Summary Statement:
Serial multimodal imaging including spectral-domain optical coherence tomography (SD-OCT) in acute stage welder’s maculopathy is described. The evolution of lesions from this specific type of photic injury is characterized to enable prompt diagnosis and early intervention to reduce recurrent exposure.
Keywords: welder’s maculopathy, photic maculopathy, optical coherence tomography, SD-OCT, arc welding, retinal phototoxicity
Abstract
Purpose:
Photic retinal toxicity induced by exposure to arc welding can lead to irreversible vision loss. Serial multimodal imaging is characterized in a patient with outer retinal damage secondary to welder’s maculopathy.
Methods:
A single case was retrospectively reviewed.
Results:
Spectral-domain optical coherence tomography (SD-OCT) acutely revealed disruption of the ellipsoid zone, hyper-reflective bands through the outer nuclear layer, and outer retinal cavitation consistent with phototoxicity. Subsequently, disruption and hypertrophy of the subfoveal retinal pigment epithelium (RPE) developed. Autofluoresence depicted central hypo-autofluorescence.
Conclusions:
We report serial multimodal imaging in welder’s maculopathy to better characterize the evolution of lesions. Multimodal imaging including SD-OCT in arc welding phototoxicity may share features with other forms of phototoxicity such as hand-held laser maculopathy.
Introduction
Phototoxicity secondary to arc welding has been documented since 1902 and is considered a potential well-known occupational hazard.1–2 In the United States alone there are 357,400 professional welders, and the number is projected to increase.2 The prevalence of welder’s maculopathy is unclear, but Stokkerman and Dunbar revealed that up to 15% of phototoxic maculopathy patients were welders.3
Phototoxic maculopathy can cause irreversible vision loss by exposure to ultraviolet light (400–440 nm), as shorter wavelengths of visible light are readily absorbed by the cornea and lens.4–5 Notably, there is a predisposition for phototoxicity to occur in younger patients due to better clarity of the clearer ocular media.5 The mechanism of phototoxicity has been inferred from prior studies based on solar or other types of photic damage including laser-induced maculopathy.6–7 The outer retina is particularly vulnerable to photic damage by photochemical damage potentially mediated by free radicals.8
The advancement of retinal imaging including diagnostic studies such as spectral-domain optical coherence tomography (SD-OCT) may be useful in the evaluation of welder’s maculopathy. Herein, we describe multimodal imaging findings in a case of acute photic maculopathy.
Case Report
A 45-year-old diabetic male presented with one day history of incidentally discovered, painless, central vision loss in his left eye. On exam, visual acuity in the right eye was 20/20 and 20/800 in the left eye. Pupils were round and reactive to light with no afferent pupillary defect. Intraocular pressures were 14 in the right eye and 13 in the left eye. Anterior segment exam revealed no abnormalities. Dilated fundus exam revealed microaneurysms and dot-blot hemorrhages consistent with mild nonproliferative diabetic retinopathy (NPDR) in both eyes. A foveal hypo-pigmented yellowish-gray lesion was visualized in the left eye. SD-OCT of the left eye revealed vertical hyper-reflective bands emanating from the ellipsoid zone and extending to the outer plexiform layer in several regions (Figure 1-A and 1-B). Additionally, a cleft-like hypo-reflective area or outer retinal cavitation was observed (Figure 1-D).
Figure 1.
Serial spectral domain-optical coherence tomography (SD-OCT) of the left eye photic exposure at presentation (A-D), 9 days (E-F), and 1 month (G, H, I). Image D demonstrates outer retinal cavitation. Images A, B, and H show hyper-reflective bands emanating from the ellipsoid zone that pass through the outer nuclear layer along Henle’s layer. Image E and F demonstrate retinal pigment epithelium irregularity and hypertrophy. Image I shows partial reformation of the subfoveal ellipsoid zone.
Upon directed questioning, the patient denied history of sun gazing, intraocular surgery, laser exposure, and performing welding. However, the patient reported that he had observed a friend perform arc welding without eye protection one day prior to presentation. He stated that he gazed over his friend’s shoulder, thereby exposing only his left eye. The patient acknowledged central vision loss in the left eye following the incident.
