Abstract
Continuous renal replacement therapy (CRRT) is commonly used to provide renal support for critically ill patients with acute kidney injury, particularly patients who are hemodynamically unstable. A variety of techniques that differ in their mode of solute clearance may be used, including continuous venovenous hemofiltration with predominantly convective solute clearance, continuous venovenous hemodialysis with predominantly diffusive solute clearance, and continuous venovenous hemodiafiltration, which combines both dialysis and hemofiltration. The present article compares CRRT with other modalities of renal support and reviews indications for initiation of renal replacement therapy, as well as dosing and technical aspects in the management of CRRT.
Key Words: acute kidney injury, continuous renal replacement therapy, dialysis, hemodialysis, hemofiltration
Abbreviations: AKI, acute kidney injury; CRRT, continuous renal replacement therapy; CVVH, continuous venovenous hemofiltration; CVVHD, continuous venovenous hemodialysis; CVVHDF, continuous venovenous hemodiafiltration; IHD, intermittent hemodialysis; PIRRT, prolonged intermittent renal replacement therapy; RRT, renal replacement therapy; UFH, unfractionated heparin
Acute kidney injury (AKI) is a common complication in critically ill patients and is associated with substantial morbidity and risk of death. Approximately 5% to 10% of patients with AKI require renal replacement therapy (RRT) during their ICU stay,1 with mortality rates of 30% to 70%.2, 3, 4 Over the past 2 decades, the incidence of RRT-requiring AKI has increased by approximately 10% per year.5 Risk factors for RRT-requiring AKI include older age, male sex, African-American race, higher severity of illness, sepsis, decompensated heart failure, cardiac surgery, liver failure, and use of mechanical ventilation. While once considered an extraordinary measure, the ability to provide RRT, even in the setting of marked hemodynamic instability, has become routine. However, substantial uncertainty remains regarding many of the fundamental aspects of RRT management, including the optimal timing of initiation and discontinuation, as well as the selection of modality.6 The present article provides an overview of key issues in the management of RRT in the critically ill patient, focused primarily on the use of continuous renal replacement therapy (CRRT).
Modalities of RRT
Multiple modalities of renal support may be used in the management of the critically ill patient with kidney failure. These include CRRT, conventional intermittent hemodialysis (IHD), and the prolonged intermittent renal replacement therapies (PIRRTs), which are a hybrid of CRRT and IHD. All of these use relatively similar extracorporeal blood circuits and differ primarily with regard to duration of therapy and, consequently, the rapidity of net ultrafiltration and solute clearance. In addition, dialytic therapies rely predominantly on diffusive solute clearance, whereas solute removal during hemofiltration occurs by convection.
IHD provides rapid solute clearance and ultrafiltration during relatively brief (3- to 5-h) treatments; the continuous therapies provide more gradual fluid removal and solute clearance over prolonged treatment times (optimally, 24 h per day but often interrupted due to system clotting or diagnostic or therapeutic procedures).1 The multiple forms of PIRRT are characterized by treatments that are generally between 8 and 16 h in duration, with slower rates of solute clearance and ultrafiltration than IHD but more rapid than CRRT. PIRRT is most commonly provided by using equipment similar to that for IHD but with lower blood and dialysate flow rates. It can also be performed by using equipment designed for CRRT but with augmented dialysate and/or ultrafiltration rates to achieve similar delivered therapy over a shorter duration.7 Peritoneal dialysis provides an effective alternative to the extracorporeal modalities of RRT,8 but a detailed discussion of this method is beyond the scope of this review.
Selection of RRT Modality
Although CRRT and PIRRT are most commonly used in hemodynamically unstable patients, there is marked variation in practice. Some centers use CRRT (or PIRRT) in all ICU patients with renal failure regardless of hemodynamic status, whereas others use IHD, albeit with adjustments in prescription, even in vasopressor-dependent patients. Although the benefit of a slow, continuous modality of renal support in hemodynamically unstable patients may seem self-evident, randomized trials have failed to show differences with regard to either mortality or recovery of kidney function comparing CRRT with either IHD9, 10, 11, 12, 13, 14, 15, 16, 17 or PIRRT.18, 19, 20 It must be recognized, however, that to provide IHD in hemodynamically unstable patients, the standard prescription may require modification, such as prolongation of treatment time to allow for more gradual ultrafiltration, use of higher dialysate sodium concentrations, and reduced dialysate temperatures.12 Although the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guideline for AKI recommends the use of CRRT for patients who are hemodynamically unstable,21 the strength of this recommendation is low. Observational data, however, do suggest that CRRT is more effective in achieving net negative fluid balance than IHD.22 In addition, in patients with fulminant hepatic failure or brain injury with increased intracranial pressure, CRRT is associated with better maintenance of cerebral perfusion than IHD.23, 24, 25, 26
Selection of CRRT Modality
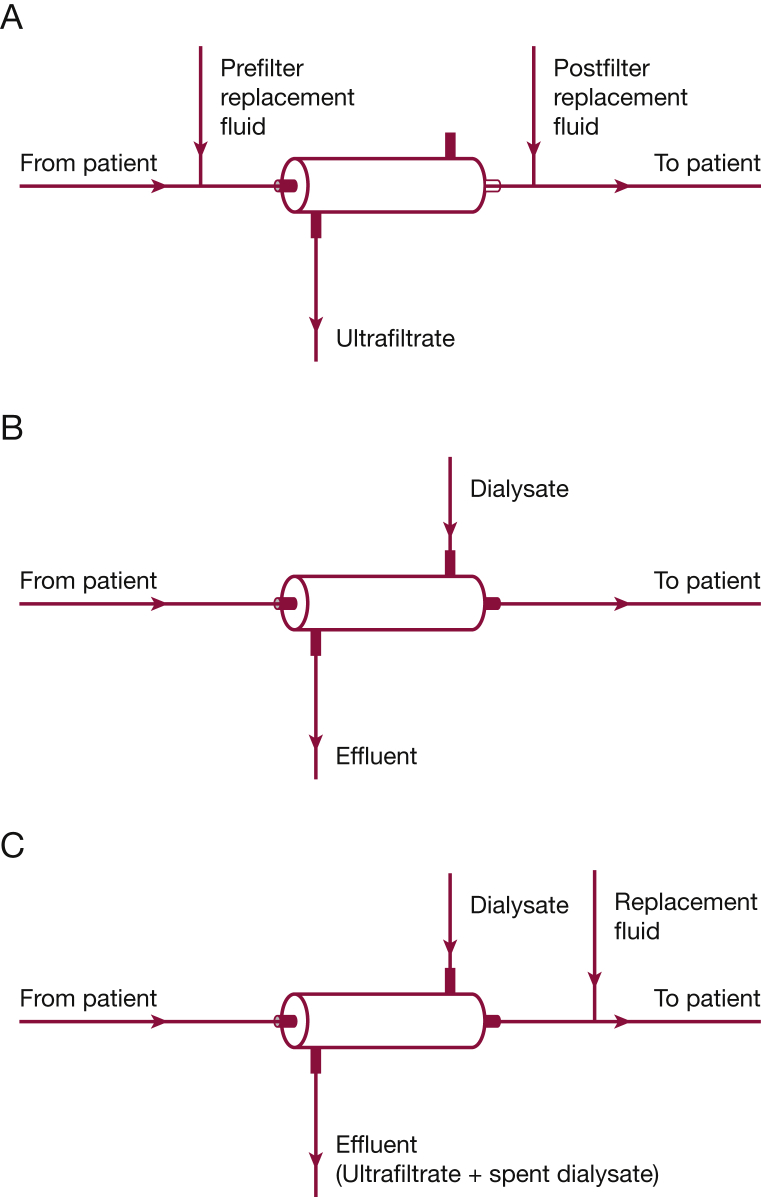
While initially developed as an arteriovenous therapy, most CRRT is now performed using pump-driven venovenous extracorporeal circuits. Although this introduces additional degrees of complexity, including pressure monitors and air detectors, the pump-driven venovenous circuit provides higher and more consistent blood flows and eliminates the hazards associated with prolonged arterial cannulation with a large-bore catheter. Multiple techniques for delivering CRRT have been developed. When used solely for volume management, the treatment is known as slow continuous ultrafiltration. More commonly, when provided as continuous venovenous hemofiltration (CVVH), continuous venovenous hemodialysis (CVVHD), or continuous venovenous hemodiafiltration (CVVHDF), CRRT provides both solute clearance and volume removal, with the differences between these modalities related to the mechanisms for solute clearance (Fig 1).
Figure 1.
