Abstract
The ethno-botanical documentation among ethnic people in Sathyamangalam wildlife sanctuary, Tamil Nadu, India has been investigated for the first time. A total of 61 medicinal plants having new combination uses were reported with adjuvant in the treatment of dermatological, Genitourinary and gastrointestinal ailments. This study could help in the recovery and conservation of traditional medicine system among educated generation. The present study was aimed to: (1) documentation of the traditional knowledge (2) quantitative analysis using Use value (UV), Informant consensus factor (ICF), Index of agreement on remedies (IAR), Relative frequency citation (RFC) and Cultural Importance index (CII) (3) validation of ethno-botanical data using in silico biological activity and toxicity prediction studies. Semi-structured direct interviews were conducted to acquire information from the study area tribes. Total of 89 tribes including both gender among various communities were interviewed and their ethno-botanical knowledge was documented. The data were assessed using ethno-botanical indices methods to estimate the consistency of usage herbal knowledge in various ailments. A total of 61 species were recorded for treatment of categorized ailments. The collected medicinal information from ethnic groups shows remarkable new usage of medicinal plants to particular ailments. Our comparative in silico studies also supported the traditional medicine results with correspondence to their bioactive. Traditional knowledge of ethnic people also linked to their culture and history. This study also infers the usage of traditional plant based medicine. Further research related to the bioactivities of reported plants should be encouraged to explore the importance in pharmaceutical industry.
Keywords: Ailments, Documentation, In silico, Quantitative indices, Traditional knowledge
Graphical abstract
1. Introduction
Indigenous knowledge is the neighbourhood information acquired by indigenous groups that is exceptional to an ethnic society. The scientific investigation and documentation of indigenous knowledge of plant resources are vital strategy to understand traditional life style of local ethnic people.1 The traditional herbal formulations from indigenous knowledge were considered as the oldest and great health care system. It includes plant species as regular medicine sources and still is an important system of healthcare in India.2 Common plants with adverse effects are being a part of our daily life and their toxic metabolites are closely related in the aspect of human's health condition.3 Traditional people are using poisonous plants either processed or as raw form over a period of time for treating diseases.4
The increasing interest in ethno-botanical studies also reveals their importance of traditional medicinal plants in various countries for local living holds and the important role these play in health care system.2,5 The impact of traditionally formulated medicines from various ancient systems in the communal health condition in India is considerably elevated and is closely associated with traditions.6 Various patented drugs and active compounds from various plant sources are also on the basis of ethno-botanical data.7
The ethno-botanical data analyzed with quantitative indices is assumed to expose the usage and value of the medicinal plants from ethnic knowledge. These approaches measure the consent of the usage by various hypotheses and playing an important role in the further selection of biomedical analysis of a medicinal plant to treat particular ailment based on the survey results with excellent information.8 Now days, In silico studies are one of the main emerging studies with the ability to predict the drug-protein interaction which relates the mechanism of action of a bioactive compounds mainly from traditional medicinal plants.9
So, there is an urgent requirement to document all ethno-botanical data as much as possible and the role of tribes in conserving them. Considering the importance of indigenous medicinal plant knowledge, this study aimed to identify potential medicinal plants and to evaluate in silico toxicological potential and biological activity of its major compounds responsible for medicinal activity.
2. Materials and methods
2.1. Study area tribal people
Sathyamangalam wildlife sanctuary located in the Nilgiri biosphere reserve covers about 1411.6 km2 (545.0 sq mi) forest area along the Western Ghats in Tamil Nadu, India (Fig. 1). This forest is mostly tropical dry forest and restricted to undersized high altitude hill tops between 750 and 1649 m above mean sea level and the slopes and plains are subjected to the average minimum and maximum temperatures of 21–27 °C with two persistent rivers namely Bhavani and Moyar. Uralis are the main ethnic group to this forest with some minor groups includes Soliga, Malayalee and Naicker communities.
Fig. 1.
Study area.
2.2. Data collection
The field surveys were conducted between May 2015 and September 2016 in proposed study area and various ethnic community people were randomly interviewed after verbally requested about the purpose of the project in the local language. In this study, 89 informants including traditional herbalist and local people were interviewed and their knowledge on medicinal plants was gathered and documented mostly by Tamil and sometime the Urali language was translated to Tamil using local translator.
2.3. Botanical identification
The collected plants were identified with help of pertinent literature and also authenticated by comparing the species deposited in Madras Herbarium (Botanical Survey of India, Coimbatore). The processed specimens were mounted on herbarium sheets using standard procedures and were deposited for future reference at the Department Herbarium of Bharathiar University.
2.4. Ethno-medicinal data analysis
The recorded data were tabulated using Microsoft Excel and then analyzed with various ethno-botanical reports such as research and review articles, books, in scientific databases to find out the uses of unknown or well-known medicinal plants. The ethno-medicinal quantitative indices were used for interpreting this entire information.
Use reports were calculated by converting collected data with reference to the previous published articles related to quantitative ethno-botanical surveys. These use-reports about medicinal plants were then grouped into 14 ailments categories based on the collected ethno-botanical details from informants. These data were assessed with quantitative indices, such as Informant consensus factor, Fidelity level, Frequency citation and Use value, were calculated from the gathered information. The new medicinal uses from the study area are identified by comparing previous reports on the particular area and related regions of south India.
2.4.1. Informant consensus factor (ICF)
ICF was calculated to highlight the usage of the relevant plants among various informants for each aliments category. The ICF value was calculated by minus the total use citations in each category (Nur) with the total number of species used (nt), divided by the total number of use citations minus one as follows:
The ICF value of approach to 0 indicates that the informants randomly use the species in the treatment of various ailments, and a value of approach to 1 indicates that relatively usage of the species by a large population to a particular ailment.10
2.4.2. Fidelity level (FL) and index of agreement on remedies (IAR)
The importance of each species in the treatment of particular illness group was determined by FL and IAR values. A high ratio indicates common use of the ideal plant species for treating specific ailment in the studied area.11 The fidelity level was calculated as follows:
The FL is the ratio of number of informants who suggesting the plant as medicine for a particular ailment category (Np) and total number of informants who suggesting the plant for any ailment category (N).
Where, Nr is the total number of citations registered for a particular species and Na is the number of illness categories that are treated with this species.
2.4.3. Frequency citation (FC) and relative frequency citation (RFC)
The relative expression of usage (FC) is calculated as follows:
| FC = (Number of times a particular species was mentioned/total number of times that all species were mentioned) × 100 |
The RFC value was obtained by dividing the FC by the total number of informants interviewed (N) and not based on used categories. When the RFC value will be approach to zero, it refers, nobody suggests the plants as useful, and when its approach to one, it refers that every informant would suggest as useful and the RFC was calculated as follows:12
2.4.4. Use value (UV) and Cultural importance index (CII)
The importance of each plant species among ethnic people was determined by UV and CII.12 Based on, the vast usage of a particular ethnically important medicinal plant species was identified using CII value. The use value of a species (UV) is the summation of the number of use reports for the specific plant species (U) and is divided by the total number of informants (N) interviewed. If the use value is high, it indicates the many use reports and important of the plant, and low value indicates the fewer use reports. These were calculated as follows
Where NC is the total number of different illness categories for each species, UR is the total number of use citations for each species, and N is the number of informant's interviewed. The ethno-botanical indices such as ICF, UV, RFC and FL could be used to determine the consent individual species in the treatment of an ailment category in a population.
2.5. In silico pharmacological activity and toxicity prediction
The present study employed online based computational bioactive screening (PASS) to obtain biological effects and relationship for compounds which are previously reported on plants major ethno-botanical uses in the study area.13 The details about the compounds including structure, SMILES and molecular formula were obtained from ACS Chemspider. Probable activity (Pa) and inactivity (Pi) percentages (ranges from 0.000 to 1.000) were used to express the prediction results. Thus, in this study the higher Pa value (>0.900) and lower Pi value indicates higher activity. The adsorption, distribution and toxicity of the listed compounds were predicted by using admetSAR online prediction tool.
3. Results
3.1. Demographical description and documentation of ethno-botanical data
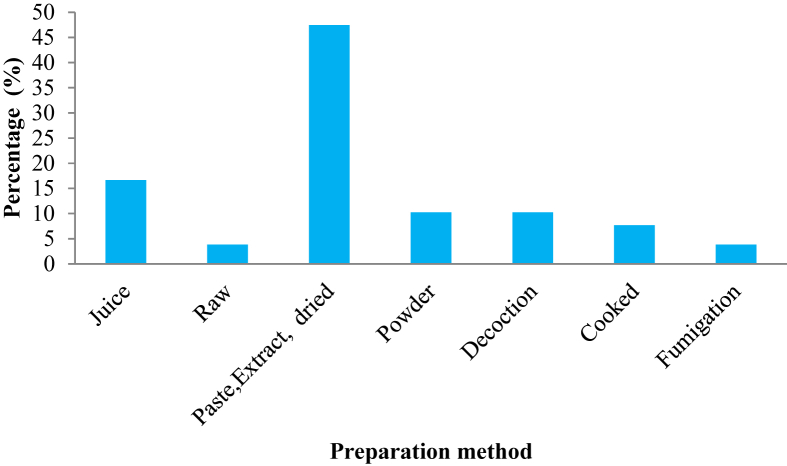
The ethnic people population was found limited in the study area, 89 of informants including male (58) and female (31) of various different age groups (ranges from 31 to 80 years) including 6 herbalists age ranges between 40 and 60 years belonging to the local communities were interrogated (Table 1). The collected data was divided and tabulated according to the corresponding 55 bio-medical symptoms into 14 major ailment categories (Table 2, Table 3) respectively to the local term used. When compared to all major ailments categories gastrointestinal ailments had reported with high number of citations (375 citations of 22 plants) which was followed by dermatological (333 citations of 19 plants) and genitourinary ailments category (222 citations of 9 plants) respectively (Table 3). The gastrointestinal (36%) and dermatological ailment category (31%) (Fig. 2) were cited as most treating ailments in the survey. A total of 61 plants species and 54 genera distributed over 23 families with various beneficial effects cited in the present study, particularly 15% of Fabaceae and 10% of Rutaceae (Fig. 3). The usage of different parts of medicinal plant used in traditional medicine were calculated in percentage, among various parts used the leaf showed highest (51%), followed by seeds, fruit, stem and rhizome (ranges between 15 and 16%), and finally flowers (3%) with the lowest among all parts used (Fig. 4). In the studied area there were two modes are normally prescribed for administration either oral or topical in various forms such as juice, paste, cooked, decoction, etc. The paste preparation method (including extract and dried form) is the most used preparation method (47%) followed by powder and decoction (Juice) is ranges between 10 and 17% (Fig. 5).
