Abstract
Background: The purpose of this study was to compare the mechanical properties of metacarpal neck fracture fixation by headless compression screw (HCS) with that of Kirschner wire (KW) cross-pinning and locking plate (LP) fixation. Methods: A metacarpal neck fracture was created in 30 fourth-generation composite Sawbones metacarpal models. A volar-based wedge was removed using a custom jig to simulate a typical apex dorsal fracture, unstable in flexion. The models were divided into 3 equal groups based on the method of fixation: retrograde cross-pinning with two 1.2-mm KWs, 2.0-mm dorsal T-plate with six 2.0-mm locking screws (LP), and a 3.0-mm retrograde HCS. Models were fixed at the proximal end, mounted in a material testing machine, and loaded through a cable tensioned over the metacarpal head, simulating grip loading. Cyclic loading from 0 to 40 N was performed, followed by loading to failure. Load, displacement, and failure mode were recorded. Results: Stiffness of the HCS (7.3 ± 0.7 N/m) was significantly greater than the KW (5.8 ± 0.5 N/m) but significantly less than the LP (9.5 ± 1.9 N/m). With cyclic loading to 40 N, the LP exhibited significantly less displacement (0.2 ± 1.3 mm) compared with the HCS (2.5 ± 2.3 mm) and KW (2.8 ± 1.0 mm). Load to failure for the HCS (215.5 ±3 9.0 N) was lower than that of the KW (279.7 ± 100.3 N) and of the LP (267.9 ± 44.1 N), but these differences were not statistically significant. Conclusions: The HCS provided mechanical fracture fixation properties comparable with KW fixation. The LP construct allowed significantly less displacement and had the highest strength of the 3 fixation methods.
Keywords: metacarpal neck fractures, headless compression screw fixation, mechanical study, K-wire fixation, metacarpal plating
Introduction
Metacarpal fractures are common, representing approximately 40% of all hand fractures with an incidence of 1.5 million annually.8,12,26,30 Fractures of the metacarpal neck, in particular, lack consensus for their management.29 When surgery is indicated, options include a variety of Kirschner wire (KW) constructs including retrograde, transverse, and bouquet pinning; plate and screws; external fixation; and intramedullary nailing. While usually successful in achieving fracture reduction and union, surgical management is associated with a complication rate of up to 36%.5,17,18,21 Common complications include infection,3,18 tendon injury,21 malunion,22 nonunion,22 avascular necrosis,15 stiffness,17,21 and tendon adhesions.7
In response to this relatively high rate of complications, alternative surgical techniques have been sought, including the recently described intramedullary headless compression screw (HCS) fixation.4 This technique involves closed fracture reduction followed by percutaneous retrograde insertion of an HCS across the fracture, countersunk in the metacarpal head. Given the limited exposure and buried hardware, this technique may result in fewer complications such as pin track infection, tendon adhesion, and stiffness. However, the biomechanical performance of an intramedullary screw relative to other fixation techniques is not known. Metacarpal neck and shaft fracture fixation with an HCS was recently studied in vivo with promising functional outcomes and high union rates at 3-month follow-up.23,28 In addition to clinical outcomes, a recent finite element analysis found minimal functional articular surface violation by the HCS in metacarpal fractures despite an intra-articular starting point.27
The purpose of this study was to develop an accurate metacarpal neck fracture mechanical model and then evaluate the strength and stiffness of 3 different fixation techniques—intramedullary HCS, K-wire cross-pinning (KW), and locking plate (LP) fixation.
Materials and Methods
A typical metacarpal neck fracture was created in 30 fourth-generation composite Sawbones (Pacific Research Laboratories, Inc, Vashon, Washington) metacarpal bone models. These were divided into 3 equal groups according to the method of fracture fixation utilized: HCS, KW, and LP. To model a comminuted apex dorsal fracture, unstable in flexion, a wedge of bone was excised at the metadiaphyseal junction using a microsagittal saw and a 3-dimensionally printed custom cutting/fixation jig (Figure 1a). The fractures were then fixed by one of 3 techniques: retrograde bicortical cross-pinning utilizing 1.1-mm KWs; LP fixation with a 2.0-mm T-plate, 1.3-mm thick (Medartis, Exton, Pennsylvania), placed dorsally with six 2.0-mm locking screws; and fixation with a 3.0-mm retrograde intramedullary HCS (Medartis) (Figure 2). Drill holes for all 3 fixation constructs were created using the cutting/fixation jig (Figures 1b and 1c) to ensure that all hardware was identically placed.
