Abstract
Background
The acromioclavicular joint (ACJ) is one of the more common sites of shoulder girdle injury, accounting for 4–12% of all such injuries, with an incidence of 3–4 cases per 100 000 persons per year in the general population. Current topics of debate include the proper standard diagnostic evaluation, the indications for surgery, and the best operative method.
Methods
This review is based on publications retrieved by a selective literature search.
Results
Mechanical trauma of the ACG can tear the ligamentous apparatus that holds the acromion, clavicle, and coracoid process together. Different interventions are indicated depending on the nature of the injury. In recent years, the horizontal component of the instability has received more attention, in addition to its vertical component. Persistent instability can lead to chronic, painful limitation of shoulder function, particularly with respect to working above the head. Surgical stabilization is therefore recommended for high-grade instability of Rockwood types IV and V. Modern reconstruction techniques enable selective vertical and horizontal treatment of the instability and have been found superior to traditional methods, particularly in young athletes. Arthroscopic techniques are advantageous because they are less invasive, do not require removal of implanted material, and afford the opportunity to diagnose any accompanying lesions definitively and to treat them if necessary. Surgery for acute injuries should be performed within three weeks of the trauma. For chronic injuries, additional tendon augmentation is now considered standard treatment.
Conclusion
High-grade ACJ instability is a complex and significant injury of the shoulder girdle that can cause persistent pain and functional impairment. The state of the evidence regarding its optimal treatment is weak. Large-scale, prospective, randomized comparative studies are needed in order to define a clear standard of treatment.
Mechanical trauma of the acromioclavicular (AC) joint can result in the rupture of the ligament complex extending between the acromion, the clavicle and the coracoid process. Corresponding to the magnitude of the force to the shoulder, the severity of the injury is classified into various grades. Higher-grade injuries with complete rupture of the coracoclavicular ligaments may result in permanent impairment of shoulder function. In addition, the marked bulging of the lateral clavicle compared to the unaffected side occasionally gives rise to esthetic concerns.
For decades, the correct diagnosis and management of acute injuries to the AC joint have remained the subject of controversy among orthopedic surgeons and trauma surgeons. Using arthroscopically assisted surgical techniques, today the injury can be treated less invasively.
This article presents the current aspects of the diagnosis and treatment of acute instability of the AC joint based on a selective search of the literature. Particular attention was given to high level of evidence studies, to the extent these were available.
Epidemiology
Acute dislocation of the AC joint typically occurs in young, athletic adults and is one of the most common injuries of the shoulder girdle (4–12%) (1). Its absolute incidence is approximately 3–4/100 000 population (2). The native stabilizers of the AC joint are frequently damaged during high-risk/high-energy contact sports, such as ice hockey, rugby or handball (3). In alpine skiing, approximately 20% (77/393) of all injuries to the shoulder girdle affect the AC joint (4).
Mechanism of injury
In case of a direct blow to the shoulder girdle, the forces act directly on the AC joint and the acromioclavicular and coracoclavicular (CC) ligaments. By contrast, in case of a fall on an extended arm, the force acts indirectly on the AC joint. Here, the humeral head presses against the acromion; thus, the mechanism is an axial compression.
Clinical diagnosis and physical examination
During the clinical examination for acute AC joint injury, patients typically present holding their arm adducted to relieve the pain. In addition, there is painful limitation of mobility of the affected shoulder (especially with flexion and abduction beyond 90°). Neurological injury to the brachial plexus has to be ruled out. When visually inspecting the patient, particular attention should be paid to bruises, abrasions and elevation of the clavicle, a pathognomonic sign of AC joint dislocation. The elevation should be understood as a “pseudo-elevation“ or depression of the scapula, resulting from the loss of the “bony bridge“ to the thorax. The area directly above the AC joint is tender and the cross-body test (horizontal adduction test) is also painful. The initial clinical examination should include testing for horizontal shifting (anterior-posterior translation) of the clavicle and assessment of the reducibility of the AC joint (5). In the presence of significant pain, mobility may be a limiting factor. In patients with only minor elevation of the clavicle, it is key to compare horizontal shifting (increased anterior-posterior translation) on the affected side with that on the unaffected side (6).
In patients with chronic instability, symptoms are unspecific and the pain can radiate into the upper arm or neck. In this case, comparative assessment of the instability of the affected side versus the unaffected side is paramount.