Table 1.
Demographic representation of informants by age group in Sathyamangalam wildlife sanctuary, India.
| Age group of informants (In years) | Local people |
Herbalists | |
|---|---|---|---|
| Male (58) | Female (31) | ||
| 31–40 | 28 | 16 | |
| 41–50 | 15 | 5 | 4 |
| 51–60 | 9 | 8 | 2 |
| 61–70 | 4 | 2 | |
| 71–80 | 2 | ||
Table 2.
List of ailments category with its corresponding tamil terms used by the tribes in Sathyamangalam wildlife sanctuary, Tamil Nadu, India.
| S. No | Ailment category and Biomedical terms | Tamil terms |
|---|---|---|
| 1 | Circulatory system ailments | |
| Anemia | Raththa soagai | |
| Heart problem | Idhaya pirachanai | |
| Cardio tonic | Idhaya valimai | |
| Blood tonic | Raththa perukki | |
| 2 | Dermatological ailments | |
| Burns | Theekkaayam | |
| Itch | Namaichaal | |
| Wounds | Kaayam | |
| Rash | Sori | |
| Inflammation | Udaleritchal | |
| Skin disease | Tholnoikal | |
| Mouth ulcer | Vaaippun | |
| Leprosy | Thoalunoi | |
| Skin lotion | Sarumamarunthu | |
| Bacterial and fungal diseases | Thotrunoi | |
| 3 | Ear, nose, throat ailments | |
| Gums ache | Eeralvali | |
| Earache | Kathu vali | |
| 4 | Eye ailments | |
| Eye diseases | Kannoikal | |
| 5 | Endocrinal ailments | |
| Diabetes | Sakkara/Neerilivunoi | |
| 6 | Fever ailments | |
| Fever | Kaaichal | |
| 7 | Gastrointestinal ailments | |
| Dysentery | Vayitrupoakku | |
| Indigestion | Ajeeranam | |
| Vomiting | Vaandhi | |
| Stomach ache | Vayitruvali | |
| Stomach ulcer | Vayitrupun | |
| Abdominal pain | Adi Vayitruvali | |
| Digestion disorders | Jeeranam kolarugal | |
| Gas trouble | Vaaivuthoandharuvu | |
| Intestinal disorders | Kudalkoalaarugal | |
| Diahhroea | Neerpokku | |
| 8 | Genitourinary ailments | |
| Bladder infection | Siruneerppaithotru | |
| Diuretic | Siruneerperukki | |
| Urinary disorders | Siruneerkoalaarugal | |
| Kidney stone | Siruneer kalladappu | |
| Leucorrhoea | Vellaipaduthal | |
| Venereal diseases | Paalvinainoikal | |
| Jaundice | Manjalkaamalai | |
| Liver diseases | Kalleeralnoikal | |
| Abortion | Karukallaipu | |
| 9 | Hemorrhoids ailments | |
| Piles | Moolam | |
| 10 | Neurology ailments | |
| Headache | Thalaivali | |
| 11 | Oncology ailments | |
| Cancer | Katti | |
| 12 | Poisonous bites ailments | |
| Snake bite | Paambu kadi | |
| Scorpion sting | Thel kadi | |
| 13 | Respiratory ailments | |
| Asthma | Kaasa noi | |
| Cold | Sali | |
| Cough | Irumal | |
| Breathing problem | Moochu thinaral | |
| Small pox | Sitrammai | |
| 14 | Skeletal muscular ailments | |
| Edema | Neer veekkam | |
| Joint pain | Moodu vali | |
| Body pain | Udal vali | |
| Rheumatism/Gout | Keel vaadham | |
| Swelling | Veekam | |
| Muscle pain | Thasai pidippu | |
| Arthritis | Moodu vali | |
| Paralyze | Mudakkuvadm |
Table 3.
Results obtained from informants belongs to Sathyamangalam wild life sanctuary, Tamil Nadu, India.
| S. No | Family/ Binomial name | Vernacular name | Parts Useda | Method of preparation | Ailments treated | Administration routeb | Total number of citation | UV | IAR | FC (%) | RFC |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
Annonaceae Annona squamosa L. |
Seetha maram | L F |
Juice Raw |
Diabetes (14) Abortion (30) |
O | 44 | 0.49 | 0.98 | 49.44 | 0.56 |
| 2 |
Asteraceae Spilanthes calva Wt. |
Vettumarunthuchedi | L | Paste | Wound (20) | T | 20 | 0.22 | 1 | 22.47 | 0.25 |
| 3 | Spilanthes acmella Murr. | Manjapoochedi | F | Paste | Gums ache (7) | T | 7 | 0.08 | 1 | 7.87 | 0.09 |
| 4 | Tridax procumbens L. | Mookuthhichedi | L | Juice, Paste |
Wound (9) | O | 9 | 0.10 | 1 | 10.11 | 0.11 |
| 5 | Eclipta prostrata (L.) | Karisilanganni | S, L, Wp |
Dried Powder |
Head ache (6) Abdominal pain (13) Jaundice (9) | T/O | 28 | 0.31 | 0.93 | 31.46 | 0.35 |
| 6 |
Fabaceae Abrus precatorius L. |
Kundumani | Se, L | Decoction Powder Juice Paste Extract |
Stomach ulcer (25) Abortion (20) Dystenry (6) Mouth ulcer (10) Cancer (8) Bacterial fungal infections (2) |
O | 71 | 0.80 | 0.96 | 79.78 | 0.90 |
| 7 | Bauhinia divaricata L. | Aathi | L | Fumigation | Fever (15) Asthma (9) |
I | 24 | 0.27 | 0.96 | 26.97 | 0.30 |
| 8 | Bauhinia tomentosa L. | Aathi | B | Paste | Diahorrea (21) | O | 21 | 0.24 | 1 | 23.60 | 0.27 |
| 9 | Prosopis juliflora (Sw.) DC. | Vannimaram | L, B | Juice Paste |
Snake bite (16) | O/T | 16 | 0.18 | 1 | 17.98 | 0.20 |
| 10 | Pongamia pinnata (L.) Pierre | Pungamaram | Fl | Dried | Abdominal pain (3) Gas trouble (6) Snake bite (6) Diabetes (8) | O | 23 | 0.26 | 0.91 | 25.84 | 0.29 |
| 11 | Canavalia cathartica Thouars | Isaakottai | L | Paste | Body pain (5) Muscle pain (4) | T | 9 | 0.10 | 1 | 10.11 | 0.11 |
| 12 | Tephrosia purpurea (L.) Pers. | Kolinjii | R | Powder | Fever (5) Indigestion (4) |
O | 9 | 0.10 | 0.88 | 10.11 | 0.11 |
| 13 | Clitoria ternatea L. | Sangupushpam | L | Juice | Dysentery (28) Indigestion (7) | O | 35 | 0.39 | 1 | 39.33 | 0.44 |
| 14 | Sesbania grandiflora (L.) Poir. | Agathimaram | L | Cooked | Indigestion (10) Dysentery (25) Eye diseases (8) |
O | 43 | 0.48 | 0.98 | 48.31 | 0.54 |
| 15 |
Apocyanaceae Plumaria alba L. |
Ezhakalari | B, R | Paste Decoction | Cancer (12) Venereal diseases (9) Urinary disorders (20) |
O | 41 | 0.46 | 0.98 | 46.07 | 0.52 |
| 16 | Rauvolfia serpentina (L.) Benth. ex Kurz | Sarpaganthi | L | Juice | Heart problem (5) Cardio tonic (9) | O | 14 | 0.16 | 1 | 15.73 | 0.18 |
| 17 | Wrightia tinctoria R.Br. | Pallayamaram | B | Paste | Itch (5) Rash (3) Wounds (10) |
T | 18 | 0.20 | 1 | 20.22 | 0.23 |
| 18 |
Rutaceae Aegle marmelos (L.) Correa |
Vilvam | F, L, B | Raw Juice Decoction Paste |
Fever (20) Cold (13) Fever (6) Blood tonic (8) Cancer (10) |
O | 57 | 0.64 | 0.95 | 64.04 | 0.72 |
| 19 | Citrus aurantiifolia (Christm.) Swingle | Elumiccai | F | Raw | Stomach ache (29) Blood tonic (20) | O | 49 | 0.55 | 0.98 | 55.06 | 0.62 |
| 20 | Citrus limon (L.) Osbeck | Kiccilippalam | L, F | Decoction Raw |
Indigestion (20) Vomiting (13) | O | 33 | 0.37 | 1 | 37.08 | 0.42 |