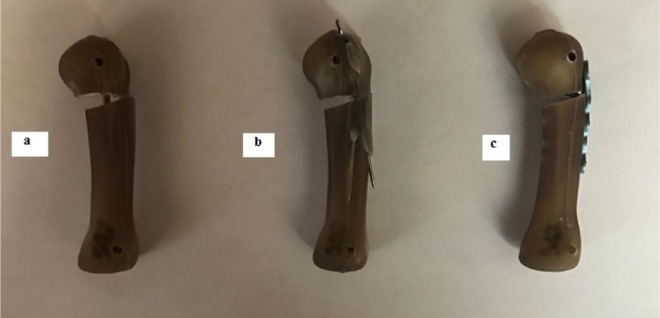
Figure 1.
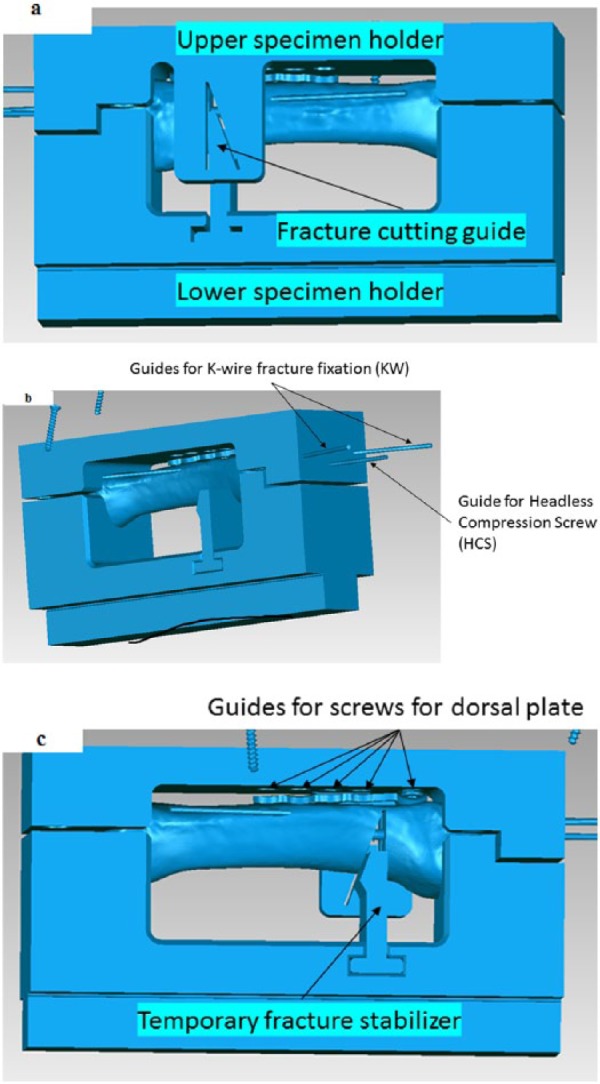
A 3-dimensionally printed custom cutting/fixation jig used for both creating the fracture (a) and for fixing the fracture using a 2.0-mm dorsal T-plate with six 2.0-mm locking screws—LP (b), a 1.2-mm Kirschner wires—KW, and a 3.0-mm retrograde screw—HCS (c).
Figure 2.
Representative models of the fracture fixation constructs: 3.0-mm retrograde screw—HCS (a), 1.2-mm Kirschner wires—KW (b), and 2.0-mm dorsal T-plate with six 2.0-mm locking screws—LP (c).
