reproductive-aged women compared with women in areas that had ≥1.5 facilities (OR: 1.57; 95% CI: 1.41–1.75). After implementation, women waited one to 14 days for a consultation visit; longer waits were associated with higher odds of second-trimester abortion.
Conclusions:
Increases in second-trimester abortion after the law’s implementation were due to women having more limited access to abortion services.
Précis
Second-trimester abortion increased after implementation of a restrictive state law due to women having more limited access to abortion services.
Introduction
State-level abortion regulations have increased since 2011,1 which make it difficult for women to access care in early pregnancy. In July 2013, Texas enacted an omnibus abortion law, House Bill 2 (HB 2). The law had four provisions: physicians providing abortion had to have admitting privileges at a hospital within 30 miles of the facility; the provision of medication abortion had to follow the US Food and Drug Administration-approved label for mifepristone; most abortions after 20 weeks’ post-fertilization were prohibited; and all abortion facilities had to meet ambulatory surgical center (ASC) standards. The first three provisions went into effect by November 1, 2013. The ASC provision was enforced briefly in October 2014 before the US Supreme Court temporarily blocked enforcement.
The number of Texas facilities providing abortion declined from 41 to 19 following the law’s passage and implementation.2 The total number of abortions decreased by 17% from 2012 to 2014, and the decrease was greater in counties where women needed to travel farther to an open facility.3 State vital statistics from 2014 documented an increase in second-trimester abortion compared to prior years.4 This is concerning since later abortion, although safe, is associated with a higher risk of complications; it is also more expensive and fewer facilities offer the service.5–7
We calculated the change in second-trimester abortion following implementation of HB 2. Facility closures and provider shortages may have contributed to increases in second-trimester abortion; therefore, we also examined whether indicators of limited access to services accounted for changes observed.
Methods
This study draws on three data sources: annual vital statistics data, mystery client calls to abortion facilities and county-level population estimates from the American Community Survey. We obtained individual-level vital statistics data on abortions performed in Texas each year between 2011 and 2014 from the Texas Department of State Health Services. These annual data included information on a woman’s age, race or ethnicity, number of previous live births, county of residence, date of abortion, gestational age at the time of abortion, and type of abortion. Information on the location where a woman obtained her abortion was not provided.
Since 2012, we have tracked the number and location of Texas facilities providing abortion and dates clinics closed by collecting and confirming information through interviews with clinic staff, requests to the Department of State Health Services on licensed facilities, and reports in the press. Beginning in January 2014, we also started conducting monthly mystery client calls to all facilities that were open in July 2013, when the Texas legislature passed HB 2, or that opened subsequently. The purpose of the calls was to determine whether the facility was providing abortion and the number of days until the next available appointment for the consultation and ultrasound visit, which was required at least 24 hours prior to a woman’s abortion following a 2011 Texas law. Female research assistants posing as women seeking information about abortion services called facilities during regular business hours in the middle of each month. They made up to four calls the same day to reach someone at the facility; if no one answered, the research assistant called twice the following day. We considered the facility closed if clinic staff did not answer the phone on two consecutive days, the call was rerouted to another facility, the phone number was no longer in service, or if there was a voicemail message that confirmed the clinic was closed. The research assistants entered onto a standardized form information about whether the clinic was open or closed and, if open, days until the next available consultation appointment. The institutional review boards at the authors’ universities approved all components of the study and Texas Department of State Health Services approved the use of vital statistics data.
Our primary outcome was the occurrence of abortions in the second trimester of pregnancy, which we defined as any procedure occurring at or after 12 weeks from last menstrual period (LMP), given that cervical preparation is often used at this gestational age.8 Prior to 2014, facilities reported gestational age by weeks from LMP. In 2014, Texas required facilities to begin reporting abortions based on weeks post-fertilization, the measurement used for dating pregnancies in HB 2. To account for this change in reporting, we estimated gestational age at the time of abortion by adding two weeks to post-fertilization age for all abortions taking place in 2014.
