Abstract
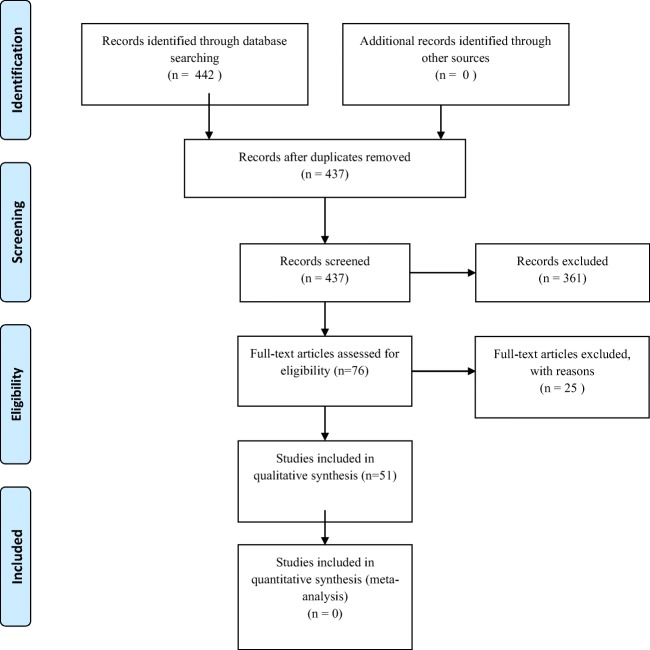
Genetics is increasingly becoming a part of modern medical practice. How people think about genetics’ use in medicine and their daily lives is therefore essential. Earlier studies indicated mixed attitudes about genetics. However, this might be changing. Using the preferred reporting items for systematic reviews and meta-analyses (PRISMA) as a guideline, we initially reviewed 442 articles that looked at awareness, attitudes, knowledge, and perception of risks among the general and targeted recruitment populations. After fitting our criteria (from the last 5 years, conducted in the USA, non-provider populations, quantitative results reported, and assessed participants 18 years and older), finally 51 eligible articles were thematically coded and presented in this paper. Awareness is reported as relatively high in the studies reviewed. Attitudes are mixed but with higher proportions reporting positive attitudes towards genetic testing and counseling. Self-reported knowledge is reasonably high, specifically with the effects of specific programs developed to raise knowledge levels of the general and targeted recruited populations. Perception of risk is somewhat aligned with actual risk. With the reasonable positive reports of genetic awareness and knowledge, there is similar positive attitude and perception of risk, supporting the need for continued dissemination of such knowledge. Given interest in incorporating community participation in genomic educational strategies, we provide this review as a baseline from which to launch community-specific educational supports and tools.
Introduction
Genetics is becoming a more significant component of modern medicine and has interfaced with many parts of the average person’s life—from newborn screening to agriculture, family planning, and consumer products. For example, the National Cancer Institute has been a leader in the integration of genetics into medical practice (McCormick and Calzone 2016). The National Human Genome Research Institute has been engaging communities for several years to design and improve educational strategies with the goal of bringing more diverse perspectives into the research and policy-making process (genome.gov). The Community Engagement in Genomics Working Group, a partnership between numerous community leaders and NHGRI staff, set the goal of understanding the knowledge, attitude, awareness, and perceived risk of genetics operating in their communities.
To accomplish this goal, we sought an understanding of what is currently known in the literature to inform their strategies for soliciting this information and interpreting it against the national landscape. Early research on how people viewed genetics contained both positive and negative perspectives (Singer et al. 2008). But it is unclear how this has changed, especially with the increased focus on genetic awareness of the last decade. As genomics and genetic testing become more embedded in common medical procedures, acceptance by the general public might be very relevant to implementation and use. The present study reviews the current literature on what people in the US report about genetics: their attitudes, knowledge, awareness, and perceptions. This review provides the background setting needed to assist the development of community-specific and population-level assessment and engagement tools to increase community participation in the broader genomics discussion.
Methods for the present review
We present the results of a systematic review of the existing quantitative measures of stakeholder engagement in published research and programs. We used the methods of Preferred Reporting Items for Systematic Reviews and Meta-Analyses to review the literature on measures of genetic understanding (Moher et al. 2009).
Phase 1: searching the literature
With assistance from a reference librarian and previously published research, we generated a master list of search terms to use in the PubMed database (Bowen et al. 2017). The following Medical Subject Headings (MeSH) terms were selected: genetic testing, genetic counseling, attitude, knowledge, awareness, and perception. These terms were then entered into the chosen database using quotations to ensure that search terms were verbatim and genetic testing and genetic counseling were separated by OR, while attitude, knowledge, awareness, and perception were separated by AND to ensure inclusion if any of the search terms were present. A master list of articles (n = 442) resulted from these search results.
Search methods
We searched the peer-reviewed literature using an electronic bibliographic database: PubMed (Web-based). This database search for all years from 2012 to 2016 occurred between May 2017 and June 2017. Exclusion of articles occurred if they surveyed children (defined in this paper as those under the age of 18) or providers (including genetic counselors), were conducted outside of the USA, only reported qualitative data, and did not cite a tool to assess knowledge, awareness, attitudes, or perceived risk.
Phase 2: abstract review
We independently reviewed each title and abstract using pre-determined inclusion and exclusion criteria and resolved disagreements through re-review and discussion until they reached consensus. Included articles appear in English, in a peer-reviewed journal, report original research, had quantitative findings, and were conducted in the USA. The full texts of articles whose abstracts met our inclusion criteria were retrieved and then examined for further inclusion/exclusion criteria.
Phase 3: data abstraction
To ensure consistency in data abstraction, we created a standardized codebook for use by all authors, based on a prior measurement review (Bowen et al. 2017). The codebook included definitions of the four content areas so that studies could efficiently be coded as having one or more of the constructs present in the study. Two authors reviewed the same studies using the codebook and identified and resolved disagreements in coding, resulting in a revised final codebook. For all studies included in the review, two authors independently coded and compared their results. Coding discrepancies within pairs found resolution through discussion among authors. We opted for this consensus method, because of the enormous variability in terminology and quality used to describe engagement characteristics and constructs across studies.
The variables extracted the following data from each article: study design, population/sample, intervention, tools used, and findings. Data entered into Excel files, and evidence tables were constructed, organized by article first author, and stratified by type of construct. Articles with more than one construct appear under every construct mentioned in the article, meaning that some articles will appear in the table more than once.
The flow of diagram or article review
Figure 1 contains the data on article eligibility and coding patterns. The search identified 442 articles using our keywords. After duplicates removed, 437 articles remained. All 437 were screened by reading the abstracts and determining if it fits our previously established eligibility requirements. Three hundred sixty-one articles did not meet our eligibility requirements, leaving 76 articles left. These articles were read in full and coded for data. Further exclusion of 25 articles occurred due to not meeting our criteria, not reporting quantitative data, not reporting any data (study design papers), or being an international article. Fifty-one articles met all criteria and were included in the analysis.
Fig. 1.
PRISMA 2009 flow diagram
Results
Tables 1 and 2 summarize the articles reviewed. We divided the abstracted measures into (1) those focused on a population-based sample and (2) those focused on a targeted or limited sample (such as a high-risk genetic group or a specific ethnic group). For each grouping, we further categorized the content into four areas: attitudes, knowledge, awareness, and perceived risk. This was done by coding the outcomes measured by one or more of the categories provided. We also labeled the articles as having an intervention, depending on study design. Some articles are listed under more than on content area and are marked as such on the tables. While some of these were hard to differentiate, they provide a method of focus for the review.
Table 1.