A-C, Schematic diagrams of modalities of continuous renal replacement therapy. A, Continuous hemofiltration. Blood flow through the hemofilter is shown from left to right. An ultrafiltrate is generated across the hemofilter membrane, and excess ultrafiltrate above the volume desired for negative fluid balance is replaced with prefilter and/or postfilter replacement solution. B, Continuous hemodialysis. Blood flow through the hemodialyzer is shown from left to right. Dialysate is perfused through the hemodialyzer on the opposite side of the membrane from the blood countercurrent to the direction of blood flow. The effluent consists of spent dialysate plus the volume of ultrafiltrate desired to achieve negative fluid balance. C, Continuous hemodiafiltration. Blood through the hemodiafilter is shown from left to right. As in continuous hemodialysis, dialysate is perfused through the hemodialyzer on the opposite side of the membrane from the blood countercurrent to the direction of blood flow. The effluent consists of spent dialysate plus ultrafiltrate. As in continuous hemofiltration, excess ultrafiltrate above the volume desired for negative fluid balance is replaced with replacement solution. In the figure, replacement solution is shown being infused postfilter; replacement solution can also be infused prefilter.
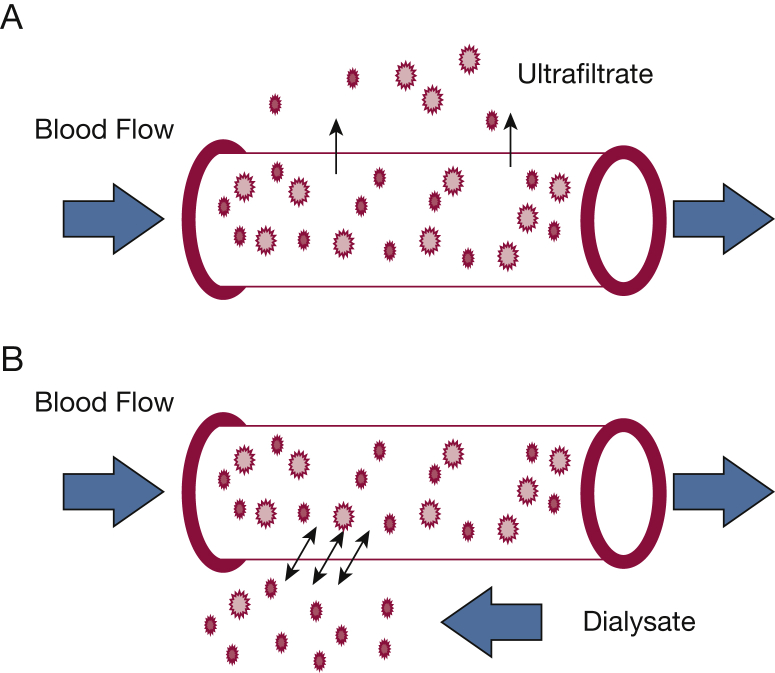
In CVVH, a high rate of ultrafiltration across the semi-permeable hemofilter membrane is created by a hydrostatic gradient, and solute transport occurs by convection (Fig 2A). Solutes are entrained in the bulk flow of water across the membrane, a process often referred to as “solvent drag.”1, 27 High ultrafiltration rates are needed to achieve sufficient solute clearance, and the ultrafiltrate volume beyond what is required to achieve desired net fluid removal is replaced with balanced IV crystalloid solutions. These replacement solutions may be infused into the extracorporeal circuit either prior to or following the hemofilter. Because the high ultrafiltration rate hemoconcentrates the blood as it passes through the hemofilter fibers, the risk of sludging and fiber occlusion is increased. Prefilter infusion of replacement fluid dilutes the blood entering the hemofilter, mitigating this hemoconcentration. However, prefilter administration of replacement fluid dilutes the solute content of the blood, reducing effective solute clearance at a fixed ultrafiltration rate. Postfilter infusion has no such effects.
Figure 2.
Convection and diffusion. A, Convection: solute transfer across the membrane occurs via entrainment of solutes in the bulk flow of water during ultrafiltration. Higher molecular weight solutes (larger symbols) and lower molecular weight (< 500-1,500 Daltons) solutes (smaller symbols) are transported across the membrane with equal efficiency until the molecular radius of the solute exceeds the membrane pore size. B, Diffusion: solute transfer across the membrane occurs by movement down a concentration gradient from blood to dialysate. Lower molecular weight (< 500-1,500 Daltons) solutes (smaller symbols) cross the membrane more readily than higher molecular weight solutes (larger symbols).
In CVVHD, dialysate is perfused across the external surface of the dialysis membrane, and solutes exit from blood to dialysate by diffusion down their concentration gradient (Fig 2B). Ultrafiltration rates are relatively low compared with those in CVVH, permitting net negative fluid balance without the need for IV replacement fluids. Although commonly considered as a purely diffusive therapy, unmeasured bidirectional filtration into the dialysate compartment and back-filtration from dialysate to blood (driven by variation in the hemodynamic pressure gradient over the length of the hemodialysis fibers) result in significant convective solute transport. CVVHDF is a hybrid, combining the dialysate flow of CVVHD with the high ultrafiltration rates and use of replacement fluids of CVVH.
The various mechanisms of solute clearance provided by CVVH and CVVHD result in different profiles of solute removal with each modality. Diffusion provides efficient clearance of low-molecular-weight solutes (< 500-1,500 Daltons); however, diffusive clearance declines rapidly as solute molecular weight increases. In contrast, solute movement in convection is limited primarily by the size of the pores in the hemofilter membrane. Clearances of lower and higher molecular weight solutes are similar, until the solute molecular radius approaches the size of the membrane pores.27 Thus, at equivalent effluent flow rates, CVVH provides higher clearances than CVVHD for solutes in the range of 1,000 to 20,000 Daltons, or even higher if high cutoff membranes with larger pores are used. Although it has been suggested that the augmented clearance of higher molecular weight solutes (eg, pro-inflammatory cytokines) provided by CVVH might be beneficial, this has not been borne out in clinical practice.17, 28, 29 Independent of diffusion and convection, adsorption of solutes in the CRRT circuit, subject to saturation of membrane binding sites, may also contribute to overall solute clearance.6 Thus, choice of CRRT modality (CVVH, CVVHD, or CVVHDF) is primarily a function of provider preference rather than patient characteristics or objective outcome data.
Indications for Initiation of RRT
The indications for initiation of CRRT generally correspond to overall indications for RRT (Table 1), including volume overload, severe metabolic acidosis and electrolyte disturbances, and overt uremic symptoms. Although these indications are well ensconced, they are subject to wide interpretation and should be considered as only semi-objective. In addition, in many patients, RRT is initiated in the setting of persistent or progressive AKI in the absence of these criteria.
Table 1.
Indications for Initiation of Continuous Renal Replacement Therapy
| Volume overload |
| Metabolic acidosis |
| Electrolyte abnormalities |
| Hyperkalemia |
| Hyponatremia |
| Hyperphosphatemia |
| Uremia |
| Encephalopathy |
| Pericarditis |
| Persistent/progressive acute kidney injury |
Volume Overload
Volume overload in AKI occurs due to the disruption of the kidney’s ability to maintain fluid balance in the face of administration of IV fluids, blood products, and/or other medications required for resuscitation and supportive treatment of a critically ill patient and may develop even in patients who are not oliguric or anuric.1 There are no prospective data establishing specific thresholds for RRT initiation. RRT is generally indicated when volume overload compromises organ function and is refractory to diuretic agents. Although observational data in both pediatric and adult populations show a strong association between severity of volume overload at initiation of RRT and mortality risk, causality has not been established.22, 30, 31 A complex interplay exists between underlying severity of illness, development of volume overload and mortality, and there is an absence of prospective data showing that initiation of extracorporeal ultrafiltration at a specific threshold of volume overload reduces mortality.
Acid-Base Abnormalities
Progressive metabolic acidosis is an inevitable consequence of kidney failure, developing due to impaired renal acid excretion.32 In patients in whom severe acidosis is refractory to medical management, such as the volume overloaded patient who cannot tolerate alkali administration, either intermittent or continuous RRT is effective.32, 33, 34 Commonly suggested thresholds for initiation of RRT include a pH < 7.1 to 7.2 or serum bicarbonate level < 12 to 15 mmol/L. Earlier initiation of RRT may be necessary in patients with acute lung injury receiving lung-protective ventilation, as severe acidemia can result from the combination of metabolic and respiratory acidosis. Although RRT augments lactate clearance, there is scant evidence that initiation of RRT to augment lactate clearance alters clinical outcomes in patients with lactic acidosis not associated with drug toxicity (eg, metformin).