Classification
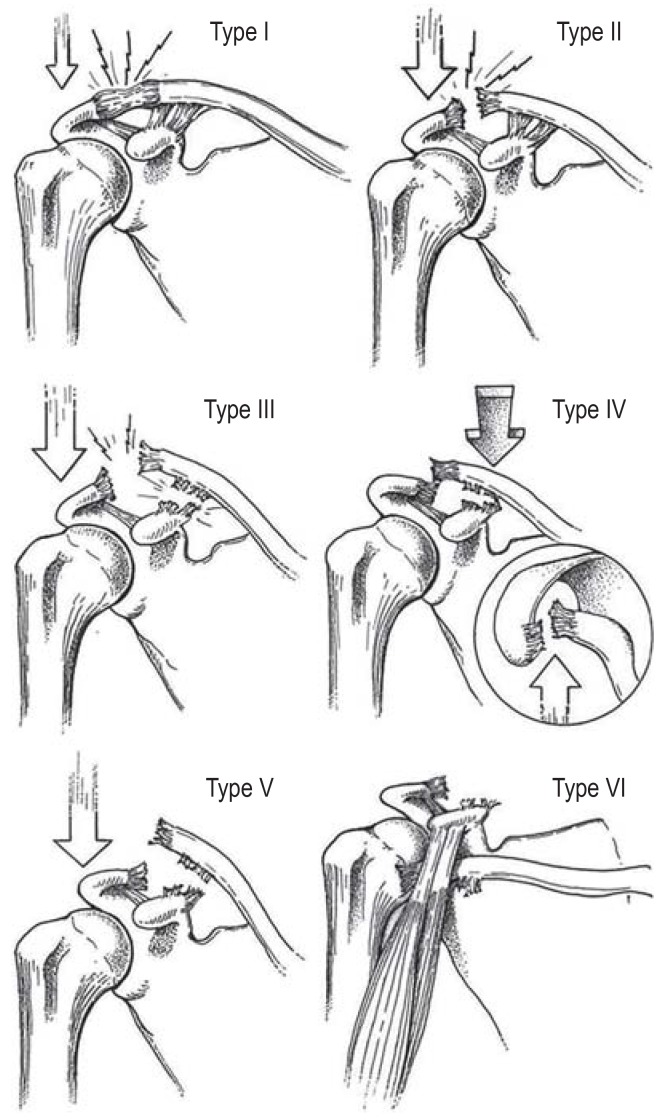
In 1989, Rockwood et al. presented a radiographic classification system for AC joint injury which is still in use today (7). Type I represents a sprain of the acromioclavicular ligament complex and type II a rupture of the AC ligaments, while the coracoclavicular (CC) ligaments are still intact. Rockwood type III injuries are characterized by a complete rupture of both the AC ligaments and the CC ligaments. However, the deltotrapezial fascia is not injured; thus, the clavicle is only displaced by the width of the shaft (25% to 100% increased CC distance). Type IV describes an injury where the lateral clavicle is displaced posteriorly. This injury is caused by a complete rupture of the AC ligaments and a partial rupture of the CC ligaments. The relative elevation of the lateral clavicle varies with the severity of the injury to the CC ligaments. A type V injury involves a complete rupture of the AC ligaments and the CC ligaments as well as a rupture of the deltotrapezial fascia. Radiography shows elevation of the lateral clavicle compared to the acromion by more than a shaft width (>100% increased CC distance). Type VI injury is characterized by a subacromial or subcoracoid position of the lateral clavicle (Figure) (7).
Figure 1.
Rockwood classification of acute AC joint injury—with reprint permission from [e7] (Reprinted by courtesy of Springer Nature).