General population
| Awareness | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Agurs-Collins | Cross-sectional survey | National dataset (HINTS) 3185 participants | N/A | Awareness of DTC testing | 35% were aware of DTC testing |
| Kolor | Cross-sectional | BRFSS participants in Connecticut, Michigan, Oregon, and Utah 21, 788 participants total (over the 3-time points) |
N/A | Awareness of DTC genetic tests, sources of information about DTC genetic tests | Less than 1% reported using a DTC genetic test. Awareness was also pretty low, ranging from 15.8% in Michigan to 29.1% in Oregon. Most commonly cited source for hearing about DTC genetic testing was from TV/Radio, followed by newspaper, magazine, internet. Least widely cited sources were a health professional and family/friends |
| Mai | Cross-sectional | 27,405 Respondents of the National Health Interview Survey in 2000, 2005, and 2010 which had the Cancer Control Module in addition to the regular questionnaire. Narrowed participant pool to those aged 25 and older and excluded those who had not heard of cancer genetic testing | N/A | Awareness and use of genetic tests, family history of cancer in first-degree relatives | From 2000 to 2005 awareness of cancer genetic testing decreased 2.9 percentage points but increased 5. 5 percentage points from 2005 to 2010 |
| Parkman | Cross-sectional survey | National telephone survey BRFSS 21,788 |
N/A | Awareness of genetic nondiscrimination laws | Awareness of nondiscrimination laws is low (less than 20%) but perceived need higher |
| Riesgrafa | Cross-sectional survey | Attendees at rural baseball games (n = 203) |
N/A | Perceptions and attitudes about genetic counseling | Mixed knowledge and attitudes about genetic counseling |
| Attitudes | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Allyse | Cross-sectional Asked hypothetical questionsa | Participants aged 18–44 years old who were invited as part of a survey company N = 1861 | Randomized to 1 of 2 versions of the survey—trisomy 13 and 18 or trisomy 21 | Prenatal testing choices, consideration of termination of pregnancy | 49.8% would consider termination for trisomy 13 and 18 vs. 41.1% for trisomy 21 |
| Dodson | Cross-sectional survey | A probability sample of the general public N = 1526 | N/A | Interest in whole genomic sequencing | Just over half of the population is interested in sequencing |
| Farrell | Cross-sectional survey Asked hypothetical questionsa | Pregnant women presenting for outpatient care at a clinic N = 334 | N/A | Decision-making needs and practices, attitudes about undergoing prenatal genetic testing | Participants expressed interest in incorporating prenatal testing into prenatal care |
| Graves | Cross-sectional online survey | General public N = 900 | N/A | Disease severity and actionability | Both actionability and severity of disease are important when deciding on next steps |
| Higuchi | Cross-sectional Asked hypothetical questionsa | Recruited US adults through Amazon Mechanical Turk n = 1789 | N/A | We investigated the effect of the mock news articles and controls on 3 outcome variables: (1) general support of prenatal testing for Down syndrome, (2) hypothetical personal decision regarding prenatal testing, and (3) beliefs and attitudes about Down syndrome | Those assigned to the mock NIPS article predicted stronger agreement that pregnant women should choose prenatal screening |
| Riesgrafa | Cross-sectional survey | Attendees at rural baseball games (n = 203) |
N/A | Perceptions and attitudes about genetic counseling | Mixed knowledge and attitudes about genetic counseling |
| Sayres | Cross-sectional | Adults 18 and older recruited through the survey company’s (Zoomerang) website N = 3164 | 2 versions of the questionnaire were possible: 1 about trisomy 18 and 13, the other about trisomy 21 | Interest in cffDNA screening, interest in terminating the pregnancy if a positive cffDNA for trisomy 13, 18, or 21 came back | 38% expressed interest in cffDNA screening and 8% expressed interest in both cffDNA and regular screening for trisomy 18 and 13. 42% expressed interest in cffDNA screening for trisomy 21. 52% of those asked about trisomy 13 and 18 would consider pregnancy termination following a positive screening. 44% of trisomy 21 participants would consider terminating the pregnancy after a positive screening |
| Shiloh | Prospective cohort | Recruited from a subset who were involved in the Multiplex Initiative enrollment required that participants be 25–40 years old, Caucasian or African American, and not affected with type 2 diabetes, atherosclerosis, osteoporosis, or cancer. Recruited by telephone N = 294 | N/A | Attitudes assessed using a semantic differential scale | Attitude scores highly correlated with peak scores |
| Steinbach | Cross-sectional survey | A web-based survey of US public N = 84 | N/A | Attitudes about disability, genetic screening, and pregnancy termination | Most respondents supported both the availability of screening and the decision to continue a pregnancy positive for aneuploidy |
| Sweeney | Cross-sectional surveys | General public recruited using telephone selection N = 480 | N/A | Beliefs about cancer and genetics | Participants reported mixed belief accuracy about genetics and positive attitudes about genetics |
| Taber | Cross-sectional survey | Patients recruited at a clinical facility N = 494 | NA | Perceptions of ambiguity about genetics | High ambiguity perceivers had poorer cognitions genetics and were less likely to want to share findings with others |
| Winkelman | Cross-sectional online survey Asked hypothetical questionsa | Public opinion surveying N = 1006 | N/A | Interest in preimplantation genetic testing | About ¾ of respondents were in favor of preimplantation testing |
| Yang | Cross-sectional Asked hypothetical questionsa | Randomly selected patients from the Mayo Clinic Registry. Had to be between ages 50–79 N = 434 | N/A | Modeled after the Health Information National Trends Survey (HINTS). Assessed knowledge of airway and digestive cancers, history of cancers, interest in MUST (noninvasive multi-organ gastrointestinal stool DNA test) | 98% were interested in MUST and would likely use it |
| Knowledge | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Carere 2016 | Online surveys at 3-time points | Customers of DTC companies N = 1042 |
genetic risk estimate, multiple SNPs for each of breast, prostate, colorectal, and lung cancer | Perceived risk | Elevated risk results were significantly associated with positive ΔPR and average risk results with negative ΔPR |
| Haga | Cross-sectional | Recruited from Durham NC through newspaper advertisements, flyers on Duke University’s campus, posters on transit buses, and online advertisements. Must have been at least 18 years old, speak English, and have internet access. No personal history of T2DM and never had a genetic test for T2DM N = 300 | N/A | A short test of functional health literacy for adults, genetic knowledge, used a survey by Morren et al. (2007) to test the future of genetic testing | Increased education positively associated with increased genetic knowledge. 52% were somewhat, and 45% were extremely interested in genetic testing. 51.3% agreed at genetic testing would affect a person’s ability to obtain health insurance |
| Mandelberger | Cross-sectional | Voluntary survey responders set up through the survey agency. Women between the ages of 18 and 45. Had no children OR had one child biologically aged 0–1 N = 428 | N/A | Source of subjects’ knowledge about genetics, personal experience with genetic testing or disease, preferences on genetic testing and counseling | 34.5% of parous women had prenatal counseling by a physician, compared to 11.1% of nulliparous women. Parous women scored significantly higher on genetics knowledge quiz (70.9 vs. 61.9%). 78.1% would prefer to get genetic information from their physician |
| Ostergren | Post-exposure reactions to laboratory reports | People requesting DTC testing N = 1030 | Receiving laboratory reports from testing | Genetic knowledge, comprehension of laboratory reports | High comprehension of reports and knowledge predicted the level of comprehension |
| Schwartz | RCT | Women 21–85 who did not have newly diagnosed or metastatic cancer and lived within a study site catchment area N = 669 | Randomly assigned to usual care or telephone counseling | Breast Cancer Genetic Counselling Knowledge Scale, Decisional Conflict Scale, Genetic counseling satisfaction scale, the impact of event scale, perceived stress scale, short form-12, mental component summary, physical component summary | TC was non-inferior to UC on all outcomes. Post-counseling knowledge score was .03 points higher for TC than UC |
| Wolfe | RCT | Undergraduate women recruited online at two universities in the Midwest and Eastern USA N = 410 | Randomly assigned 1 of 3 conditions: (1) BRCA Gist, the NCI website, or a control tutorial about nutrition | Knowledge of breast cancer, heredity, and genetic testing, Gist comprehension of genetic breast cancer risk, interest in genetic testing, worry, and Pedigree Assessment Tool (PAT) | BRCA Gist participants scored significantly higher than NCI participants, and both scored significantly higher than the control group on total declarative knowledge. BRCA Gist and NCI groups were significantly more accurate in categorizing risk. BRCA Gist participants reported lower levels of interest in genetic testing than NCI or control |
| Yee | RCT | Pregnant women 18 and older between 6 and 26 weeks gestation who spoke English and not having undergone prenatal testing. Exclusions include multiple gestations N = 150 | Assigned to standard care with provider-based counseling or augmented counseling with an interactive computer program | Rapid Estimate of Adult Literacy in Medicine, knowledge test | Women randomized to the interactive computer counseling scored significantly higher on prenatal knowledge than the standard care group |
| Perceived risks | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Boeldt | Longitudinal cohort | Data used from participants in the Scripps Genomic Health Initiative N = 2037 |
N/A | Health Belief Model—the seriousness subsection to elicit what condition they most feared. Perceived control. Speilberger State-Trait Anxiety Inventory. Impact of Events Scale-revised. Godin Leisure-Time Exercise Questionnaire | Most feared diseases: heart attack (males) and Alzheimer’s (females) |
| Carere 2015 | Online surveys at 3-time points | Customers of DTC companies N = 1042 | Genetic risk estimate, multiple SNPs for each of breast, prostate, colorectal, and lung cancer | Perceived risk | Elevated risk results were significantly associated with positive ΔPR and average risk results with negative ΔPR |
aArticle is used in more than one category
Table 2.