We assessed the service environment by focusing on three indicators of access: accessibility of services, measured as distance to facilities; availability of services (size of the facility network in a region); and ability of open facilities to accommodate women seeking care (number of days to appointments, or timeliness of care).9
To measure the one-way distance women may have traveled for care, we used the population-weighted centroid of women’s county of residence as their starting location.10 We did not know the location where women obtained care because this information was not included in the vital statistics data we received. Based on a 2014 survey of abortion clients,2 we found that 73% of women seeking care at Texas abortion facilities traveled to their nearest open facility or obtained care within 10 miles of that facility. Therefore, in these analyses, we assumed women traveled to the nearest open Texas facility. We estimated the distance to women’s nearest facility by computing the driving distance between their starting location and the location of all Texas facilities that were open on the date of their abortion, using Open Source Routing Machine 4.911 and our records of the date of facility closures, and identifying the smallest value. Based on a visual inspection of a LOWESS plot, we categorized one-way distance as less than 10 miles, 10 to 49 miles, 50 to 99 miles, and ≥100 miles. We differentiated women living ≥100 miles from a facility (versus <100 miles) because the mandatory waiting period between the consultation and procedure for these women is reduced from 24 to two hours.
To estimate the size of the facility network in a woman’s region of residence, we divided the number of open facilities in each of Texas’ eight health service regions by the region’s population of women aged 15 to 44 years, using five-year estimates from the 2011–2015 American Community Survey. We then multiplied this value by 250,000 women to create a measure that would be comparable across regions and would account for differences in the impact of the number of facilities that closed and population size of reproductive-aged women in potential need of services. We re-calculated the relative size of the network in a region at each time point that a facility closed (or opened). By linking a woman’s county of residence to the health service region, we determined the size of the facility network in the area on the date of her abortion. Based on a visual inspection of a LOWESS plot and distribution of observations in the pre- and post-policy periods, we categorized the regional network size as <1 facility per 250,000 women, 1 to 1.4 facilities, and ≥1.5 facilities.
We estimated the timeliness with which women were likely to receive care using data from the mystery client calls on the number of days until the next available consultation visit (i.e., wait time). First, we computed the average wait time each month in a metropolitan area by summing the number of days until the next available consultation at all facilities in the area and dividing that value by the total number of open facilities in the area that month. Because we did not begin the mystery calls until January 2014, we used open facilities’ January data to approximate wait times in November and December 2013. Mystery client calls were not conducted in May 2014; therefore, we estimated the May wait time using the average number of days to schedule a consultation visit in April and June 2014. To minimize sampling variation, we created a moving average for each metropolitan area using three months of data that included one month on either side of the index month. For example, the average wait time in a metropolitan area in February 2014 was estimated using the number of days until the next available consultation visit reported in January, February and March. Finally, we used quartiles to categorize the expected number of days until the next consultation visit in a woman’s nearest metropolitan area in the month of her abortion: <3 days, 3 to 4 days, 5 to 9 days, ≥10 days.
We compared changes that occurred in the year after the law was implemented (November 1, 2013-October 31, 2014) with a matched 12-month period before HB 2 was introduced (November 1, 2011-October 31, 2012). We chose this timeframe for the comparison period because any changes that occurred in the service environment were unlikely due to the anticipated impacts of abortion regulations proposed in the 2013 legislative session. We compared the mean gestational age at abortion in each period, using t-tests, and computed the distribution of abortions, according to procedure type and gestational age (medication <12 weeks, surgical <12 weeks, any procedure 12–15 weeks, any procedure ≥16 weeks). We also computed the total number of abortions and percentage of abortions performed ≥12 weeks of gestation, overall and by women’s age (<18 years, 18–24, 25–29, ≥30), race or ethnicity (Hispanic, White, Black, Asian, other or unknown), number of previous live births (0, 1 to 2, ≥3), one-way distance to the nearest Texas facility, and facility network size in a woman’s region of residence. In each period, we assessed demographic differences in second-trimester abortion using chi-squared tests.
To assess the association between receiving abortion care after implementation of HB 2 and obtaining an abortion ≥12 weeks of gestation, we used mixed-effects logistic regression, which enabled us to account for the clustering of observations within counties. We estimated three nested models to examine the change in the association between the policy periods and second-trimester abortion. Model 1 adjusted for women’s demographic characteristics (i.e., age, race or ethnicity, number of live births) that have been associated with obtaining abortion care later in pregnancy in other studies.12,13 Model 2 included additional adjustments for one-way distance to the nearest open Texas facility at the time of a woman’s abortion. Model 3 adjusted for the variables in Model 2 and the facility network size in a woman’s region of residence at the time of her abortion. We conducted mediation analyses to determine the degree to which demographic characteristics, distance and facility network size explained the change in second-trimester abortion associated with the post- versus pre-policy period.14,15 Specifically, we calculated the percent change in the beta coefficients between nested models (e.g., (βModel1 – βUnadjusted Model)/βUnadjusted Model). We estimated non-parametric 95% confidence intervals (CIs) for the percent change between estimates using a 1000-iteration bootstrap, sampling with replacement at the county level.