Imaging studies
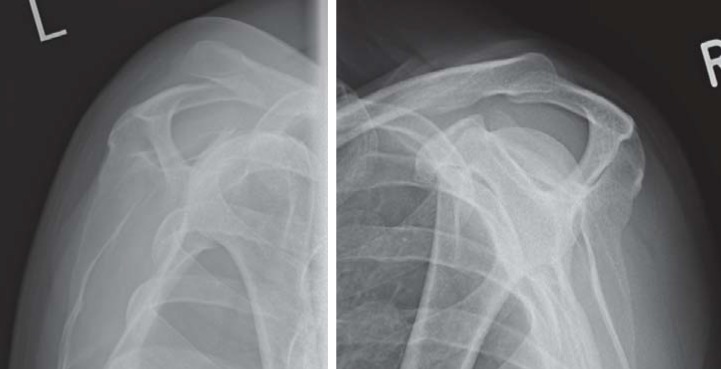
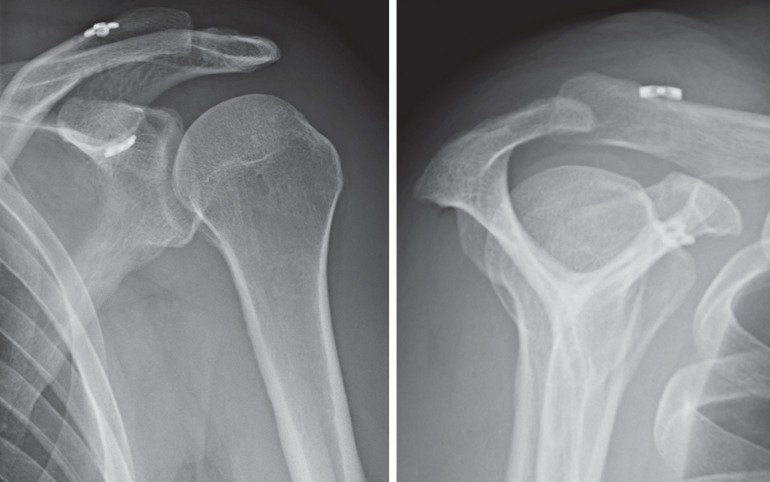
Conventional radiographic assessment of patients with clinically suspected instability of the AC joint should include a bilateral, weight-bearing Zanca view radiograph (10 kg, “water-bearer” radiograph, Figure 2), an axial radiograph and bilateral Alexander view radiographs (outlet view with cross-body maneuver) (figure 3) (8). Non-weight-bearing Zanca view radiographs should no longer be used, as they may result in significant underestimation of the injury (9). Furthermore, taking into account radiation hygiene considerations, panoramic radiographs should not be obtained, but selective radiographs of the two AC joints, excluding the superior thoracic aperture.
Figure 3.
Bilateral weight-bearing Alexander view radiographs to assess the horizontal stability of the acromioclavicular joint
With these special diagnostic techniques, a relative elevation of the lateral clavicle, a dorsal displacement of the clavicle, and a higher-grade horizontal instability can be diagnosed (6, 10).
Magnetic resonance (MR) imaging is not a standard diagnostic modality and is not suitable for differentiating AC joint injuries. It may be used for a more detailed assessment of ligament complex tears (11) or to rule out concomitant injuries (12).
Management
Indication
Despite the high prevalence of acute injury to the AC joint, only few evidence-based treatment recommendations are available (13). They are primarily based on the Rockwood classification or the modified Rockwood classification proposed by ISAKOS; however, their interobserver and intraobserver reliability is poor (κ = 0.278 and 0.468, respectively) (6, 14, 15).
In Germany, conservative treatment of lower-grade acute AC joint injuries of Rockwood type I to II is still considered the standard of care (16, 17). For Rockwood type III injuries, the currently available data is not sufficient to support surgical or conservative treatment (18). In general, surgical management is rather recommended to younger patients with high functional requirements, regular performance of shoulder-straining activities (e.g. overhead work, overhead sporting activities) and injury to the dominant arm. By contrast, conservative treatment is more commonly used in older patients with lower functional requirements and/or with comorbidities (16). The treatment decision is further influenced by the subclassification of Rockwood type III injuries in Rockwood type IIIA and Rockwood type IIIB, as proposed by ISAKOS (6). Rockwood type IIIA injuries without dynamic horizontal instability of the AC joint are considered uncomplicated in nature and consequently are often treated conservatively. However, this approach is also not supported by scientific data from the literature. By contrast, Rockwood type IIIB injuries are characterized by a dynamic horizontal instability, shown to be an independent risk factor for poor functional outcomes (19).
In German-speaking countries and across Europe, there is widespread agreement that high-grade AC joint injuries (Rockwood type IV and V) represent a relative indication for surgery (20). Yet, here again, individual factors, requirements and wishes of patients should be taken into account in the decision-making process (box 1) (21).
BOX 1. Summary of assessment and treatment of acute AC joint injury.
-
Initial treatment
-
Sling for comfort
(Rockwood type I and II injuries) for max. 2 weeks
-
-
Imaging studies
Zanca view radiograph with bilateral weight-bearing (10 kg); bilateral Alexander view radiograph, axial view
-
Follow-up
After 2 weeks: start of physiotherapy (adapted to pain levels)
-
Specialist referral to evaluate indication for surgery
Rockwood type III to VI injuries
By contrast, in the United States, surgical treatment of acute AC joint separation has become the exception rather than the rule. There, patients are only surgically treated if conservative treatment has failed, because allografts are readily available.