| 21 | Toddalia asiatica Lamk. | Masihachedi | B | Paste | Paralyze (15) | O/T | 15 | 0.17 | 1 | 16.85 | 0.19 |
| 22 | Murraya paniculata (L.) Jack | Sedisil maram | L | Paste | Wounds (20) | T | 20 | 0.22 | 1 | 22.47 | 0.25 |
| 23 | Glycosmis pentaphylla (Retz.) DC. | Molehulukki | R | Paste | Asthma (15) | O | 15 | 0.17 | 1 | 16.85 | 0.19 |
| 24 |
Lamiaceae Vitex negundo L. |
Nochi | L | Juice | Joint pain (26) Head ache (13) |
O | 39 | 0.44 | 0.97 | 43.82 | 0.49 |
| 25 | Ocimum basilicum L. | Thiruneetrupachhai | L | Fumigation | Asthma (25) | I | 25 | 0.28 | 1 | 28.09 | 0.32 |
| 26 | Leucas aspera (Willd.) Link | Thumbai | Wp | Fumigation | Head ache (20) | I | 20 | 0.22 | 1 | 22.47 | 0.25 |
| 27 | EuphorbiaceaeEuphorbia hirta L. | Ammaan pachcharsi | Wp | Powder | Leucorrhoea (28) | O | 28 | 0.31 | 1 | 31.46 | 0.35 |
| 28 | Euphorbia nivulia Buch.-Ham. | Illaikanni | L | Juice | Ear ache (14) | T | 14 | 0.16 | 1 | 15.73 | 0.18 |
| 29 | Jatroba curcas L. | Kattaamankku | B | Decoction | Stomach ache (19) | O | 19 | 0.21 | 1 | 21.35 | 0.24 |
| 30 | Phyllanthus amarus L. | Keeva nelly | R, F | Juice | Liver problems (34) | O | 34 | 0.38 | 1 | 38.20 | 0.43 |
| 31 | Acalypha indica L. | Kuppaimeni | L | Paste | Burns (10) Itch (27) Skin lotion (9) Bacterial and fungal diseases (11) Edema (18) |
T | 65 | 0.73 | 0.98 | 73.03 | 0.82 |
| 32 | AsclepiadaceaeCalotropis gigantea (L.) Dryand. | Vellai erukku | R | Paste | Rash (20) Edema (17) |
T | 37 | 0.42 | 0.97 | 41.57 | 0.47 |
| 33 | Calotropis procera (Aiton) Dryand. | Erukku | L | Paste | Skin diseases (30) | T | 30 | 0.34 | 1 | 33.71 | 0.38 |
| 34 | Hemidesmus indicus (L.) R. Br. ex Schult. | Nannari | L R |
Decoction | Head ache (20) Stomach disorders (20) |
I/O | 40 | 0.45 | 0.97 | 44.94 | 0.50 |
| 35 | Pergularia daemia (Forssk.) Chiov. | Vellyparuthi | L | Decoction | Head ache (20) | I | 20 | 0.22 | 1 | 22.47 | 0.25 |
| 36 |
Solanaceae Solanum xanthocarpum Schrad |
Kandangkathhiri | F L |
Cooked Paste |
Intestinal disorders (10) Small pox (23) |
O/T | 33 | 0.37 | 0.97 | 37.08 | 0.42 |
| 37 | Solanum nigrum L. | Chukuti chedi | L F |
Cooked | Mouth ulcer (12) Intestinal disorders (19) | O | 31 | 0.35 | 0.97 | 34.83 | 0.39 |
| 38 | Solanum indicum L. | Mullu chundal | F | Cooked | Intestinal disorders (12) | O | 12 | 0.13 | 1 | 13.48 | 0.15 |
| 39 | Datura metal L. | Oomathai | L | Paste | Joint pain (14) Rheumatism/Gout (15) | T | 29 | 0.33 | 1 | 32.58 | 0.37 |
| 40 |
Malvaceae Sida acuta Burn. |
Kala karandai | L | Paste | Skin disease (23) Burns (10) Wounds (12) |
T | 45 | 0.51 | 1 | 50.56 | 0.57 |
| 41 | Abutilon indicum (L.) Sweet | Thuthi | Wp, L | Cooked Paste |
Piles (10) Inflammation (15) Dysentery (9) | O | 34 | 0.38 | 0.94 | 38.20 | 0.43 |
| 42 | AcanthaceaeAndrographis paniculata (Burm.f.) Nees | Periya nangai | L | Paste Juice |
Joint pain/ Rheumatism (12) Gout (5) Swelling (4) Arthritis (8) Leprosy (8) Indigestion (10) |
O/T | 47 | 0.53 | 0.96 | 52.81 | 0.59 |
| 43 | Justicia adhatoda L. | Adathodai | L | Decoction | Cold (9) Cough (10) Breathing problem (7) |
O | 26 | 0.29 | 1 | 29.21 | 0.33 |
| 44 | Ruellia patula Jacq. | Puni chedi | L | Paste | Fever (10) | T | 10 | 0.11 | 1 | 11.24 | 0.13 |
| 45 |
Pedaliaceae Sesamum indicum L. |
Ellu | Se, L | Powder Paste | Abortion (30) Diuretic (13) Wound (8) |
O/T | 51 | 0.57 | 0.98 | 57.30 | 0.64 |
| 46 |
Myrtaceae Psidium guajava L. |
Koyyamaram | L | Paste | Indigestion (11) | O | 11 | 0.12 | 1 | 12.36 | 0.14 |
| 47 | Syzygium cumini L. | Navalmaram | F, L | Powder | Diabetes (20) | O | 20 | 0.22 | 1 | 22.47 | 0.25 |
| 48 |
Oxalidaceae Oxalis corniculata L. |
Pulichikeerai | L, R | Cooked Paste |
Blood tonic (10) Fever (10) | O | 20 | 0.22 | 0.95 | 22.47 | 0.25 |
| 49 | NyctaginaceaeBoerhavia diffusa L. | Saranda kodi | Wp | Paste | Digestive disorder (9) Urinary tract infection (11) Bladder infection (6) |
O | 26 | 0.29 | 0.96 | 29.21 | 0.33 |
| 50 |
Convolvulaceae Ipomea obscura (L.) Ker.-Gawl |
Shiruttallai | Sl | Juice | Wound (6) Fever (5) |
T | 11 | 0.12 | 0.9 | 12.36 | 0.14 |
| 51 | Evolvulus alsinoides L. | Vishnukarandai | L | Paste | Burn (6) Wound (8) |
T | 14 | 0.16 | 1 | 15.73 | 0.18 |
| 52 | Rivea hypocrateriformis (Desr.) Choisy | Minna chedi | L | Cooked | Indigestion (7) | O | 7 | 0.08 | 1 | 7.87 | 0.09 |
| 53 |
Rubiaceae Haldina cordifolia (Roxb.) Ridsdale |
Manja Kadambai | B | Paste | Anemia (8) Urinary disorders (12) |
O | 20 | 0.22 | 0.95 | 22.47 | 0.25 |
| 54 | Rubia cordifolia L. | Chevvali kodi | L | Paste | Scorpion sting (9) | T | 9 | 0.10 | 1 | 10.11 | 0.11 |
| 55 |
Oleaceae Jasminum angustifolium (L.) Willd. |
Kattu malligai | L | Juice | Diahrroea (8) | O | 8 | 0.09 | 1 | 8.99 | 0.10 |
| 56 |
Poaceae Saccharum officinarum L. |
Karumppu | S | Juice | Rash (5) | T | 5 | 0.06 | 1 | 5.62 | 0.06 |
| 57 |
Mimosoideae Acacia nilotica (L.) Delile |
Karuvelam | L | Paste | Wound (6) Piles (3) Cough (5) |
O/T | 13 | 0.15 | 0.83 | 14.61 | 0.16 |
| 58 | MenispermaceaeCocculus hirsutus (L.) Diels | Kattukodi | L | Paste | Blood tonic (6) Piles (4) Dysentery (8) Diabetes (2) |
O | 20 | 0.22 | 0.84 | 22.47 | 0.25 |
| 59 | Tinospora sinensis (Lour.) Merr. | Seenthal kodi | L | Powder | Burn (10) Edema (12) |
T | 22 | 0.25 | 0.95 | 24.72 | 0.28 |
| 60 |
Zingiberaceae Zingiber officinale Roscoe |
Injii | Rh | Paste Powder |
Head ache (6) Abdominal pain (10) Gums ache (11) Digestive disorder (6) Indigestion (7) |
T/O | 40 | 0.45 | 0.92 | 44.94 | 0.50 |
| 61 | SapindaceaeCardiospermum halicacabum L. | Thatu putu chedi | L | Paste | Joint pain (8) Arthritis (10) Asthma (12) Swelling (4) Burn (8) Body pain (12) |
T/O | 54 | 0.61 | 0.96 | 60.67 | 0.68 |
B- bark, L-leaf, S-stem, Se-seed, Fl-flower, F-fruit, R-root, Rh-rhizome, Wp-whole plant, Sl-stem latex.
O- oral, T-topical, I- inhalation.
Fig. 2.
Ailment percentages of reported ethno-botanical data.
Fig. 3.
Family diversity of reported ethno-botanical data.
Fig. 4.
Usage percentages of different parts.
Fig. 5.
Common preparation methods of medicinal plants.