For women who obtained abortions after HB 2, we also assessed the relationship between the expected timeliness of care and second-trimester abortion. We first plotted the monthly average number of days until the next available consultation visit for each of the metropolitan areas with at least one facility that remained open for six or more months after HB 2 to facilitate a visual comparison of variation in wait times. Then, we estimated a mixed-effects logistic regression model for second-trimester abortion that included the number of days until the next available consultation visit, one-way distance to the nearest open Texas facility, and facility network size, as well as women’s demographic characteristics. All analyses were conducted using Stata 15.1.
Results
Of the 123,429 abortions included in the two 12-month periods before and after implementation of HB 2, we excluded records for non-Texas residents or that were missing information on women’s county of residence (n=5,048), gestational age (n=31), or other demographic characteristics (n=274). This resulted in a final sample of 118,076 abortions. The sample included 64,902 Texas-resident abortions before HB 2 was introduced (November 2011-October 2012) and 53,174 abortions after implementation of the law (November 2013-October 2014).
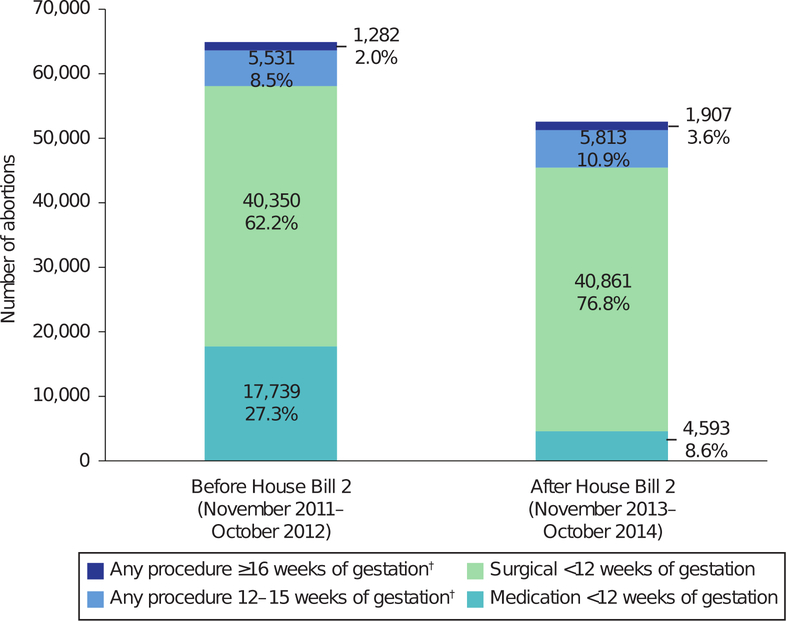
The mean gestational age at abortion increased from 7.3 weeks to 8.3 weeks between the two periods (p<.001). Overall, 6,183 (10.5%) abortions occurred ≥12 weeks of gestation before HB 2 and 7,720 (14.5%) abortions occurred ≥12 weeks of gestation after implementation of the law (p<.001; Figure 1). Additionally, the number of first-trimester medication abortions decreased from 17,729 (27.3% of all procedures) to 4,593 (8.6%). The number of procedures ≥22 weeks of gestation also decreased from 220 (0.3%) before HB 2 was introduced to 39 (0.1%) after the law’s implementation (not shown).
Figure 1.
Abortion procedure type and gestational age at abortion*, before and after implementation of Texas House Bill 2. *Beginning January 2014, abortions were reported using weeks postfertilization instead of weeks from last menstrual period. For abortions occurring in 2014, gestational age at the time of abortion was estimated by adding two weeks to postfertilization age. †Procedures ≥12 weeks include 183 (1.3%) nonsurgical procedures.
In both policy periods, women who were <18 years of age, Black, lived further from an open Texas facility at the time of their abortion, and lived in a region with a smaller facility network were more likely to have a second-trimester abortion (all p<.01; Table 1). Additionally, more women who obtained abortions lived <10 miles from the nearest facility before implementation of HB 2 than after (78.2% versus 61.6%), and the percentage living ≥100 miles from the nearest facility increased by 43% between periods (from 12.0% to 17.2%). The percentage and number of women who obtained abortions living in a region with ≥1.5 facilities per 250,000 reproductive-aged women also decreased from 66.9% before HB 2 to 12.2% after the law, and the percentage of women who lived in a region with <1 facility per 250,000 women increased (2% versus 40%).
Table 1.