Following fracture fixation, the proximal end of each model was secured to the base of a materials tensile testing machine (ESM 301 by Testing Machines Inc) through specially designed grips (Figure 3). A metal cable secured to the base of the machine was passed over the metacarpal head, then over a pulley, and secured to a wire grip at the other end of the tensile testing machine. The metacarpal was carefully aligned to ensure that, when the slack from the cable was removed, the cable produced an angle of 85° as it passed over the metacarpal head. This arrangement was intended to simulate loading of the metacarpal bone by flexor and extensor tendon forces produced during grip.19 The force applied to the cable and cable displacement were measured via force and displacement sensors and digitally recorded. The models were loaded cyclically for 20 cycles at a rate of 0.5 mm per second with the force in the cable varying during each cycle from 0 to 40 N. This was done to simulate grip loading during immediate active motion exercises after fracture fixation.24 Following the cyclic loading phase, a progressive load was applied at a rate of 0.5 mm per second until failure. From the recorded cable force and displacement data, the following outcome parameters were calculated: maximum cable displacement during cyclic loading, total stiffness defined as the ratio between maximum force to failure and the corresponding displacement, force to failure, and displacement at failure. In addition, for each specimen, the mode of failure was recorded. Statistical analysis consisting of analysis of variance (ANOVA) followed by a Bonferroni post hoc test was conducted to determine the differences, if any, between the 3 methods of fixation.
Figure 3.
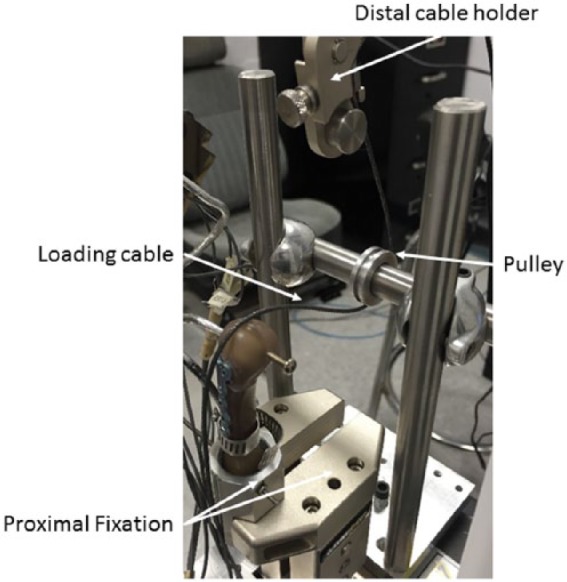
Experimental setup for loading the fracture fixation models. The tensile testing machine (ESM 301 by Testing Machines Inc) was equipped with special grips to hold and align the specimen and to load the specimen in flexion through a cable and pulley system.
Results
The ANOVA analysis showed significant differences between the 3 fixation methods (HCS, KW, and LP) in maximum volar displacement, as measured by total cable excursion, during both cyclic loading (P = .002) and loading to failure (P = .034). The associated Bonferroni post hoc analysis indicated that the HCS and KW fixations produced similar maximum displacements (P > .05). During cyclic loading, both HCS (P = .01) and KW (P = .003) produced maximum displacements that were significantly higher than the LP fixation (Table 1). Also during loading to failure, both produced maximum displacements higher than the LP fixation (Table 1), but only the HCS fixation was significantly different than the LP (P = .03).
Table 1.
Initial Stiffness, Displacement With Cyclic Loading, Final Stiffness, Load to Failure, and Displacement at Failure of the HCS, KW, and LP Models.
| Variables tested | HCS | KW | LP |
|---|---|---|---|
| Displacement after cyclic loading, mm | 2.5 ± 0.1 | 2.8 ± 0.5 | 0.2 ± 1.0 |
| Stiffness, N/m | 7.3 ± 0.7 | 5.8 ± 0.5 | 9.5 ± 1.9 |
| Load to failure, N | 215.5 ± 39.0 | 279.7 ± 100.3 | 267.9 ± 44.1 |
| Displacement to failure, mm | 8.7 ± 2.5 | 6.6 ± 2.8 | 3.6 ± 0.2 |
Note. HCS = headless compression screw; KW = Kirschner wire; LP = locking plate.
The ANOVA analysis showed significant differences in the total stiffness between the 3 fixation methods (P < .001). Specifically, the Bonferroni post hoc analysis showed that the stiffness of the HCS fixation was significantly higher than that of the KW fixation (P = .019), and both the HCS fixation and the KW fixation were significantly lower than the LP fixation (P < .001; Table 1).
There were no statistically significant differences in load to failure between the 3 fixation methods (P = .06). However, the average load to failure of the HCS fixation was lower than both the KW and the LP fixations (Table 1).