Targeted recruitment
| Awareness | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Armstrong | Cross-sectional | Patients with Aetna healthcare insurance whose physicians ordered BRCA testing N = 3874 | N/A | Respondents’ report of receiving genetic counseling by a genetics clinician | Mutations were identified in 161 (5.3%) of these women who received comprehensive testing. Only 1334 (36.8%) reported receiving genetic counseling from a genetics clinician before testing; the lowest rates (130 [12.3%]) were among patients of obstetrician/gynecologists. The most commonly reported reason for not receiving this clinical service was lack of clinician recommendation. Those who received it demonstrated greater knowledge about BRCA (mean score difference adjusted for demographics and clinician specialty, β = 0.99 [95% CI, 0.83–1.14]; p < .001) and expressed greater understanding (β = 0.47 [95% CI, 0.41–0.54]; p < .001) and satisfaction |
| Patela | Cross-sectional survey | Patients in high-risk clinics N = 165 | N/A | Knowledge of guidelines for colon screening | Many had general knowledge; few had risk specific knowledge. High-risk clinic participants scored higher on knowledge tests |
| Sussnera | Cross-sectional | Potential participants filled out a family history from for HBOC risk at breast surgery clinics at Mount Sinai and then were contacted by PI or RA for follow-up phone call. Women aged 18 or older who self-identified as Latina, had never undergone BRCA testing or genetic counseling, had an increased risk for breast or ovarian cancer at a young age (< 55) and/family member with breast/ovarian cancer at a young age N = 120 | N/A | A bidirectional acculturation scale for Hispanics, Group-based medical mistrust scale, perceived risk of carrying BRCA 1/2 mutation, awareness of genetic counseling for cancer risk, attitudes about BRCA genetic counseling, intention to undergo BRCA genetic testing | Average awareness was above average for genetic counseling but below average for BRCA counseling. Largely positive attitudes towards BRCA genetic counseling. Average knowledge of BRCA counseling was high. Medical mistrust was fairly low |
| Attitudes | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Allain | Cross-sectional | The email was sent to potential participants through FORCE (facing our risk of cancer empowered) N = 1699 | N/A | experience with genetic testing, awareness of what they thought could be affected by genetic testing | 66.4% discussed genetic testing with their provider in the last 3 years. 69.2% said they had undergone genetic testing |
| Caminiti | Cross-sectional survey Asked hypothetical questionsa | Parents in families with epilepsy patients recruited from a clinical setting N = 250 | N/A | Interested in having offspring tested for epilepsy risk | Interest general high (85.7%) among parents with affected offspring, lower (74%) among those with no affected offspring |
| Caseli | Cross-sectional survey Asked hypothetical questionsa | An online survey of Alzheimer’s group membership N = 4036 | N/A | Attitudes and knowledge about genetic testing | Knowledge about testing was mixed and attitudes positive. 70.4% were willing to undergo presymptomatic testing even in the absence of any effective intervention |
| Dedert | Cross-sectional | Participants had to have served in the military since October 2001 and be between the ages of 18 and 65. Recruited from the registry of the mental illness research, education, and clinical center at the Durham Veterans’ Administration medical center N = 146 | N/A | Knowledge of PTSD test, a survey of knowledge of genetics, a survey of attitudes towards genetic testing, perceived benefits/limitations of genetic testing for PTSD | PTSD group had less favorable towards genetic testing on both the survey of attitudes towards genetic testing and the perceived benefits of genetic testing for PTSD |
| Fitzgerald-Butta | Cross-sectional study | Parents of children with CHD N = 287 | N/A | Knowledge and attitudes about genetic testing | Participants general had positive attitudes about genetics and knowledge was related to educational level. 57.9–89.4% of participants were “somewhat likely or very likely” to undergo genetic testing for their children. Knowledge summary score was 73.8% correct |
| Freedman | Cross-sectional Asked hypothetical questionsa | First-degree adult (18+) relatives of African American and European American patients at the Wake Forest Baptist Health outpatient dialysis facilities who had ESKD and who were performing in-center hemodialysis or peritoneal dialysis N = 130 | N/A | Asked under what circumstances the participants would want to know their genetic test results | Would want results returned if their disease risk could be reduced by: (98%) diet or exercise, (98%) physician-directed treatment, could not be reduced by known treatments (82%) |
| Hooker | Randomized controlled trial Asked hypothetical questionsa | Inflammatory bowel disease patients from GI clinic N = 257 | Hypothetical vignette of genetic testing for IBD | Perceived control, the utility of testing, genetic literacy | Intervention participants rated higher utility after exposure, with high literacy participants rating higher utility |
| Matro | Prospective cohort Asked hypothetical questionsa | Adults 18 and older with and without a prior history of cancer but with a suspected increase in hereditary cancer risk. Participants are part of the Gastrointestinal Tumor Risk Assessment Program (TRAP) at Fox Chase Cancer Center N = 385 | N/A | Health belief model, the transtheoretical model of behavior change, Anderson model of health service utilization. Knowledge and awareness of GI cancer risk testing, willingness to pay | 21% were willing to have genetic testing only if paid by insurance and 79% were willing to pay out of pocket |
| Narcissa | Cross-sectional Asked hypothetical questionsa | US residents who were a parent or guardian of one or more children with ASD. Participants were recruited via email by local and regional autism advocacy groups N = 162 | N/A | Parental perceptions regarding the ASD diagnostic process. Rest of survey looked at the perceived role of genetics in ASD and parental experience in genetic testing for ASD | 82.1% indicated that ASD was a combination of genetics and environment, 11.9% indicated it was entirely genetic. 6% believed completely non-genetic factors caused it. 27.8% indicated their child had undergone genetic testing for ASD with abnormal results reported for only 7.3% of the children tested. 80% of participants who had a younger, as of yet undiagnosed child, would want their child tested even if it could not confirm or rule out a diagnosis |
| O’Neil 2013 | Cross-sectional | Smokers aged 17–22 who attended the University of Florida. Must have smoked at least 1 cigarette in the prior week and at least 50 cigarettes in their lifetime N = 128 | N/A | The family history of lung cancer, smoking duration, number of serious quit attempts, and motivation to quit. Interest in GSTM1 enzyme testing | An average of 31 months as a smoker, moderate quit motivation (3.9 out of 7 on the scale). Moderately strong intentions for testing (5.21 out of 7 on the scale) |
| Scott | Cross-sectional | African Americans age 18–83. Recruited from local hospitals, health fairs, colleges, and community settings in the Washington D.C. area N = 304 | N/A | Genetic psycho-social questionnaire (GPSI), alcohol use disorder identification test (AUDIT) | 85% of participants expressed willingness to test |
| Strobel | Cross-sectional | Alcohol-dependent participants recruited from 2 different clinical research studies focused on the use of naltrexone as a treatment option. Participants were at least 18 years old and met the DSM-IV criteria for alcohol dependence N = 457 | N/A | Drinking outcome measured with the Time Line Follow Back (TLFB). Survey on genetics asked which health disorders were influenced by genetics | 89% reported a willingness to provide genetic samples for clinical purposes related to the treatment of an AUD. Primary area of concern for genetic testing was the loss of health or life insurance. 83% of respondents agreed or strongly agreed that AUD was at least partially inherited |
| Sussnera | Cross-sectional | Potential participants filled out a family history from for HBOC risk at breast surgery clinics at Mount Sinai and then were contacted by PI or RA for follow-up phone call. Women aged 18 or older who self-identified as Latina, had never undergone BRCA testing or genetic counseling, had an increased risk for breast or ovarian cancer at a young age (< 55) and/family member with breast/ovarian cancer at a young age N = 120 | N/A | A bidirectional acculturation scale for Hispanics, Group-based medical mistrust scale, perceived risk of carrying BRCA 1/2 mutation, awareness of genetic counseling for cancer risk, attitudes about BRCA genetic counseling, intention to undergo BRCA genetic testing | Average awareness was above average for genetic counseling but below average for BRCA counseling. Largely positive attitudes towards BRCA genetic counseling. Average knowledge of BRCA counseling was high. Medical mistrust was fairly low |
| Waxler | Pre-post measures with comparison | Participants recruited through the non-profit parent support group, the WSA. Participants had to be parents of children diagnosed with WS (Williams syndrome) N = 600 | N/A | Perception of diagnostic experience, if they had seen a genetic counselor | 40.09% had a primarily positive diagnostic experience, 25.51% had a primarily mixed experience, and 34.4% a primarily negative experience |