Distribution of abortions and abortions ≥12 weeks of gestation*, before and after implementation of Texas House Bill 2 (HB 2)
| Characteristic | Before HB 2 (Nov 2011-Oct 2012) |
After HB 2 (Nov 2013-Oct 2014) |
||||
|---|---|---|---|---|---|---|
| No. (%) of abortions† |
No. (%) abortions ≥12 weeks‡ |
p-value§ | No. (%) of abortions† |
No. (%) abortions ≥12 weeks† |
p-value§ | |
| Total | 64,902 (100) | 6,183 (10.5) | -- | 53,174 (100) | 7,720 (14.5) | -- |
| Age, years | <.001 | <.001 | ||||
| <18 | 1,902 (2.9) | 417 (21.9) | 1,655 (3.1) | 446 (26.9) | ||
| 18–24 | 25,094 (38.7) | 3,088 (12.3) | 20,883 (39.3) | 3,468 (16.6) | ||
| 25–29 | 17,630 (27.2 ) | 1,630 (9.2) | 14,385 (27.0) | 1,846 (12.8) | ||
| ≥30 | 20,276 (31.2) | 1,678 (8.3) | 16,251 (30.6) | 1,960 (12.1) | ||
| Race or ethnicity | <.001 | <.001 | ||||
| Hispanic | 24,592 (37.9) | 2,543 (10.3) | 19,542 (36.8) | 2,696 (13.8) | ||
| White | 19,607 (30.2) | 1,899 (9.7) | 15,437 (29.0) | 2,127 (13.8) | ||
| Black | 16,306 (25.1) | 2,025 (12.4) | 14,226 (26.8) | 2,431 (17.1) | ||
| Asian | 2,867 (4.4) | 199 (6.9) | 2,774 (5.2) | 286 (10.3) | ||
| Other or unknown | 1,530 (2.4) | 147 (9.6) | 1,195 (2.2) | 180 (15.1) | ||
| Number of previous births | .484 | <.001 | ||||
| 0 | 23,988 (37.0) | 2,513 (10.5) | 19,590 (36.8) | 2,667 (13.6) | ||
| 1–2 | 30,875(47.6) | 3,213 (10.4) | 25,173 (47.3) | 3 716 (14.8) | ||
| ≥3 | 10,039 (15.5) | 1,087 (10.8) | 8,411 (15.8) | 1,337 (15.9) | ||
|
One-way distance to nearest Texas facility, miles|| |
<.001 | <.001 | ||||
| <10 | 50,751 (78.2) | 5,209 (10.3) | 32,773 (61.6) | 4,388 (13.4) | ||
| 10–49 | 10,267(15.8) | 1,093 (10.6) | 13,130 (24.7) | 2,065 (15.7) | ||
| 50–99 | 1,973 (3.0) | 282 (14.3) | 3,500 (6.6) | 617 (17.6) | ||
| ≥100 | 1,911 (2.9) | 229 (12.0) | 3,771 (7.1) | 650 (17.2) | ||
|
Facility network in region of residence, facilities per 250,000 women¶ |
<.006 | <.001 | ||||
| <1 | 1,281 (2.0) | 163 (12.7) | 21,285 (40.0) | 3,737 (17.6) | ||
| 1–1.4 | 20,214 (31.1) | 2,180 (10.8) | 25,415 (47.8) | 3,252 (12.8) | ||
| ≥1.5 | 43,407 (66.9) | 4,470 (10.3) | 6,474 (12.2) | 731 (11.3) | ||
Beginning January 2014, abortions were reported using weeks’ post-fertilization instead of weeks from last menstrual period. For abortions occurring in 2014, gestational age at the time of abortion was estimated by adding 2 weeks to post-fertilization age.
Column percentages. Percentages may not sum to 100 due to rounding.
Row percentages
Chi-squared p-value comparing the distribution of abortions ≥12 weeks of gestation
One-way distance estimated from the population-weighted centroid of a woman’s county of residence to the nearest open Texas facility on the date of her abortion.