Severe Electrolyte Abnormalities
Multiple electrolyte abnormalities are associated with AKI. Severe hyperkalemia is the most life-threatening and requires prompt treatment to prevent cardiotoxicity and arrhythmias. Initiation of RRT is indicated when hyperkalemia is refractory to medical therapy or recurs following the initial treatment. Although rigid thresholds based on level of serum potassium cannot be provided, RRT solely for the management of hyperkalemia is rarely appropriate when the potassium level is < 6 mmol/L. Conversely, RRT is generally appropriate in patients in whom the potassium level remains > 6.5 mmol/L despite medical management. Although IHD provides more rapid correction of hyperkalemia and is the preferred modality in this setting, CRRT provides effective, albeit slower, control of the plasma potassium concentration.35 Other electrolyte abnormalities, such as severe hyponatremia or hypernatremia and severe hyperphosphatemia, may accompany AKI and should be a factor in the decision to initiate RRT. In patients with severe hyponatremia in the setting of AKI, CRRT may permit the slower and more controlled correction of sodium concentration needed to prevent the neurologic sequelae of osmotic demyelination, compared with IHD.32
Uremia and Progressive or Persistent Azotemia
The use of RRT for the management of overt uremic symptoms, such as encephalopathy and pericarditis, is well established. Although these are relatively late complications of AKI, other manifestations of uremia, such as platelet dysfunction, impaired nutrition, increased susceptibility to infection and sepsis, heart failure, and pulmonary edema, may be difficult to distinguish from other etiologies in the critically ill patient with multiple organ dysfunction.36 It is far more common, when specific indications are not present for RRT, to be initiated prophylactically in response to persistent or progressive azotemia prior to the development of overt uremic manifestations. The appropriate timing for such initiation remains a topic of debate and is discussed below.
Drug and Toxin Removal
A variety of toxins and drugs, such as toxic alcohols, lithium, salicylate, valproic acid, and metformin, are dialyzable, and the timely use of RRT in cases of poisoning and drug intoxications with these agents may be able to avert serious complications. The ability of RRT to remove a particular drug or toxin from the circulation is a function of its size, volume of distribution, and protein binding. Thus, RRT is effective for the removal of smaller, nonprotein-bound molecules with a volume of distribution < 1 L/kg body weight.37 However, because the goal in the treatment of intoxications and overdoses is the rapid clearance of the offending agent, IHD is generally preferred over CRRT in this setting, even in patients who are hemodynamically unstable.38, 39
The role of RRT in the management of hyperammonemia is uncertain. Based on molecular weight, ammonia is readily cleared by both diffusion and convection. As with the treatment of poisoning and intoxication, IHD will provide more rapid reduction in blood ammonia levels. However, in small case series, high-dose CRRT has been shown to be efficacious for the acute management of severe hyperammonemia (> 400 μmol/L) in infants with inborn errors of metabolism.40, 41 The role of CRRT in adults with hyperammonemia complicating liver failure is less certain. CRRT is associated with reductions in plasma ammonia levels.42, 43 In a retrospective analysis of registry data, CRRT was associated with improved 21-day transplant-free survival among patients with acute liver failure compared with IHD or no RRT.43 However, these data are not sufficient to establish causality, and there are no prospective studies that have specifically evaluated the use of CRRT for the management of hyperammonemia in liver disease.
Timing of Initiation of RRT
In the absence of specific indications, the optimal timing for initiation of RRT in AKI is uncertain. Earlier initiation of AKI allows for optimization of volume status, early correction of acid-base and electrolyte disturbances, and control of azotemia prior to the development of the major metabolic disturbances that serve as objective indications. However, these potential benefits of early initiation need to be balanced with the risks and burdens associated with RRT, including vascular access (eg, hemorrhage, thrombosis, vascular injury, infection), intradialytic hypotension, and resource utilization as well as with the potential concern that RRT may impair subsequent recovery of kidney function.44 Furthermore, it is often uncertain whether an individual patient will have persistent AKI or rapid recovery of kidney function, and currently there are no tools to reliably predict the clinical trajectory for the individual patient with AKI.
Multiple observational studies have suggested improved survival associated with earlier initiation of RRT.2, 45, 46, 47, 48, 49, 50, 51, 52 However, these studies only included patients who ultimately received RRT and did not account for patients with AKI who did not undergo early RRT and who either recovered kidney function or died without receiving RRT. Excluding these patients from analysis results in potential bias as the actual clinical question is not one of early vs late initiation of RRT but rather early vs non-early RRT in patients in whom there is no urgent indication.
Several randomized controlled trials have helped to inform our understanding of this question, although there has been discordance in the results of these trials. The Effect of Early vs Delayed Initiation of Renal Replacement Therapy on Mortality in Critically Ill Patients With Acute Kidney Injury (ELAIN) trial was a single-center, unblinded randomized controlled trial of 231 critically ill patients at a university hospital in Germany with stage 2 AKI (doubling of serum creatinine level or urine output < 0.5 mL/kg per hour for 12 h).53 Patients were randomized to receive either immediate initiation of RRT or to a strategy in which RRT was delayed until an absolute indication was present or AKI had progressed to stage 3 (tripling of serum creatinine level, urine output < 0.3 mL/kg per hour for 24 h, or anuria for 12 h). All 112 patients in the early arm and 108 of 119 patients (91%) in the delayed arm received CVVHDF, with a median time from stage 2 AKI to initiation of RRT of 6 h in the early arm compared with 25.5 h in the delayed arm (median difference, 21 h). Ninety-day all-cause mortality was 39.3% in the early arm compared with 54.7% in the delayed arm (P = .03).
In contrast, the Artificial Kidney Initiation in Kidney Injury (AKIKI) trial was a multicenter, randomized controlled trial across 31 ICUs in France.54 In this trial, 619 patients with stage 3 AKI who did not have emergent indications were randomized to undergo immediate initiation of RRT or a strategy of delayed initiation based on clinical indications. Of the 308 patients randomized to undergo the delayed strategy, only 157 (51%) ultimately received RRT. For those patients receiving RRT, the median time from reaching stage 3 AKI to randomization was 4.3 h in the early arm compared with 57 h in the delayed arm. Sixty-day mortality did not differ between the two treatment arms (48.5% vs 49.7%; P = .79). No differences in the overall outcome were observed in subgroup analyses of 348 patients with septic shock and 207 patients with ARDS.55
The results of the more recently completed Initiation of Dialysis Early Versus Delayed in the Intensive Care Unit (IDEAL-ICU) trial are similar to those of the AKIKI trial.56 The IDEAL-ICU trial enrolled 488 patients with sepsis and AKI in 29 ICUs in France. Patients who did not have an emergent indication for RRT were randomized to either begin RRT within 12 h of meeting RIFLE-F criteria (corresponding to stage 3 AKI) or to have RRT delayed until either an emergent indication for RRT developed or for 48 h. Of the 246 patients randomized to early RRT 239 (97%) initiated RRT a median of 7.6 h after meeting RIFLE-F criteria while 149 of the 242 (62%) patients randomized to the delayed arm initiated RRT after a median of 51.5 h. Ninety-day mortality was 58% in the early-initiation arm as compared to 54% in the delayed-initiation arm (P = .38).
Important differences between the ELAIN and AKIKI and IDEAL-ICU trials should be noted. The key entry criterion for both the AKIKI and IDEAL-ICU trials (stage 3 AKI) was the criterion for late initiation of RRT in the ELAIN trial. In addition, in both the AKIKI and IDEAL-ICU trials, all modalities of RRT could be used, whereas in ELAIN, only CVVHDF was used. Critically, both the AKIKI and IDEAL-ICU trials excluded patients with emergent criteria for initiation of RRT, such as severe hyperkalemia or pulmonary edema, whereas the majority of patients in the ELAIN trial had fluid overload or pulmonary edema prior to enrollment. Although future clinical trials are needed to address the significant equipoise regarding the optimal timing of RRT, we believe that in clinical practice, in the absence of emergent indications such as intractable hyperkalemia or severe volume overload, an approach of delayed RRT initiation is not unreasonable.57
Dose of CRRT
Solute Control
The dose of CRRT is assessed based on the effluent flow rate, the sum of dialysate and total ultrafiltrate flow.58, 59 During CVVH, the concentration of low-molecular-weight solutes such as urea in the ultrafiltrate is close to that in plasma water. Similarly, during CVVHD, because the dialysate flow rate is commonly an order of magnitude lower than the blood flow rate, virtually complete equilibration of low-molecular-weight solutes is achieved between plasma and dialysate. Thus, regardless of modality of CRRT, clearance of urea and other low-molecular-weight solutes is approximately equal to effluent flow.
Although several studies published 15 to 20 years ago suggested that higher effluent flow rates were associated with improved survival,3, 60 the results were inconsistent,27, 61 and this relationship was not confirmed in two large, multicenter, randomized controlled trials. In the VA/NIH Acute Renal Failure Trial Network (ATN) study, 1,124 critically ill patients with AKI were randomized to receive RRT using either a more-intensive strategy (CVVHDF at an effluent flow of 35 mL/kg per hour, or IHD or PIRRT six times per week) or a less-intensive strategy (CVVHDF at an effluent flow of 20 mL/kg per hour, or IHD or PIRRT three times per week).62 Within each treatment arm, patients switched between CVVHDF or PIRRT and IHD based on hemodynamic status. More intensive renal support was not associated with differences in mortality, recovery of kidney function, or the rate of nonrenal organ failure across the entire study population or when assessed based on the percentage of time receiving CVVHDF or PIRRT.63 The Randomized Evaluation of Normal versus Augmented Level (RENAL) Replacement Therapy Study randomized 1,508 patients with AKI across 31 ICUs in Australia and New Zealand to CVVHDF at an effluent flow of either 25 or 40 mL/kg per hour.64 As in the ATN study, the use of more intensive solute clearance was not associated with improved clinical outcomes. On the basis of these data, the KDIGO Clinical Practice Guidelines recommend a target dose for CRRT of 20 to 25 mL/kg per hour, noting that a higher prescribed dose may be required to ensure delivery of this target dose.21
Volume Management
A second dimension to the prescription of RRT is volume management. Net ultrafiltration may be adjusted independently of solute clearance. As previously discussed, severity of volume overload is strongly associated with mortality risk in both children and adults with RRT-requiring AKI.22, 30, 31 However, optimal strategies for volume management are uncertain, requiring a balance between the provision of net ultrafiltration to achieve euvolemia, optimization of cardiopulmonary status, and the risk of exacerbating hypotension. Management must be individualized for each patient, with frequent reassessment of ultrafiltration targets. It should be recognized that short-term fluctuation in BP is generally unrelated to volume status and that transient hypotension during CRRT needs to be carefully assessed for nonvolume-mediated factors and often requires management independent of alterations in ultrafiltration targets.