| Wu | Cross-sectional | Recruited through circulating an announcement to the ~40 different clinical genetic centers in the Mid-Atlantic Regional Human Genetics Network. Participants were affected adults and relatives of those with Treacher Collins Syndrome N = 31 | N/A | The perceived emotional burden of TCS, interest in prenatal genetic testing for TCS, the likelihood of terminating a pregnancy based on the prenatal genetic test | – 65% reported that having a child with TCS was of a more significant concern than the risk of miscarriage from genetic testing – Likelihood of genetic testing depends on how accurate the test was. 87% would undergo testing if the test were 100% accurate vs. 6.7% willing to undergo testing if the test was just 20% accurate |
| Yusuf | Cross-sectional survey | Brest cancer patients attending medical visit N = 308 | N/A | Willingness to undergo testing in multiple situations | General patients were willing to undergo testing for many reasons. Nonwhite patients less willing |
| Knowledge | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Adams | Cross-sectional | Parents of children with Batten Disease via the Batten Disease Support and Research Association N = 179 | N/A | Opinions about genetic testing in children GTIC | 73% agreed that genetic testing should be available to asymptomatic people regardless of benefit. 74% agreed the parent should get the final say on whether their child gets genetic testing done. 82% agreed that genetic testing results should always be discussed with a medical professional |
| Fitzgerald-Butta | Cross-sectional study | Parents of children with CHD N = 287 | N/A | Knowledge and attitudes about genetic testing | Participants general had positive attitudes about genetics and knowledge was related to educational level. 57.9–89.4% of participants were “somewhat likely or very likely” to undergo genetic testing for their children. Knowledge summary score was 73.8% correct |
| Gallo | Randomized trial | People with sickle cell disease or trait from multiple settings N = 234 | 3 group educational sessions | SCKnowIQ (knowledge) measure | Had higher knowledge scores post-intervention compared to control |
| Gebhart | Cross-sectional | Patients and partners initiating IVF treatment at a private clinic N = 117 | N/A | Perceptions towards preimplantation genetic screening | 60% accepted PGS. 69% reported no previous knowledge of preimplantation genetic screening before the IVF treatment cycle |
| Patela | Cross-sectional survey | Patients in high-risk clinics N = 165 | N/A | Knowledge of guidelines for colon screening | Many had general knowledge; few had risk specific knowledge. High-risk clinic participants scored higher on knowledge tests |
| Sussnera | Cross-sectional | Potential participants filled out a family history from for HBOC risk at breast surgery clinics at Mount Sinai and then were contacted by PI or RA for follow-up phone call. Women aged 18 or older who self-identified as Latina, had never undergone BRCA testing or genetic counseling, had an increased risk for breast or ovarian cancer at a young age (< 55) and/family member with breast/ovarian cancer at a young age N = 120 | N/A | A bidirectional acculturation scale for Hispanics, Group-based medical mistrust scale, perceived risk of carrying BRCA 1/2 mutation, awareness of genetic counseling for cancer risk, attitudes about BRCA genetic counseling, intention to undergo BRCA genetic testing | Average awareness was above average for genetic counseling but below average for BRCA counseling. Largely positive attitudes towards BRCA genetic counseling. Average knowledge of BRCA counseling was high. Medical mistrust was fairly low |
| Weber | Pre-post measures with a comparison | Students in genetics undergraduate classes N = 84 | Personal DTC testing information | Quiz scores in class | Receiving personal genetic information did not improve personal genomics quiz scores |
| Perceived risk | |||||
| Author (date) | Study design | Population/sample | Intervention | Tools used | Findings |
| Anderson 2016 | Cross-sectional survey | High/moderate risk women from clinical setting N = 1885 | N/A | Perceived risk of ovarian and breast cancer | Most high-risk women did not know their risk of ovarian cancer |
| Himes | Cross-sectional survey | Sisters and daughters of breast cancer patients N = 85 | N/A | Risk perceptions, knowledge | Very little info shared among families, but the info shared improved knowledge about personal risk |
| Sussnera | Cross-sectional | Potential participants filled out a family history from for HBOC risk at breast surgery clinics at Mount Sinai and then were contacted by PI or RA for follow-up phone call. Women aged 18 or older who self-identified as Latina, had never undergone BRCA testing or genetic counseling, had an increased risk for breast or ovarian cancer at a young age (< 55) and/family member with breast/ovarian cancer at a young age N = 120 | N/A | A bidirectional acculturation scale for Hispanics, Group-based medical mistrust scale, perceived risk of carrying BRCA 1/2 mutation, awareness of genetic counseling for cancer risk, attitudes about BRCA genetic counseling, intention to undergo BRCA genetic testing | Average awareness was above average for genetic counseling but below average for BRCA counseling. Largely positive attitudes towards BRCA genetic counseling. Average knowledge of BRCA counseling was high. Medical mistrust was fairly low |
| Tong | RCT-only looking at information gathered before randomization (so before the RCT) | Women 21–85 seeking BRCA 1/2 genetic counseling and having at least a 10% risk for carrying a BRCA 1/2 mutation. Excluded those who had previous genetic counseling/testing, recently diagnosed with metastatic breast or ovarian cancer, or had a cognitive impairment N = 696 | N/A | Perceived risk, cancer-specific distress using the Event Impact Scale, breast cancer genetic counseling knowledge scale, measured numeracy with Lipkus’ 3 item scale, decisional conflict scale, measured quality of life with SF-12, surgery intentions | 23.3% would consider RRM (risk-reducing mastectomy), 42.5% would consider RRO (risk-reducing oophorectomy) |
aArticle is used in more than one category
General populations
Table 1 presents the studies that contained an attempt at a population-based sample.
Awareness
Two articles addressed the general public’s awareness of genetic testing or genetic screening. Mai et al. compared awareness from 2000, 2005, and 2010 national health interview surveys and found that while awareness significantly decreased from 44.4 to 41.5% from 2000 to 2005 (p < .001), it significantly increased to 47% in 2010 (p < .001) (2014). This finding is similar to results in a smaller study by Riesgraf et al. which surveyed rural residents (n = 203) from the Midwest and found 47.4% of participants reported they had heard of genetic counseling (2015). Two articles looked explicitly at awareness of direct-to-consumer (DTC) genetic tests. Agurs-Collins et al. found that only 35.1% had ever heard or read about DTC genetic tests (2015). Kolor et al. found that awareness was even lower, with percentages ranging from 29.1% (CI 26.4–31.9%) in Oregon to 15.8% in Michigan (CI 14.6–17.1%) with a national average being 22.1% (CI 21.0–23.2%) (2012).
One article assessed awareness among the general public of genetic nondiscrimination laws. Parkman et al. found that less than 20% of the adult population were aware of genetic nondiscrimination laws, despite 80% reporting that such laws would be very important (2015).
Attitudes
One article contained attitudes of preimplantation genetic diagnosis (PGD). Winkleman et al. found that the majority of respondents supported PGD to screen for genetic diseases, specifically 72.9% supported screening for “diseases that are fatal in the first few years of life”, 66.7% supported screening for “diseases that cause lifelong disability”, and 48% supported screening for “diseases that may not occur until later in life” (2015).
Six articles addressed attitudes towards prenatal genetic testing and screening, with half of the articles explicitly looking at attitudes towards noninvasive prenatal screening/testing (NIPS/NIPT). A study in which participants looked at mock news articles on either NIPS, amniocentesis, or no article, Higuchi et al. found that those assigned to the mock NIPS article predicted stronger agreement that pregnant women should choose prenatal testing (OLS .297, p < .001) (2016). Steinbach et al. found similar results, with a majority (71.9%) of respondents supporting the use of NIPS, either alone or in combination with other prenatal genetic tests (2016). Farrell et al. found that women, both of low and high-risk pregnancies, expressed support for incorporating NIPT into their prenatal care (2014). Two articles addressed attitudes towards prenatal testing for trisomy 13 and 18 and trisomy 21. In a study where participants were randomized to a survey about cell-free fetal (cff) DNA testing for either trisomy 13 and 18 or trisomy 21, Allyse et al. found that there was substantive interest in the use of cffDNA testing rather than traditional screening mechanisms, with little difference between the groups (trisomy 13/18 37.7%, trisomy 21 38.9%) (2014). In a similar study, Sayres et al. found 46% of respondents to the survey on trisomy 13/18 expressed interest in cffDNA screening compared to 47% of respondents to the trisomy 21 survey (2014). One study looked at whole genome sequencing (WGS) among parents and their children. Dodson et al. found that 61.8% of parents were at least somewhat interested in WGS for themselves, and 57.8% were at least slightly interested in WGS for their children (2015).