The size of a clinic network in a woman’s region of residence was computed using the number of open facilities in the region on the date of her abortion and 2011–2015 American Community Survey estimates of the number of women aged 15 to 44 years in the region
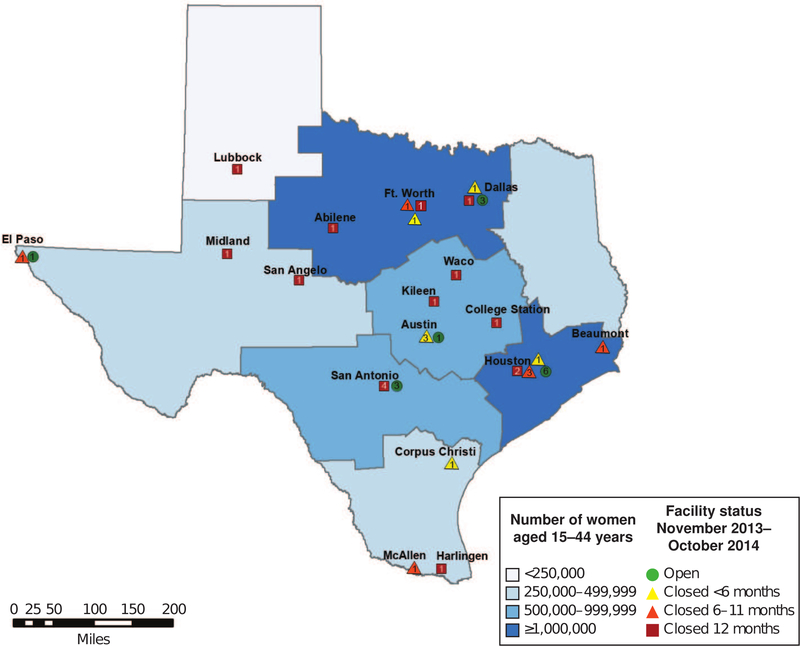
The 21 facilities that closed for ≥6 months after passage of HB 2 were distributed throughout the state (Figure 2). Regions with <1 facility per 250,000 women after HB 2 included less populated areas, such as the Panhandle (Lubbock), South (McAllen and Harlingen) and East Texas, as well as North Central Texas, where there were numerous facility closures in the Dallas-Ft. Worth metropolitan area.
Figure 2.
Population of women aged 15–44 years and abortion facility closures after implementation of House Bill 2 in Texas Health Service Regions. Number in symbol represents the total number of facilities. Some facility locations have been modified to improve readability.
In the unadjusted mixed-effects logistic regression model, the odds ratio (OR) for obtaining an abortion ≥12 weeks of gestation after implementation of HB 2 compared to the period before passage of the law was 1.45 (95% confidence interval [CI]: 1.40, 1.50). After adjusting for women’s demographic characteristics only (Table 2, Model 1), the OR for second-trimester abortion after implementation of HB 2 was 1.44 (95% CI: 1.39, 1.50). In the model that also included one-way distance to the nearest open Texas facility at the time of a woman’s abortion, the OR for policy period was 1.40 (95% CI: 1.34, 1.45) and the OR was 1.17 (95% CI: 1.10, 1.25) after further adjustment for facility network size. In the fully adjusted model (Table 2, Model 3), women who lived 50–99 miles from the nearest open Texas facility had higher odds of second-trimester abortion than women whose nearest facility was <10 miles; living ≥100 miles was not significantly associated with second-trimester abortion. Compared with women living in a region with ≥1.5 facilities per 250,000 women, those in regions with 1–1.4 open facilities and with <1 open facility had higher odds of second-trimester abortion.
Table 2.
Odds ratios for obtaining an abortion ≥12 weeks of gestation* among Texas resident women
| Characteristic | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Period | |||
| Before HB 2 (Nov 2011 – Oct 2012) | 1 (ref) | 1 (ref) | 1 (ref) |
| After HB 2 (Nov 2013 – Oct 2014) | 1.44 (1.39–1.50) | 1.40 (1.34–1.45) | 1.17 (1.10–1.25) |
|
One-way distance to nearest Texas facility, miles† |
|||
| <10 | -- | 1 (ref) | 1 (ref) |
| 10–49 | -- | 1.15 (1.05–1.26) | 1.06 (0.97–1.16) |
| 50–99 | -- | 1.30 (1.16–1.45) | 1.24 (1.11–1.39) |
| ≥100 | -- | 1.19 (1.06–1.34) | 0.95 (0.84–1.08) |
|
Facility network in region of residence, facilities per 250,000 women‡ |
|||
| <1 | -- | -- | 1.57 (1.41–1.75) |
| 1–1.4 | -- | -- | 1.07 (1.00–1.14) |
| ≥1.5 | -- | -- | 1 (ref) |
OR: Odds ratios from mixed-effects logistic regression models with adjustments for age, race and ethnicity, and number of previous births; CI Confidence interval.
Not included in the model.
Beginning January 2014, abortions were reported using weeks’ post-fertilization instead of weeks from last menstrual period. For abortions occurring in 2014, gestational age at the time of abortion was estimated by adding 2 weeks to post-fertilization age.
One-way distance estimated from the population-weighted centroid of a woman’s county of residence to the nearest open Texas facility on the date of her abortion.