Role of CRRT in Sepsis
Although cytokine modulation by CVVH has been proposed as an adjunctive therapy in sepsis, clinical trials have not shown any meaningful benefit. In a trial of 80 patients randomized to receive isovolemic hemofiltration or usual care, there was no improvement in clinical parameters or mortality with hemofiltration.28 Similarly, in the High-Volume Versus Standard-Volume Haemofiltration for Septic Shock Patients With Acute Kidney Injury (IVOIRE) trial, which compared CVVH at 35 and 70 mL/kg per hour in patients with septic AKI, no benefit was associated with the higher dose of hemofiltration.29 Thus, current data do not support the use of CRRT as an adjunctive therapy in sepsis beyond its role for renal support.
Technical Issues in CRRT Management
Vascular Access
Initiation of CRRT requires vascular access, which is generally established through placement of a large-bore double lumen catheter in an internal jugular, femoral, or subclavian vein. In adults, catheter design and position must be sufficient to sustain blood flow rates of 200 to 300 mL/min. Cannulation of the right internal jugular vein is generally preferred over the left, given the straighter course from the right side to the right atrium. Although femoral catheters are generally associated with higher rates of bacteremia than internal jugular catheters,65 comparable rates of colonization, bacteremia, and thrombosis were observed with femoral and internal jugular dialysis catheters in a randomized controlled trial of 750 patients with RRT-requiring AKI.66 However, the relative risk for femoral catheter colonization was higher in patients with a BMI > 28.4 kg/m2. Subclavian cannulation is generally avoided because of the higher risk of insertion complications and because of the risk of subsequent venous stenosis.67, 68 Based on these considerations, the KDIGO Clinical Practice Guidelines for AKI recommend the right internal jugular vein as the preferred location for catheter placement, followed by the femoral and the left internal jugular veins.21
Proper positioning of the catheter tip is critical for adequate catheter function. For internal jugular catheters, the catheter tip should be at the junction of the superior vena cava and right atrium or in the right atrium, depending on catheter design, rather than more proximally in the superior vena cava.69 To permit proper positioning, a longer catheter is required when the left internal jugular vein is cannulated than when the right is used. Even longer catheters are required for femoral catheters to permit placement with the catheter tip within, or as close to, the inferior vena cava. Catheter malposition is associated with restricted blood flow and increased risk of recirculation. In addition, catheter malfunction is a frequent cause for interruption in circuit flow and filter clotting. Adequacy of catheter function should be assessed whenever there is frequent system clotting. Although tunneled catheters are not recommended for routine use, they are associated with decreased risks of infection and higher blood flow rates, and should be considered when the need for RRT is expected to exceed 1 to 3 weeks.21
Anticoagulation for CRRT
Clotting of the extracorporeal circuit is the most common complication during CRRT. Practice patterns regarding the use of anticoagulation vary widely, with estimates of 30% to 60% of patients undergoing CRRT without anticoagulation.62, 70 Although the use of anticoagulation is often avoided in patients who are coagulopathic, thrombocytopenic, or are having active hemorrhage, anticoagulation-free treatment may also be successful in the absence of coagulopathy and thrombocytopenia. Strategies to minimize the risk of clotting of the extracorporeal circuit include the following: use of higher blood flow rates; minimization of filtration fraction (the ratio of ultrafiltration to plasma flow) by using CVVHD rather than CVVH, or by infusing replacement fluids prefilter during CVVH and CVVHDF; ensuring optimal catheter function and responding promptly to machine alarms to minimize interruptions in blood flow; and increasing the frequency of scheduled replacement of the extracorporeal circuit.62, 64 In the absence of anticoagulation, increased vigilance is required to ensure there is no compromise of delivered dose.71
When anticoagulation is used, the most common strategies rely on heparin or citrate. Either unfractionated heparin (UFH) or low-molecular-weight heparin may be used. Dosing protocols for UFH during CRRT vary widely, ranging from very low dose (initial bolus of 500-1,000 units followed by infusions of 300-500 units per hour), designed to minimize systemic effects, to bolus doses of 30 units/kg followed by infusions of 5 to 10 units/kg per hour with a target systemic activated partial thromboplastin time of 1.5 to 2.0 times the upper limit of normal.72 Low-molecular-weight heparins have been proposed as an alternative to UFH given higher anti-factor Xa activity, a more consistent anticoagulant response, and a lower incidence of heparin-induced thrombocytopenia. However, consistent superiority of low-molecular-weight heparin compared with UFH has not been shown.73, 74 In patients with heparin-induced thrombocytopenia, all heparin anticoagulation should be discontinued, and anticoagulation with direct thrombin inhibitors initiated.21 Argatroban is generally preferred; however, it is hepatically metabolized. In patients with both liver failure and AKI, bivalirudin is preferred given its significant nonrenal and nonhepatic metabolism.
The use of citrate as an anticoagulant is based on its rapid chelation of calcium in the extracorporeal circuit, inhibiting multiple calcium-dependent steps in the coagulation cascade. The citrate-calcium complex dissociates in the systemic circulation, and the citrate is rapidly metabolized, serving as an alkalinizing agent. Citrate is infused into the extracorporeal circuit with a goal of reducing the ionized calcium concentration to < 0.4 mmol/L. Because some of the citrate-calcium complex is lost in the effluent, systemic infusion of calcium is required to prevent hypocalcemia. Regional citrate anticoagulation is associated with improved circuit patency, lower risks of bleeding, and avoidance of the risk of heparin-induced thrombocytopenia compared with heparin.75, 76, 77, 78, 79 However, citrate anticoagulation is associated with increased risks of multiple electrolyte and acid-base disturbances. Close monitoring of both circuit and systemic blood ionized calcium levels is required to ensure sufficient efficacy without systemic hypocalcemia. Hypernatremia may result when hypertonic citrate solutions are used. Because metabolism of citrate potentially yields bicarbonate in a 1:3 ratio, citrate anticoagulation may predispose to development of metabolic alkalosis. In addition, in patients with severe liver disease or other impairment in citrate metabolism, citrate may accumulate and contribute to a high-anion-gap metabolic acidosis. Thus, in addition to monitoring the ionized calcium in the extracorporeal circuit to ensure adequate calcium chelation, systemic electrolytes, magnesium, total and ionized calcium, and blood pH need to be monitored frequently. Recommendations are to check these laboratory readings 1 h after initiating or making any change in citrate anticoagulation or the CRRT prescription, and then at least every 6 h. Citrate accumulation should be suspected if the need for calcium infusion to maintain systemic ionized calcium levels increases, if there is an increasing anion-gap metabolic acidosis, or if the ratio of systemic total calcium to ionized calcium is > 2.5. If citrate toxicity is suspected, the use of citrate should be suspended or discontinued.
Drug Dosing During CRRT
Medication dosing during CRRT can be challenging because drug dosing needs to account for multiple factors beyond the extracorporeal drug removal, including nonrenal clearance, residual kidney function, and changes in volume of distribution and protein binding.37, 80 Errors in drug dosing can lead to both toxicity from inadequate dose reduction and treatment failure from underdosing.37 The latter is of particular importance for antibiotic dosing in patients with sepsis accompanying their AKI.80, 81
A detailed discussion of drug dosing during CRRT is beyond the scope of the present review; however, the following broad guidelines are provided. For medications such as analgesics, sedatives, and vasopressors, which have an observable clinical effect, dosing should be titrated to the desired clinical response. Drugs with high molecular weight, that are highly protein bound, or that have very large volumes of distribution will be poorly cleared by CRRT, and dosing does not need to be adjusted for RRT. The extracorporeal clearance of low-molecular-weight drugs that are nonprotein bound will approximate effluent flow; for protein-bound drugs, the estimated clearance needs to be adjusted for the percent unbound fraction. For all medications with readily measurable blood levels, dosing should be adjusted based on pharmacokinetic monitoring. Finally, it must be recognized that although published guides provide estimates for dosing of many agents, they provide only general parameters that may not correspond to the specific CRRT mode and dose used.82
Nutritional Management
Patients with AKI who are undergoing CRRT are usually in substantial negative nitrogen balance due to high protein catabolic rates. In addition, CRRT results in amino acid loss as well as losses of water-soluble vitamins and other micronutrients. Caloric intake of approximately 35 kcal/kg per day should be provided, with a target protein intake of 1.5 g/kg per day and with supplementation of water-soluble vitamins.83, 84 Although enteral feeding is preferred, parenteral support may be necessary.