Two articles looked at attitudes towards genetic testing for cancer among the general public. In a survey of attitudes towards pan-digestive cancer screening using a multi-organ stool DNA test (MUST), Yang et al. found that 96% of participants would use MUST (2014). In a follow-up to community survey of knowledge and beliefs about cancer and genetics, Sweeney et al. found that the majority (83%) of respondents said they would be willing to take a genetic blood test, higher than the 2001 survey (78%) (2016).
A study on actionability and disease severity in the context of genetic testing found that the majority of participants (n = 900) found both actionability (87%) and disease severity (85%) useful when deciding what genomic results they might want to learn (Graves et al. 2015). A study on general attitudes towards genetic testing found that attitudes in their sample were relatively split, with just about half (47.6%) of participants eventually undergoing genetic testing (Shiloh et al. 2013). This is consistent with Riesgraf et al. who found among participants in a study on attitudes about genetic counseling, specifically that willingness to undergo genetic counseling was evenly split, with 54.7% indicating they would use genetic counseling and 45.3% indicating there were no circumstances in which they would use genetic counseling (2015). Finally, Taber et al. found that perceptions of genome sequencing results were favorable (2015).
Knowledge
Four articles looked at the general public’s knowledge of genetic testing and counseling. Ostergren et al. found that among 1030 direct-to-consumer genetics test participants, there was high comprehension, with an average knowledge score of 79.1% correct (2015). Haga et al. found similar findings, with an average participant score of factual knowledge of genetics of 84% (2013). Carere found that among DTC customers, genetic knowledge was relatively high, with an average baseline score of 8.15 (out of 9) (SD.95) (2016). In a study comparing prenatal genetic knowledge among parous vs. nulliparous women, Mandelberger et al. found that parous women scored significantly higher than nulliparous women on the fundamental genetics quiz (70.9 vs. 61.9%, p < .03) (2015).
Three articles examined how knowledge of genetic testing and counseling would increase after an intervention. Schwartz et al. conducted a study comparing usual care for in-person genetic counseling to telephone genetic counseling and found that post-counseling knowledge score, although not reaching statistical significance, was .03 points higher among telephone counseling participants versus usual care counseling participants (2014). In a randomized trial comparing participants assigned to either an interactive prenatal genetic testing information aid or standard care counseling, Yee et al. found that participants randomized to the interactive tool correctly answered a more significant amount of questions than those randomized to receive usual care counseling (2014). Wolfe et al. created an online tutoring program for patients considering BRCA testing and compared participants assigned to their BRCA Gist program with participants assigned to the National Cancer Institute website and a control group (2015). They found that the BRCA Gist participants scored significantly higher than National Cancer Institute website participants (p < .001), and both scored significantly higher than control group participants (p < .001) (Wolfe et al. 2015).
Perception of risk
Two articles looked at perceived risk after DTC tests. Carere et al. found that elevated risk results associated significantly with a positive change of perceived risk (p < .02), meaning that perceived risk increased when participants received elevated risk results (2015). Boeldt et al. found that among DTC customers, the most commonly cited perceived risks were for heart attack (19.1%) and Alzheimer’s disease (18.6%) (2015).
Targeted recruitment
Table 2 presents the articles that recruited a targeted or selected sample.
Awareness
Three articles looked at awareness of genetic counseling or testing. In a study of patients undergoing testing for Lynch syndrome, Patel et al. found that 63% (n = 104) had heard of genetic testing, with a higher number of patients from high-risk clinics reporting they had heard of genetic testing than those recruited from the general population clinics (71.3 vs. 52.1%, p < .015) (2016). In a study of high-risk Latinas undergoing BRCA genetic counseling, Sussner et al. found that more than half of participants had heard or read “almost nothing” or “relatively little” about BRCA genetic counseling (2013). Armstrong et al. found that awareness of genetic counseling related to physician recommendation, with only 36.8% of patients reporting receiving genetic counseling before testing (2015).
Attitudes
One of the articles focused on attitudes towards prenatal and genetic testing in children. In a study of parents of children affected with Treacher Collins syndrome (TCS), Wu et al. found that 65% of participants reported that the risk of having a child with TCS was of a more significant concern than the risk of miscarriage from prenatal genetic testing (2012). Also, the likelihood of undergoing genetic testing or having their child undergo genetic testing was dependent on how accurate the hypothetical test was, with 87% reporting they would undergo prenatal genetic testing if accuracy were 100% vs. just 6.5% stating they would undergo prenatal genetic testing if accuracy were only 20% (Wu et al. 2012).
Four of the articles tried to identify parental attitudes towards genetic testing in children. In a study of parents with multiple affected offspring with epilepsy, Caminiti et al. found that 85.7% of these parents responded with “definitely or probably yes” for genetic testing with clinical utility and 100% penetrance (2016). However, 74% of parents of no affected offspring responded positively to genetic testing for their offspring (Caminiti et al. 2016). This positive attitude towards genetic testing in children is consistent in other studies, such as Fitzgerald-Butt et al. who found that among parents of children with congenital heart defects, 57.9–89.4% (SD 19.1%) of participants were “somewhat likely or very likely” to undergo genetic testing for their children (2014). Narcisa et al. also found that among parents of at least one child diagnosed with Autism Spectrum Disorder (ASD), that 80% of participants who had a younger, as of yet undiagnosed child, would “want their child tested even if it could not confirm or rule out a diagnosis” (2012). It is not just genetic tests that parents are generally in favor of; it is genetic counseling as well. Waxler et al. found that parents of children diagnosed with Williams Syndrome were more likely to have a positive or mixed diagnostic experience if they saw a genetic counselor (n = 386, 81.60%) (2013).
Positive attitudes towards genetic testing are present when considering genetic testing for cancer in adults. O’Neill et al. found that among young college-aged smokers, participants held moderately strong intentions for GSTM1 enzyme testing (5.21 on a 7-point scale) (2013). Yusuf et al. found similar results among breast cancer patients, who were “generally willing to undergo molecular testing biopsies, and blood draws to guide therapy (75%) and research (46%)” (2015). Similar attitudes presented among high-risk Latinas who had mostly positive attitudes about BRCA genetic counseling (Sussner et al. 2013).
Positive attitudes occurred among participants of studies of genetic testing for non-cancer diseases. Among participants with Alcohol Use Disorder, Scott et al. and Strobel et al. found that 85% (n = 259) and 89%, respectively, expressed willingness to test and provide genetic samples for clinical use (Scott et al. 2014; Strobel et al. 2013). In a study looking at genetic testing for Alzheimer’s disease, Caselli et al. found that 70.4% (2775/3939) were willing to undergo presymptomatic testing even in the absence of any effective intervention (2014). In a study of genetic testing for patients with irritable bowel disorder (IBD), Hooker et al. found that patients perceived the genetic test as more useful for understanding disease etiology and family risks than the standard test (p < .001) (2014). Freedman et al. found that family members of a loved one with nephropathy had intentions to undergo genetic testing (2013). Only one study identified a group that had a more negative attitude towards genetic testing. In a study of veterans and their families on genetic testing for PTSD, Dedert et al. found that compared with non-PTSD participants, those with PTSD had significantly less favorable attitudes towards genetic testing (p < .05) (2012).
Regarding attitudes related to genetic testing in general, Allain et al. found that only 54.3% of participants had heard of the Genetic Information Nondiscrimination Act (GINA) (2012). Also, Matro et al. found that there was a high willingness-to-pay for genetic testing, with 79% (n = 303) willing to pay out-of-pocket, and just 21% (n = 82) were only willing to be tested if entirely covered by insurance (2014).
Knowledge
Overall, genetic knowledge was relatively high among targeted samples. Fitzgerald-Butt et al. found in a study of parents with children who had a congenital heart defect that the mean genetic knowledge summary score was 73.8% correct, with questions on the interaction of the environment and genetics being answered correctly the most, and underlying genetic knowledge being answered correctly the least (2014). Similarly, in a study of parents with children with Batten Disease, Adams et al. found that the mean total score on knowledge questions was 84% correct (SD 11%) (2014). In a study among high-risk Latinas seeking BRCA genetic testing, Sussner et al. found that mean knowledge of genetic counseling was “fairly high” (2013). Patel et al. found that participants from high-risk clinics scored significantly higher on colorectal cancer screening knowledge than those recruited from general population clinics (35.1 vs.12.7%, p < .001) (2016). There was one study in which the majority of participants did not have high knowledge. In a study of patients at a private IVF clinic, Gebhart et al. found that 69% of participants reported no previous knowledge of preimplantation genetic screening before the IVF treatment cycle (2015).