The size of the facility network in a woman’s region of residence was computed using the number of open facilities in the region on the date of her abortion and 2011–2015 American Community Survey estimates of the number of women aged 15 to 44 years in the region.
Demographics did not account for the higher odds of obtaining an abortion ≥12 weeks of gestation after versus before implementation of HB 2 (percent attenuation: −1.9%; 95% CI −4.5%, 0.1%). Distance and facility network size accounted for 9.4% (95% CI −28.8%, −2.9%) and 57.7% (95% CI: −88.8% to −22.8%) of the increased odds of obtaining an abortion ≥12 weeks of gestation after HB 2, respectively.
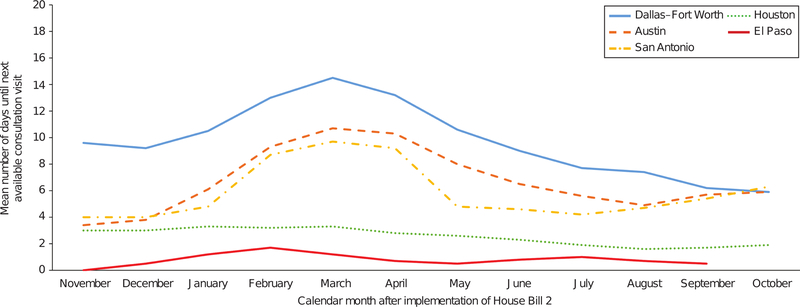
As documented in the mystery client calls, the next consultation visit was available the same day at some open facilities but could be as long as 26 days from the date of the call during the 12-month period after implementation of HB 2 (not shown). The average number of days until the next consultation visit varied over time and across the five metropolitan areas with at least one facility that remained open for six or more months (Figure 3). Facilities in Dallas-Ft. Worth had the longest average wait times; they were unable to schedule women for consultations for at least 13 days between February and April 2014. During these months, the average wait times in Austin and San Antonio ranged from nine to 11 days and then decreased beginning in May 2014. Although wait times fluctuated over the 12-month period at facilities in Houston and El Paso, women could consistently schedule their consultation visit in four days or less, on average.
Figure 3.
Mean number of days until the next available consultation visit* in a woman’s nearest Texas metropolitan area after implementation of Texas House Bill 2. *Days until the next available consultation visit is a 3-month moving average calculated from the wait times at open facilities in the index, preceding, and subsequent month. Wait times in November and December 2013 were based on January 2014 data.
In the multivariable-adjusted regression model among Texas residents who obtained abortion care after implementation of HB 2, the number of days until the next available consultation visit was significantly associated with having an abortion ≥12 weeks of gestation (Table 3). Compared with women whose nearest city had an average wait time <3 days during the month of their abortion, those whose nearest metropolitan area had wait times between five and nine days and ≥10 days had higher odds of having a second-trimester abortion. The associations between one-way distance to the nearest Texas facility, facility network size in a woman’s region of residence and having a second-trimester abortion were similar to those from the analyses that included women obtaining care before and after implementation of HB 2. However, the OR for women whose nearest facility was 50–99 miles was not statistically significant.
Table 3.
Odds ratios for obtaining an abortion ≥12 weeks of gestation* after implementation of Texas House Bill 2 (HB 2), according to indicators of abortion access
| Characteristic | OR (95% CI) |
|---|---|
|
Next available consultation visit in the nearest Texas city, days† |
|
| < 3 | 1 (ref) |
| 3–4 | 1.21 (1.09–1.33) |
| 5–9 | 1.31 (1.17–1.47) |
| ≥10 | 1.59 (1.41–1.79) |
|
One-way distance to nearest Texas facility, miles‡ |
|
| <10 | 1 (ref) |
| 10–49 | 1.03 (0.90–1.18) |
| 50–99 | 1.16 (0.99–1.36) |
| ≥100 | 1.04 (0.89–1.20) |
|
Facility network in region of residence, facilities per 250,000 women§ |
|
| <1 | 1.46 (1.28–1.67) |
| 1–1.4 | 1.28 (1.14–1.44) |
| ≥1.5 | 1 (ref) |
OR: Odds ratios from mixed-effects logistic regression models with adjustments for age, race and ethnicity, and number of previous births; CI Confidence interval.
Beginning January 2014, abortions were reported using weeks’ post-fertilization instead of weeks from last menstrual period. For abortions occurring in 2014, gestational age at the time of abortion was estimated by adding 2 weeks to post-fertilization age.
Days until the next available consultation visit is a three-month moving average calculated from the wait times at open facilities in the nearest Texas city in the index month, and preceding and subsequent month, of a woman’s abortion.