Complications of CRRT
As with all medical interventions, CRRT is not without its risks (Table 2).33 Initiation of CRRT requires placement of a large-bore central venous catheter that may need to be maintained for a prolonged duration. Well-recognized complications of catheter insertion include vascular or visceral injury resulting in hemorrhage, pneumothorax, hemothorax, and arterio-venous fistula formation. Prolonged catheter use is associated with venous thrombosis or stenosis. Blood exposure to the extracorporeal circuit may trigger immediate allergic or delayed immunologic reactions secondary to cytokine activation.85 Bradykinin-mediated membrane reactions have been associated with certain synthetic membranes in conjunction with the use of angiotensin-converting enzyme inhibitors.86 Air embolization may occur at the time of catheter insertion or removal and at any time during treatment if air is entrained into the circuit beyond the return line air detector.
Table 2.
Complications Associated With CRRT
| Catheter-related complications |
| Hemorrhage |
| Infection |
| Venous thrombosis |
| Venous stenosis |
| Traumatic arteriovenous fistula |
| Pneumothorax |
| Hemothorax |
| Air embolism |
| Visceral injury |
| Extracorporeal circuit-related complications |
| Allergic reaction to hemodialyzer/hemofilter or tubing |
| Circuit thrombosis |
| Hemolysis |
| Air embolism |
| Hypothermia |
| Hypotension |
| Electrolyte disturbances |
| Hypophosphatemia |
| Hypokalemia |
| Hypocalcemia |
| Hypomagnesemia |
| Incorrect medication dosing |
CRRT = continuous renal replacement therapy.
The most common complication during CRRT is circuit clotting, and the most common reason for circuit clotting is inadequate catheter function resulting in flow restriction and pressure alarms that interrupt blood flow. Prompt catheter replacement may be necessary if a blood flow of 200 to 300 mL/min cannot be sustained. Excessive filtration fraction may lead to hemoconcentration within the hemofilter, also contributing to filter clotting. If there is no catheter dysfunction, blood flow is maximized, and filtration fraction is < 20%, initiation or intensification of anticoagulation should be considered. Complications of heparin anticoagulation can include bleeding and heparin-induced thrombocytopenia. Citrate anticoagulation may result in citrate toxicity from citrate accumulation, overt hypocalcemia from inadequate calcium replacement, and both metabolic acidosis and metabolic alkalosis.
Electrolyte abnormalities during CRRT are common. Hypophosphatemia may result from continuous removal in the extracorporeal circuit and can delay weaning from mechanical ventilation.62, 64 Hypophosphatemia may be avoided by pre-emptive enteral or parenteral phosphate supplementation or by the use of phosphate-containing dialysate or replacement fluids.87 Other electrolyte abnormalities are less common, although hyponatremia and hypernatremia and hyperkalemia have resulted from compounding errors in custom manufactured dialysate and replacement fluids.88 To monitor electrolyte status, laboratory monitoring should be performed at least daily during treatment.
Unlike conventional IHD, dialysate and replacement fluids are usually not warmed. Modest thermal losses during CRRT cause vasoconstriction and are believed to contribute to increased hemodynamic stability but may mask the onset of fever. If thermal losses are more substantial, significant hypothermia may ensue, necessitating aggressive external warming.
Hypotension during CRRT is common, occurring in some series in more than one third of patients, but is most often unrelated to the CRRT procedure, per se.12, 89, 90 Ultrafiltration exacerbating hemodynamic instability is the most common treatment-related factor contributing to hypotension. Negative inotropic and vasodilating properties associated with acetate- and lactate-buffered solutions previously contributed to treatment-related hypotension; however, with the availability of bicarbonate-buffered dialysate and replacement fluids, this scenario is no longer a significant consideration.90 Hypotension may also be seen upon initiation of treatment, particularly if the circuit prime is not reinfused; this result has been of particular concern in pediatric patients and may be mitigated by using albumin to prime the circuit.91 Although increases in blood flow through the extracorporeal circuit were associated with increased circuit volume and hypotension with older dialysis systems, there is minimal change in extracorporeal volume and thus negligible hemodynamic stress associated with changes in blood flow using current CRRT technology and hollow fiber filters.90, 92, 93 When hypotension is associated with volume depletion, it should be treated with volume reinfusion and adjustment in ultrafiltration targets; in other circumstances, alternative etiologies should be considered and the hypotension managed with titration of vasopressor support.
Discontinuation of CRRT
There are no specific criteria for discontinuation of CRRT because of recovery of kidney function or transition to other modalities of RRT.59, 94, 95 An initial manifestation of recovery of kidney function is increased urine output, although specific criteria are sparse. In the observational Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) study, a urine output > 400 mL/d without concomitant diuretic therapy was a predictor of successful CRRT discontinuation.96 In this observational cohort, patients who were successfully discontinued from CRRT without requiring re-initiation were more likely to survive to hospital discharge compared with those requiring re-initiation of CRRT. In another study, urine output > 500 mL/d was proposed as a criterion for discontinuation of RRT in a study of initiation and discontinuation of therapy in patients with AKI.97 The usefulness of this criterion is uncertain, however, as the treating clinicians continued RRT despite this recommendation approximately two thirds of the time, citing continued volume overload as the most common reason for continuation of RRT. In the ATN study, a 6-h timed urine collection was obtained when the urine output was > 750 mL/d.62 RRT was continued if the measured creatinine clearance was < 12 mL/min, was discontinued if > 20 mL/min, and was left to clinician judgment if the measured creatinine clearance was between 12 and 20 mL/min. Although these strategies can inform clinical decision-making, precise criteria for discontinuation of RRT are lacking.
The transition of patients with improved hemodynamic status but persistent AKI to other modalities of RRT is also highly variable. PIRRT may be used as a transitional therapy or patients may transition directly to IHD, as clinical status warrants. Transition from CRRT to PIRRT or IHD may facilitate initiation of physical therapy and mobilization out of bed. In general, patients with persistent RRT-dependent AKI must be transitioned to IHD prior to ICU discharge.
Ethical Issues in Initiating and Discontinuing RRT
Issues related to the clinical and ethical appropriateness of initiation or continuation of RRT often occur in patients with AKI. Discussions of initiation and discontinuation of therapy with patients and/or their family/surrogate decision-makers should be framed in light of the overall prognosis and goals of care, and need to consider other life-sustaining treatments in addition to RRT. It is important to ensure that both the primary managing service and nephrology consultants managing the RRT provide a consistent assessment of prognosis and treatment options, presented in a clear but sympathetic manner, to facilitate the process of shared decision-making.98 The high mortality of AKI in the setting of critical illness and the complex and emotionally laden aspects of the decisions associated with initiating or discontinuing renal support suggest that early involvement of palliative care services may be of benefit.99 Time-limited trials of RRT may be a useful strategy in circumstances in which there is uncertainty of prognosis or when the patient or family/surrogate decision-maker are not prepared to make a definite decision regarding initiating or discontinuing RRT and other life-sustaining care.100
Conclusions
CRRT has become a mainstay in the management of AKI in critically ill patients. In patients who do not have objective indications for the emergent initiation of renal support, the optimal timing of RRT remains controversial. Although the use of continuous therapies may facilitate management in hemodynamically unstable patients, existing data do not show that use of CRRT results in improved survival or recovery of kidney function compared with alternatives such as conventional IHD and PIRRT. Large, well-designed clinical trials have established that for the majority of patients, augmenting solute clearance using effluent flow rates > 20 to 25 mL/kg per hour is not associated with improved outcomes; however, optimal strategies for volume management still must be defined. Similarly, other aspects of the management of CRRT are subject to substantial variations in practice, including strategies for anticoagulation. Finally, the role of CRRT needs to be considered in the setting of overall goals of care and the use of other life-sustaining treatments.
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: P. M. P. has received research support from BioPorto and consulting fees from Novartis, GE Healthcare, Baxter, HealthSpan Dx, and Durect. None declared (S. T.).