One study assessed the impact of an intervention on genetic knowledge. Gallo et al. conducted a study of participants with sickle cell disease or trait and assigned them to an e-book, CHOICES in-person intervention, or no intervention (2016). At 24 months, both e-book and CHOICES participants had higher knowledge scores compared to controls, with participants in the CHOICES intervention having a significantly higher knowledge improvement rate over time than the e-book group (p < .004) (Gallo et al. 2016).
In a study of undergraduate students in a genetics course, Weber et al. assessed whether genetics quiz scores would increase if students were given the opportunity to look at their genetic information and found that student anticipation of obtaining their genomics data did not result in improved personal genomics quiz scores (2015).
Perception of risk
Three studies looked at the perception of genetic risk among targeted study participants. Andersen et al. found that high-risk women with a family history of breast or ovarian cancer were significantly more likely than others to perceive their risk of breast cancer to be higher than others their age (65.7 vs. 42.1%, p < .05) (2016). In a study on breast cancer risk perception among relatives of family members who tested negative for BRCA mutations, two-thirds of respondents stated their perceived risk of carrying the BRCA1/2 mutation was “somewhat, very, or extremely” likely (Sussner et al. 2013). Tong et al. looked at the intentions for risk-reducing surgery among high-risk women referred for BRCA counseling and found that perceived breast cancer risk was associated with 14–16% (p < .001) increased odds of considering a risk-reducing mastectomy and that women with a higher perceived mutation risk had a 74% (p < .007) increased odds of considering risk-reducing oophorectomy (2015). One article assessed perceptions of risk after genome sequencing among sisters and daughters who had tested negative for a BRCA 1/2 mutation and found that those who shared with their family what their genetic counselor told them had a more accurate perception of risk (Himes et al. 2016).
Discussion
Community leaders have expressed a desire to measure awareness and understanding of genomics (Kaplan et al. 2017). To enable an internal assessment, we identified the need to have tools that can measure the general awareness, attitudes, knowledge, and perceived risk of genomics in the general population. The findings surfaced here provide interesting starting points to inform the use of assessment tools to further inform educational strategies.
This review systematically scanned the literature to identify what people think about genetics. We found that in general people report high levels of knowledge and positive attitudes about genetics. Knowledge scores and attitudinal ratings among both general populations and targeted samples were high. Intervention data, while limited, indicate slight improvements in knowledge, possibly because of the high baseline values. A recent summary and review presented at a national meeting (Kaphingst 2018) found that knowledge can be measured differently and is often poorly defined, indicating that this should be an area of future research. If general knowledge about genetics is only weakly useful to people making decisions about testing and interpretation, then other variables might be influencing behaviors regarding genetics and could be better conceptualized and measured.
As access to genetic tools expands, more public exposure to genomics and genomics education could occur during a variety of activities such as visiting the doctor, having a baby, watching the nightly news, and through social conversations. As genomics further intersects with law, public health, medicine, agriculture, research, politics, and consumer products, decision-making in the field of genomics will have considerable consequences to members of the public and specific patient and community groups. It is essential that people have the appropriate tools to actively participate in broader discussions and decision-making, especially in setting policy, research priorities, protections, and strategies for equitable inclusion. Citizen groups are actively seeking informational sources for foundational knowledge of genomics, its applications, and the ethical considerations to enable and empower them to further engage with genomic issues and decision-making (Follett and Strezov 2015). In response, educators, clinicians, researchers, and the governmental representatives have convened to understand better how to meet overall and specific needs for genetic knowledge and understanding.
One of the interesting findings to come from this review is the alignment of attitudes and awareness reports of genetic testing, when the actual tests studied, situations, and populations are quite different. Generally, people report positive attitudes about genetics, despite differences in the uses of genetic technology and findings for diagnostic and clinical decisions, as well as general judgments about genetic utility. One explanation for this is that individual respondents are not considering the individual differences among all the different ways that genetic knowledge and testing can be used and the various ramifications that results can have. Clearer definitions of what is being measured and how the engaged sample defines the testing under scrutiny might clarify this. Also, more careful conceptualization of what is meant by knowledge and what aspects of knowledge are relevant to the problem under study could clarify this (Kaphingst 2018). General knowledge about DNA might not be relevant in a situation where testing reveals a child at risk of a later-onset disease process.
Further complicating this picture is the use of hypothetical situations as cues for responses to surveys as opposed to actual cases in which genetics is relevant to medical decisions. In this review, we found that attitudes towards genetic testing in the hypothetical were quite high. We first saw this gap between the early research on the predicted uptake of Huntington’s disease testing as potentially very high, and the actual uptake when offered, which was several percentage points lower. This discrepancy points to the need for better more careful research into what people think about genetics in specific situations (Forrest et al. 2012).
In the studies we reviewed on public awareness, it seems that only about half or less of the general public reports awareness of genetics as useful or relevant. Though this is impressive, a substantial part of the population is still unaware of genetics. Of those who have some awareness, reports are positive towards testing, though this is not surprising given that a majority of those who encounter genomic education come through the clinic. There is high general support for the use of genetic testing preimplantation during assisted reproduction and high interest in personalized testing in general, for example among children of adults with incurable dementia-related diseases. Genomics is also perceived to be a tool in supporting treatment of childhood conditions.
Interestingly, a significant gap exists between someone’s stated willingness to utilize genetic testing and pursuing I, as indicated by the relatively positive attitudes about genetics compared to the national uptake of testing in the general public, which is low (Wilkes et al. 2017). This could be due to concerns regarding how genetic information is used, especially in determining access to health and life insurance. Further, many people are not aware of the current federal protections in place, as found in the review.
Those who encounter genomics in the clinical setting (targeted recruitment) have a slightly higher knowledge of the subject than the general population. Targeted populations perceive genomic medicine as a tool providing critical information when faced with medical decisions. Attitudes in targeted population towards the use of genomic technology are positive for understanding disease etiology, risk brackets, and treatment plans. Of the targeted populations surveyed, there were also negative attitudes when associating genetics with PTSD. Given the historical misuse of genetic data and the intersection of genomics with social stigma and ill-informed perception, it is vital the attitudes and perceived risk of people surveyed are from all stakeholders involved in the outcomes of decision-making.
The research on the knowledge, awareness, attitudes, and perceived risk beyond patients engaged in health care is considerably sparser. This research essentially has excluded a diverse sample of participants, participants who do not have access to health care or access care through fragmented systems that do not have easy methods of collecting survey data. We need to understand how broader, more diverse population samples view genetics and how people receive care in public clinics and through more patchwork systems and referrals understand and use genetic information. Targeting assessments to such settings is one solution for filling this gap. Another idea is to create more forums that provide knowledge on genomics and opportunities to discuss the application of genomics tools to modern life. Because genetic counseling has been an important source of education of familial genetics, including a discussion of broader ethical, legal, and social issues into clinic settings is an important mechanism of disseminating information through the family and their more expansive network. Given the limited access and availability of genetic counseling and the barriers to receiving genomics-informed care, investing in community-driven genomics educational strategies is ideal. In developing community-specific educational strategies, special attention should focus on groups that are absent from historical and current conversations on genetics, health, research, or policy (Anderson et al. 2012; Brandt et al. 2008; Sadler et al. 2010; Doherty et al. 2004; Khoury et al. 2003). Successful partnerships and educational strategies require recognition and validation of previous social misuse of genetic data.