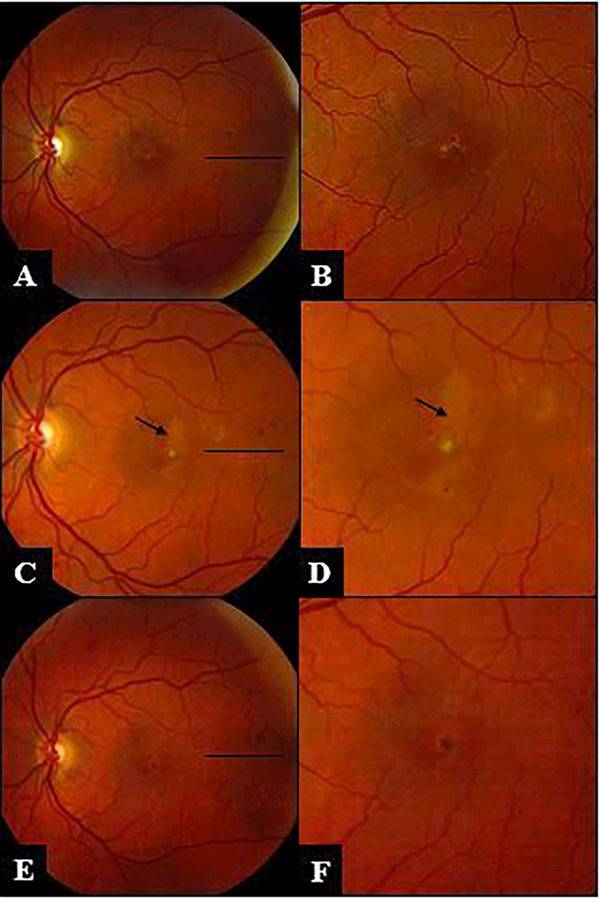
Follow-up fundus examination nine days later revealed central hyperpigmentation consistent with RPE hypertrophy and progression to a new outer retinal streak-like lesion (Figure 2). Repeat SD-OCT of the left eye revealed progressive loss of the ellipsoid zone and RPE hypertrophy (Figure 1-E and 1-F). Fluorescein angiography was obtained and revealed vascular changes consistent with his mild diabetic retinopathy (Figure 3). Autofluorescence of the left eye depicted a small focal area of foveal hypo-autofluorescence. Humphrey visual field 10–2 of the left eye showed a central superior scotoma.
Figure 2.
Serial fundus photos of the left eye demonstrating lesion evolution: focal RPE changes are noted at 9 days (A, B), progression to outer retinal streaks develops at 17 days (C, D), resolution of outer retinal streaks and RPE hypertrophy occurs at 30 days (E, F).
Figure 3.
Fluorescein angiography 9 days following initial presentation demonstrates vascular changes including microaneurysms consistent with background non-proliferative diabetic retinopathy (A, B). Autofluorescence at 17 days reveals focal central hypoautofluorescence (C).
One month following his initial visit, the best corrected visual acuity improved to 20/60. Fundus exam depicted resolution of outer retinal streaks but there was persistence of pigmentary changes (Figure 2-E and F). Outer retinal cavitation resolved, but central RPE hypertrophy persisted (Figure 1-G and H). There was partial reformation of the ellipsoid layer and external limiting membrane (Figure 1-I).
Discussion
To our knowledge, this is the first report demonstrating chronological evolution of welder’s maculopathy lesions by serial multimodal imaging including spectral-domain optical coherence tomography, as well as exhibiting similarities in imaging features in comparison to hand-held laser maculopathy.
The clinical and imaging findings in our case are consistent with prior reports of outer retinal damage secondary to retinal phototoxicity. It is notable that there is significant overlap between photic changes in welding maculopathy and findings of hand-held laser maculopathy. The clinical findings of a yellowish-gray foveal outer retinal lesion evolving to hyper-pigmentation and RPE hypertrophy as well as outer retinal streak has been described in association with laser induced photic injury.5–6 Outer retinal cavitation, ellipsoid loss, and hyper-reflective bands through the outer nuclear layer have also been previously well-described as SD-OCT features associated with hand-held laser maculopathy.5–6 SD-OCT scans through the clinically visualized outer retinal streak display characteristic hyper-reflectivity through the outer nuclear layer also seen in hand-held laser photic injury. Further, evolution of lesions from arc welding appears to mimic that of photic injury from laser toxicity. In our case, there was partial reformation of the ellipsoid zone and external limiting membrane as well as resolution of outer retinal cavitation occurring over a four-week period. Foveal retinal pigment epithelial hypertrophy was persistent and limited visual potential.