References
- 1.Tolwani A. Continuous renal-replacement therapy for acute kidney injury. N Engl J Med. 2012;367(26):2505–2514. doi: 10.1056/NEJMct1206045. [DOI] [PubMed] [Google Scholar]
- 2.Liu K.D., Himmelfarb J., Paganini E. Timing of initiation of dialysis in critically ill patients with acute kidney injury. Clin J Am Soc Nephrol. 2006;1(5):915–919. doi: 10.2215/CJN.01430406. [DOI] [PubMed] [Google Scholar]
- 3.Saudan P., Niederberger M., De Seigneux S. Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute renal failure. Kidney Int. 2006;70(7):1312–1317. doi: 10.1038/sj.ki.5001705. [DOI] [PubMed] [Google Scholar]
- 4.Uchino S., Kellum J.A., Bellomo R. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294(7):813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 5.Hsu R.K., McCulloch C.E., Dudley R.A., Lo L.J., Hsu C.Y. Temporal changes in incidence of dialysis-requiring AKI. J Am Soc Nephrol. 2013;24(1):37–42. doi: 10.1681/ASN.2012080800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macedo E., Mehta R.L. Continuous dialysis therapies: core curriculum 2016. Am J Kidney Dis. 2016;68(4):645–657. doi: 10.1053/j.ajkd.2016.03.427. [DOI] [PubMed] [Google Scholar]
- 7.Marshall M.R., Ma T., Galler D., Rankin A.P.N., Williams A.B. Sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring renal replacement therapy: towards an adequate therapy. Nephrol Dial Transplant. 2004;19(4):877–884. doi: 10.1093/ndt/gfg625. [DOI] [PubMed] [Google Scholar]
- 8.Burdmann E.A., Chakravarthi R. Peritoneal dialysis in acute kidney injury: lessons learned and applied. Semin Dial. 2011;24(2):149–156. doi: 10.1111/j.1525-139X.2011.00868.x. [DOI] [PubMed] [Google Scholar]
- 9.Mehta R.L., McDonald B., Gabbai F.B. A randomized clinical trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int. 2001;60(3):1154–1163. doi: 10.1046/j.1523-1755.2001.0600031154.x. [DOI] [PubMed] [Google Scholar]
- 10.Augustine J.J., Sandy D., Seifert T.H., Paganini E.P. A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis. 2004;44(6):1000–1007. doi: 10.1053/j.ajkd.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 11.Uehlinger D.E., Jakob S.M., Ferrari P. Comparison of continuous and intermittent renal replacement therapy for acute renal failure. Nephrol Dial Transplant. 2005;20(8):1630–1637. doi: 10.1093/ndt/gfh880. [DOI] [PubMed] [Google Scholar]
- 12.Vinsonneau C., Camus C., Combes A. Continuous venovenous haemodiafiltration versus intermittent haemodialysis for acute renal failure in patients with multiple-organ dysfunction syndrome: a multicentre randomised trial. Lancet. 2006;368(9533):379–385. doi: 10.1016/S0140-6736(06)69111-3. [DOI] [PubMed] [Google Scholar]
- 13.Lins R.L., Elseviers M.M., Van der Niepen P. Intermittent versus continuous renal replacement therapy for acute kidney injury patients admitted to the intensive care unit: results of a randomized clinical trial. Nephrol Dial Transplant. 2009;24(2):512–518. doi: 10.1093/ndt/gfn560. [DOI] [PubMed] [Google Scholar]
- 14.Schefold J.C., von Haehling S., Pschowski R. The effect of continuous versus intermittent renal replacement therapy on the outcome of critically ill patients with acute renal failure (CONVINT): a prospective randomized controlled trial. Crit Care. 2014;18(1):R11. doi: 10.1186/cc13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bagshaw S.M., Berthiaume L.R., Delaney A., Bellomo R. Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med. 2008;36(2):610–617. doi: 10.1097/01.CCM.0B013E3181611F552. [DOI] [PubMed] [Google Scholar]
- 16.Pannu N., Klarenbach S., Wiebe N., Manns B., Tonelli M. Alberta Kidney Disease N. Renal replacement therapy in patients with acute renal failure: a systematic review. JAMA. 2008;299(7):793–805. doi: 10.1001/jama.299.7.793. [DOI] [PubMed] [Google Scholar]
- 17.Friedrich J.O., Wald R., Bagshaw S.M., Burns K.E.A., Adhikari N.K. Hemofiltration compared to hemodialysis for acute kidney injury: systematic review and meta-analysis. Critical Care. 2012;16(4):R146. doi: 10.1186/cc11458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang L., Yang J., Eastwood G.M., Zhu G., Tanaka A., Bellomo R. Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: a meta-analysis. Am J Kidney Dis. 2015;66(2):322–330. doi: 10.1053/j.ajkd.2015.02.328. [DOI] [PubMed] [Google Scholar]
- 19.Kielstein J.T., Kretschmer U., Ernst T. Efficacy and cardiovascular tolerability of extended dialysis in critically ill patients: a randomized controlled study. Am J Kidney Dis. 2004;43(2):342–349. doi: 10.1053/j.ajkd.2003.10.021. [DOI] [PubMed] [Google Scholar]
- 20.Schwenger V., Weigand M.A., Hoffmann O. Sustained low efficiency dialysis using a single-pass batch system in acute kidney injury—a randomized interventional trial: the REnal Replacement Therapy Study in Intensive Care Unit PatiEnts. Crit Care. 2012;16(4):R140. doi: 10.1186/cc11445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. 2012;2012(suppl):1–138. [Google Scholar]
- 22.Bouchard J., Soroko S.B., Chertow G.M. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76(4):422–427. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- 23.Davenport A. Continuous renal replacement therapies in patients with liver disease. Semin Dial. 2009;22(2):169–172. doi: 10.1111/j.1525-139X.2008.00539.x. [DOI] [PubMed] [Google Scholar]
- 24.Davenport A. Continuous renal replacement therapies in patients with acute neurological injury. Semin Dial. 2009;22(2):165–168. doi: 10.1111/j.1525-139X.2008.00548.x. [DOI] [PubMed] [Google Scholar]
- 25.Lin C.M., Lin J.W., Tsai J.T. Intracranial pressure fluctuation during hemodialysis in renal failure patients with intracranial hemorrhage. Acta Neurochir Suppl. 2008;101:141–144. doi: 10.1007/978-3-211-78205-7_24. [DOI] [PubMed] [Google Scholar]
- 26.Ronco C., Bellomo R., Brendolan A., Pinna V., La Greca G. Brain density changes during renal replacement in critically ill patients with acute renal failure. Continuous hemofiltration versus intermittent hemodialysis. J Nephrol. 1999;12(3):173–178. [PubMed] [Google Scholar]
- 27.Tolwani A.J., Campbell R.C., Stofan B.S., Lai K.R., Oster R.A., Wille K.M. Standard versus high-dose CVVHDF for ICU-related acute renal failure. J Am Soc Nephrol. 2008;19(6):1233–1238. doi: 10.1681/ASN.2007111173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Payen D., Mateo J., Cavaillon J.M. Impact of continuous venovenous hemofiltration on organ failure during the early phase of severe sepsis: a randomized controlled trial. Crit Care Med. 2009;37(3):803–810. doi: 10.1097/CCM.0b013e3181962316. [DOI] [PubMed] [Google Scholar]
- 29.Joannes-Boyau O., Honore P.M., Perez P. High-volume versus standard-volume haemofiltration for septic shock patients with acute kidney injury (IVOIRE study): a multicentre randomized controlled trial. Intensive Care Med. 2013;39(9):1535–1546. doi: 10.1007/s00134-013-2967-z. [DOI] [PubMed] [Google Scholar]
- 30.Sutherland S.M., Zappitelli M., Alexander S.R. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis. 2010;55(2):316–325. doi: 10.1053/j.ajkd.2009.10.048. [DOI] [PubMed] [Google Scholar]
- 31.Vaara S.T., Korhonen A.M., Kaukonen K.M. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care. 2012;16(5):R197. doi: 10.1186/cc11682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yessayan L., Yee J., Frinak S., Szamosfalvi B. Continuous renal replacement therapy for the management of acid-base and electrolyte imbalances in acute kidney injury. Adv Chronic Kidney Dis. 2016;23(3):203–210. doi: 10.1053/j.ackd.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 33.Finkel K.W., Podoll A.S. Complications of continuous renal replacement therapy. Seminars in Dialysis. 2009;22(2):155–159. doi: 10.1111/j.1525-139X.2008.00550.x. [DOI] [PubMed] [Google Scholar]
- 34.Cerda J., Tolwani A.J., Warnock D.G. Critical care nephrology: management of acid-base disorders with CRRT. Kidney Int. 2012;82(1):9–18. doi: 10.1038/ki.2011.243. [DOI] [PubMed] [Google Scholar]