All models in the HCS and the KW groups failed by volar displacement of the distal fracture fragment followed by fixation failure at the proximal end (Figure 4). All models in the LP group failed by fracture at their proximal end with no observable displacement of the simulated fracture, minimal to no deformation of the T-plate, and no screw pull-out.
Figure 4.
View of the models of the fracture fixation constructs after failure: 3.0-mm retrograde screw—HCS (a), 1.2-mm Kirschner wires—KW (b), and 2.0-mm dorsal T-plate with six 2.0-mm locking screws—LP (c).
Discussion
Surgical treatment of metacarpal neck fractures has historically been successful.5,17,18,21 A variety of techniques including KW constructs (retrograde, transverse, and bouquet pinning), plate and screws, external fixation, and intramedullary nailing have high union rates and low failure rates.5,17,18,21 In addition, biomechanical studies have found dorsal plating, KW pinning, and intramedullary nailing to have reasonable stability across a metacarpal fracture site with dorsal plating being the most stable.2,16,32 While clinically successful and biomechanically sound, the utility of these strategies is limited by a complication rate of up to 36%.5,17,18,21 These complications include infection,3,18 tendon injury,21 malunion,22 nonunion,22 avascular necrosis,15 stiffness,17,21 and tendon adhesions.7 As a result of these complications, novel fixation techniques have been proposed. One concept proposed and analyzed in the current study is the use of an intramedullary HCS.
HCSs have been used with increasing frequency in hand surgery. This construct was initially described for scaphoid fracture fixation,1,11 but its use has recently increased to a number of different injuries including scapholunate ligament tears,25 radial and ulnar styloid fractures,20 and fractures of the phalanges and metacarpals.7 Metacarpal neck and shaft fracture fixation with an HCS was recently studied in vivo with promising functional outcomes and high union rates at 3-month follow-up.23,28 Furthermore, HCSs have been shown to generate greater than 60 N of compression in previous biomechanical modeling.14 In addition to clinical and mechanical outcomes, a recent finite element analysis found minimal functional articular surface violation by the HCS in metacarpal fractures despite an intra-articular starting point.27 One concern expressed is that of shaft refracture in 2 out of 20 patients after blunt trauma in prior in vivo studies.23 While previous analyses show promise for this construct, the stability of HCS fixation of metacarpal neck fractures has not been studied.
This study compared the mechanical properties of 2 clinically proven metacarpal neck fracture fixation constructs, LP and KW, with an HCS. We aimed to study this novel technique of HCS because of the high complication rates5,17,18,21 in KW and LP constructs reported in prior studies. We compared the 3 techniques in stiffness, displacement with cyclic loading to 40 N simulating active range of motion hand therapy exercises, load to failure, and displacement at failure. The HCS model exhibited similar mechanical properties to the KW but performed inferiorly to the LP model. These results are similar to a biomechanical analysis of metacarpal shaft fractures,6 which found cross-pinning and intramedullary metacarpal nailing had similar biomechanical stability with dorsal plating having superior stability.6
The finding of similar mechanical properties between KW and HCS models is important because KW fixation is clinically proven but with the disadvantage of having exposed hardware which predisposes to infection. A recent analysis of pin track infections in hand and wrist fractures reported a rate of 7%.31 A study of KW placement techniques found that burying pins reduced infection rates from 34.5% to 7.4% in a randomized control trial.13 However, buried pins come with the medical and financial burden of a required secondary procedure to remove the pins.13
The results of this study also found mechanical superiority of dorsal plating, similar to a prior mechanical study of metacarpal shaft fracture fixation.6 However, LP fixation requires a more extensive soft tissue dissection and is associated with greater finger stiffness. A prospective comparative study of LP and intramedullary KW fixation in fifth metacarpal neck fractures found a significantly decreased range of motion in the LP group.9 In addition, the LP construct is associated with an increased risk of tendon injury.21
The findings of this study must be viewed in the context of the strengths and weaknesses of the mechanical testing models. The biggest strength of our study is that our models were highly reproducible as we used identical biomaterials and a hardware placement and cutting jigs. However, as we used Sawbones (synthetic bone models), the reliability of our conclusions as they apply to in vitro applications is limited. In addition, we tested the models only in flexion loading. While this is the most likely mode of failure, lateral bending and rotational loads could contribute to clinical displacement and failure. We did not evaluate rotational stability because rotational malunion of metacarpal neck fractures does not appear to be a true clinical problem. In addition, there are other surgical techniques for metacarpal neck fractures such as bouquet intramedullary pinning10 that were not compared in this mechanical analysis. The preferred pinning technique regionally has been retrograde cross-pinning, and therefore, this KW model was utilized.