It can be expected that in the near future studies evaluating failure of conservative treatment will be published which can help to redefine the indication for conservative management.
Timing of treatment
In the surgical management of acute AC joint injuries, the timing of the surgical intervention represents a factor of clinical relevance. Experts speak of an acute injury up to 3 weeks after the accident and of a chronic injury 6 or more weeks after the accident (level of evidence [LoE] V) (22). The subacute stage of injury between the third and sixth week after the trauma has not been classified in detail.
Song et al. concluded from a systematic review of the literature that early treatment within the first 3 weeks may achieve better outcomes in terms of shoulder function and reduction. However, the authors call for studies with a higher level of evidence to support this conclusion (LoE IV) (23). A French multicenter trial even defined the critical period for treatment as 10 days (24). This is in line with recent basic research in histology, describing a very dynamic biological healing response of the injured ligamentous structures.
Even though high level of evidence studies have not yet been conducted, it is reasonable to recommend, based on the available evidence, that surgical treatment of acute AC joint injuries should be performed as early as possible, but not later than within 3 weeks after the trauma.
Conservative treatment
The early stage of conservative treatment of acute AC joint injuries includes:
Pain-adapted immobilization for a maximum of 2 weeks
Local cooling
As-needed (PRN) analgesics.
Active exercising of the shoulder begins in week 3. The ranges of motion are gradually increased in adaptation to pain levels. During the first 6 weeks, an abduction limit of 90° in the scapular level should be observed. Increased exertions and, in particular, activities involving lifting should be avoided during the first 3 months. Starting from month 3, controlled building of shoulder girdle muscles can be initiated.
Conservative treatment of Rockwood type III injuries is associated in more than half of the patients with the development of scapular dyskinesis, culminating in SICK scapula syndrome (25). Scapular dyskinesis refers to malpositioning and abnormal movements of the scapula in relation to the thorax (26). The SICK scapula syndrome describes an overuse syndrome with muscular fatigue, scapular dyskinesis and pain (27). Using a specific six-week training and stretching program for scapula-stabilizing muscles and trunk muscles, AC joint-associated scapular dyskinesis can be treated successfully with conservative management in almost 80% of cases.
Surgical treatment—Techniques
In daily clinical practice, both arthroscopically assisted acromioclavicular joint stabilization with so-called “pulley systems” and hook plate fixation are regarded as standard techniques. During hook plate stabilization using an open approach, the implant is placed in such a way that the hook of the plate rests underneath the acromion and the plate is fixed with the screws on the clavicle (efigure 1). During arthroscopically assisted AC joint stabilization, a transclavicular-transcoracoid tunnel is drilled under arthroscopic guidance and a suture anchor construct is placed, supported by 2 small titanium plates underneath the coracoid and above the clavicle to secure the reduction achieved (28). Here, today a technique with only one CC tunnel of a significantly smaller diameter (2.4 mm) is increasingly used to minimize the risk of clavicular and coracoid fracture (efigure 2) (29, 30).
eFigure 1.
Postoperative radiograph of a temporary hook plate retention
eFigure 2.
Postoperative radiograph of an arthroscopic stabilization using the pulley implant technique
A survey conducted by Balke et al. found that specialists in shoulder surgery preferred arthroscopic stabilization, while the hook plate was most commonly used for basic care by non-specialists (20). Both techniques have technical advantages and disadvantages as well as a specific complication profile, significantly influencing the individual choice of the procedure (Box 2 and 3) (31).
BOX 2. Hook plate advantages and disadvantages as well as its specific complication profile (from [1–6]).
-
Advantages
Possibility of early functional postoperative treatment; up to 90° abduction possible
Efficient basic care
Low technical requirements
No residual foreign body after implant removal
-
Disadvantages and complications
No treatment of glenohumeral co-pathologies (prevalence up to 20%, especially >45 years) Implant removal required
Acromial osteolysis (prevalence 20–50%)
Acromion fracture (prevalence approx. 2%)
Subacromial impingement (prevalence up to 40%)
BOX 3. Advantages and disadvantages as well as specific complication profile of arthroscopic stabilization (from [7–11]).
-
Advantages
Simultaneous treatment of glenohumeral co-pathologies
Single-stage, minimally invasive surgery
High patient acceptance
-
Disadvantages and complications
Technically challenging procedure to be performed by specialists
More restrictive postoperative treatment
Implant retention and implant irritation (prevalence up to 25%)
Iatrogenic clavicle and coracoid fractures (prevalence up to 20%)
Recently, this exclusively coracoclavicular technique has been supplemented by an additional AC joint cerclage without increase in approach-related morbidity to address the high risk of persistent dynamic posterior translation (DPT). Only with this addition, native biomechanical stability could be restored (32). Comparative clinical studies will have to be performed in the future to obtain data demonstrating the advantages of these technical advancements.