3.2. Quantitative analysis of ethno-botanical indices
Plants with 20 or more than citations were considered as frequently cited plants and indicated by RFC which was ranges from 0.09 to 0.90 (Table 3). These plants can be explained by their reliable medicinal source among informants of studied area. In the present study, the highest number of citations was for Abrus precatorius L. (71 citations with RFC 0.90) used in the treatment of gastrointestinal, dermatological and oncological ailments, followed by Acalypha indica L. (65 citations with RFC 0.82) and Aegle marmelos (L.) Correa (57 citations with RFC 0.72). The higher RFC indicates the more citation (at least 40 out of 89 interviewed informants) and implies the most common medicinal plants among the tribes of Sathyamangalam wildlife sanctuary. The relative use of particular medicinal plant for treating an ailment category was highlighted by ICF value. Based on the calculated ICF values (ranges from 0.88 to 1.00) the ailments are further categorized into Higher, Moderate and Lower ICF value ailments. The eye ailment category shows highest ICF value (1.00) with 8 reports of 1 species and genitourinary (0.96), skeletal-muscular (0.96), gastrointestinal (0.96) and dermatological (0.95) ailments are also categorized as high ICF value ailments category. The moderate and lowest ICF values were observed for diseases of the circulatory system ailments (0.92) followed by Hemorrhoids ailments (0.88) (Table 4). This high value indicates the homogeneity of ethno-medicinal knowledge between the informants. Medicinally significant plant was determined by FL it was calculated for the entire ailment category and tabulated (Table 4). Hemorrhoids, oncology and eye ailments are reported as categories consists lower FL (<<50) than other ailments. Among 14 listed ailment categories 11 ailments at least have one plant had the highest FL (100%) particularly dermatological and gastrointestinal ailments were reported with high number of FL 100% plants (8 respectively). The individual with most use-reports was considered as common medicine for a particular ailment treatment. Based on the use-reports collected from ethnic people CII, UV and IAR indices were calculated to highlight the usage priority, importance, recommendation and sharing medicinal knowledge about the particular species among the informants. In this study Abrus precatorius L. (CII-3.191, UV-0.80, IAR-0.96), Aegle marmelos (L.) Correa (CII-2.562, UV-0.64, IAR-0.95), Cardiospermum halicacabum L. (CII-1.820, UV-0.61, IAR-0.96), Andrographis paniculata (Burm.f.) Nees (CII-1.584, UV-0.53, IAR-0.96), Zingiber officinale Roscoe (CII-1.348, UV-0.45, IAR-0.92) and Acalypha indica L. (CII-1.461, UV-0.73, IAR-0.98) were showed commendable values this indicates the importance of the species among the studied area tribes (Table 3, Table 4). Among 61 recorded medicinal plants from the studied area, 19 plants revealed new use reports which were identified by comparing previous reported literature (Table 5). The local names of the cited plants were almost same among all community in the study area indicates the homogeneity and relevance of particular individual species in herbal medicine.
Table 4.
ICF value for the illness category and FL and CII values for the reported plants in Sathyamangalam wildlife sanctuary, Tamil Nadu, India.
| S. No | Illness category | Number of citation (Nur) |
Number of species cited (Nt) |
ICF | FL% and CII |
|---|---|---|---|---|---|
| Illness with High ICF value | |||||
| 1 | Eye ailments | 8 | 1 | 1.00 | Sesbania grandiflora (L.) Pers. (19/0.966) |
| 2 | Genitourinary ailments | 222 | 9 | 0.96 | Haldina cordifolia (Roxb.) Ridsdale (60/0.449) Boerhavia diffusa L. (65/0.584) Sesamum indicum L. (84/1.146a) Phyllanthus amarus Schumach. & Thonn. (100/0.382) Euphorbia hirta L. (100/0.315) Plumaria alba L. (71/0.921) Abrus precatorius L. (28/3.191a) Annona squamosa L. (68/0.989a) Eclipta prostrata (L.) L. (32/0.944) |
| 3 | Skeletal muscular ailments | 179 | 9 | 0.96 | Cardiospermum helicacabum L. (63/1.820a) Tinospora sinensis (Lour.) Merr. (55/0.494) Andrographis paniculata (Burm.f.) Nees (62/1.584a) Datura metel L. (100/0.326) Calotropis gigantea (L.) Dryand. (46/0.831a) Acalypha indica L. (28/1.461) Vitex negundo L. (67/0.876a) Toddalia asiatica (L.) Lam. (100/0.169) Canavalia cathartica Thouars (100/0.101) |
| 4 | Dermatological ailments | 333 | 19 | 0.95 | Spilanthes calva DC. (100/0.225) Tridax procumbens (L.) L. (100/0.101) Abrus precatorius L. (17/3.191) Wrightia tinctoria R.Br. (100/0.202) Murraya paniculata (L.) Jack (100/0.225) Acalypha indica L. (88/1.461a) Calotropis gigantea (L.) Dryand. (54/0.831a) Calotropis procera (Aiton) Dryand. (100/0.337) Solanum nigrum L. (39/0.697) Sida acuta Burm.f. (100/0.506) Abutilon indicum (L.) Sweet (43/1.146) Andrographis paniculata (Burm.f.) Nees (17/1.584) Sesamum indicum L. (16/1.146) Ipomoea obscura (L.) Ker Gawl. (55/0.247) Evolvulus alsinoides (L.) L. (100/0.157) Saccharum officinarum L. (100/0.056) Acacia nilotica (L.) Delile (46/0.438) Tinospora sinensis (Lour.) Merr. (45/0.494) Cardiospermum halicacabum L. (16/1.820) |
| Illness with moderate ICF value | |||||
| 5 | Ear, nose, throat ailments | 32 | 3 | 0.94 | Zingiber officinale Roscoe (28/1.348) Euphorbia nivulia Buch.-Ham. (100/0.157) Spilanthes acmella (L.) L. (100/0.079) |
| 6 | Neurology ailments | 85 | 6 | 0.94 | Zingiber officinale Roscoe (15/1.348) Hemidesmus indicus (L.) R. Br. ex Schult. (50/0.899) Pergularia daemia (Forssk.) Chiov. (100/0.225) Leucas aspera (Willd.) Link (100/0.225) Vitex negundo L. (33/0.876) Eclipta prostrata (L.) L. (21/0.944) |
| 7 | Gastrointestinal ailments | 375 | 22 | 0.94 | Eclipta prostrata (L.) L. (46/0.944a) Abrus precatorius L. (44/3.191a) Bauhinia tomentosa L. (100/0.236) Pongamia pinnata (L.) Pierre (39/0.775) Tephrosia purpurea (L.) Pers. (44/0.202) Clitoria ternatea L. (100/0.393) Sesbania grandiflora (L.) Pers. (81/0.966a) Citrus aurantiifolia (Christm.) Swingle (59/1.101) Citrus limon (L.) Osbeck (100/0.371) Jatropha curcas L. (100/0.213) Hemidesmus indicus (L.) R. Br. ex Schult. (50/0.899) Solanum xanthocarpum Schrad. & H. Wendl. (30/0.742) Solanum nigrum L. (61/0.697a) Solanum indicum L. (100/0.135) Abutilon indicum (L.) Sweet (26/1.146) Andrographis paniculata (Burm.f.) Nees (21/1.584) Psidium guajava L. (100/0.124) Boerhavia diffusa L. (35/0.584) Rivea hypocrateriformis Choisy (100/0.079) Jasminum angustifolium (L.) Willd. (100/0.090) Cocculus hirsutus (L.) W.Theob.(67/0.899a) Zingiber officinale Roscoe (58/1.348a) |
| 8 | Respiratory ailments | 179 | 9 | 0.94 | Bauhinia divaricata L. (38/0.539) Aegle marmelos (L.) Correa (23/2.562) Glycosmis pentaphylla (Retz.) DC. (100/0.169) Ocimum basilicum L. (100/0.281) Solanum xanthocarpum Schrad. & H. Wendl. (70/0.742a) Justicia adhatoda L. (100/0.292) Acacia nilotica (L.) Delile (38/0.438) Cardiospermum halicacabum L. (22/1.820) |
| 9 | Endocrinal ailments | 44 | 4 | 0.93 | Annona squamosa L. (47/0.989a) Pongamia pinnata (L.) Pierre (35/0.775) Syzygium cumini (L.) Skeels (100/0.225) (L.) Cocculus hirsutus (L.) W.Theob. (11/0.899) |
| 10 | Fever ailments | 71 | 6 | 0.93 | Ipomoea obscura (L.) Ker Gawl. (45/0.247) Oxalis corniculata L. (50/0.449) Ruellia patula Jacq. (100/0.112) Aegle marmelos (L.) Correa (46/2.562a) Tephrosia purpurea (L.) Pers. (56/0.202) Bauhinia divaricata L. (63/0.539) |
| 11 | Oncology ailments | 30 | 3 | 0.93 | Abrus precatorius L. (11/3.191) Plumaria alba L. (29/0.921) Aegle marmelos (L.) Correa (18/2.562) |
| 12 | Poisonous bites ailments | 31 | 3 | 0.93 | Rubia cordifolia L. (100/0.101) Pongamia pinnata (L.) Pierre (26/0.775) Prosopis juliflora (Sw.) DC. (100/0.180) |
| 13 | Circulatory system ailments | 66 | 6 | 0.92 | Cocculus hirsutus (L.) W.Theob. (43/0.899a) Haldina cordifolia (Roxb.) Ridsdale (60/0.449a) Oxalis corniculata L. (50/0.449) Citrus aurantiifolia (Christm.) Swingle (41/1.101a) Aegle marmelos (L.) Correa (14/2.562) Rauvolfia serpentina (L.) Benth. ex Kurz (100/0.157) |
| Illness with moderate ICF value | |||||
| 14 | Hemorrhoids ailments | 3 | 3 | 0.88 | Abutilon indicum (L.) Sweet (29/1.146) Acacia nilotica (L.) Delile (23/0.438) Cocculus hirsutus (L.) W.Theob. (25/0.899) |
Species were considered more consent to treat particular ailment ethno-botanically.