One-way distance estimated from the population-weighted centroid of a woman’s county of residence to the nearest open Texas facility on the date of her abortion.
The size of the facility network in a woman’s region of residence was computed using the number of open facilities in the region on the date of her abortion and 2011–2015 American Community Survey estimates of the number of women aged 15 to 44 years in the region.
Discussion
The number of abortions occurring ≥12 weeks of gestation increased by 25% in the year following implementation of Texas HB 2 compared with the 12-month period before the law’s introduction and passage, despite an overall decrease in the total number of abortions. Although the decrease in abortions ≥22 weeks of gestation was likely due to the law’s provision prohibiting abortions after this point in pregnancy, our analyses indicate that changes in facility network size following clinic closures explained a substantial portion of the overall increase in second-trimester abortion. Difficulties finding a provider have been associated with obtaining abortion care later in pregnancy.16 Indeed, as reported in other studies from Texas,17–19 women struggled to find up-to-date information about services online or did not receive an accurate referral from providers in the initial months after HB 2; some had their consultation or procedure appointments canceled, which contributed to delays reaching another open facility.
We also observed that women living farther from an open Texas facility were more likely to obtain an abortion ≥12 weeks of gestation. As documented in several studies,18–20 women traveling longer distances for care face difficulties arranging transportation, take time off work, possibly have to stay overnight and find childcare, and cover the increased cost of these expenses, which may further delay their care. However, unlike prior research from Texas demonstrating a linear trend between increasing distance to a facility and a decreasing number of abortions after HB 2,3 there was not a similar increase in second-trimester abortion as distance to a facility increased. Specifically, women living ≥100 miles from a facility were not more likely to have a second-trimester abortion than those living near a facility. This result may be attributable to these women making fewer visits to a facility because the mandatory waiting period between the consultation and abortion was reduced from 24 to two hours. Furthermore, although distance attenuated the association between policy period and second-trimester abortion, it had a smaller effect than other variables, suggesting that other indicators of abortion access may play a more important role in women’s ability to obtain timely care.
Another novel aspect of our study is that we were able to document the timeliness with which women were likely able to make their initial consultation visit and model the association between wait time and obtaining a second-trimester abortion. We observed considerable variation in wait times across metropolitan areas after implementation of HB 2 – as well as within some cities, which was probably due to women’s demand for services exceeding provider availability. This expands on previous research21 demonstrating an association between second-trimester abortion and appointment wait times by illustrating the role that facility-level delays have on women obtaining care later in pregnancy.
Although there is an increased need for second-trimester abortion services, Texas passed legislation in 2017 prohibiting physicians from performing dilation and evacuation, the most commonly used procedure in the second trimester. The law is enjoined as of this writing, but if it is allowed to go into effect, providers will have few evidence-based options for later abortion care. Given the limited number of US providers offering care ≥16 weeks of pregnancy, women, particularly those with fewer resources, may be forced to continue unwanted pregnancies.22,23
This study has several limitations. Our approach to account for the change in reporting gestational age may bias our estimates of second-trimester abortion if providers still reported weeks from LMP rather than post-fertilization age. However, given the large decrease in the number of abortions ≥22 weeks of gestation, it is unlikely that our findings are primarily due to a bias in our estimating approach. We also may have underestimated the distance women traveled and the number of days until the consultation visit, since other studies have reported that, after HB 2, women did not obtain care at the nearest facility or traveled out of state.2,17,19 Because we do not have information on women’s preference for medication abortion or gestational age when they presented for care, we do not know whether the nearest facility could provide the services they needed. Finally, we were unable to account for some of the increase in second-trimester abortion, which may be related to changes in the cost of care or further delays between the consultation and procedure visit.
Implementation of HB 2 adversely affected multiple dimensions of women’s access to abortion care, which contributed to the observed increases in second-trimester abortion. States considering similar laws restricting access to abortion can expect clinically significant changes in women’s health outcomes.
Supplementary Material
Acknowledgements:
This project was supported by a grant from the Susan Thompson Buffett Foundation, and a center grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2C HD042849) awarded to the Population Research Center at the University of Texas at Austin. The funders played no role in the design and conduct of the study; interpretation of the data; or preparation, review, or approval of this manuscript for publication.
Footnotes
Presented on October 14–16, 2017.at the North American Forum on Family Planning in Atlanta, GA.