Results
Clinical outcome data from studies evaluating Rockwood type I and type II injuries have not been sufficiently reported in the literature. It is assumed that conservative treatment of these injuries typically results in full recovery without any residual deficits.
However, data from retrospective studies on Rockwood type I and type II injuries showed potential long-term complications after 20 months (33), 6.3 years (34) and 10.2 years (35), respectively. Mouhsine et al. (34) found that 42% of patients with Rockwood type II injuries had to change their job and sporting activities and 27% of patients underwent surgery because of persistent complaints. Mikek et al. (35) showed in 52% of study participants persistent AC joint-specific symptoms and functional impairments after 10.2 years. By contrast, Shaw et al. (33) reported a decrease in symptoms by 40% after 6 months and of 14% after 12 months.
However, two low-evidence-level studies (LoE IV) found significant shoulder pain and limitation of mobility within the first 6 months after the trauma (36) and secondary surgical treatment in up to 27% of patients (37).
The management of Rockwood type III injuries has been the subject of controversy for many years. Due to the lack of evidence in support of a clear advantage of surgical treatment in the literature, most studies recommend conservative management of Rockwood type III injuries (38, 39). Prospective randomized trials comparing advanced surgical techniques with conservative treatment should be performed in the future to improve the evidence base on this subject too.
Today, the majority of high-grade AC joint dislocations (Rockwood type IV to type VI) are treated surgically. Consequently, reports of experiences with conservative treatment are rare. In a multicenter trial, McKee et al. found that conservative treatment of high-grade AC joint instabilities may not necessarily be associated with poorer clinical outcomes compared to temporary hook plate retention (McKee et al. 2012) (40). They were not able to demonstrate the superiority of temporary hook plate retention over non-surgical treatment in high-grade AC joint separations. Unfortunately, the study also included Rockwood type III to type V injuries, a fact that decreases its value. So far, no prospective randomized trial comparing arthroscopically assisted advanced stabilization with conservative treatment has been published.
Mainly good and very good clinical outcomes after acute surgical stabilization of the AC joint have been reported in the literature, regardless of the technique used (19, e1– e3). Likewise independent of the technique used, however, radiographic reduction losses were reported in 10% to 50% of cases for temporary hook plate retention and CC suture cerclages or minimally invasive pulley techniques. Yet, these radiographic finding show no correlation with clinical outcomes so that they do not represent an indication for surgical revision (34– 37).
To date, comparisons of the two techniques have been limited to retrospective studies and meta-analyses (21, 31). No significant difference was found for the functional outcome, but a trend towards better outcomes for arthroscopic/minimally invasive techniques has been reported. Subjective patient satisfaction and cosmetic results were significantly better after arthroscopic surgery (31). First prospective randomized trials (LoE I) have recently demonstrated a significant advantage for arthroscopic techniques. Stein et al. followed up 29 patients after arthroscopically assisted stabilization (two pulley systems) and 27 patients after hook plate fixation over a period of at least 24 months. After 24 months, they found significant advantages for patients treated with minimally invasive surgery in all clinical scores (e4). In another randomized controlled trial, Müller et al. assessed 29 patients after hook plate fixation and 32 patients after arthroscopically assisted stabilization (two pulley systems) with regard to their ability to engage in sporting activities and compared these with a control group (n = 140). After 24 months, here again a clear advantage for the group treated with minimally invasive surgery was found with regard to sporting ability and return to previous sporting levels (e5).
The use of an additional AC cerclage appears to result in reduced dynamic posterior translation (e6). We will have to wait for long-term results from prospective randomized comparative studies to verify the clinical usefulness of additional AC cerclage.
Conclusion
In German-speaking countries, there is general agreement in the current discussion of treatment options that high-grade instabilities require acute stabilization to prevent late complications and challenging stabilization surgery in case of chronic instability. In patients with chronic injuries (more than 3 weeks after the trauma), a tendon should be used as a biological augmentation.
Prospective randomized trials and basic research are urgently needed to determine the optimum timing for surgical intervention and to establish when after the trauma augmentation using a graft is actually required. For the time being, an acute injury should be surgically treated as soon as possible.
The only prospective randomized trials comparing hook plate fixation with the arthroscopically assisted techniques have shown advantages of arthroscopy use (e4, e5).