Table 5.
Plants with adverse effects from Sathyamangalam wild life sanctuary, Tamil Nadu, India.
| S. No | Binomial name | Adverse effect and interaction |
|---|---|---|
| 1 | Annona squamosa L. | The seed is poisonous. Consuming seed leads to abortion. Sometime used as rat poison |
| 2 | Tridax procumbens (L.) L. | Over dosage of leaves leads to ulcer effect. |
| 3 | Abrus precatorius L. | Consuming seeds leads to abortion, Hallucination, coma. Consult doctor after consuming |
| 4 | Prosopis juliflora (Sw.) DC. | Consumption of fruits of this plant leads to paralysis |
| 5 | Plumaria alba L. | Accidental contact of latex of this plant leads to severe skin irritation |
| 6 | Wrightia tinctoria R.Br. | Consuming seeds and latex causes ulcer |
| 7 | Aegle marmelos (L.) Correa | Over dosage leads to emetic condition |
| 8 | Vitex negundo L. | Over dosage leads to gastric disorders |
| 9 | Leucas aspera (Willd.) Link | Raw consumption will lead to abortion |
| 10 | Jatropha curcas L. | Seed consumption leads to neurotoxic effects |
| 11 | Calotropis spp. | The latex causes severe eye and skin irritation |
| 12 | Pergularia daemia (Forssk.) Chiov. | Latex leads to skin and eye irritation. |
| 13 | Datura metel L. | Accidental consumption of fruits leads to coma, hallucination effects. |
| 14 | Sesamum indicum L. | Consumption of seeds leads to abortion |
| 15 | Acacia nilotica (L.) Delile | Consumption of seeds leads to vomiting |
3.3. Validation of ethno-botanical data using In silico studies
Based on the ethno-botanical uses and literature review the components of the 22 medicinal plants and their pharmacological activities were studied to validate the traditional use by in silico study. The biological spectrum analysis (PASS online) used to reveal the correlation between the activities of structural properties of bioactive compounds (Table 7). Previously, Andrographis paniculata (Burm.f.) Nees was used ethnically in the treatment of skeletal ailments but the predicted biological spectrum (PASS) results of reported compounds revealed these could acts as best hepatic agent (Pa-0.964) and anti-allergic (Pa-0.721) (Table 6). The admetSAR online prediction was also done to predict the absorption, metabolism and toxicity of the listed compounds of medicinally important species (Table 5). From the results all the reported compounds were considered as they can easily metabolized, absorbed and transported through human intestinal [Example spilanthol, oleanolic acid, ramnazin-3-O-rutinoside, 2,4,8,9-tetrahydroxy-6H-(1)benzofuro(3,2-c)chromen-6-one, torvoside A, β-ionone, umbelliferone and (±)-limonene]. The toxicity profile also reveals the carcinogenicity and cardiogenicity of the identified compounds and the results reveals some non-toxic [(±)-limonene, umbelliferone, procyanidin B1 and spilanthol] and less toxic [4-(β-D-glucopyranosyloxy) benzoic acid, vitexin, (2R,3S,4R,5R,6E)-5-acetamido-2-(acetoxymethyl)-6-(hydroxyimino) tetrahydro-2H-pyran-3,4-diyl diacetate, isoorientin and swertisin] properties of the compounds (Table 6). The remaining herbal species also should be investigated to determine the efficacy and safety evaluation.
Table 7.
In silico validation of important ethno-botanical plants of Sathyamangalam wild life sanctuary, Tamil Nadu, India.
| S. No | Binomial name | Ethno uses | Reported pharmacological activities | Reported compounds | PASS prediction |
admetSAR predictiona |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predicted bioactivities | Pa | Pi | A | M | T | |||||
| 1 | Annona squamosa L. | Diabetes Abortion |
Anti-diabetic effect, Effects on early pregnancy48 | 4-(β-d-glucopyranosyloxy)benzoic acid
|
Anti-diabetic activity | 0.988 | 0.001 | + | +++ | + |
| Antiinfective | 0.972 | 0.002 | ||||||||
Procyanidin B1
|
Anti-diabetic activity | 0.979 | 0.001 | +++ | +++ | ND | ||||
| Phobic disorders treatment | 0.929 | 0.004 | ||||||||
| Antiseborrheic | 0.881 | 0.006 | ||||||||
| 2 |
Spilanthes calva DC. and Spilanthes acmella (L.) L. |
Wound Gums ache |
Vasorelaxant and antioxidant activities49 | Spilanthol
|
Wound healing | 0.820 | 0.005 | +++ | +++ | ND |
| Treatment of anxiety disorder | 0.802 | 0.026 | ||||||||
| 3 | Sesbania grandiflora (L.) Pers. | Eye ailments | Anemia, Bronchitis, Ophthalmia, rheumatism hepatoprotective50 | Oleanolic acid
|
Antidiabetic | 0.987 | 0.001 | +++ | +++ | ND |
| Anticancer | 0.984 | 0.002 | ||||||||
| Antinociceptive | 0.895 | 0.001 | ||||||||
| Antineoplastic | 0.877 | 0.005 | ||||||||
| Antiviral | 0.836 | 0.002 | ||||||||
| 4 | Abrus precatorius L. | Stomach ulcer Abortion Dystenry Mouth ulcer Cancer Bacterial fungal infections |
Anti-microbial, Abortion51 | Apigenin
|
Wound healing | 0.963 | 0.003 | +++ | + | ND |
| Anticancer | 0.926 | 0.002 | ||||||||
| Antimutagenic | 0.899 | 0.003 | ||||||||
Vitexin
|
Cardioprotectant | 0.950 | 0.002 | +++ | +++ | + | ||||
| Free radical scavenger | 0.948 | 0.001 | ||||||||
| Hepatoprotectant | 0.920 | 0.002 | ||||||||
| Chemopreventive | 0.864 | 0.003 | ||||||||
| Antihemorrhagic | 0.826 | 0.002 | ||||||||
| 5 | Bauhinia tomentosa L. | Diahorrea | Anti diarrhea, anti-inflammatory activity52 | Hesperidin
|
Free radical scavenger | 0.991 | 0.001 | +++ | ++ | ND |
| Anticarcinogenic | 0.985 | 0.001 | ||||||||
| Chemopreventive | 0.981 | 0.001 | ||||||||
| Hepatoprotectant | 0.977 | 0.001 | ||||||||
| Antiprotozoal | 0.853 | 0.004 | ||||||||
| 6 | Pongamia pinnata (L.) Pierre | Abdominal pain Gas trouble Snake bite Diabetes |
Anti-diabetic53 | Cyqualon
|
Anticancer | 0.927 | 0.004 | +++ | ++ | ND |
| Antidiabetic | 0.703 | 0.008 | ||||||||
| Choleretic | 0.822 | 0.003 | ||||||||
| 7 | Acalypha indica L. | Burns Itch Skin lotion Bacterial and fungal diseases Edema |
Wound healing, Analgesic, anti-inflammatory54 | (2R,3S,4R,5R,6E)-5-Acetamido-2-(acetoxymethyl)-6-(hydroxyimino)tetrahydro-2H-pyran-3,4-diyl diacetate
|
Transplant rejection treatment | 0.936 | 0.002 | ++ | +++ | + |
| Antidiabetic | 0.856 | 0.001 | ||||||||
| 8 | Calotropis gigantean (L.) Dryand. | Rash Edema |
Wound healing55 | Ramnazin-3-O-rutinoside
|
Free radical scavenger | 0.993 | 0.000 | +++ | +++ | ND |
| Cardioprotectant | 0.992 | 0.001 | ||||||||
| Anticarcinogenic | 0.987 | 0.001 | ||||||||
| Antiprotozoal (Leishmania) | 0.918 | 0.003 | ||||||||
| 9 | Vitex negundo L. | Joint pain Head ache |
Arthritis56 | Casticin
|
Antimutagenic | 0.928 | 0.002 | +++ | + | ND |
| Free radical scavenger | 0.845 | 0.002 | ||||||||
| Anticancer | 0.953 | 0.003 | ||||||||
| 10 | Eclipta prostrata (L.) L. | Head ache Abdominal pain Jaundice |
Antibacterial, Antioxidant, hypolipidemic57 | 2,4,8,9-Tetrahydroxy-6H-[1]benzofuro[3,2-c]chromen-6-one
|
Anticancer | 0.956 | 0.003 | +++ | +++ | ND |
| Astringent | 0.823 | 0.001 | ||||||||
| Antiseborrheic | 0.733 | 0.031 | ||||||||
| 11 | Cocculus hirsutus (L.) W.Theob. | Blood tonic Piles Dysentery Diabetes | Spermatogenic and anti-diabetic activity58 | Hirsutine
|
Antinociceptive | 0.814 | 0.002 | +++ | + | ND |
| Analgesic | 0.800 | 0.005 | ||||||||
| Vasodilator | 0.736 | 0.006 | ||||||||
| 12 | Solanum spp. | Mouth ulcer Intestinal disorders Small pox | Neuropharmacological activity59 | Torvoside A
|
Anticancer | 0.942 | 0.002 | +++ | +++ | ND |
| Hepatoprotectant | 0.902 | 0.002 | ||||||||
| Antiprotozoal | 0.896 | 0.003 | ||||||||
| Antineoplastic | 0.872 | 0.005 | ||||||||
| 13 | Aegle marmelos (L.) Correa | Fever Cold Blood tonic Cancer |
Anticancer60 | β-Ionone
|
Antineoplastic | 0.892 | 0.005 | +++ | +++ | ND |
| Dermatologic | 0.831 | 0.004 | ||||||||
| Antipsoriatic | 0.786 | 0.004 | ||||||||
| 14 | Haldina cordifolia (Roxb.) Ridsdale | Anemia Urinary disorders | Anti-amoebic61 | Umbelliferone
|
Cardiovascular analeptic | 0.908 | 0.003 | +++ | +++ | ND |
| Antimutagenic | 0.898 | 0.002 | ||||||||
| Antiseborrheic | 0.875 | 0.006 | ||||||||
| 15 | Citrus aurantiifolia (Christm.) Swingle | Stomachache Blood tonic | Anti-ulcer62 | (±)-Limonene
|
Carminative | 0.961 | 0.001 | +++ | +++ | ND |
| Antieczematic | 0.896 | 0.005 | ||||||||
| Antineoplastic | 0.818 | 0.010 | ||||||||
| Chemoprotective | 0.781 | 0.002 | ||||||||