In contrast to hand-held laser maculopathy, the outer retinal streak visualized in this welding maculopathy case does not exhibit hypo-autofluorescence, despite sharing a similar appearance by SD-OCT to outer retinal streaks described in association with laser-induced maculoopathy. To date, no other published reports of welding maculopathy document the presence of accompanying outer retinal streaks. The authors hypothesize that this difference in autofluorescence findings may be secondary to greater degree of exposure and concentration of thermal energy in direct laser injury cases leading to more significant retinal damage. Outer retinal streaks described in association with hand-held laser toxicity are typically the result of the repetitive, self-inflicted exposures to high-power lasers.6 There was a single, likely relatively brief exposure to ultraviolet light from arc welding in this case. Additional studies describing multimodal imaging of outer retinal streaks in welding maculopathy are necessary.
A review of the existing literature reveals the majority of welding maculopathy cases were associated with mild, reversible outer retinal changes such as focal ellipsoid loss and subsequently patients typically retained good vision. Our case depicts a more rare and severe manifestation of welding photic injury in which foveal retinal pigment epithelial hypertrophy limited the patient’s vision. Also, interestingly, this patient sustained unilateral photoxicity. Unilateral solar retinopathy has been reported to occur due to an asymmetrical reflex blink response.9 It is possible that the patient may have exposed his left eye to a greater degree, and potentially may have also had a greater blink response in the right eye.
Mild diabetic retinal changes were noted in both eyes; however, there was no evidence of macular edema in either eye. It is unlikely that this patient’s diabetic retinopathy contributed to the specific and serial outer retinal changes captured by multimodal imaging. Outer retinal cavitation and vertical hyper-reflective bands or outer retinal streaks have been characteristically described in association with retinal phototoxicity, not diabetic retinopathy.
Multimodal serial imaging is an effective clinical tool to help establish a diagnosis of welding maculopathy and enables better characterization of these photic lesions. Our case demonstrates that photic injury from arc welding shares several clinical and imaging features with laser induced maculopathy.
Acknowledgments
Financial Disclosures:
Supported by unrestricted departmental funding from Research to Prevent Blindness (New York, NY) and by grant P30 EY010572 from the National Institutes of Health (Bethesda, MD). Drs. Bhavsar and Faridi receive financial support from the Portland VA Healthcare System.
This work was completed at Casey Eye Institute, OHSU.
Footnotes
The authors do not have any conflict of interest.
References
- 1.Terrien F Des trouble visual provoque por l’electricete, Arch. Ophthalomol. 1902; 22:692–696. [Google Scholar]
- 2.Bureau of Labor Statistics, U.S. Department of Labor. Welders, Cutters, Solderers, and Brazers. Occupational Outlook Handbook, 2016–17 Edition. December 17, 2015. https://www.bls.gov/ooh/production/welders-cutters-solderers-and-brazers.htm (visited January 31, 2017). [Google Scholar]
- 3.Stokkermans TJ, Dunbar MT (1998) Solar retinopathy in a hospital-based primary care clinic. J Am Optom Assoc 1998;69(10):625–636 [PubMed] [Google Scholar]
- 4.Vukicevic M, Heriot W. Phototoxic maculopathy associated with arc welding: clinical findings and associated functional vision impairment. Clin Experiment Ophthalmol. 2008. October;36(7):695–7. [DOI] [PubMed] [Google Scholar]
- 5.Mainster MA, Turner PL: Retinal injuries from light: Mechanisms, Hazards and Prevention. Edited by: Ryan SJ, Hinton DR, Schachat AP, Wilkinson P. In Retina. Volume 2. 4th edition. St Louis. Mosby Elsevier Publishers; 2006;1857–1870. [Google Scholar]
- 6.Bhavsar KV, Wilson D, Margolis R, et al. Multimodal imaging in hand-held laser-induced maculopathy. Am J Ophthalmol. 2015. February;159(2):227–31.e2. [DOI] [PubMed] [Google Scholar]
- 7.Rusu I, Sherman J, Gallego-Pinazo R, et al. Spectral-domain optical coherence tomography and fundus autofluorescence findings in a case of laser pointer-induced maculopathy. Retin Cases Brief Rep. 2013. Fall;7(4):371–5. [DOI] [PubMed] [Google Scholar]
- 8.Hope-Ross MW, Mahon GJ, Gardiner TA, Archer DB. Ultrastructural findings in solar retinopathy. Eye (Lond). 1993;7(Pt 1):29–33. [DOI] [PubMed] [Google Scholar]
- 9.Sheth J, Vidhya N, Sharma A. Spectral-domain optical coherence tomography findings in chronic solar retinopathy. Oman J Ophthalmol. 2013. September;6(3):208–9. [DOI] [PMC free article] [PubMed] [Google Scholar]