- 35.Kellum J.A., Murugan R., Nadim M.K. Indications, timing, and patient selection. In: Kellum J.A., Bellomo R., Ronco C., editors. Continuous Renal Replacement Therapy. Oxford University Press; New York: 2016. pp. 48–56. [Google Scholar]
- 36.Meyer T.W., Hostetter T.H. Uremia. N Engl J Med. 2007;357(13):1316–1325. doi: 10.1056/NEJMra071313. [DOI] [PubMed] [Google Scholar]
- 37.Mueller B.A., Pasko D.A., Sowinski K.M. Higher renal replacement therapy dose delivery influences on drug therapy. Artif Organs. 2003;27(9):808–814. doi: 10.1046/j.1525-1594.2003.07283.x. [DOI] [PubMed] [Google Scholar]
- 38.Ghannoum M., Nolin T.D., Lavergne V., Hoffman R.S., EXTRIP Workgroup Blood purification in toxicology: nephrology's ugly duckling. Adv Chronic Kidney Dis. 2011;18(3):160–166. doi: 10.1053/j.ackd.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 39.Patel N., Bayliss G.P. Developments in extracorporeal therapy for the poisoned patient. Adv Drug Deliv Rev. 2015;90:3–11. doi: 10.1016/j.addr.2015.05.017. [DOI] [PubMed] [Google Scholar]
- 40.Spinale J.M., Laskin B.L., Sondheimer N., Swartz S.J., Goldstein S.L. High-dose continuous renal replacement therapy for neonatal hyperammonemia. Pediatr Nephrol. 2013;28(6):983–986. doi: 10.1007/s00467-013-2441-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hanudel M., Avasare S., Tsai E., Yadin O., Zaritsky J. A biphasic dialytic strategy for the treatment of neonatal hyperammonemia. Pediatr Nephrol. 2014;29(2):315–320. doi: 10.1007/s00467-013-2638-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Slack A.J., Auzinger G., Willars C. Ammonia clearance with haemofiltration in adults with liver disease. Liver Int. 2014;34(1):42–48. doi: 10.1111/liv.12221. [DOI] [PubMed] [Google Scholar]
- 43.Cardoso FS, Gottfried M, Tujios S, Olson JC, Karvellas CJ, US Acute Live Failure Study Group. Continuous renal replacement therapy is associated with reduced serum ammonia levels and mortality in acute liver failure [published online ahead of print August 31, 2017]. Hepatology.https://doi.org/10.1002/hep.29488. [DOI] [PMC free article] [PubMed]
- 44.Wald R., Adhikari N.K.J., Smith O.M. Comparison of standard and accelerated initiation of renal replacement therapy in acute kidney injury. Kidney Int. 2015;88(4):897–904. doi: 10.1038/ki.2015.184. [DOI] [PubMed] [Google Scholar]
- 45.Gettings L.G., Reynolds H.N., Scalea T. Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early vs. late. Intensive Care Med. 1999;25(8):805–813. doi: 10.1007/s001340050956. [DOI] [PubMed] [Google Scholar]
- 46.Durmaz I., Yagdi T., Calkavur T. Prophylactic dialysis in patients with renal dysfunction undergoing on-pump coronary artery bypass surgery. Ann Thorac Surg. 2003;75(3):859–864. doi: 10.1016/s0003-4975(02)04635-0. [DOI] [PubMed] [Google Scholar]
- 47.Sugahara S., Suzuki H. Early start on continuous hemodialysis therapy improves survival rate in patients with acute renal failure following coronary bypass surgery. Hemodial Int. 2004;8(4):320–325. doi: 10.1111/j.1492-7535.2004.80404.x. [DOI] [PubMed] [Google Scholar]
- 48.Elahi M.M., Lim M.Y., Joseph R.N., Dhannapuneni R.R., Spyt T.J. Early hemofiltration improves survival in post-cardiotomy patients with acute renal failure. Eur J Cardiothorac Surg. 2004;26(5):1027–1031. doi: 10.1016/j.ejcts.2004.07.039. [DOI] [PubMed] [Google Scholar]
- 49.Demirkilic U., Kuralay E., Yenicesu M. Timing of replacement therapy for acute renal failure after cardiac surgery. J Card Surg. 2004;19(1):17–20. doi: 10.1111/j.0886-0440.2004.04004.x. [DOI] [PubMed] [Google Scholar]
- 50.Manche A., Casha A., Rychter J., Farrugia E., Debono M. Early dialysis in acute kidney injury after cardiac surgery. Interact Cardiovasc Thorac Surg. 2008;7(5):829–832. doi: 10.1510/icvts.2008.181909. [DOI] [PubMed] [Google Scholar]
- 51.Karvellas C.J., Farhat M.R., Sajjad I. A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: a systematic review and meta-analysis. Crit Care. 2011;15(1):R72. doi: 10.1186/cc10061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang X., Jie Yuan W. Timing of initiation of renal replacement therapy in acute kidney injury: a systematic review and meta-analysis. Ren Fail. 2012;34(3):396–402. doi: 10.3109/0886022X.2011.647371. [DOI] [PubMed] [Google Scholar]
- 53.Zarbock A., Kellum J.A., Schmidt C. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA. 2016;315(20):2190–2199. doi: 10.1001/jama.2016.5828. [DOI] [PubMed] [Google Scholar]
- 54.Gaudry S., Hajage D., Schortgen F. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med. 2016;375(2):122–133. doi: 10.1056/NEJMoa1603017. [DOI] [PubMed] [Google Scholar]
- 55.Gaudry S., Hajage D., Schortgen F. Timing of renal support and outcome of septic shock and acute respiratory distress syndrome. A post hoc analysis of the AKIKI randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):58–66. doi: 10.1164/rccm.201706-1255OC. [DOI] [PubMed] [Google Scholar]
- 56.Barbar S.D., Clere-Jehl R., Bourredjem A. Timing of renal-replacement therapy in patients with acute kidney injury and sepsis. N Engl J Med. 2018;379(15):1431–1442. doi: 10.1056/NEJMoa1803213. [DOI] [PubMed] [Google Scholar]
- 57.Vanmassenhove J., Vanholder R., Van Biesen W., Lameire N. Haste makes waste-Should current guideline recommendations for initiation of renal replacement therapy for acute kidney injury be changed? Semin Dial. 2018;31(3):204–208. doi: 10.1111/sdi.12693. [DOI] [PubMed] [Google Scholar]
- 58.Van Wert R., Friedrich J.O., Scales D.C., Wald R., Adhikari N.K.J., University of Toronto Acute Kidney Injury Research Group High-dose renal replacement therapy for acute kidney injury: systematic review and meta-analysis. Crit Care Med. 2010;38(5):1360–1369. doi: 10.1097/CCM.0b013e3181d9d912. [DOI] [PubMed] [Google Scholar]
- 59.Bouchard J., Weidemann C., Mehta R.L. Renal replacement therapy in acute kidney injury: intermittent versus continuous? How much is enough? Adv Chronic Kidney Dis. 2008;15(3):235–247. doi: 10.1053/j.ackd.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 60.Ronco C., Bellomo R., Homel P. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet. 2000;356(9223):26–30. doi: 10.1016/S0140-6736(00)02430-2. [DOI] [PubMed] [Google Scholar]
- 61.Bouman C.S., Oudemans-Van Straaten H.M., Tijssen J.G., Zandstra D.F., Kesecioglu J. Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective, randomized trial. Crit Care Med. 2002;30(10):2205–2211. doi: 10.1097/00003246-200210000-00005. [DOI] [PubMed] [Google Scholar]
- 62.VA/NIH Acute Renal Failure Trial Network. Palevsky P.M., Zhang J.H. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359(1):7–20. doi: 10.1056/NEJMoa0802639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Palevsky P.M., O'Connor T.Z., Chertow G.M. Intensity of renal replacement therapy in acute kidney injury: perspective from within the Acute Renal Failure Trial Network Study. Crit Care. 2009;13(4):310. doi: 10.1186/cc7901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.RENAL Replacement Therapy Study Investigators. Bellomo R., Cass A. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med. 2009;361(17):1627–1638. doi: 10.1056/NEJMoa0902413. [DOI] [PubMed] [Google Scholar]
- 65.Oliver M.J., Callery S.M., Thorpe K.E., Schwab S.J., Churchill D.N. Risk of bacteremia from temporary hemodialysis catheters by site of insertion and duration of use: a prospective study. Kidney Int. 2000;58(6):2543–2545. doi: 10.1046/j.1523-1755.2000.00439.x. [DOI] [PubMed] [Google Scholar]
- 66.Parienti J.J., Thirion M., Megarbane B. Femoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trial. JAMA. 2008;299(20):2413–2422. doi: 10.1001/jama.299.20.2413. [DOI] [PubMed] [Google Scholar]
- 67.el-Nachef M.W., Rashad F., Ricanati E.S. Occlusion of the subclavian vein: a complication of indwelling subclavian venous catheters for hemodialysis. Clin Nephrol. 1985;24(1):42–46. [PubMed] [Google Scholar]
- 68.Schwab S.J., Quarles L.D., Middleton J.P., Cohan R.H., Saeed M., Dennis V.W. Hemodialysis-associated subclavian vein stenosis. Kidney Int. 1988;33(6):1156–1159. doi: 10.1038/ki.1988.124. [DOI] [PubMed] [Google Scholar]