| 16 | Andrographis paniculata (Burm.f.) Nees | Skeletalmuscular ailments | Anti-inflammatory63 | (−)-Andrographolide
|
Choleretic | 0.980 | 0.001 | +++ | +++ | ND |
| Hepatitis | 0.975 | 0.002 | ||||||||
| Antineoplastic | 0.964 | 0.004 | ||||||||
| Antiallergic | 0.721 | 0.007 | ||||||||
| 17 | Sesamum indicum L. | Genitourinary ailments | Affecting sex hormones64 | Sesamin
|
Anticancer | 0.800 | 0,005 | +++ | + | ND |
| Antineoplastic | 0.797 | 0.012 | ||||||||
| Antidyskinetic | 0.742 | 0.010 | ||||||||
| Antineurotic | 0.738 | 0.030 | ||||||||
| Carminative | 0.761 | 0.004 | ||||||||
| 18 | Oxalis corniculata L. | Blood tonic Fever | Cardioprotective65 | Isoorientin
|
Cardioprotectant | 0.963 | 0.002 | +++ | +++ | + |
| Anticancer | 0.922 | 0.004 | ||||||||
| Hepatoprotectant | 0.913 | 0.002 | ||||||||
| Antihemorrhagi | 0.821 | 0.002 | ||||||||
Swertisin
|
Cardioprotectant | 0.957 | 0.002 | +++ | +++ | + | ||||
| Chemopreventive | 0.901 | 0.002 | ||||||||
| Antineoplastic | 0.783 | 0.014 | ||||||||
| Antidiabetic | 0.769 | 0.005 | ||||||||
| 19 | Zingiber officinale Roscoe | Ear, nose, throat ailments, Neurology ailments |
Digestive disorders66 | Zingerone
|
Antidiabetic | 0.920 | 0.003 | +++ | +++ | ND |
| Fibrinolytic | 0.867 | 0.004 | ||||||||
| Antimutagenic | 0.796 | 0.004 | ||||||||
(+)-[6]-Gingerol
|
Preneoplastic treatment | 0.773 | 0.004 | +++ | +++ | ND | ||||
| Fibrinolytic | 0.758 | 0.008 | ||||||||
| Vasodilator | 0.729 | 0.007 | ||||||||
| Antipyretic | 0.725 | 0.004 | ||||||||
Shogaol
|
Antimutagenic | 0.851 | 0.003 | +++ | +++ | ND | ||||
| Antieczematic | 0.842 | 0.011 | ||||||||
| Mucositis treatment | 0.803 | 0.013 | ||||||||
| Antiinflammatory | 0.732 | 0.012 | ||||||||
| 20 | Cardiospermum helicacabum L. | Skeletal muscular ailments | Anti-arthritic activity67 | Arachidic acid
|
Anti-diabetic | 0.945 | 0.002 | +++ | +++ | ND |
| Phobic disorders | 0.939 | 0.003 | ||||||||
| Mucositis treatment | 0.874 | 0.008 | ||||||||
| Antihypoxic | 0.798 | 0.004 | ||||||||
Luteolin
|
Antimutagenic | 0.915 | 0.002 | +++ | + | ND | ||||
| Vasoprotector | 0.894 | 0.003 | ||||||||
| Antihemorrhagic | 0.836 | 0.002 | ||||||||
| Antioxidant | 0.717 | 0.004 | ||||||||
A-Absorption, M-Metabolism, T-Toxicity; The scale of ranges from low (+), medium (++), high (+++) and not detected (ND).
Table 6.
New uses obtained from informants belongs to Sathyamangalam wild life sanctuary, Tamil Nadu, India.
| S. No | Binomial name | Medicinal uses from present study | Reported medicinal uses from other studies |
|---|---|---|---|
| 1 | Eclipta prostrata (L.) L. | Head ache | Liver injuries, jaundice32 |
| 2 | Abrus precatorius L. | Stomach ulcer, Dysentery, Mouth ulcer | Rheumatism, Anti-diabetic, Head ache35 |
| 3 | Bauhinia divaricata L. | Asthma | Fever14 |
| 4 | Prosopis juliflora (Sw.) DC. | Snake bite | Poisonous effect36 |
| 5 | Pongamia pinnata (L.) Pierre | Abdominal pain, Gas trouble, Snake bite | Diarrhea37 |
| 6 | Canavalia cathartica Thouars | Body pain, Muscle pain | Indigestion16 |
| 7 | Rauvolfia serpentina (L.) Benth. ex Kurz | Heart problem, Cardio tonic | Blood pressure38 |
| 8 | Citrus aurantiifolia (Christm.) Swingle | Stomach ache | Blood tonic39 |
| 9 | Toddalia asiatica (L.) Lam. | Paralyze | Stomachic, Anti-pyretic, Diarrhea40 |
| 10 | Murraya paniculata (L.) Jack | Wounds | Helminthiasis, liver disease41 |
| 11 | Euphorbia hirta L. | Leucorrhoea | Boils, Warts, Ulcers42 |
| 12 | Pergularia daemia (Forssk.) Chiov. | Head ache | Acidity43 |
| 13 | Andrographis paniculata (Burm.f.) Nees | Leprosy | Dyspepsia, anthelmintic, stomach ache5 |
| 14 | Evolvulus alsinoides (L.) L. | Burn, Wound | Fever44 |
| 15 | Rivea hypocrateriformis Choisy | Indigestion | Ethno veterinary important45 |
| 16 | Haldina cordifolia (Roxb.) Ridsdale | Anemia | Urinary disorders14 |
| 17 | Saccharum officinarum L. | Rash | Gastrointestinal ailments, infertility46 |
| 18 | Acacia nilotica (L.) Delile | Piles, Cough | Wound healing and sex related ailments44 |
| 19 | Tinospora sinensis (Lour.) Merr. | Burn wound healing | Insecticides47 |
4. Discussion
4.1. Demographical description and documentation of ethno-botanical data
Comparing the demographical depiction of the present study with other related studies in nearer area, the average age of local population is close in the studied area.14, 15, 16 Among the interviewed communal tribes herbalist and traditional healers were also limited in number, it clearly indicates the improper sharing of their knowledge on medicinal plants. The extensive single species usage in herbal treatment was specify the particular medicine for particular symptom which can be used to treat all related symptoms to the same category with some adjuvant like honey, milk, etc.17,18 This study also claims some poly herbal combinations can be used in the treatment of various gastrointestinal and dermal associated ailments mainly from Fabaceae and Rutaceae family members. It clearly shows the various bioactive contents responsible for the medicinal properties in Fabaceae and Rutaceae.19,20 When compared this medicinal plant (61 plants) diversity of present study with other related regional studies (with 41 and 65 plants) it clearly shows the including of some new reports which are not yet reported.14, 15, 16 This variation in medicinal plant diversity clearly indicates the influence of nature and climate of selected region of the study area. The use of leaf as common medicinal part to treat various ailments was correlated with several ethno-botanical survey and also support the using of other parts because its well known the plants are the factory of chemicals hence its does not denote the particular parts contain more bioactive than other.21 However, the collection of whole plant may be leads to its disappearance from the area and also the collection and abundance of leaf compared with the other parts makes the most using parts in herbal medicine system.22 Oral administration and paste preparation are most common methods used in Siddha medicinal system and similar results of various surveys also supporting the present study results.23,24
4.2. Quantitative analysis of ethno-botanical indices
This study also proves the importance of ethno medicinal plants in the treatment of genitourinary ailment. The ethnic people have grater medicinal information on indigenous plants. Gastrointestinal system and genitourinary ailment diseases have been reported to have the highest ICF in other surveys and these results indicates the sign of unhealthy lifestyle.25,26 Some results from current study also correlated with other surveys carried out in India, such as Cardiospermum halicacabum L. (63%), Solanum nigrum L. (61%) were mentioned to treat same ailment categories in a reported earlier, however these two reported low FL of 63% and 61% respectively to treat skeletal muscular and gastrointestinal ailments category.27 Three of 14 listed ailment categories i.e. eye, oncology and Hemorrhoids ailments reported with low FL < 50%. But related studies also revealed the activities of Aegle marmelos (L.) Correa (18), Sesbania grandiflora (L.) Pers. (19) and Abutilon indicum (L.) Sweet (29) in the reported uses, it clearly shows the lack of sharing their medicinal knowledge among tribal communities.28,29 The higher fidelity level indicates the consent use of these medicinal plants for the treatment of particular ailment by informants of the studied area. However, least CII, UV and IAR values were indicate the limited knowledge of medicinal uses and may be due to its adverse effects of those plants. For example, Annona squamosa L. was recorded and reported as anti-diabetic agent,30 despite the fact consuming the fruit may leads to the abortion.31 Eclipta prostrata (L.) L. used for neurological disorders (headache) by tribes in the present study area. It is also reported to treat Liver injuries and jaundice by the traditional healers of Chithoor district, Andhra Pradesh, India.32 Likewise, there are about 19 species were reported with new uses by comparing with other ethno-botanical studies. This new medicinal information can lead to evaluating active principles to derive new drug molecules.