In conclusion, the HCS model exhibited similar mechanical properties with a simulated grip model compared with cross-pinning with KWs. The HCS has the benefit of being internally buried in the bone, thus avoiding pin site complications and the restrictions pins place on early motion exercises. While the LP construct was superior in all mechanical testing, this benefit should be weighed against the more extensive surgical dissection required and the potential for tendon adhesions and postoperative stiffness.
Acknowledgments
The authors thank Medartis for its support in this biomechanical study. Medartis provided the implants, cutting jigs, and engineering support. They also thank Jason Toy for his assistance with this project.
Footnotes
Authors’ Note: Investigation was performed at the Biomechanics Laboratory, Department of Mechanical Engineering, Drexel University, Philadelphia, Pennsylvania, and at the Rothman Institute of Orthopaedics, Thomas Jefferson University Hospitals, Philadelphia, Pennsylvania.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This was a purely mechanical study; there were no human or animal subjects. Therefore, a statement of human and animal rights was not applicable.
Statement of Informed Consent: This was a purely mechanical study; there were no human or animal subjects. Therefore, informed consent was not applicable.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Amadio P, Taleisnik J. Fractures of the carpal bones. In:Green DP, Hotchkiss RN, Pederson C, eds. Green’s Operative Hand Surgery. 4th ed. Philadelphia, PA: Churchill Livingston; 1999:809-856. [Google Scholar]
- 2. Barr C, Behn AW, Yao J. Plating of metacarpal fractures with locked or nonlocked screws, a biomechanical study: how many cortices are really necessary? Hand. 2013;8(4):454-459. doi: 10.1007/s11552-013-9544-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Botte MJ, Davis JL, Rose BA, et al. Complications of smooth pin fixation of fractures and dislocations in the hand and wrist. Clin Orthop. 1992;1992(276):194-201. [PubMed] [Google Scholar]
- 4. Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg. 2010;35(8):1260-1263. doi: 10.1016/j.jhsa.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 5. Creighton JJ, Steichen JB. Complications in phalangeal and metacarpal fracture management. Results of extensor tenolysis. Hand Clin. 1994;10(1):111-116. [PubMed] [Google Scholar]
- 6. Curtis BD, Fajolu O, Ruff ME, Litsky AS. Fixation of metacarpal shaft fractures: biomechanical comparison of intramedullary nail crossed K-wires and plate-screw constructs. Orthop Surg. 2015;7(3):256-260. doi: 10.1111/os.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. del Piñal F, Moraleda E, Rúas JS, et al. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg. 2015;40(4):692-700. doi: 10.1016/j.jhsa.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 8. Diao E. Metacarpal fixation. Hand Clin. 1997;13(4):557-571. [PubMed] [Google Scholar]
- 9. Facca S, Ramdhian R, Pelissier A, et al. Fifth metacarpal neck fracture fixation: locking plate versus K-wire? Orthop Traumatol Surg Res. 2010;96(5):506-512. doi: 10.1016/j.otsr.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 10. Foucher G. “Bouquet” osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg. 1995;20(3 pt 2):S86-S90. [DOI] [PubMed] [Google Scholar]
- 11. Grewal R, Assini J, Sauder D, et al. A comparison of two headless compression screws for operative treatment of scaphoid fractures. J Orthop Surg. 2011;6(1):27. doi: 10.1186/1749-799X-6-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harding IJ, Parry D, Barrington RL. The use of a moulded metacarpal brace versus neighbour strapping for fractures of the little finger metacarpal neck. J Hand Surg. 2001;26(3):261-263. doi: 10.1054/jhsb.2000.0509. [DOI] [PubMed] [Google Scholar]