- 69.Morgan D., Ho K., Murray C., Davies H., Louw J. A randomized trial of catheters of different lengths to achieve right atrium versus superior vena cava placement for continuous renal replacement therapy. Am J Kidney Dis. 2012;60(2):272–279. doi: 10.1053/j.ajkd.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 70.Uchino S., Bellomo R., Morimatsu H. Continuous renal replacement therapy: A worldwide practice survey. Intensive Care Med. 2007;33(5):1563–1570. doi: 10.1007/s00134-007-0754-4. [DOI] [PubMed] [Google Scholar]
- 71.Vesconi S., Cruz D.N., Fumagalli R. Delivered dose of renal replacement therapy and mortality in critically ill patients with acute kidney injury. Critical Care. 2009;13(2):R57. doi: 10.1186/cc7784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van de Wetering J., Westendorp R.G., van der Hoeven J.G., Stolk B., Feuth J.D., Chang P.C. Heparin use in continuous renal replacement procedures: the struggle between filter coagulation and patient hemorrhage. J Am Soc Nephrol. 1996;7(1):145–150. doi: 10.1681/ASN.V71145. [DOI] [PubMed] [Google Scholar]
- 73.Joannidis M., Kountchev J., Rauchenzauner M. Enoxaparin vs. unfractionated heparin for anticoagulation during continuous veno-venous hemofiltration: a randomized controlled crossover study. Intensive Care Med. 2007;33(9):1571–1579. doi: 10.1007/s00134-007-0719-7. [DOI] [PubMed] [Google Scholar]
- 74.Reeves J.H., Cumming A.R., Gallagher L., O'Brien J.L., Santamaria J.D. A controlled trial of low-molecular-weight heparin (dalteparin) versus unfractionated heparin as anticoagulant during continuous venovenous hemodialysis with filtration. Crit Care Med. 1999;27(10):2224–2228. doi: 10.1097/00003246-199910000-00026. [DOI] [PubMed] [Google Scholar]
- 75.Oudemans-van Straaten H.M., Bosman R.J., Koopmans M. Citrate anticoagulation for continuous venovenous hemofiltration. Crit Care Med. 2009;37(2):545–552. doi: 10.1097/CCM.0b013e3181953c5e. [DOI] [PubMed] [Google Scholar]
- 76.Oudemans-van Straaten H.M., Kellum J.A., Bellomo R. Clinical review: anticoagulation for continuous renal replacement therapy—heparin or citrate? Crit Care. 2011;15(1):202. doi: 10.1186/cc9358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wu M.Y., Hsu Y.H., Bai C.H., Lin Y.F., Wu C.H., Tam K.W. Regional citrate versus heparin anticoagulation for continuous renal replacement therapy: a meta-analysis of randomized controlled trials. Am J Kidney Dis. 2012;59(6):810–818. doi: 10.1053/j.ajkd.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 78.Tolwani A.J., Prendergast M.B., Speer R.R., Stofan B.S., Wille K.M. A practical citrate anticoagulation continuous venovenous hemodiafiltration protocol for metabolic control and high solute clearance. Clin J Am Soc Nephrol. 2006;1(1):79–87. doi: 10.2215/CJN.00040505. [DOI] [PubMed] [Google Scholar]
- 79.Tolwani A., Wille K.M. Advances in continuous renal replacement therapy: citrate anticoagulation update. Blood Purif. 2012;34(2):88–93. doi: 10.1159/000342378. [DOI] [PubMed] [Google Scholar]
- 80.Pea F., Viale P., Pavan F., Furlanut M. Pharmacokinetic considerations for antimicrobial therapy in patients receiving renal replacement therapy. Clin Pharmacokinet. 2007;46(12):997–1038. doi: 10.2165/00003088-200746120-00003. [DOI] [PubMed] [Google Scholar]
- 81.Wong W.T., Choi G., Gomersall C.D., Lipman J. To increase or decrease dosage of antimicrobials in septic patients during continuous renal replacement therapy: the eternal doubt. Curr Opin Pharmacol. 2015;24:68–78. doi: 10.1016/j.coph.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 82.Lewis S.J., Mueller B.A. Antibiotic dosing in patients with acute kidney injury: “enough but not too much”. J Intensive Care Med. 2016;31(3):164–176. doi: 10.1177/0885066614555490. [DOI] [PubMed] [Google Scholar]
- 83.Macias W.L., Alaka K.J., Murphy M.H., Miller M.E., Clark W.R., Mueller B.A. Impact of the nutritional regimen on protein catabolism and nitrogen balance in patients with acute renal failure. JPEN J Parenter Enteral Nutr. 1996;20(1):56–62. doi: 10.1177/014860719602000156. [DOI] [PubMed] [Google Scholar]
- 84.McClave S.A., Taylor B.E., Martindale R.G. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) JPEN J Parenter Enteral Nutr. 2016;40(2):159–211. doi: 10.1177/0148607115621863. [DOI] [PubMed] [Google Scholar]
- 85.Ebo D.G., Bosmans J.L., Couttenye M.M., Stevens W.J. Haemodialysis-associated anaphylactic and anaphylactoid reactions. Allergy. 2006;61(2):211–220. doi: 10.1111/j.1398-9995.2006.00982.x. [DOI] [PubMed] [Google Scholar]
- 86.Krieter D.H., Grude M., Lemke H.D. Anaphylactoid reactions during hemodialysis in sheep are ACE inhibitor dose-dependent and mediated by bradykinin. Kidney Int. 1998;53(4):1026–1035. doi: 10.1111/j.1523-1755.1998.00837.x. [DOI] [PubMed] [Google Scholar]
- 87.Troyanov S., Geadah D., Ghannoum M., Cardinal J., Leblanc M. Phosphate addition to hemodiafiltration solutions during continuous renal replacement therapy. Intensive Care Med. 2004;30(8):1662–1665. doi: 10.1007/s00134-004-2333-2. [DOI] [PubMed] [Google Scholar]
- 88.Culley C.M., Bernardo J.F., Gross P.R. Implementing a standardized safety procedure for continuous renal replacement therapy solutions. Am J Health Syst Pharm. 2006;63(8):756–763. doi: 10.2146/ajhp050402. [DOI] [PubMed] [Google Scholar]
- 89.Akhoundi A., Singh B., Vela M. Incidence of adverse events during continuous renal replacement therapy. Blood Purif. 2015;39(4):333–339. doi: 10.1159/000380903. [DOI] [PubMed] [Google Scholar]
- 90.Sigwalt F., Bouteleux A., Dambricourt F., Asselborn T., Moriceau F., Rimmele T. Clinical complications of continuous renal replacement therapy. Contrib Nephrol. 2018;194:109–117. doi: 10.1159/000485608. [DOI] [PubMed] [Google Scholar]
- 91.Fernandez S., Santiago M.J., Gonzalez R. Hemodynamic impact of the connection to continuous renal replacement therapy in critically ill children. Pediatr Nephrol. 2018 doi: 10.1007/s00467-018-4047-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schytz P.A., Mace M.L., Soja A.M. Impact of extracorporeal blood flow rate on blood pressure, pulse rate and cardiac output during haemodialysis. Nephrol Dial Transplant. 2015;30(12):2075–2079. doi: 10.1093/ndt/gfv316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sherman R.A. We lower blood flow for intradialytic hypotension. Semin Dial. 2016;29(4):295–296. doi: 10.1111/sdi.12486. [DOI] [PubMed] [Google Scholar]
- 94.Gibney N., Hoste E., Burdmann E.A. Timing of initiation and discontinuation of renal replacement therapy in AKI: unanswered key questions. Clin J Am Soc Nephrol. 2008;3(3):876–880. doi: 10.2215/CJN.04871107. [DOI] [PubMed] [Google Scholar]
- 95.Gibney R.T.N., Bagshaw S.M., Kutsogiannis D.J., Johnston C. When should renal replacement therapy for acute kidney injury be initiated and discontinued? Blood Purification. 2008;26(5):473–484. doi: 10.1159/000157325. [DOI] [PubMed] [Google Scholar]
- 96.Uchino S., Bellomo R., Morimatsu H. Discontinuation of continuous renal replacement therapy: a post hoc analysis of a prospective multicenter observational study. Crit Care Med. 2009;37(9):2576–2582. doi: 10.1097/CCM.0b013e3181a38241. [DOI] [PubMed] [Google Scholar]
- 97.Mendu M.L., Ciociolo G.R., McLaughlin S.R. A Decision-making algorithm for initiation and discontinuation of RRT in severe AKI. Clin J Am Soc Nephrol. 2017;12(2):228–236. doi: 10.2215/CJN.07170716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bosslet G.T., Pope T.M., Rubenfeld G.D. An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med. 2015;191(11):1318–1330. doi: 10.1164/rccm.201505-0924ST. [DOI] [PubMed] [Google Scholar]
- 99.Okon T.R., Vats H.S., Dart R.A. Palliative medicine referral in patients undergoing continuous renal replacement therapy for acute kidney injury. Ren Fail. 2011;33(7):707–717. doi: 10.3109/0886022X.2011.589946. [DOI] [PubMed] [Google Scholar]
- 100.Scherer J.S., Holley J.L. The Role of time-limited trials in dialysis decision making in critically ill patients. Clin J Am Soc Nephrol. 2016;11(2):344–353. doi: 10.2215/CJN.03550315. [DOI] [PMC free article] [PubMed] [Google Scholar]