4.3. Validation of ethno-botanical data using In silico studies
In silico studies are more valuable in ethno botanical research to validate and find potential bioactive compounds which leads in development of new drugs.33 From the PASS results of listed species we found that most of the ethno-botanical uses correlate their predicted bioactivities and some compounds targeted as new ligands for particular receptor targets.34 The greater Pa values indicate the binding capacity of the particular compounds as ligands to that respective receptor.34 In silico studies combined with traditional knowledge evidently recommend a reasonable efficient background and support in the drug formulation of suitable drug for laboratory testing.
5. Conclusion
From this study, 61 ethno-botanical plants among tribes of Sathyamangalam wildlife sanctuary, were validated and documented through in silico for treating various illness categories. The obtained quantitative results (UV, ICF, CII and FL), in silico validation and new reports from this study also used to reveal compounds responsible for bio-activities of herbal formulations. This study results also indicates the importance of experience and knowledge about traditional herbal formulation by the tribes in the treatment of various ailments. The present study suggested promoting programs such as digital documentation of traditional knowledge. These could be used to derive some drug development and application of medicinal plants to treat various disorders and also to promote obtains medicine from nature.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Contributor Information
Pavithra Chinnasamy, Email: pavipkp@gmail.com.
Rajendran Arumugam, Email: arajendran222@yahoo.com, drarajendra@gmail.com.
References
- 1.Panghal M., Arya V., Yadav S., Kumar S., Yadav J.P. Indigenous knowledge of medicinal plants used by Saperas community of Khetawas, Jhajjar District, Haryana, India. J Ethnobiol Ethnomed. 2010;6(1):4. doi: 10.1186/1746-4269-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gurib-Fakim A. Medicinal plants: traditions of yesterday and drugs of tomorrow. Mol Aspect Med. 2006;27(1):1–93. doi: 10.1016/j.mam.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Lewis W.H., Elvin-Lewis M.P. John Wiley & Sons; 2003. Medical Botany: Plants Affecting Human Health. [Google Scholar]
- 4.Mukherjee P.K., Wahile A. Integrated approaches towards drug development from Ayurveda and other Indian system of medicines. J Ethnopharmacol. 2006;103(1):25–35. doi: 10.1016/j.jep.2005.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Alagesaboopathi C. Ethnomedicinal plants and their utilization by villagers in Kumaragiri hills of Salem district of Tamilnadu, India. Afr J Trad CAM. 2009;6(3):222–227. doi: 10.4314/ajtcam.v6i3.57157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ravishankar B., Shukla V.J. Indian systems of medicine: a brief profile. Afr J Trad Complem & Alter Med. 2007;4(3):319–337. doi: 10.4314/ajtcam.v4i3.31226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rates S.M.K. Plants as source of drugs. Toxicon. 2001;39(5):603–613. doi: 10.1016/s0041-0101(00)00154-9. [DOI] [PubMed] [Google Scholar]
- 8.Mutheeswaran S., Pandikumar P., Chellappandian M., Ignacimuthu S. Documentation and quantitative analysis of the local knowledge on medicinal plants among traditional Siddha healers in Virudhunagar district of Tamil Nadu, India. J Ethnopharmacol. 2011;137(1):523–533. doi: 10.1016/j.jep.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Ekins S. Predicting undesirable drug interactions with promiscuous proteins in silico. Drug Discov Today. 2004;9(6):276–285. doi: 10.1016/S1359-6446(03)03008-3. [DOI] [PubMed] [Google Scholar]
- 10.Heinrich M., Ankli A., Frei B., Weimann C., Sticher O. Medicinal plants in Mexico: healers consensus andcultural importance. Soc Sci Med. 1998;47:1863–1875. doi: 10.1016/s0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- 11.Andrade-Cetto A. Ethnobotanical study of the medicinal plants from Tlanchinol, Hidalgo, México. J Ethnopharmacol. 2009;122:163–171. doi: 10.1016/j.jep.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Tardío J., Pardo-de Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of southern Cantabria (northern Spain) Eco Bot. 2008;62:24–39. [Google Scholar]
- 13.Jamkhande P.G., Wattamwar A.S., Pekamwar S.S., Chandak P.G. Antioxidant, antimicrobial activity and in silico PASS prediction of Annona reticulata Linn. root extract. Beni-Suef Uni J Basic & Appl Sci. 2014;3(2):140–148. [Google Scholar]
- 14.Revathi P., Parimelazhagan T. Traditional knowledge on medicinal plants used by the Irula tribe of Hasanur hills, Erode District, Tamil Nadu, India. Ethnobot Leaflets. 2010;4(2):136–160. [Google Scholar]
- 15.Poongodi A., Thilagavathi S., Aravindhan V., Rajendran A. Observations on some ethnomedicinal plants in Sathyamangalam forests of Erode district, Tamil Nadu, India. J Med Plants Res. 2011;5(19):4709–4714. [Google Scholar]
- 16.Revathi P., Parimelazhagan T., Manian S. Ethnomedicinal plants and novel formulations used by Hooralis tribe in Sathyamangalam forests, Western Ghats of Tamil Nadu, India. J Med Plants Res. 2013;7(28):2083–2097. [Google Scholar]
- 17.Muthu C., Ayyanar M., Raja N., Ignacimuthu S. Medicinal plants used by traditional healers in Kancheepuram District of Tamil Nadu, India. J Ethnobiol Ethnomed. 2006;2(1):1. doi: 10.1186/1746-4269-2-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prabhu S., Vijayakumar S., MorvinYabesh J.E., Ravichandran K., Sakthivel B. Documentation and quantitative analysis of the local knowledge on medicinal plants in Kalrayan hills of Villupuram district, Tamil Nadu, India. J Ethnopharmacol. 2014;157:7–20. doi: 10.1016/j.jep.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Valenciennes E., Smadja J., Conan J.Y. Screening for biological activity and chemical composition of Euodia borbonica var. borbonica (Rutaceae), a medicinal plant in Reunion Island. J Ethnopharmacol. 1999;64(3):283–288. doi: 10.1016/s0378-8741(98)00137-8. [DOI] [PubMed] [Google Scholar]
- 20.Gond S.K., Verma V.C., Kumar A., Kumar V., Kharwar R.N. Study of endophytic fungal community from different parts of Aegle marmelos Correa (Rutaceae) from Varanasi (India) World J Microbiol Biotechnol. 2007;23(10):1371–1375. [Google Scholar]
- 21.Dutra R.C., Campos M.M., Santos A.R., Calixto J.B. Medicinal plants in Brazil: pharmacological studies, drug discovery, challenges and perspectives. Pharmacol Res. 2016;112:4–29. doi: 10.1016/j.phrs.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 22.Tandon N., Yadav S.S. Contributions of Indian Council of Medical Research (ICMR) in the area of Medicinal plants/traditional medicine. J Ethnopharmacol. 2016;197:39–45. doi: 10.1016/j.jep.2016.07.064. [DOI] [PubMed] [Google Scholar]
- 23.Usha S., Rajasekaran C., Siva R. Ethnoveterinary medicine of the Shervaroy hills of Eastern Ghats, India as alternative medicine for animals. J Trad Complem Med. 2016;6(1):118–125. doi: 10.1016/j.jtcme.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vijayakumar S., Harikrishnan J.P., Prabhu S., Yabesh J.M., Manogar P. Quantitative ethnobotanical survey of traditional Siddha medical practitioners from Thiruvarur District with hepatoprotective potentials through In Silico methods. Achiev Life Sci. 2016;10(1):11–26. [Google Scholar]
- 25.Sadeghi Z., Mahmood A. Ethno-gynecological knowledge of medicinal plants used by Baluch tribes, southeast of Baluchistan, Iran. Rev Brasil de Farmacog. 2014;24(6):706–715. [Google Scholar]
- 26.Yaseen G., Ahmad M., Sultana S., Alharrasi A.S., Hussain J., Zafar M. Ethnobotany of medicinal plants in the thar Desert (Sindh) of Pakistan. J Ethnopharmacol. 2015;163:43–59. doi: 10.1016/j.jep.2014.12.053. [DOI] [PubMed] [Google Scholar]
- 27.Ayyanar M., Ignacimuthu S. Ethnobotanical survey of medicinal plants commonly used by Kani tribals in Tirunelveli hills of Western Ghats, India. J Ethnopharmacol. 2011;134(3):851–864. doi: 10.1016/j.jep.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 28.Maity P., Hansda D., Bandyopadhyay U., Mishra D.K. Biological activities of crude extracts and chemical constituents of Bael, Aegle marmelos (L.) Corr. Ind J Exp Biol. 2009;47(11):849–861. [PubMed] [Google Scholar]
- 29.Sharma R. Medicinal plants diversity in Bhilai city district Durg, Chhattisqarh, India. Int J Pharm & Life Sci. 2016;7(3):4952–4966. [Google Scholar]