Conflict of interest
Erin LePoire, Deborah Bowen, Lorelei Walker, and Bashakhi Basu declare that they have no conflicting interests.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- Adams HR, Rose K, Augustine EF, Kwon JM, deBlieck EA, Marshall FJ, Vierhile A, Mink JW, Nance MA. Experience, knowledge, and opinions about childhood genetic testing in batten disease. Mol Genet Metab. 2014;111(2):197–202. doi: 10.1016/j.ymgme.2013.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agurs-Collins T, Ferrer R, Ottenbacher A, Waters EA, O’Connell ME, Hamilton JG. Public awareness of direct-to-consumer genetic tests: findings from the 2013 U.S. Health Information National Trends Survey. J Cancer Educ. 2015;30(4):799–807. doi: 10.1007/s13187-014-0784-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allain DC, Friedman S, Senter L. Consumer awareness and attitudes about insurance discrimination post-enactment of the Genetic Information Nondiscrimination Act. Familial Cancer. 2012;11(4):637–644. doi: 10.1007/s10689-012-9564-0. [DOI] [PubMed] [Google Scholar]
- Allyse M, Sayres LC, Goodspeed TA, Cho MK. Attitudes towards non-invasive prenatal testing for aneuploidy among US adults of reproductive age. J Perinatol. 2014;34(6):429–434. doi: 10.1038/jp.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen MR, Thorpe J, Buist DS, et al. Cancer risk awareness and concern among women with a family history of breast or ovarian cancer. Behav Med (Washington, DC) 2016;42(1):18–28. doi: 10.1080/08964289.2014.947234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson B, McLosky J, Wasilevich E, Lyon-Callo S, Duquette D, Copeland G. Barriers and facilitators for utilization of genetic counseling and risk assessment services in young female breast cancer survivors. J Cancer Epidemiol. 2012;2012:298745. doi: 10.1155/2012/298745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong J, Toscano M, Kotchko N. Utilization and outcomes of BRCA genetic testing and counseling in a nationally commercially insured population: the ABOUT Study. JAMA Oncol. 2015;1(9):1251–1260. doi: 10.1001/jamaoncol.2015.3048. [DOI] [PubMed] [Google Scholar]
- Boeldt DL, Schork NJ, Topol EJ, Bloss CS. Influence of individual differences in disease perception on consumer response to direct-to-consumer genomic testing. Clin Genet. 2015;87(3):225–232. doi: 10.1111/cge.12419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen D, Hyams T, Goodman M, West K, Harris-Wai J, Yu J-H. Systematic review of quantitative measures of stakeholder engagement. Clin Transl Sci. 2017;10(5):314–336. doi: 10.1111/cts.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt R, Ali Z, Sabel A, McHugh T, Gilman P (2008) Cancer genetics evaluation: barriers to and improvements for referral. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/18373400 [DOI] [PubMed]
- Caminiti CB, Hesdorffer DC, Shostak S, Goldsmith J, Sorge ST, Winawer MR, Phelan JC, Chung WK, Ottman R. Parents’ interest in genetic testing of their offspring in multiplex epilepsy families. Epilepsia. 2016;57(2):279–287. doi: 10.1111/epi.13287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carere DA, VanderWeele T, Moreno TA, et al. The impact of direct-to-consumer personal genomic testing on perceived risk of breast, prostate, colorectal, and lung cancer: findings from the PGen study. BMC Med Genet. 2015;8(1):63. doi: 10.1186/s12920-015-0140-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carere DA, Kraft P, Kaphingst KA, Roberts JS, Green RC. Consumers report lower confidence in their genetics knowledge following direct-to-consumer personal genomic testing. Genet Med. 2016;18(1):65–72. doi: 10.1038/gim.2015.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caselli RJ, Langbaum J, Marchant GE, Lindor RA, Hunt KS, Henslin BR, Dueck AC, Robert JS. Public perceptions of presymptomatic testing for Alzheimer’s disease. Mayo Clin Proc. 2014;89(10):1389–1396. doi: 10.1016/j.mayocp.2014.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedert EA, Elbogen EB, Hauser MA, Hertzberg JS, Wilson SM, Dennis MF, Calhoun PS, Kirby AC, Beckham JC. Consumer perspectives on genetic testing for psychiatric disorders: the attitudes of veterans with posttraumatic stress disorder and their families. Genet Test Mol Biomarkers. 2012;16(9):1122–1129. doi: 10.1089/gtmb.2012.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodson DS, Goldenberg AJ, Davis MM, Singer DC, Tarini BA. Parent and public interest in whole genome sequencing. Public Health Genomics. 2015;18(3):151–159. doi: 10.1159/000375115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty P, Stott A, Kinder K (2004) Delivering services to hard to reach families in on track areas: definition, consultation and needs assessment. Home Office Development and Practice Report 15:1–18
- Farrell RM, Agatisa PK, Nutter B. What women want: lead considerations for current and future applications of noninvasive prenatal testing in prenatal care. Birth. 2014;41(3):276–282. doi: 10.1111/birt.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald-Butt SM, Klima J, Kelleher K, Chisolm D, McBride KL. Genetic knowledge and attitudes of parents of children with congenital heart defects. Am J Med Genet A. 2014;164(12):3069–3075. doi: 10.1002/ajmg.a.36763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Follett R, Strezov V. An analysis of citizen science-based research: usage and publication patterns. PLoS One. 2015;10(11):e0143687. doi: 10.1371/journal.pone.0143687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest L, Delatycki M, Curnow L, Couns MG, Skene L, Aitken M (2012) An audit of clinical service examining the uptake of genetic testing by at-risk family members. Retrieved from https://www.nature.com/articles/gim2011 [DOI] [PubMed]
- Freedman BI, Fletcher AJ, Sanghani VR, Spainhour M, Graham AW, Russell GB, Cooke Bailey JN, Iltis AS, King NMP. Perceptions regarding genetic testing in populations at risk for nephropathy. Am J Nephrol. 2013;38(6):453–457. doi: 10.1159/000356244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo AM, Wilkie DJ, Yao Y, Molokie RE, Stahl C, Hershberger PE, Zhao Z, Suarez ML, Johnson B, Angulo R, Carrasco J, Angulo V, Thompson AA. Reproductive health CHOICES for young adults with sickle cell disease or trait: randomized controlled trial outcomes over two years. J Genet Couns. 2016;25(2):325–336. doi: 10.1007/s10897-015-9874-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebhart MB, Hines RS, Penman A, Holland AC. How do patient perceived determinants influence the decision-making process to accept or decline preimplantation genetic screening? Fertil Steril. 2015;105(1):188–193. doi: 10.1016/j.fertnstert.2015.09.022. [DOI] [PubMed] [Google Scholar]
- Graves KD, Sinicrope PS, McCormick JB, Zhou Y, Vadaparampil ST, Lindor NM. Public perceptions of disease severity but not actionability correlate with interest in receiving genomic results: nonalignment with current trends in practice. Public Health Genomics. 2015;18(3):173–183. doi: 10.1159/000375479. [DOI] [PubMed] [Google Scholar]
- Haga SB, Barry WT, Mills R, Ginsburg GS, Svetkey L, Sullivan J, Willard HF. Public knowledge of and attitudes toward genetics and genetic testing. Genet Test Mol Biomarkers. 2013;17(4):327–335. doi: 10.1089/gtmb.2012.0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higuchi EC, Sheldon JP, Zikmund-Fisher BJ, Yashar BM. Non-invasive prenatal screening for trisomy 21: consumers’ perspectives. Am J Med Genet. 2016;170(2):375–385. doi: 10.1002/ajmg.a.37460. [DOI] [PubMed] [Google Scholar]
- Himes DO, Clayton MF, Donaldson GW, Ellington L, Buys SS, Kinney AY. Breast cancer risk perceptions among relatives of women with uninformative negative BRCA1/2 test results: the moderating effect of the amount of shared information. J Genet Couns. 2016;25:258–269. doi: 10.1007/s10897-015-9866-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker GW, Peay H, Erby L, Bayless T, Biesecker BB, Roter DL. Genetic literacy and patient perceptions of IBD testing utility and disease control: a randomized vignette study of genetic testing. Inflamm Bowel Dis. 2014;20(5):901–908. doi: 10.1097/MIB.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Initiatives and Resources for Minority and Special Populations (n.d.) Retrieved from https://www.genome.gov/10001192/initiatives-and-resources-for-minority-and-special-populations/. Accessed 1 Nov 2018
- Kaphingst K(2018). Beyond knowledge: addressing genomic literacy in the translation of genomic technologies. Society of Behavioral Medicine, New Orleans, LA, April 12th, 2018
- Kaplan B, Caddle-Steele C, Chisholm G, Esmond WA, Ferryman K, Gertner M, Goytia C, Hauser D, Richardson LD, Robinson M, Horowitz CR. A culture of understanding: reflections and suggestions from a genomics research community board. Prog Community Health Partnersh. 2017;11(2):161–165. doi: 10.1353/cpr.2017.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury MJ, McCabe LL, McCabe ER. Population screening in the age of genomic medicine. N Engl J Med. 2003;348(1):50–58. doi: 10.1056/NEJMra013182. [DOI] [PubMed] [Google Scholar]