In addition, the arthroscopically assisted techniques enable targeted treatment of horizontal instability and direct assessment and treatment of intraarticular concomitant injuries without the need to remove implanted material.
Figure 2.
Bilateral weight-bearing radiographs: “Water bearer radiographs“ to assess the vertical stability of the acromioclavicular joint
Key Messages.
Acute dislocation of the acromioclavicular joint is a common injury in athletes and characterized by painful impairment of shoulder function and elevation (“pseudo-elevation“) of the lateral clavicle.
Persistent AC joint instabilities can result in persistent pain and functional impairment of the shoulder girdle.
Accurate classification and correct choice of treatment requires radiographic assessment with vertical and horizontal weight-bearing radiographs.
Rockwood type I to type II injuries can be treated conservatively. Rockwood type III to type VI injuries should be referred to a specialized orthopedic surgeon to review the indication for surgical treatment.
First prospective randomized data indicate superiority of arthroscopically assisted techniques over hook plate fixation.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest
PD Dr. Martetschläger has an advisor and lecturer contract with Arthrex.
Prof. Scheibel receives license fees from Arthrex. He has an advisor and lecturer contract with Arthrex.
The remaining authors declare no conflict of interest.
References
- 1.Nordqvist A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an urban population. J Shoulder Elbow Surg. 1995;4:107–112. doi: 10.1016/s1058-2746(05)80063-1. [DOI] [PubMed] [Google Scholar]
- 2.Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49:774–784. [PubMed] [Google Scholar]
- 3.Kraus N, Scheibel M. [Injuries of the acromioclavicular joint in athletes] Chirurg. 2014;85:854–863. doi: 10.1007/s00104-014-2770-6. [DOI] [PubMed] [Google Scholar]
- 4.Kocher MS, Feagin JA Jr. Shoulder injuries during alpine skiing. Am J Sports Med. 1996;24:665–669. doi: 10.1177/036354659602400517. [DOI] [PubMed] [Google Scholar]
- 5.Feucht MJ, Braun S. Imhoff A, Feucht MJ, editors. AC-Gelenk-Stabilisierung (akut) Atlas sportorthopädisch-sporttraumatologische Operationen. Berlin Heidelberg: Springer. 2013:17–21. [Google Scholar]
- 6.Beitzel K, Mazzocca AD, Bak K, et al. ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy. 2014;30:271–278. doi: 10.1016/j.arthro.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Williams GR, Nguyen VD, A. RC. Classification and radiographic analysis of acromioclavicular dislocations. Appl Radiol. 1989;18:29–34. [Google Scholar]
- 8.Tauber M. Bildgebung in der Schulter- und Ellenbogenchirurgie: Schultereckgelenksprengung - akut und chronisch. Obere Extremität. 2017;12(Suppl.1):34–35. [Google Scholar]
- 9.Ibrahim EF, Forrest NP, Forester A. Bilateral weighted radiographs are required for accurate classification of acromioclavicular separation: an observational study of 59 cases. Injury. 2015;46:1900–1905. doi: 10.1016/j.injury.2015.06.028. [DOI] [PubMed] [Google Scholar]
- 10.Melenevsky Y, Yablon CM, Ramappa A, Hochman MG. Clavicle and acromioclavicular joint injuries: a review of imaging, treatment, and complications. Skeletal Radiol. 2011;40:831–842. doi: 10.1007/s00256-010-0968-3. [DOI] [PubMed] [Google Scholar]
- 11.Maier D, Jaeger M, Reising K, Feucht MJ, Sudkamp NP, Izadpanah K. Injury patterns of the acromioclavicular ligament complex in acute acromioclavicular joint dislocations: a cross-sectional, fundamental study. BMC Musculoskelet Disord. 2016;17 doi: 10.1186/s12891-016-1240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tischer T, Salzmann GM, El-Azab H, Vogt S, Imhoff AB. Incidence of associated injuries with acute acromioclavicular joint dislocations types III through V. Am J Sports Med. 2009;37:136–139. doi: 10.1177/0363546508322891. [DOI] [PubMed] [Google Scholar]
- 13.Beitzel K, Cote MP, Apostolakos J, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013;29:387–397. doi: 10.1016/j.arthro.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Rockwood CA. Rockwood CA, Green DP, editors. Injuries to the acromioclavicular joint . Fractures in Adults. Philadelphia: JB Lippincott Co. 1984 [Google Scholar]