- 30.Gupta R.K., Kesari A.N., Murthy P.S., Chandra R., Tandon V., Watal G. Hypoglycemic and antidiabetic effect of ethanolic extract of leaves of Annona squamosa L. in experimental animals. J Ethnopharmacol. 2005;99(1):75–81. doi: 10.1016/j.jep.2005.01.048. [DOI] [PubMed] [Google Scholar]
- 31.Damasceno D.C., Volpato G.T., Sartori T.C.F. Effects of Annona squamosa extract on early pregnancy in rats. Phytomed. 2002;9(7):667–672. doi: 10.1078/094471102321616508. [DOI] [PubMed] [Google Scholar]
- 32.Reddy K.R. Folk medicine from Chittoor District, Andhra Pradesh, India, used in the treatment of jaundice. Int J Crude Drug Res. 1988;26(3):137–140. [Google Scholar]
- 33.Barlow D.J., Buriani A., Ehrman T., Bosisio E., Eberini I., Hylands P.J. In-silico studies in Chinese herbal medicines' research: evaluation of in-silico methodologies and phytochemical data sources, and a review of research to date. J Ethnopharmacol. 2012;140(3):526–534. doi: 10.1016/j.jep.2012.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lagunin A., Stepanchikova A., Filimonov D., Poroikov V.P.A.S.S. Prediction of activity spectra for biologically active substances. Bioinform. 2000;16(8):747–748. doi: 10.1093/bioinformatics/16.8.747. [DOI] [PubMed] [Google Scholar]
- 35.Sharma H.K., Chhangte L., Dolui A.K. Traditional medicinal plants in Mizoram, India. Fitoterapia. 2001;72(2):146–161. doi: 10.1016/s0367-326x(00)00278-1. [DOI] [PubMed] [Google Scholar]
- 36.Albuquerque U.P., Melo J.G., Medeiros M.F. Natural products from ethnodirected studies: revisiting the ethnobiology of the zombie poison. Evidence-based complem Alter Med. 2012;2012(202508):9. doi: 10.1155/2012/202508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brijesh S., Daswani P.G., Tetali P., Rojatkar S.R., Antia N.H., Birdi T.J. Studies on Pongamia pinnata (L.) Pierre leaves: understanding the mechanism (s) of action in infectious diarrhea. J Zhejiang Uni Sci B. 2006;7(8):665–674. doi: 10.1631/jzus.2006.B0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rahman M.A., Uddin S.B., Wilcock C.C. Medicinal plants used by Chakma tribe in Hill Tracts districts of Bangladesh. Ind J Trad Knowled. 2007;6(3):508–517. [Google Scholar]
- 39.Ong H.C., Norzalina J. Malay herbal medicine in gemencheh, Negri Sembilan, Malaysia. Fitoterapia. 1999;70(1):10–14. [Google Scholar]
- 40.Gritto M.J., Nandagopalan V., Doss A. Ethno-botanical study on the traditional healers in pachamalai hills of Eastern Ghats, Tamilnadu, South India. J Med Pl. 2015;3(2):80–85. [Google Scholar]
- 41.Rahmatullah M., Ferdausi D., Mollik A., Jahan R., Chowdhury M.H., Haque W.M. A survey of medicinal plants used by Kavirajes of Chalna area, Khulna district, Bangladesh. Afr J Trad Complem & Alter Med. 2010;7(2):91–97. doi: 10.4314/ajtcam.v7i2.50859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vedavathy S., Sudhakar A., Mrdula V. Tribal medicinal plants of Chittoor. Anc Sci Life. 1997;16(4):307. [PMC free article] [PubMed] [Google Scholar]
- 43.Kosalge S.B., Fursule R.A. Investigation of ethnomedicinal claims of some plants used by tribals of Satpuda Hills in India. J Ethnopharmacol. 2009;121(3):456–461. doi: 10.1016/j.jep.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 44.Katewa S.S., Chaudhary B.L., Jain A. Folk herbal medicines from tribal area of Rajasthan, India. J Ethnopharmacol. 2004;92(1):41–46. doi: 10.1016/j.jep.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 45.Pandit P.K. Inventory of ethno veterinary medicinal plants of Jhargram Division, West Bengal, India. Ind Forest. 2010;136(9):1183. [Google Scholar]
- 46.Nag A., Galav P., Katewa S.S. Indigenous animal healthcare practices from Udaipur district, Rajasthan. Ind J Tradi Knowl. 2007;6(4):583–588. [Google Scholar]
- 47.Khumukcham N., Biswas D., Singh N.S., Deb L. Herbal Insecticides, Repellents and Biomedicines: Effectiveness and Commercialization. Springer India; 2016. Prospects for development of Biomedicines from the Medicinal plants of Northeastern India; pp. 147–187. [Google Scholar]
- 48.Baskaran R., Pullencheri D., Somasundaram R. Characterization of free, esterified and bound phenolics in custard apple (Annona squamosa L) fruit pulp by UPLC-ESI-S/MS. Food Res Int. 2016;82:121–127. [Google Scholar]
- 49.Barbosa A.F., Carvalho M.G.D., Smith R.E., Sabaa-Srur A.U. Spilanthol: occurrence, extraction, chemistry and biological activities. Revi Brasil de Farmacog. 2016;26(1):128–133. [Google Scholar]
- 50.Wagh V.D., Wagh K.V., Tandale Y.N., Salve S.A. Phytochemical, pharmacological and phytopharmaceutics aspects of Sesbania grandiflora (Hadga): a review. J Pharm Res. 2009;2(5):889–892. [Google Scholar]
- 51.Gupta J., Amit G. Isolation and characterization of flavonoid glycoside from leaves of Abrus precatorius. IJCS. 2016;4(1):14–17. [Google Scholar]
- 52.Rao Y.K., Fang S.H., Tzeng Y.M. Antiinflammatory activities of flavonoids and a triterpene caffeate isolated from Bauhinia variegata. Phytoth Res. 2008;22(7):957–962. doi: 10.1002/ptr.2448. [DOI] [PubMed] [Google Scholar]
- 53.Li L., Li X., Shi C. Pongamone A–E, five flavonoids from the stems of a mangrove plant, Pongamia pinnata. Phytochem. 2006;67(13):1347–1352. doi: 10.1016/j.phytochem.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 54.Rahman M.A., Bachar S.C., Rahmatullah M. Analgesic and anti-inflammatory activity of methanolic extract of Acalypha indica Linn. Pak J Pharm Sci. 2010;23(3):256–258. [PubMed] [Google Scholar]
- 55.Deshmukh P.T., Fernandes J., Atul A., Toppo E. Wound healing activity of Calotropis gigantea root bark in rats. J Ethnopharmacol. 2009;125(1):178–181. doi: 10.1016/j.jep.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 56.Zheng C.J., Zhao X.X., Ai H.W. Therapeutic effects of standardized Vitex negundo seeds extract on complete Freund's adjuvant induced arthritis in rats. Phytomed. 2014;21(6):838–846. doi: 10.1016/j.phymed.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 57.Karthikumar S., Vigneswari K., Jegatheesan K. Screening of antibacterial and antioxidant activities of leaves of Eclipta prostrata (L) Sci Res Essays. 2007;2(4):101–104. [Google Scholar]
- 58.Badole S., Patel N., Bodhankar S., Jain B., Bhardwaj S. Antihyperglycemic activity of aqueous extract of leaves of Cocculus hirsutus (L.) Diels in alloxan-induced diabetic mice. Ind J Pharmacol. 2006;38(1):49. [Google Scholar]
- 59.Arthan D., Svasti J., Kittakoop P., Pittayakhachonwut D., Tanticharoen M., Thebtaranonth Y. Antiviral isoflavonoid sulfate and steroidal glycosides from the fruits of Solanum torvum. Phytochem. 2002;59(4):459–463. doi: 10.1016/s0031-9422(01)00417-4. [DOI] [PubMed] [Google Scholar]
- 60.Charoensiddhi S., Anprung P. Bioactive compounds and volatile compounds of Thai bael fruit (Aegle marmelos (L.) Correa) as a valuable source for functional food ingredients. Int Food Res J. 2008;15(3):287–295. [Google Scholar]
- 61.Iqbal P.F., Bhat A.R., Azam A. Antiamoebic coumarins from the root bark of Adina cordifolia and their new thiosemicarbazone derivatives. Europ J Medi Chem. 2009;44(5):2252–2259. doi: 10.1016/j.ejmech.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 62.Yadav A.R., Chauhan A.S., Rekha M.N., Rao L.J.M., Ramteke R.S. Flavour quality of dehydrated lime [Citrus aurantifolia (Christm.) Swingle] Food Chem. 2004;85(1):59–62. [Google Scholar]
- 63.Rao Y.K., Vimalamma G., Rao C.V., Tzeng Y.M. Flavonoids and andrographolides from Andrographis paniculata. Phytochem. 2004;65(16):2317–2321. doi: 10.1016/j.phytochem.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 64.Wu W.H., Kang Y.P., Wang N.H., Jou H.J., Wang T.A. Sesame ingestion affects sex hormones, antioxidant status, and blood lipids in postmenopausal women. The J Nutrition. 2006;136(5):1270–1275. doi: 10.1093/jn/136.5.1270. [DOI] [PubMed] [Google Scholar]
- 65.Abhilash P.A., Nisha P., Prathapan A. Cardioprotective effects of aqueous extract of Oxalis corniculata in experimental myocardial infarction. Exper Toxicol Pathol. 2011;63(6):535–540. doi: 10.1016/j.etp.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 66.Verma S.K., Singh M., Jain P., Bordia A. Protective effect of ginger, Zingiber officinale Rose on experimental atherosclerosis in rabbits. Ind J Exper Biol. 2004;42(7):736–738. [PubMed] [Google Scholar]
- 67.Jeyadevi R., Sivasudha T., Rameshkumar A., Kumar L.D. Anti-arthritic activity of the Indian leafy vegetable Cardiospermum halicacabum in Wistar rats and UPLC–QTOF–MS/MS identification of the putative active phenolic components. Inflam Res. 2013;62(1):115–126. doi: 10.1007/s00011-012-0558-z. [DOI] [PubMed] [Google Scholar]