References
- 1.Nash E, Gold RB, Mohammed L, Ansari-Thomas Z, Cappello O. Policy trends in the states, 2017. Washington, D.C.: Guttmacher Institute; 2018. https://www.guttmacher.org/article/2018/01/policy-trends-states-2017. Accessed June 9, 2018. [Google Scholar]
- 2.Gerdts C, Fuentes L, Grossman D, et al. The impact of clinic closures on women obtaining abortion services after implementation of a restrictive law in Texas. Am J Public Health 2016;106(5):857–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grossman D, White K, Hopkins K, Potter JE. Change in distance to nearest facility and abortion in Texas, 2012 to 2014. JAMA 2017;317(4):437–439. doi: 10.1001/jama.2016.17026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grossman D The use of public health evidence in Whole Woman’s Health v Hellerstedt. JAMA Intern Med 2017;177(2):155–156. doi: 10.1001/jamainternmed.2016.6839 [DOI] [PubMed] [Google Scholar]
- 5.Upadhyay UD, Desai S, Zlidar V, et al. Incidence of emergency department visits and complications after abortion. Obstet Gynecol 2015;125(1):175–183. [DOI] [PubMed] [Google Scholar]
- 6.Zane S, Creanga AA, Berg CJ, et al. Abortion-related mortality in the United States 1998–2010. Obstet Gynecol 2015;126(2):258–265. doi: 10.1097/AOG.0000000000000945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones RK, Ingerick M, Jerman J. Differences in abortion service delivery in hostile, middle-ground and supportive states in 2014. Womens Health Issues 2018;28(3):212–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allen RH, Goldberg AB. Cervical dilation before first-trimester surgical abortion (<14 weeks’ gestation). Contraception 2016;93(4):277–291. [DOI] [PubMed] [Google Scholar]
- 9.Penchansky R, Thomas JW. The concept of access: Definition and relationship to consumer satisfaction. Med Care 1981;19(2):127–140. [DOI] [PubMed] [Google Scholar]
- 10.US Census Bureau. Centers of population https://www.census.gov/geo/reference/centersofpop.html. Accessed June 9, 2018.
- 11.Huber S, Rust C. Calculate travel time and distance with OpenStreetMap data using the Open Source Routing Machine (OSRM). Stata J 16(2):416–423. [Google Scholar]
- 12.Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM. Timing of steps and reasons for delays in obtaining abortions in the United States. Contraception 2006;74(4):334–344. [DOI] [PubMed] [Google Scholar]
- 13.Colman S, Joyce T. Regulating abortion: Impact on patients and providers in Texas. J Policy Anal Manage 2011;30(4):775–797. doi: 10.1002/pam.20603 [DOI] [Google Scholar]
- 14.Hayes A Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Commun Monogr 2009;76(4):408–420. [Google Scholar]
- 15.Preacher K, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 2008;40(3):879–891. [DOI] [PubMed] [Google Scholar]
- 16.Drey EA, Foster DG, Jackson RA, Lee SJ, Cardenas LH, Darney PD. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol 2006;107(1):128–135. [DOI] [PubMed] [Google Scholar]
- 17.Fuentes L, Lebenkoff S, White K, et al. Women’s experiences seeking abortion care shortly after the closure of clinics due to a restrictive law in Texas. Contraception 2016;93(4):292–297. doi: 10.1016/j.contraception.2015.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baum SE, White K, Hopkins K, Potter JE, Grossman D. Women’s experience obtaining abortion care in Texas after implementation of restrictive abortion laws: A qualitative study. PLOS ONE 2016;11(10):e0165048. doi: 10.1371/journal.pone.0165048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jerman J, Frohwirth LF, Kavanaugh ML, Blades N. Barriers to abortion care and their consequences for patients traveling for services: Qualitative findings from two states. Perspect Sex Reprod Health 2017;49(2):95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White K, deMartelly V, Grossman D, Turan JM. Experiences accessing abortion care in Alabama among women traveling for services. Womens Health Issues 2016;26(3):298–304. [DOI] [PubMed] [Google Scholar]
- 21.Jones RK, Jerman J. Time to appointment and delays in accessing care among US abortion patients New York, NY: Guttmacher Institute; 2016. https://www.guttmacher.org/report/delays-in-accessing-care-among-us-abortion-patients. Accessed June 9, 2018. [Google Scholar]
- 22.Jones RK, Jerman J. Abortion incidence and service availability in the United States, 2014. Perspect Sex Reprod Health 2017;49(1):17–27. doi: 10.1363/psrh.12015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Upadhyay UD, Weitz TA, Jones RK, Barar R, Foster DG. Denial of abortion because of provider gestational age limits in the United States. Am J Public Health 2014;104(9):1687–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.