- Kolor K, Duquette D, Zlot A, Foland J, Anderson B, Giles R, Wrathall J, Khoury MJ. Public awareness and use of direct-to-consumer personal genomic tests from four state population-based surveys, and implications for clinical and public health practice. Genet Med. 2012;14(10):860–867. doi: 10.1038/gim.2012.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mai PL, Vadaparampil ST, Breen N, McNeel TS, Wideroff L, Graubard BI. Awareness of cancer susceptibility genetic testing: the 2000, 2005, and 2010 National Health Interview Surveys. Am J Prev Med. 2014;46(5):440–448. doi: 10.1016/j.amepre.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandelberger AH, Robins JC, Buster JE, Strohsnitter WC, Plante BJ. Preconception counseling: do patients learn about genetics from their obstetrician-gynecologists? J Assist Reprod Genet. 2015;32(7):1145–1149. doi: 10.1007/s10815-015-0491-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matro JM, Ruth KJ, Wong Y-N, McCully KC, Rybak CM, Meropol NJ, Hall MJ. Cost sharing and hereditary cancer risk: predictors of willingness-to-pay for genetic testing. J Genet Couns. 2014;23(6):1002–1011. doi: 10.1007/s10897-014-9724-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormick KA, Calzone KA. The impact of genomics on health outcomes, quality, and safety. Nurs Manag. 2016;47(4):23–26. doi: 10.1097/01.NUMA.0000481844.50047.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narcisa V, Discenza M, Vaccari E, Rosen-Sheidley B, Hardan AY, Couchon E. Parental interest in a genetic risk assessment test for autism spectrum disorders. Clin Pediatr (Phila) 2012;52(2):139–146. doi: 10.1177/0009922812466583. [DOI] [PubMed] [Google Scholar]
- O’Neill SC, Lipkus IM, Sanderson SC, Shepperd J, Docherty S, McBride CM. Motivations for genetic testing for lung cancer risk among young smokers. Tob Control. 2013;22(6):406–411. doi: 10.1136/tobaccocontrol-2011-050306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostergren JE, Gornick MC, Carere DA, Kalia SS, Uhlmann WR, Ruffin MT, Mountain JL, Green RC, Roberts JS, for the PGen Study Group How well do customers of direct-to-consumer personal genomic testing services comprehend genetic test results? Findings from the impact of personal genomics study. Public Health Genomics. 2015;18(4):216–224. doi: 10.1159/000431250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkman AA, Foland J, Anderson B, Duquette D, Sobotka H, Lynn M, Nottingham S, Dotson WD, Kolor K, Cox SL. Public awareness of genetic nondiscrimination laws in the four states and perceived importance of life insurance protection. J Genet Couns. 2015;24(3):512–521. doi: 10.1007/s10897-014-9771-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SG, Ahnen DJ, Kinney AY, Horick N, Finkelstein DM, Hill DA, Lindor NM, MaCrae F, Lowery JT. Knowledge and uptake of genetic counseling and colonoscopic screening among persons at increased risk for lynch syndrome and their endoscopists from the Family Health Promotion Project. Am J Gastroenterol. 2016;111(2):285–293. doi: 10.1038/ajg.2015.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riesgraf RJ, Veach PM, MacFarlane IM, LeRoy BS. Perceptions and attitudes about genetic counseling among residents of a midwestern rural area. J Genet Couns. 2015;24(4):565–579. doi: 10.1007/s10897-014-9777-5. [DOI] [PubMed] [Google Scholar]
- Sadler GR, Lee H-C, Seung-Hwan Lim R, Fullerton J. Recruiting hard-to-reach United States population sub-groups via adaptations of snowball sampling strategy. Nurs Health Sci. 2010;12(3):369–374. doi: 10.1111/j.1442-2018.2010.00541.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayres LC, Allyse M, Goodspeed TA, Cho MK. Demographic and experiential correlates of public attitudes towards cell-free fetal DNA screening. J Genet Couns. 2014;23(6):957–967. doi: 10.1007/s10897-014-9704-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MD, Valdimarsdottir HB, Peshkin BN, Mandelblatt J, Nusbaum R, Huang AT, Chang Y, Graves K, Isaacs C, Wood M, McKinnon W, Garber J, McCormick S, Kinney AY, Luta G, Kelleher S, Leventhal KG, Vegella P, Tong A, King L. Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. J Clin Oncol. 2014;32(7):618–626. doi: 10.1200/JCO.2013.51.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott DM, Nwulia E, Kwagyan J, Cain G, Marshall VJ, Kalu N, Ewing A, Taylor RE. Genetic testing for the susceptibility to alcohol dependence: interest and concerns in an African American population. Genet Test Mol Biomarkers. 2014;18(8):538–545. doi: 10.1089/gtmb.2013.0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiloh S, Wade CH, Roberts JS, Alford SH, Biesecker BB. On averages and peaks: how do people integrate attitudes about multiple diseases to reach a decision about multiplex genetic testing? Med Decis Mak. 2013;33(1):71–77. doi: 10.1177/0272989X12464432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer E, Couper MP, Raghunathan TE, Van Hoewyk J, Antonucci TC. Trends in U.S. attitudes toward genetic testing, 1990–2004. Public Opin Q. 2008;72(3):446–458. doi: 10.1093/poq/nfn033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinbach RJ, Allyse M, Michie M, Liu EY, Cho MK. “This lifetime commitment”: public conceptions of disability and noninvasive prenatal genetic screening. Am J Med Genet A. 2016;170A(2):363–374. doi: 10.1002/ajmg.a.37459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strobel B, McManus L, Leong S, et al. A cross-sectional study of attitudes about the use of genetic testing for clinical care among patients with an alcohol use disorder. Alcohol Alcohol (Oxford, Oxfordshire) 2013;48(6):700–703. doi: 10.1093/alcalc/agt130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussner KM, Jandorf L, Thompson HS, Valdimarsdottir HB. Barriers and facilitators to BRCA genetic counseling among at-risk Latinas in New York City. Psycho-Oncology. 2013;22(7):1594–1604. doi: 10.1002/pon.3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney SM, Hastrup JL, Hyland A, Rivard C. A follow-up community survey of knowledge and beliefs about cancer and genetics. J Cancer Educ. 2016;31(2):253–260. doi: 10.1007/s13187-015-0856-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taber JM, Klein WM, Ferrer RA, et al. Perceived ambiguity as a barrier to intentions to learn genome sequencing results. J Behav Med. 2015;38(5):715–726. doi: 10.1007/s10865-015-9642-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A, Kelly S, Nusbaum R, Graves K, Peshkin BN, Valdimarsdottir HB, Wood M, McKinnon W, Garber J, McCormick SR, Jandorf L, Schwartz MD. Intentions for risk-reducing surgery among high-risk women referred for BRCA1/BRCA2 genetic counseling. Psycho-Oncology. 2015;24(1):33–39. doi: 10.1002/pon.3560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waxler JL, Cherniske EM, Dieter K, Herd P, Pober BR. Hearing from parents: the impact of receiving the diagnosis of Williams syndrome in their child. Am J Med Genet. 2013;161(3):534–541. doi: 10.1002/ajmg.a.35789. [DOI] [PubMed] [Google Scholar]
- Weber KS, Jensen JL, Johnson SM. Anticipation of personal genomics data enhances interest and learning environment in genomics and molecular biology undergraduate courses. PLoS One. 2015;10(8):e0133486. doi: 10.1371/journal.pone.0133486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkes MS, Fancher TL, McDermott H, Lehman E, Bell RA, Green MJ (2017) Increasing confidence and changing behaviors in primary care providers engaged in genetic counseling. Retrieved from https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-017-0982-4 [DOI] [PMC free article] [PubMed]
- Winkelman WD, Missmer SA, Myers D, Ginsburg ES. Public perspectives on the use of preimplantation genetic diagnosis. J Assist Reprod Genet. 2015;32(5):665–675. doi: 10.1007/s10815-015-0456-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe CR, Reyna VF, Widmer CL, Cedillos EM, Fisher CR, Brust-Renck PG, Weil AM. Efficacy of a web-based intelligent tutoring system for communicating genetic risk of breast cancer: a fuzzy-trace theory approach. Med Decis Mak. 2015;35(1):46–59. doi: 10.1177/0272989X14535983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu RL, Lawson CS, Jabs EW, Sanderson SC. Attitudes toward prenatal genetic testing for Treacher Collins syndrome among affected individuals and families. Am J Med Genet. 2012;158A(7):1556–1567. doi: 10.1002/ajmg.a.35379. [DOI] [PubMed] [Google Scholar]
- Yang D, Hillman SL, Harris AM, Sinicrope PS, Devens ME, Ahlquist DA. Patient perceptions of stool DNA testing for pan-digestive cancer screening: a survey questionnaire. World J Gastroenterol: WJG. 2014;20(17):4972–4979. doi: 10.3748/wjg.v20.i17.4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yee LM, Wolf M, Mullen R, et al. A randomized trial of a prenatal genetic testing interactive computerized information aid. Prenat Diagn. 2014;34(6):552–557. doi: 10.1002/pd.4347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf RA, Rogith D, Hovick SR, et al. Attitudes towards molecular testing for personalized cancer therapy. Cancer. 2015;121(2):243–250. doi: 10.1002/cncr.28966. [DOI] [PMC free article] [PubMed] [Google Scholar]