- 13. Hargreaves D, Drew S, Eckersley R. Kirschner wire pin tract infection rates: a randomized controlled trial between percutaneous and buried wires. J Hand Surg Br. 2004;29(4):374-376. doi: 10.1016/j.jhsb.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 14. Hart A, Harvey EJ, Lefebvre L-P, et al. Insertion profiles of 4 headless compression screws. J Hand Surg. 2013;38(9):1728-1734. doi: 10.1016/j.jhsa.2013.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Heo Y-M, Kim S-B, Yi J-W, et al. Avascular necrosis of the head of the third metacarpal bone. J Korean Orthop Assoc. 2012;47(2):146-149. doi: 10.4055/jkoa.2012.47.2.146. [DOI] [Google Scholar]
- 16. Hiatt SV, Begonia MT, Thiagarajan G, et al. Biomechanical comparison of 2 methods of intramedullary K-wire fixation of transverse metacarpal shaft fractures. J Hand Surg. 2015;40(8):1586-1590. doi: 10.1016/j.jhsa.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 17. Kollitz KM, Hammert WC, Vedder NB, et al. Metacarpal fractures: treatment and complications. Hand. 2014;9(1):16-23. doi: 10.1007/s11552-013-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kurzen P, Fusetti C, Bonaccio M, et al. Complications after plate fixation of phalangeal fractures. J Trauma Inj Infect Crit Care. 2006;60(4):841-843. doi: 10.1097/01.ta.0000214887.31745.c4. [DOI] [PubMed] [Google Scholar]
- 19. Liporace FA, Kinchelow T, Gupta S, et al. Minifragment screw fixation of oblique metacarpal fractures: a biomechanical analysis of screw types and techniques. Hand. 2008;3(4):311-315. doi: 10.1007/s11552-008-9108-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Logan AJ, Lindau TR. The management of distal ulnar fractures in adults: a review of the literature and recommendations for treatment. Strategies Trauma Limb Reconstr. 2008;3(2):49-56. doi: 10.1007/s11751-008-0040-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg. 1998;23(5):827-832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 22. Ring D. Malunion and nonunion of the metacarpals and phalanges. Instr Course Lect. 2006;55:121-128. [PubMed] [Google Scholar]
- 23. Ruchelsman DE, Puri S, Feinberg-Zadek N, et al. Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg. 2014;39(12):2390-2395. doi: 10.1016/j.jhsa.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 24. Schnuind F, An K, Cooney W, et al. Advances in the Biomechanics of the Hand and Wrist. New York, NY: Plenum Press; 1994. [Google Scholar]
- 25. Serenó L, Ferrer I, Soy F, et al. Designing and prototyping of new device for scapholunate ligament repair. Proc CIRP. 2013;5:270-275. doi: 10.1016/j.procir.2013.01.053. [DOI] [Google Scholar]
- 26. Statius Muller MG, Poolman RW, van Hoogstraten MJ, et al. Immediate mobilization gives good results in boxer’s fractures with volar angulation up to 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization. Arch Orthop Trauma Surg. 2003;123(10):534-537. doi: 10.1007/s00402-003-0580-2. [DOI] [PubMed] [Google Scholar]
- 27. ten Berg PWL, Mudgal CS, Leibman MI, et al. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg. 2013;38(2):322-330.e2. doi: 10.1016/j.jhsa.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 28. Tobert D, Klausmeyer M, Mudgal C. Intramedullary fixation of metacarpal fractures using headless compression screws. J Hand Microsurg. 2016;8(3):134-139. doi: 10.1055/s-0036-1593390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tosti R, Ilyas AM, Mellema JJ, et al. Interobserver variability in the treatment of little finger metacarpal neck fractures. J Hand Surg. 2014;39(9):1722-1727. doi: 10.1016/j.jhsa.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 30. van Aaken J, Kämpfen S, Berli M, et al. Outcome of boxer’s fractures treated by a soft wrap and buddy taping: a prospective study. Hand. 2007;2(4):212-217. doi: 10.1007/s11552-007-9054-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van Leeuwen WF, van Hoorn BTJA, Chen N, et al. Kirschner wire pin site infection in hand and wrist fractures: incidence rate and risk factors. J Hand Surg Eur Vol. 2016;41(9):990-994. doi: 10.1177/1753193416661280. [DOI] [PubMed] [Google Scholar]
- 32. Watt AJ, Ching RP, Huang JI. Biomechanical evaluation of metacarpal fracture fixation: application of a 90° internal fixation model. Hand. 2015;10(1):94-99. doi: 10.1007/s11552-014-9673-3. [DOI] [PMC free article] [PubMed] [Google Scholar]