- 15.Ringenberg JD, Foughty Z, Hall AD, Aldridge JM 3rd, Wilson JB, Kuremsky MA. Interobserver and intraobserver reliability of radiographic classification of acromioclavicular joint dislocations. J Shoulder Elbow Surg. 2018;27:538–544. doi: 10.1016/j.jse.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 16.Tauber M. Management of acute acromioclavicular joint dislocations: current concepts. Arch Orthop Trauma Surg. 2013;133:985–995. doi: 10.1007/s00402-013-1748-z. [DOI] [PubMed] [Google Scholar]
- 17.Reid D, Polson K, Johnson L. Acromioclavicular joint separations grades I-III: a review of the literature and development of best practice guidelines. Sports Med. 2012;42:681–696. doi: 10.2165/11633460-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 18.Longo UG, Ciuffreda M, Rizzello G, Mannering N, Maffulli N, Denaro V. Surgical versus conservative management of Type III acromioclavicular dislocation: a systematic review. Br Med Bull. 2017;122:31–49. doi: 10.1093/bmb/ldx003. [DOI] [PubMed] [Google Scholar]
- 19.Scheibel M, Droschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39:1507–1516. doi: 10.1177/0363546511399379. [DOI] [PubMed] [Google Scholar]
- 20.Balke M, Schneider MM, Shafizadeh S, Bathis H, Bouillon B, Banerjee M. Current state of treatment of acute acromioclavicular joint injuries in Germany: is there a difference between specialists and non-specialists? A survey of German trauma and orthopaedic departments. Knee Surg Sports Traumatol Arthrosc. 2015;23:1447–1452. doi: 10.1007/s00167-013-2795-2. [DOI] [PubMed] [Google Scholar]
- 21.Helfen T, Siebenburger G, Ockert B, Haasters F. [Therapy of acute acromioclavicular joint instability. Meta-analysis of arthroscopic/minimally invasive versus open procedures]. Unfallchirurg. 2015;118:415–426. doi: 10.1007/s00113-015-0005-z. [DOI] [PubMed] [Google Scholar]
- 22.Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42:235–241. doi: 10.1177/0363546513490656. [DOI] [PubMed] [Google Scholar]
- 23.Song T, Yan X, Ye T. Comparison of the outcome of early and delayed surgical treatment of complete acromioclavicular joint dislocation. Knee Surg Sports Traumatol Arthrosc. 2016;24:1943–1950. doi: 10.1007/s00167-014-3225-9. [DOI] [PubMed] [Google Scholar]
- 24.Barth J, Duparc F, Andrieu K, et al. Is coracoclavicular stabilisation alone sufficient for the endoscopic treatment of severe acromioclavicular joint dislocation (Rockwood types III, IV, and V)? Orthop Traumatol Surg Res. 2015;101:297–303. doi: 10.1016/j.otsr.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Carbone S, Postacchini R, Gumina S. Scapular dyskinesis and SICK syndrome in patients with a chronic type III acromioclavicular dislocation Results of rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2015;23:1473–1480. doi: 10.1007/s00167-014-2844-5. [DOI] [PubMed] [Google Scholar]
- 26.Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11:142–151. doi: 10.5435/00124635-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661. doi: 10.1016/s0749-8063(03)00389-x. [DOI] [PubMed] [Google Scholar]
- 28.Walz L, Salzmann GM, Fabbro T, Eichhorn S, Imhoff AB. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J Sports Med. 2008;36:2398–2406. doi: 10.1177/0363546508322524. [DOI] [PubMed] [Google Scholar]
- 29.Martetschlager F, Saier T, Weigert A, et al. Effect of coracoid drilling for acromioclavicular joint reconstruction techniques on coracoid fracture risk: a biomechanical study. Arthroscopy. 2016;32:982–987. doi: 10.1016/j.arthro.2015.11.049. [DOI] [PubMed] [Google Scholar]
- 30.Spiegl UJ, Smith SD, Euler SA, Dornan GJ, Millett PJ, Wijdicks CA. Biomechanical consequences of coracoclavicular reconstruction techniques on clavicle strength. Am J Sports Med. 2014;42:1724–1730. doi: 10.1177/0363546514524159. [DOI] [PubMed] [Google Scholar]
- 31.Jensen G, Katthagen JC, Alvarado LE, Lill H, Voigt C. Has the arthroscopically assisted reduction of acute AC joint separations with the double tight-rope technique advantages over the clavicular hook plate fixation? Knee Surg Sports Traumatol Arthrosc. 2014;22:422–430. doi: 10.1007/s00167-012-2270-5. [DOI] [PubMed] [Google Scholar]
- 32.Saier T, Venjakob AJ, Minzlaff P, et al. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2015;23:1498–1505. doi: 10.1007/s00167-014-2895-7. [DOI] [PubMed] [Google Scholar]
- 33.Shaw MB, McInerney JJ, Dias JJ, Evans PA. Acromioclavicular joint sprains: the post-injury recovery interval. Injury. 2003;34:438–442. doi: 10.1016/s0020-1383(02)00187-0. [DOI] [PubMed] [Google Scholar]
- 34.Mouhsine E, Garofalo R, Crevoisier X, Farron A. Grade I and II acromioclavicular dislocations: results of conservative treatment. J Shoulder Elbow Surg. 2003;12:599–602. doi: 10.1016/s1058-2746(03)00215-5. [DOI] [PubMed] [Google Scholar]
- 35.Mikek M. Long-term shoulder function after type I and II acromioclavicular joint disruption. Am J Sports Med. 2008;36:2147–2150. doi: 10.1177/0363546508319047. [DOI] [PubMed] [Google Scholar]
- 36.Shaw MBK, McInerney JJ, Dias JJ, Evans PA. Acromioclavicular joint sprains: the post-injury recovery interval. Injury. 2003;34:438–442. doi: 10.1016/s0020-1383(02)00187-0. [DOI] [PubMed] [Google Scholar]
- 37.Mikek M. Long-term shoulder function after type I and II acromioclavicular joint disruption. Am J Sports Med. 2008;36:2147–2150. doi: 10.1177/0363546508319047. [DOI] [PubMed] [Google Scholar]
- 38.Korsten K, Gunning AC, Leenen LP. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. Int Orthop. 2014;38:831–838. doi: 10.1007/s00264-013-2143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Phillips AM, Smart C, Groom AF. Acromioclavicular dislocation. Conservative or surgical therapy. Clin Orthop Relat Res. 1998:10–17. [PubMed] [Google Scholar]
- 40.Canadian Orthopaedic Trauma S. Multicenter randomized clinical trial of nonoperative versus operative treatment of acute acromio-clavicular joint dislocation. J Orthop Trauma. 2015;29:479–487. doi: 10.1097/BOT.0000000000000437. [DOI] [PubMed] [Google Scholar]
- E1.Salzmann GM, Walz L, Buchmann S, Glabgly P, Venjakob A, Imhoff AB. Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med. 2010;38:1179–1187. doi: 10.1177/0363546509355645. [DOI] [PubMed] [Google Scholar]
- E2.Greiner S, Braunsdorf J, Perka C, Herrmann S, Scheffler S. Mid to long-term results of open acromioclavicular-joint reconstruction using polydioxansulfate cerclage augmentation. Arch Orthop Trauma Surg. 2009;129:735–740. doi: 10.1007/s00402-008-0688-5. [DOI] [PubMed] [Google Scholar]
- E3.Di Francesco A, Zoccali C, Colafarina O, Pizzoferrato R, Flamini S. The use of hook plate in type III and V acromio-clavicular Rockwood dislocations: clinical and radiological midterm results and MRI evaluation in 42 patients. Injury. 2012;43:147–152. doi: 10.1016/j.injury.2011.04.002. [DOI] [PubMed] [Google Scholar]
- E4.Stein T, Muller D, Blank M, et al. Stabilization of acute high-grade acromioclavicular joint separation: a prospective assessment of the clavicular hook plate versus the double double-button suture procedure. Am J Sports Med. 2018;46:2725–2734. doi: 10.1177/0363546518788355. [DOI] [PubMed] [Google Scholar]
- E5.Muller D, Reinig Y, Hoffmann R, et al. Return to sport after acute acromioclavicular stabilization: a randomized control of double-suture-button system versus clavicular hook plate compared to uninjured shoulder sport athletes. Knee Surg Sports Traumatol Arthrosc. 2018;26:3832–3847. doi: 10.1007/s00167-018-5044-x. [DOI] [PubMed] [Google Scholar]
- E6.Hann C, Kraus N, Minkus M, Maziak N, Scheibel M. Combined arthroscopically assisted coraco- and acromioclavicular stabilization of acute high-grade acromioclavicular joint separations. Knee Surg Sports Traumatol Arthrosc. 2018;26:212–220. doi: 10.1007/s00167-017-4643-2. [DOI] [PubMed] [Google Scholar]
- E7.Warth RJ, Martetschlager F, Gaskill TR, Millett PJ. Acromioclavicular joint separations. Curr Rev Musculoskelet Med. 2013;6:71–78. doi: 10.1007/s12178-012-9144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]